* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download co management guidelines
Survey
Document related concepts
Transcript
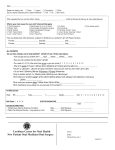
MEMORANDUM TO: Co-Managing Optometrists FROM: R. Douglas Cullom, M.D. DATE: January 1, 2006 RE: Co-management of Surgical Care Cullom Eye and Laser Center is committed to complying with specific statutes and regulations governing the practice of medicine and optometry. With this in mind we have revised our co management process to ensure the decision to co management is a result of a determination of what is best for the patient and not economic considerations. If co management is done on a routine basis for predominantly financial reasons, it represents unethical behavior. Above all patients’ interest must never be compromised as a result of co management. Included in the packet are guidelines for compliant co management, pre and post evaluation guidelines, patient consult forms, transfer of care and acknowledgement of division of care related to fees forms, helpful hints for filing Medicare global fees and a quick guide on calculating the split. Thank you for the opportunity to co manage cataract and refractive patients. I appreciate your assistance with these compliance guidelines. As always, please do not hesitate to give me a call if you have any questions. ___Doug Cullom________ R. Douglas Cullom, M.D. CO MANAGEMENT GUIDELINES Co-management is defined as the sharing of postoperative responsibilities between the operating surgeon and another provider. If co management of surgical patients is being considered, justifiable circumstances* should exist. Co management requires a written transfer agreement** between the surgeon and the receiving doctor. The receiving doctor cannot bill*** for any part of the service included in the global period until (s) he has provided at least one service. Specific modifiers must be used on claims (54,55) *Justifiable circumstances: Situations that arise where surgeon concludes the delegation of postoperative care is in the patients best interest. The patient must voluntarily consent to this in writing. Justifiable circumstances include: surgeon taking leave of absence, patient is unable to travel, large distance between patients home and surgeon’s office, patient voluntarily wishes to be followed by another provider. Comanagement is not to be done as a matter of routine policy on all patients. **Transfer agreement: A transfer agreement between the surgeon and the receiving doctor (optometrist) contains the surgeon’s discharge instructions and effective transfer date. A unique transfer agreement should be constructed for each patient. For overlapping postoperative co-management of 2nd eye, if the surgeon has transferred care for the first operated eye prior to the second surgical procedure then two transfer letters must exist. The patient must be reassured that he/she has access to the surgeon, if necessary at no additional cost. ***Billing: Modifier 54 is used to designate the surgical event; modifier 55 is used with the claims for postoperative care. 66984-55 = surgical event 66984-55 = postoperative care by surgeon 66984-55 postoperative care by the receiving doctor/co-manager. Co-management is working together and relies upon effective communication in both directions. There needs to be coordination between the surgeon and the receiving office to make sure all pre-operative requirements are met and all post op days are accounted for. Pre & postoperative examination guidelines for reports. Herewith please find samples for preoperative evaluation. Please forward preoperative examination along with transfer agreement prior to patients visit with surgeon. Please note preoperative evaluation for specific guidelines. Please forward postoperative report upon completion by fax. Fax number (757) 345-3102 Cataract and Refractive Lensectomy Guidelines Cataract Preoperative Evaluation Patient’s who are determined to have a visually significant cataract that is affecting the patient’s ability to do daily activities can be referred to Dr. Cullom for a pre-operative consultation. During that visit, in addition to the examination, Dr. Cullom will go over the risks and benefits of cataract surgery and have an operative consent signed. The patient is usually set up for another visit to have biometrics performed-keratometry, A scan and IOLmaster. This will assist in choosing the proper intraocular lens. Logistical aspects of the surgery as well as medications are discussed. Counseling includes a discussion of the expectations concerning best corrected visual acuity(BCVA) including preoperative conditions that may prevent perfect results, such as age related macular degeneration. Counseling regarding uncorrected visual acuity (UCVA) may address goals of surgery i.e. plano for distance or being left moderately nearsighted to allow for near work to be performed without correction. Realistic expectations are discussed. Patients with high amounts of astigmatism may not be able to rid themselves entirely of glasses. Possible upgrade to a multifocal implant may be considered if the patient desires. Indications: The primary indication for cataract surgery is decreased vision or glare from cataract formation causing a decreased ability to perform daily activities. Other indications may be traumatic injury to the lens, phacomorphic glaucoma and phacolytic glaucoma, Refractive Lensectomy Pre-operative Evaluation Although patients who undergo refractive lensectomy undergo essentially the same procedure as cataract patients they require much more counseling-especially regarding expectations. They also need a careful pre-operative examination to be certain that they are good candidates for refractive lensectomy (RL). Refractive lensectomy may also involve a discussion of multifocal lenses and issues associated with this choice. Present options include the Alcon ReSor lens and the AMO Rezoom lens. The ReStor lens provides good near, fair