* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download amantadine - DavisPlus
Survey
Document related concepts
Transcript
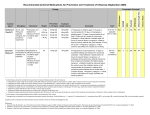
Name /bks_53161_deglins_md_disk/amantadine 02/20/2014 01:33PM Plate # 0-Composite pg 1 # 1 tion. EENT: blurred vision, dry mouth. Resp: dyspnea. CV: hypotension, HF, edema. GU: urinary retention. Derm: mottling, livedo reticularis, melanoma, rashes. Hemat: leukopenia, neutropenia. 1 amantadine (a-man-ta-deen) Symmetrel Classification Therapeutic: antiparkinson agents, antivirals Pregnancy Category C Interactions Drug-Drug: Concurrent use of antihistamines, phenothiazines, quinidine, disopyramide, and tricyclic antidepressants mayqanticholinergic effects (dry mouth, blurred vision, constipation).qrisk of adverse CNS reactions withalcohol. qrisk of CNS stimulation with other CNS stimulants. Indications Symptomatic initial and adjunct treatment of Parkinson’s disease. Prophylaxis and treatment of influenza A viral infections. Route/Dosage Parkinson’s Disease Action PO (Adults): 100 mg 1– 2 times daily (up to 400 mg/day). Potentiates the action of dopamine in the CNS. Prevents penetration of influenza A virus into host cell. Therapeutic Effects: Relief of Parkinson’s symptoms. Prevention and decreased symptoms of influenza A viral infection. Influenza A Viral Infection Pharmacokinetics Absorption: Well absorbed from the GI tract. Distribution: Distributed to various body tissues and fluids. Crosses blood-brain barrier and enters breast milk. Metabolism and Excretion: Excreted unchanged in the urine. Half-life: 10– 28 hr. Renal Impairment TIME/ACTION PROFILE (antiparkinson effect) ROUTE ONSET PEAK DURATION PO within 48 hr up to 2 wk unknown Contraindications/Precautions Contraindicated in: Hypersensitivity. Use Cautiously in: Seizure disorders; Liver disease; Psychiatric problems; HF; Renal impairment (dosep/qdosing interval required if CCr ⱕ50 mL/min); Mayqsusceptibility to rubella infections; OB, Lactation: Safety not established; Geri:qsensitivity to adverse effects. Adverse Reactions/Side Effects CNS: ataxia, dizziness, insomnia, anxiety, confusion, depression, drowsiness, psychosis, seizures, urges (gambling, sexual). GI: nausea, vomiting, anorexia, constipa⫽ Canadian drug name. ⫽ Genetic Implication. PO (Adults and Children ⬎12 yr): Treatment— 200 mg/day as a single dose or 100 mg bid (not ⬎100 m g/day in geriatric patients); Prophylaxis— 100 mg/day in 1– 2 divided doses. PO (Children 10– 12 yr): 100 mg q 12 hr or 5 mg/kg/day in 1– 2 divided doses; not to exceed 200 mg/day. PO (Children 1– 9 yr): 5 mg/kg/day in 1– 2 divided doses; not to exceed 150 mg/ day. PO (Adults): CCr 30– 50 mL/min— 200 mg on the first day, then 100 mg once daily; CCr 15– 29 mL/min— 200 mg on the first day, then 100 mg every other day; ⬍15 mL/min or hemodialysis patients— 200 mg once every 7 days. NURSING IMPLICATIONS Assessment ● Monitor BP periodically. Assess for drug-induced orthostatic hypotension. ● Monitor vital signs and mental status periodically during first few days of dose ad- justment in patients receiving ⬎200 m g daily; side effects are more likely. ● Assess for HF (peripheral edema, weight gain, dyspnea, rales/crackles, jugular ve- nous distention), especially in patients on chronic therapy or with a history of HF. ● Assess patient for the appearance of a diffuse red mottling of the skin (livedo retic- ularis), especially in the lower extremities or on exposure to cold. Disappears with CAPITALS indicate life-threatening, underlines indicate most frequent. Strikethrough ⫽ Discontinued. PDF Page #1 Name /bks_53161_deglins_md_disk/amantadine 02/20/2014 01:33PM ● ● ● pg 2 # 2 ● May cause dizziness or blurred vision. Advise patient to avoid driving or other ac- 2 ● Plate # 0-Composite tivities that require alertness until response to the drug is known. continued therapy but may not completely resolve until 2– 12 wk after therapy has been discontinued. Geri: Monitor intake and output closely in geriatric patients. May cause urinary retention. Report significant discrepancy or bladder distention. Parkinson’s Disease: Assess akinesia, rigidity, tremors, and gait disturbances before and throughout therapy. Influenza Prophylaxis or Treatment: Monitor respiratory status (rate, breath sounds, sputum) and temperature periodically. Supportive treatment is indicated if symptoms occur. Toxicity and Overdose: Symptoms of toxicity include CNS stimulation (confusion, mood changes, tremors, seizures, arrhythmias, and hypotension). There is no specific antidote, although physostigmine has been used to reverse CNS effects. Potential Nursing Diagnoses Impaired physical mobility Risk for infection (Indications) Implementation ● Do not confuse amantadine with amiodarone. ● PO: Do not administer last dose of medication near bedtime; may produce insom- nia in some patients. ● Administering amantadine in divided doses may decrease CNS side effects. ● The contents of capsules may be mixed with food or fluids if the patient has diffi- culty swallowing. ● Antiviral Prophylaxis: Treatment should be started in anticipation of contact or as soon as possible after exposure and continue for at least 10 days following exposure. Infectious period is just before onset of symptoms to up to 1 wk after. If vaccine is unavailable or contraindicated, may be administered up to 90 days to protect from repeated exposures. ● May be used with inactivated influenza A virus vaccine until protective antibody response develops. Administer for 2– 3 wk after vaccine has been given. ● Antiviral Treatment: Administer as soon as possible after onset of symptoms and continue for 24– 48 hr after symptoms disappear. ● Advise patient to make position changes slowly to minimize orthostatic hypoten● ● ● ● ● sion. Inform patient that frequent mouth rinses, good oral hygiene, and sugarless gum or candy may decrease dry mouth. Consult health care professional if dry mouth persists for ⬎2 wk. Advise patient to confer with health care professional before taking OTC medications, especially cold remedies, or drinking alcoholic beverages. Instruct patient to notify health care professional if confusion, mood changes, difficulty with urination, edema and shortness of breath, new or increased gambling, sexual, or other intense urges, or worsening of Parkinson’s disease symptoms occurs. Antiviral: Instruct patient and family to notify health care professional if influenza symptoms occur when amantadine is used as prophylaxis or if symptoms do not improve in a few days when product is used for treatment. Parkinson’s Disease: Advise patient that up to 2 wk of therapy may be needed for full benefit of medication. Notify health care professional if medication gradually loses its effectiveness. Amantadine should be tapered gradually; abrupt withdrawal may precipitate a parkinsonian crisis. Evaluation/Desired Outcomes ● Decrease in akinesia and rigidity. Full therapeutic effects may require 2 wk of therapy. ● Absence or reduction of influenza A symptoms. Why was this drug prescribed for your patient? Patient/Family Teaching ● Advise patient to take medication around the clock as directed and not to skip doses or double up on missed doses. If a dose is missed, do not take within 4 hr of the next dose. 䉷 2015 F.A. Davis Company PDF Page #2