intermediate vision, and good distance vision. The Rezoom lens give good near and intermediate distance vision, but has a slightly higher incidence of night vision flare and halos. Both lenses result in a small compromise for distance vision, but may allow patients to be less reliant on glasses. Patients presently doing monovision should be treated as such with standard intraocular lenses. Patients that are more particular about good distance vision such as engineers, pilots, truck drivers or just those who desire the best distance vision possible should stick with standard intraocular lenses set for distance. Indications: The desire to eliminate or decrease the dependence on glasses or contacts for distance and/or near vision is the main indication for RL. The best RL patients are those over 40 years particularly those in their 50’s or older who may have early nuclear sclerosis or other cataractous changes of the lens, however do not have much loss of actual visual acuity. Because of this, they do not qualify for cataract surgery by their insurance carrier or Medicare. Hyperopes, especially over +2.00 dioptors may be especially good candidates. This range is less predictable with conventional lasik. High myopes who do not qualify for LASIK may be good candidates, but do have an increased risk of post-op retinal detachment. Patients who are presently in mono-vision contact lenses may also make excellent candidates. Astigmatism can be controlled by changing the location of the incision or utilizing a toric intraocular implant, but high amounts make less predictable results. Remaining astigmatism can be treated after healing by LASIK or PRK if the patient desires. Cataract Surgery and Refractive Lensectomy Risks and Alternatives RISKS (this section is written in layman’s terms) Surgery is performed under topical anesthesia with intravenous sedation resulting in minimal patient discomfort. Mild discomfort for the first 24 hours is typical, but severe pain would be extremely unusual. Since this RL is essentially the same as cataract surgery, the same risks apply. These risks include, but are not limited to: 1. Infection, which if serious can lead to complete loss of vision 2. Swelling in the central area of the retina, cystoid macular edema, which usually improves with time. 3. Clouding of the outer layer of the eye, corneal edema, which typically resolves, but in rare cases requires correction with corneal transplantation. 4. Detachment of the retina (particularly in highly near-sighted eyes). Retinal detachment can usually be repaired. 5. Increased astigmatism 6. Inaccuracy of the intra-ocular lens power 7. Decentration of the intra-ocular lens, which may provide unwanted images and increased glare 8. Development of increased pressure in the eye (glaucoma). 9. The need for a second operation to remove retained lens fragments in very rare cases. Although all of these complications can occur, their incidence following cataract surgery is very low. DISADVANTAGES OF SURGERY 1. One definite disadvantage that may be more obvious with clear lensectomy, (especially in a patient less than 50 years of age), is the loss of the near focusing power of the eye (accommodation). Thus, it must be clearly understood that even with a successful surgery and an accurate intraocular lens calculation targeted to correct the eye’s distance vision, close vision will usually remain blurred, requiring a separate pair of glasses for close and intermediate vision. It may be possible to deliberately correct one of the eyes for close vision instead of distance, which would allow the patient to read without glasses, even though this eye would then be nearsighted and require a corrective lens for distance vision. This combination of a distance eye and a reading eye is called monovision. It has been employed quite successfully in many contact lens patients. This option will be discussed and demonstrated by the operating surgeon. A discussion of the multifocal intraocular lenses Rezoom or ReStor may also be addressed. These lenses require extensive discussion of near, intermediate issues as well as possible induced night vision problems. 2. Even with the latest formulas used to evaluate lens implantation power it is possible to be off on predicted refractive outcome. This is more common in high refractive errors. In the event of a minor error in the calculation, the vision can usually be corrected by a glass prescription, which should be considerably weaker than the patient’s original prescription. A large error in the lens calculation could be corrected by a stronger pair of glasses, contact lenses, or the exchange of the implant or the insertion of a second implant in another operation, or possibly laser surgery. 3. Since only one eye will undergo surgery at a time, the patient will experience a period of imbalance between the two eyes (anisometropia). This usually cannot be corrected with spectacle glasses because of the marked difference in the prescriptions, so the patient will either temporarily have to wear a contact lens in the non-operated eye or will function with only one clear eye for distance vision. Surgery, in the second eye can usually be accomplished within 1 to 4 weeks, once the first eye is stabilized. NON-SURGICAL ALTERNATIVES Non-surgical alternatives to clear lens extraction are to continue to wear spectacle lenses or contact lenses. Although there are essentially no risks to wearing glasses, the quality of vision with strong farsighted or nearsighted glasses is not normal because of an enlarged image and a slight decrease in peripheral vision caused by the thickness of the lenses. Although contact lenses provide higher quality and more normal vision, they have a slight risk of complications, especially if they are worn overnight. The risks of contact lenses include: infection, which if involving the central cornea can rarely cause loss of vision; allergies (giant papillary conjunctivitis, GPC) which can make wearing the lenses difficult; mild irritation; and discomfort. Alternatives to cataract surgery includes changing daily activity habits, such as stopping night driving and using better lighting when reading. Post-operative Management Of Cataract Surgery and Refractive Lensectomy Postoperative Visit Schedule* Day 1-Surgeon 1 Week 4-6 weeks 3 months (optional) *This is a minimal recommendation. Increase frequency of visit with any unusual findings or significant change in vision. Always refer patient back to surgeon immediately if there are any concerns about recovery. Frequently cataract surgery on the second eye is indicated one or two weeks after the first procedure. In this case the one week visit may be performed by the surgeon the day after the second eye operation. Medications: Zymar antibiotic- one drop operated eye four times a day for one week Acular non-steroidal- one drop operated eye four times a day for one week Pred Forte steroid - One drop operated eye four times a day for one week then One drop operated eye three times a day for one week then One drop operated eye two times a day for one week then One drop operated eye one time a day for one week. Medication flow sheet outlining above is provided to patient Note Zymar and Acular are begun the day prior to surgery and must be filled at the pharmacy by a script provided by Dr. Cullom. Pred forte is supplied by Dr. Cullom Zymar is a broad spectrum flouraquinalone topical antibiotic Pred forte steroid helps control post-operative inflammation Acular, a non-steroidal anti-inflammatory, has been shown to decrease the incidence of cystoid macular edema as well as anterior segment inflammation. Patients with pre-operative glaucoma should continue their glaucoma medications Post-operative Guidelines: If there are any concerns about your patient whether from a post-operative examination or a worrisome call to your office by the patient please call our office immediately to arrange an examination by the surgeon. If Dr. Cullom is not available, there is always an ophthalmologist on call who will see your patient. Calling 757.875.7875 or 345-3001 at any time will get you in touch with our office or the ophthalmologist on call. All visits: -check uncorrected visual acuity (UCVA)-operated eye at distance - check UCVA-operated eye at near if goal is near vision -careful slit lamp exam -Intraocular pressure Dilated funduscopic exam should be done if vision is below that expected or with new or significant symptoms of flashes, floaters, or shadows in vision. Manifest refraction and new glasses prescription is usually done 3-4 weeks post-operatively, but occasionally sooner if required Common complaints occurring at any visit: Foreign body sensation at incision. Explain to the patient that this can last for several months in some cases, though usually is present only for a couple of days. If bothersome I will begin patient on erythromycin ointment at bedtime for a week and increase artificial tears. Unusual visual sensations, photopsias, often noted on day one as arcuate peripheral light. Reassurance that these almost always go away completely. If these are described a pulsation of peripheral flickers and associated with new onset floaters, a careful dilated peripheral retinal exam is indicated. Post-op day 1 (done by the surgeon) UCVA Slit lamp exam IOP UCVA –Occasionally lower than expected if there is some residual corneal edema. A manifest refraction may be done especially in refractive lensectomy patients if UCVA is not what is expected. Slit lamp exam-Evaluate cornea for edema. Carefully check anterior chamber for inflammation and depth. Note that wound is secure. (Usually this is a self sealing suture-less wound. IOP-May be elevated from retained viscoelastic. Although this material protects the corneal endothelium during surgery, it frequently results in increased IOP for 24-48 hours. If pressure is significantly elevated i.e. above 30 mmHg the surgeon may elect to put gentle pressure on the limbus posterior to the paracentesis incision to allow aqueous to drain from the anterior chamber. This is done after instillation of topical antibiotic. This procedure should be done only by the surgeon and never beyond post-op day one. Increased pressure can also be treated with standard glaucoma medications as indicated. 1 Week Post-op Visit UCVA Consider Manifest Refraction with BCVA (optional) Slit Lamp Exam IOP Counseling UCVA, BCVA and Manifest Refraction-. Presbyopic patients may require temporary or permanent reading glasses particularly if the pre-op goal was plano. Refraction is optional on this visit. Slit lamp examination- Cornea should be clear. An occasional patient may have a foreign body sensation at the wound which can be helped with nightly erythromycin ointment. Anterior chamber reaction should be gone. An increase in cell and flare may indicate early endophthalmitis especially if accompanied by increased vitreous cells, decreased vision or pain. Patients with any significant anterior chamber inflammation should be referred immediately to the surgeon. Posterior chamber intraocular lens should be in good position. IOP -should be normal. Occasionally a “steroid responder” may have an increased IOP from the steroid use and a quick taper of the Pred Forte may be considered or topical glaucoma medications may be considered. Counseling- Presbyopic patients, even when properly counseled before surgery may have difficulty adjusting to new reading glasses. Monovision patients may struggle with an adjustment period as well. Temporary glasses for distance or near may be required until second eye is done. Refractive lensectomy patients may be more demanding and concerned about uncorrected visual acuity. They may have post-operative astigmatism that requires PRK or LASIK. This can be discussed with the surgeon. Small amounts of residual astigmatism are usually not treated with laser correction. 1 Month Post-operative visit UCVA MR with BCVA Slit lamp exam IOP Dilated funduscopic exam UCVA, BCVA, Manifest refraction-spectacle correction if required are given at this visit Slit lamp exam: Cornea and anterior chamber should be clear. IOP-should be in control Dilated funduscopic exam-should be performed. Diabetics need to watched closely for worsening of nonprolifitive diabetic retinopathy which commonly occurs during the first post-operative month Counseling: Most patients are doing very well at this visit. Now that the excitement of their new vision is less acute, many patients may have minor problems that need discussion. Problems such as minor eye dryness or the need for new or different reading glasses are generally easily corrected. 3 Month Post-operative Visit (if required) UCVA BCVA with manifest refraction Slit Lamp Exam Applanation Tonometry LASIK, LASEK and PRK Guidelines LASIK, LASEK & PRK Pre-operative Evaluation All LASIK and surface laser correction at the Cullom Eye and Laser Center is performed with the latest and most up to date technology available. Flap formation is done with the Intralase laser which allows for a more consistent and thinner flap. This decreases the incidence of post LASIK dry eye. It also greatly reduces the chance of flap complications. There are also less induced high order aberrations than a bladed keratome, and several large studies have shown that lasik with laser flaps give better visual outcomes than bladed keratomes. Customized wavefront guided treatments have been shown by the FDA to give slightly better quality of vision in dim illumination as well as a higher chance of better than 20/20 visual outcomes. All patients who qualify for customized laser correction will automatically be treated by that method at the Cullom Eye and Laser Center. Patients who are out of the custom diopter range or have other contraindications may be treated by non custom LASIK. Proper patient selection is of utmost importance in obtaining excellent results with LASIK and PRK. Proper selection requires a thorough history addressing patient motivation and expectation, a complete medical and surgical history and a complete dilated eye examination, topography and pachymetry. For the convenience of the co-managing doctor, pachymetry, topography wave-front analysis* and additional pre-operative evaluation can be scheduled with Dr. Cullom or his staff at Hampton Roads Eye Associates in Newport News or the Laser Center in Williamsburg. (At this time Wave-front analysis portion of evaluation is only being performed at the Williamsburg location) Candidacy Myopia to -11 Diopters Hyperopia to +6 Diopters Astigmatism to -6 Diopters Astigmatism combined with hyperopia or myopia is treatable with the VISX laser. Age 18 yrs or older Stable refraction-less than 3/4 Diopter change over a year Contraindication to LASIK or PRK: Active collagen vascular, autoimmune or immunodeficiency diseases (Systemic Lupus Erythemetosis, Rhuematoid Arthritis, Sjögren's disease etc.) Medication use-amiodarone, isotretinoin (Accutane) Ocular Herpes zoster or simplex Pregnancy Keratoconus Caution: Diabetes (must be well controlled) Severe atopic disease Severe amblyopia History Motivation The reason a patient desires Laser Vision Correction will give the examining doctor an understanding of patient expectations and desires. Patient motivations may be occupational, recreational, or purely lifestyle related. It is important to document the patient's occupation and hobbies to determine how they use their vision. Spectacle wearing low myopes i.e. -2.00 dioptors in the early presbyobic age should be given extra attention since they may be accustomed to taking their glasses off for reading. A frank discussion of the tradeoffs of correcting all their myopia as well as the option of monovision should be discussed. Although LASIK is generally safe for patients with very active lifestyles, those expecting frequent blows around the eyes like boxers and karate participants may consider PRK as an alternative. Patients having unrealistic expectations should be screened out during this phase of the exam. Past Medical history: Active collagen vascular diseases including Rheumatoid Arthritis, Systemic Lupus Erythemetosis, Sjogren's disease-may increase risk of scarring and corneal melts Diabetes mellitus that is in poor control may result in poor refractions. Refractive surgery should be avoided in those with significant retinopathy. Pregnancy-hormonal changes during pregnancy can alter refractions therefore LASIK is postponed until several months after pregnancy. Family history of significant medical or ocular diseases Past Ocular History Contact Lens HistoryType of lens: Soft daily wear, Soft extended wear, Rigid Gas Permeable, PMMA. Hours/day Note: Before final refraction and topography, patients should be out of their contact lenses for: * Soft lenses- 10-14 days minimum RGP lenses-3 weeks minimum or until refraction is stable *Logistically, this can be difficult to achieve. For the co-managing doctor and the patient's convenience we frequently do the final refraction and topography the day prior (preferably) or the day of the surgery. This limits the patient's time out of contact lenses. Ocular surgeries, corneal injuries, dry eyes History of herpes simplex or zoster keratitis-LVC contraindicated Glaucoma -patients with well-controlled glaucoma may be considered for LVC. Proper baseline studies are important since IOP measurements measure lower after LVC. Retinal diseases/injuries Strabismus surgery Medications Drug allergies-including history of steroid response glaucoma Accutane and Amiodorone -increase risk of corneal scarring Prednisone -may alter refraction, increase risk cataract formation Mydriasis inducing medications-many OTC medications as well as "herbal" – appetite suppressants can enlarge the pupils. Patients with large pupils on initial evaluation should return after stopping these medications to re-check pupil size. Ocular Examination Visual Acuity-uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) If the patient is not correctable to 20/20, evaluate the cause of reduced vision. These include irregular corneal curvature (corneal warpage or keratoconus), corneal or lenticular opacity, and retinal or optic nerve pathology. In the absence of these findings and after other indicated studies are obtained amblyopia may be diagnosed. Refraction-manifest and cycloplegic. Perform the cycloplegic refraction with 1 % cyclogyl in younger patients and 1% mydriacyl in older patients. It is important to "push plus" as many patients are discovered to be over "minus" in their present correction. Treatment of these patients can lead to over corrections. Care must be taken to find all the cylinder correction. Use Keratometry and retinoscopy to help uncover subtle astigmatism. Contact lenses must be out as noted above prior to a final refraction. Pupil size-should be checked in dim illumination. Patients with large pupils, particularly high myopes, are at increased risk for night vision problems such as halos, starburst and decreased night contrast sensitivity. This is felt to be less of a problem with custom treatments. Motility exam-Significant phorias and tropias should be documented. Patients who have prism in their glasses to control diplopia should not be treated. Though they may see 20/20 with each eye, there may be diplopia without the prism correction. Manual keratometry: will help in finding subtle astigmatism. Distortion of the mires is a warning sign of irregular astigmatism and possibly keratoconus. Tonometry - obtain as a baseline on all patients. IOP by appplanation tonometry usually runs lower after laser vision correction. Anterior slit lamp examination: Lids/lashes: Blepharitis should be identified and controlled prior to LASIK/PRK. Lid abnormalities may predispose to exposure and poor healing. Cornea: It is very important to identify anterior basement membrane disease (ABMD)--which can be seen as subtle microcysts or "fingerprints" below the epithelium on retroillumination. These patients do better with PRK instead of LASIK. PRK may smooth away this redundant basement membrane and it avoids the sloughing that occurs when undergoing LASIK. Search for evidence of dry eye syndrome such as decreased tear film break up time and corneal punctate staining. Other corneal disease such as Fuch's dystrophy should be identified. Old corneal scars should be documented. Anterior chamber: should be without evidence of inflammation. Lens: document lens opacities-even if minor. Lensectomy and intraocular lens placement may be a better refractive surgery choice for those with significant cataract formation. Dilated Funduscopic Exam-The macula should be examined for evidence of myopic or age related degeneration. A careful peripheral retinal exam is done to rule out lattice degeneration, retinal holes or breaks. The pressure of the suction ring during LASIK may slightly increase the risk of retinal detachment in patients with these conditions. Schirmer's test with anesthesia- perform on any patient with evidence of dry eye syndrome. Consider this on women over 40 and patients over 50 yrs. Place punctal plugs and or consider twice daily restasis therapy PRIOR to LASIK on any patients with significant dry eye signs or symptoms and those with Schirmer's less than 5 mm. Pachymetry*-is critical in determining adequate tissue for LASIK (including possible enhancement) on high amounts of myopia. Although intralase flaps allow for thinner and more accurate flaps, occasionally a thin cornea will preclude treatment of even moderate amounts of myopia. Patients with borderline corneal thickness may be better candidates for surface treatments such as PRK. Corneal topography*-is used to look for evidence of irregular astigmatism, keratoconus, form fruste keratoconus, and contact lens related corneal warpage. Keratoconus and significant irregular astigmatism is a contraindication for LASIK/PRK. Follow patients with contact lens related corneal warpage until corneal topographies are stable. Use corneal topography to uncover subtle regular astigmatism and guide the refraction. Lasik, Lasek & PRK Post-operative Management Postoperative Visit Schedule* LASIK Day 1 1 Week 1 Month 3 Months 6 Months 1 Year PRK Day 1 Day 2-5 (as needed until epithelialized) 1 Week 1 Month 3 Month 6 Month 1 Year * This is a minimal recommendation. Increase frequency of visit with any unusual findings or significant change in vision. When in doubt always refer patient back to surgeon for second opinion. Medications: See medication sheets on the following pages for medication protocols for LASIK and PRK/LASEK. These are handed to patients at the time of surgery. I encourage preservative free artificial tears at least four times a day for the first month. Take care that PRK patients do not suddenly stop there pred forte taper. Usual pred forte tapering regimen for PRK is 4 times a day for one week, the 3 times a day for one week, then twice a day for one week, then daily for one week. (We supply all drops to the patient the day of surgery) Post-operative Guidelines: All visits: -check uncorrected visual acuity (UCVA)-OU -careful slit lamp exam All visits after 1 week: -consider Manifest Refraction and best corrected visual acuity (BCVA)-OU Many rare but serious complications (infectious keratitis, diffuse lamellar keratitis, and epithelial ingrowth) can present the first week, therefore never allow patients to postpone this visit. Check tonometry at 3 months and sooner if on topical steroids. Prior to enhancement patient must undergo cycloplegic refraction. Enhancements are considered when the refraction is stable-typically not until three months. Post-op day 1 (normally done by the surgeon) UCVA Slit lamp exam Counseling UCVA -day one is highly variable. Though typically 20/20 to 20/30, it may be up to 20/50 in high myopes. Day one UCVA is not predictable of final UCVA. Patients are typically over-corrected initially in anticipation of slight regression – especially hyperopes. Patients under-corrected at day one and one week may also improve considerably as the epithelium smoothes, dryness improves and the flap settles. Slit lamp exam-Day one the most important evaluation is of the flap placement. The edge of the flap is mostly epithelialized by the next day. Some edema may be present which will disappear by the next visit. StriaeEvaluate carefully for shifted or dislodged flaps (usually from rubbing the eye the first 2-4 hrs after the procedure). Fine peripheral microstriae are common in higher myopes, as the flap needs to settle in an area to which significant tissue has been removed. These may be observed. Return to the surgeon, any patients with significant central microstriae, especially accompanied by poor BCVA, for re-floating of the flap. Macrostriae involve deeper layers of the cornea and must be seen by the surgeon. Any patients with questionable striae should be returned to the surgeon since the treatment is much easier and effective right after surgery. Interface Debris -minor interface debris-such as meibomian secretions, small fibers are of minimal significance and do not affect visual acuity. The surgeon should remove any fibers protruding from the border of the flap. These can act as wicks and introduce infection under the flap. Epithelial defects -are now extremely rare with the introduction of the intralase laser flap. They may rarely occur in patients with peri-operative trauma such as rubbing the eye (look also for a dislodged flap) in hyperopes, patients with anterior basement membrane syndrome (ABMD), dry eyes and older age. Epithelial defects are treated with a bandage contact lens (BCL) after surgery. Follow these patients daily with BCL in place until healed. Careful removal of the BCL using artificial tears and avoiding the flap is essential. Watch patients with significant epithelial defects closely for interface inflammation such as DLK. They may also take slightly longer to achieve good UCVA. Diffuse lamellar keratitis (DLK, Sands of the Sahara)-presents 1-5 days after LASIK. Inflammation is confined to the interface with no flap or stromal extension in early phases (as opposed to infection). A “pseudoDLK” appearance with minor fine haze at the peripheral flap is sometimes seen with the intralase flaps. This is opposed to the true granular appearing cells of DLK. Any doubts treat as DLK. Grade 1: white granular cells in the periphery of the interface Grade 2: White granular cells in the interface center involving the visual axis with or with out peripheral involvement Grade 3: Dense aggregates of clumped cells appear centrally with relative clearing peripherally. Grade 4: Scarring and stromal melting Etiology is unclear, but epidemic cases are related to endotoxin exposure or oils from keratome blades. Grade 1 and 2 are treated with intensive topical steroids-initially every one hour- with topical antibiotic coverage. Grades 3 and 4 require lifting the flap for interface irrigation and scrapping and possible oral steroids. One should always be aware that infectious keratitis, though rare, may initially mimic DLK. Suspect infection with any inflammation extending into the stroma and flap especially when associated with pain. Suspected cases of DLK or infectious keratitis are referred immediately to the surgeon for evaluation and treatment. Patients with large epithelial defects or looseness are followed closely during the first week for DLK. Counseling- Remind patients during the early postoperative period to expect: 1. fluctuations in vision 2. intermittent dryness 3. night vision problems These symptoms are more common with higher corrections and generally resolve over the next several weeks. I mention that although their Snellen Acuity may be excellent on day one; expect a big improvement in the quality of vision. Research on Navy Seals undergoing Laser Vision Correction demonstrated subtle contrast sensitivity loss in dim illumination took up to 12 weeks to fully recover. Acute visual changes or sudden onset of ocular pain warrants an immediate return visit for evaluation. 1 Week Post-op Visit UCVA Manifest Refraction with BCVA Slit Lamp Exam Counseling UCVA-generally 20/15 to 20/30 for intralase LASIK, 20/30-20/100 for PRK. Higher myopes who require more overcorrection may be > 20/30. Surface dryness with superficial punctuate keratitis can limit UCVA slightly at this visit. MR and BCVA -the manifest refraction at this visit may help predict the need for enhancement. The refractive error is not yet stable however, particularly in higher myopes and hyperopes. An occasional patient may require temporary distance glasses for situations such as night driving. Presbyopic patients may require temporary or permanent reading glasses. Slit lamp examination- at one-week careful examination to look for evidence of significant striae, epithelial ingrowth, interface inflammation -such as DLK, or infection. Epithelial ingrowth –extremely rare with intralase flaps. More common after enhancements. May be noted in the first 1-2 weeks, but may take up to 4 weeks to present Appearance varies from small pearls of epithelium at the flap edge to a peninsula extending from a flap edge with a whorl pattern. Severe cases can lead to stromal melt. Small non-progressive areas at the edge require no treatment. Progressive cases are treated by the surgeon by lifting the flap and debridement of stromal and flap surface. Anyone with a suspicion of epithelial ingrowth should be referred to the surgeon for evaluation. Diffuse lamellar keratitis –See above on day one discussion. This must be treated immediately and aggressively. Please call Dr. Cullom and have patient follow up immediately. Counseling: Though most patients are extremely happy at the one-week visit, some patients require encouragement at this visit. Patients may need to have reassurance that night vision problems, crispness of vision, and minor eye dryness generally improve substantially over the next several weeks. Presbyopic patients, even when properly counseled before surgery may have difficulty adjusting to new reading glasses. Monovision patients may struggle with an adjustment period as well. Temporary glasses for distance or near may rarely be required, especially for patients doing monovision who have problems with night driving. PRK patients still have a way to go before obtaining their full improved vision. 1 Month Post-operative visit UCVA MR with BCVA Slit lamp exam UCVA and BCVA are generally close to target at the one-month visit, though hyperopes and very high myopes, (especially younger patients) and PRK patients may continue to improve over the next several months. Manifest Refraction: at this visit will give patients a sense of whether enhancement will be required. Slit lamp exam: Flap should be clear, gutter well healed, and there should be no interface inflammation, significant striae, or epithelial ingrowth. As mentioned above, DLK presents within five days of treatment, but may occur later after minor flap trauma. Epithelial ingrowth rarely presents this late. Dry Eyes: Every visit should include careful attention to complaints and slit lamp evidence of corneal dryness. Examine the cornea carefully for evidence of dry eye- decreased breakup time, superficial punctate keratopathy (SPK), and decreased BCVA. Flap formation cuts the superficial corneal nerves and although intralase laser flaps are much thinner at the periphery temporary corneal desensitization occurs. This can last six months or longer in some cases. This results in less blinking and worsening of dry eye symptoms, particularly during concentrated efforts such as computer use or driving. There is also less neural feedback to the lacrimal gland and therefore less reflex tear formation. Patients with significant dry eye signs or symptoms should be started on restasis eye drops twice daily, ideally 2 weeks prior to surgery and continuing this for several months afterwards. I will also place punctal plugs at the first sign of a dry eye problem. Additionally, preservative-free artificial tears such as Bion tears, Theratears or Refresh tears should be used from four times a day to every one-hour. Use an ointment such as Refresh-PM or Genteal gel at night may be need to help relieve severe symptoms particularly in patients who sleep with their eyes slightly open and have worse dryness in the morning. Counsel patients to avoid air vents directed at their eyes while sleeping. Wearing protective sunglasses and/or clear glasses when biking or other outdoor activities helps as well. Counseling: Most patients are doing very well at this visit. Now that the excitement of their new vision is less acute, many patients may have minor problems that need discussion. Problems such as minor eye dryness or the need for new or different reading glasses are generally easily corrected. Enhancements: Customized treatments as well as the use of intralase for all flap formation has greatly reduced our enhancement rate. However, patients still occasionally come in slightly under or overcorrected. If there is significant undercorrection along with dissatisfaction in vision, it may be time to discuss the need for an enhancement. Patients may be 20/40 and very happy with their vision or 20/25 and having a difficult time with their vision. I generally try not to enhance patients before 3 months to allow for stability. Patients with low initial corrections may stabilize sooner and therefore can be treated sooner. The key is to show stability of refraction over several visits. Remember that sometimes patients with slightly myopic outcomes are happy as this may allow for more range of vision up close. Care must be taken not talk a happy patient into a procedure that may trade one problem for another. For example, a 45 year old patient that is -0.50 D and 20/25 at distance states that he is satisfied with his vision. If that patient receives an enhancement he may suddenly need readers and be much less satisfied with his outcome. 3 Month Post-operative Visit UCVA BCVA with manifest refraction Cycloplegic refraction- (if enhancement considered) Slit Lamp Exam Applanation Tonometry UCVA BCVA MR CR: Uncorrected vision is usually (but not always) stable at this point. A cycloplegic refraction will help guide the need for enhancement. Occasionally a patient appearing to have residual myopia is shown by cycloplegic refraction to be emmetropic or minimally myopic. Slit Lamp Exam: The cornea should be well healed without striae, inflammation, and evidence of epithelial ingrowth or dryness Applanation Tonometry: should be considered at this visit Counseling: Problems with night vision, dryness or uncorrected visual acuity are uncommon at this point, but each should be addressed. Enhancements are generally first considered around this period. The flap may be lifted well after the first year of surgery for most patients, therefore enhancements by lifting the flap may be delayed if the patient desires. One limit to enhancement is adequate corneal tissue, therefore patients with borderline corneal thickness, must be counseled appropriately. 6 and 12 Month Visit Generally a repeat of the 3 month visit. Applanation tonometry is optional at this point, but should be done yearly. Perform a dilated funduscopic exam with any complaints of floaters, flashes or decreased vision. CONFIRMATION OF POSTOPERATIVE C0-MANAGEMENT SELECTION BY PATIENT. CATARACT SURGERY PATIENT NAME ___________________________________ (PRINT) My surgeon, R Douglas Cullom, has given me and I have read, the instructions regarding proper eye care following cataract surgery. It is my desire to have my own optometrist, Dr _____________, perform my postoperative follow-up care after my cataract surgery as soon as it is medically appropriate. I have discussed this post-operative selection with my ophthalmologist R. Douglas Cullom M.D. R. Douglas Cullom M.D. has informed me that an optometrist may lawfully provide post-operative care under applicable state law. I understand that my optometrist will contact Dr. Cullom immediately if I experience any complications related to my eye surgery. I understand that I may also contact R. Douglas Cullom M.D. at any time after the surgery. I acknowledge that my optometrist will bill my insurance for my postoperative care and will receive payment from my insurance company for service rendered. I have been advised by the surgeon and my optometrist of the financial details of this arrangement including charges and length of global period. PATIENT SIGNATURE ____________________________ DATE: ________________ WITNESS _______________________________________ DATE:_________________ OPTOMETRIST CONFIRMATION I have agreed to provide follow up care for______________________. I will see the patient after surgery when R Douglas Cullom M.D. notifies me the he is releasing the patient to my care. I agree to notify Dr Cullom immediately should complications arise and to provide written progress reports during my portion of the postoperative period. _____________________________________________ Optometrist Signature DATE:___________________ CONFIRMATION OF POSTOPERATIVE C0-MANAGEMENT SELECTION BY PATIENT. REFRACTIVE SURGERY PATIENT NAME ___________________________________ (PRINT) My surgeon, R Douglas Cullom, has given me and I have read, the instructions regarding proper eye care following refractive surgery. It is my desire to have my own optometrist, Dr _____________, perform my preoperative and postoperative follow-up care relating to my refractive surgery as soon as it is medically appropriate. I have discussed this post-operative selection with my ophthalmologist R. Douglas Cullom M.D. R. Douglas Cullom M.D. has informed me that an optometrist may lawfully provide post-operative care under applicable state law. I understand that my optometrist will contact Dr. Cullom immediately if I experience any complications related to my eye surgery. I understand that I may also contact R. Douglas Cullom M.D. at any time after the surgery. I acknowledge that my surgeon will reimburse my optometrist for pre and postoperative care. I have been advised by the surgeon and my optometrist of the financial details of this arrangement s including charges; postoperative care schedule and enhancement fees. PATIENT SIGNATURE ____________________________ DATE: ________________ WITNESS _______________________________________ DATE:_________________ OPTOMETRIST CONFIRMATION I have agreed to provide follow up care for______________________. I will see the patient after surgery when R Douglas Cullom M.D. notifies me the he is releasing the patient to my care. I agree to notify Dr Cullom immediately should complications arise and to provide written progress reports during my portion of the postoperative period. _____________________________________________ Optometrist Signature DATE:___________________ CONFIRMATION OF POSTOPERATIVE C0-MANAGEMENT SELECTION BY PATIENT. REFRACTIVE LENSECTOMY PATIENT NAME ___________________________________ (PRINT) My surgeon, R Douglas Cullom, has given me and I have read, the instructions regarding proper eye care following refractive lensectomy surgery. It is my desire to have my own optometrist, Dr _____________, perform my preoperative and postoperative follow-up care relating to my refractive lensectomy surgery as soon as it is medically appropriate. I have discussed this post-operative selection with my ophthalmologist R. Douglas Cullom M.D. R. Douglas Cullom M.D. has informed me that an optometrist may lawfully provide post-operative care under applicable state law. I understand that my optometrist will contact Dr. Cullom immediately if I experience any complications related to my eye surgery. I understand that I may also contact R. Douglas Cullom M.D. at any time after the surgery. I acknowledge that my surgeon will reimburse my optometrist for pre and postoperative care. I have been advised by the surgeon and my optometrist of the financial details of this arrangement s including charges; postoperative care schedule and enhancement fees. PATIENT SIGNATURE ____________________________ DATE: ________________ WITNESS _______________________________________ DATE:_________________ OPTOMETRIST CONFIRMATION I have agreed to provide follow up care for ______________________. I will see the patient after surgery when R Douglas Cullom M.D. notifies me the he is releasing the patient to my care. I agree to notify Dr Cullom immediately should complications arise and to provide written progress reports during my portion of the postoperative period. _____________________________________________ Optometrist Signature DATE:___________________ HELPFUL HINTS FOR FILING MEDICARE GLOBAL FEES 1. The date of surgery is the date of service. 2. The global procedure is 66984-55. If the second eye is done in the global period of the first eye, then include a modifier 79. Also in block 24D specify which eye. 3. The diagnosis code is 366.16, it is more specific than 366.9. Be sure to list which eye. 4. File separate claims for each eye. 5. There are 90 days in the global period. In block 19 of the CMS-1500 form write the day your doctor assumed care of the patient. This will be the second day after surgery. After the assumed care date, you put the relinquished care date also in block 19, which would be 90 days after surgery. 6. Do not bill Medicare until you actually see the patient. 7. Your units in 24G should be 89-you can bill for this amount of days per Medicare, as long as the M.D. has turned the patient over to the O.D. 8. The place of service has to be 11 and the type of service has to be 2. 9. Block 17 a & b should be Dr Cullom, his UPIN is G70256 HOW TO CALCULATE THE 54-55 SPLIT 1. Multiply the total charge by 20% 2. Divide that number by 90 to arrive at the daily rate. 3. Multiply that by the number of days your doctor was responsible for post op care Fee for service patients. 20% of collections.