* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Infection Control Practices to Improve Patient Care
Survey
Document related concepts
Traveler's diarrhea wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Gastroenteritis wikipedia , lookup
Common cold wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Schistosomiasis wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis B wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Hepatitis C wikipedia , lookup
Anaerobic infection wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Neonatal infection wikipedia , lookup
Urinary tract infection wikipedia , lookup
Transcript
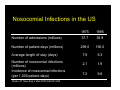
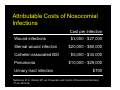
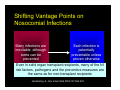
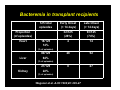
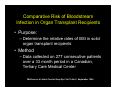
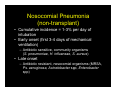
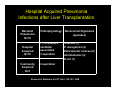
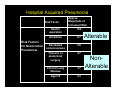
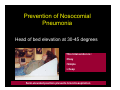
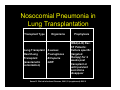
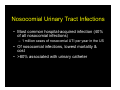
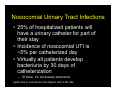
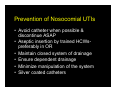
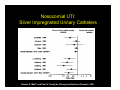
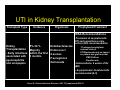
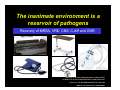
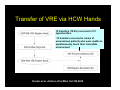
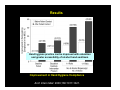
Nosocomial Infections in Solid Organ Transplant Recipients Focus On Prevention Through the Reduction of Alterable Risk Factors Gonzalo Bearman MD, MPH Assistant Professor of Medicine, Epidemiology and Community Health Associate Hospital Epidemiologist Virginia Commonwealth University Outline • Why are nosocomial infections important? • Nosocomial infections in transplants – Data From VCU – Alterable risk factors and preventive measures • BSI • Hospital acquired pneumonia • UTI – Transplant specific antibiotic prophylaxis • Heart/Lung, Renal and Liver transplants – Hand Hygiene • Importance of system level changes involving the measurement and feedback of new technologies and NI process measures that minimize patient risk What this presentation will not cover: • Opportunistic infections! – Fungal, Viral, Parasitic Infections, Prion diseases • Hospital associated or community outbreaks! – Legionella – Aspergillus, etc, etc, etc Nosocomial Infections • 5-10% of patients admitted to acute care hospitals acquire infections – 2 million patients/year – ¼ of nosocomial infections occur in ICUs – 90,000 deaths/year – Attributable annual cost: $4.5 – $5.7 billion • Cost is largely borne by the healthcare facility not 3rd party payors Weinstein RA. Emerg Infect Dis 1998;4:416-420. Jarvis WR. Emerg Infect Dis 2001;7:170-173. Major Sites of Nosocomial Infections • • • • Urinary tract infection Surgical site infection Bloodstream infection Pneumonia (ventilator-associated) Nosocomial Infections • 70% are due to antibiotic-resistant organisms • Invasive devices are more important than underlying diseases in determining susceptibility to nosocomial infection Burke JP. New Engl J Med 2003;348:651-656. Safdar N et al. Current Infect Dis Reports 2001;3:487-495. Nosocomial Infections in the US 1975 1995 Number of admissions (millions) 37.7 35.9 Number of patient days (millions) 299.0 190.0 7.9 5.3 2.1 1.9 7.2 9.8 Average length of stay (days) Number of nosocomial infections (millions) Incidence of nosocomial infections (per 1,000 patient-days) Burke JP. New Engl J Med 2003;348:651-656. Attributable Costs of Nosocomial Infections Cost per Infection Wound infections $3,000 - $27,000 Sternal wound infection $20,000 - $80,000 Catheter-associated BSI $5,000 - $34,000 Pneumonia Urinary tract infection $10,000 - $29,000 $700 Nettleman M. In: Wenzel RP, ed. Prevention and Control of Nosocomial Infections, 4th ed. 2003:36. Shifting Vantage Points on Nosocomial Infections Many infections are inevitable, although some can be prevented Each infection is potentially preventable unless proven otherwise Even in solid organ transplant recipients, many of the NI risk factors, pathogens and the preventive measures are the same as for non-transplant recipients Gerberding JL. Ann Intern Med 2002;137:665-670. Nosocomial BSI in Solid Organ Transplant Recipients Most infections during the first month after transplantation are related to surgical complications. These infections are similar to those occurring in general surgical patients. Snydman, D. Clinical Infectious Diseases, 2001;33 (supplement):S5-S8. Bacteremia in transplant recipients • Prospective analysis of 125 bacteremic episodes in 111 transplant recipients: – Recipients: • 18 heart transplants • 26 Kidney transplants • 80 liver transplants Wagener et al. AJIC 1992;20: 239-47 Bacteremia in transplant recipients 125 total episodes Proportion (of episodes) Heart 18/125 14% Early Onset (< 14 days) Late Onset (> 14 days) 32/125 (26%) 93/125 (74%) 4 14 28 52 0 27 (% of episodes) Liver 80/125 64% (% of episodes) Kidney 27/125 22% (% of episodes) Wagener et al. AJIC 1992;20: 239-47 Bacteremia in transplant recipients Kidney Transplant Liver Transplant Heart Transplant Aerobic Gram Negative Rods (48% of pathogens) 48% of blood cultures: E.coli, Klebesiella, Enterobacteriaciae 49% of blood cultures: P.aeruginosa Enterobacter sps 39% of blood cultures: E.Coli P.aeruginosa Gram Positive Organisms (50% of pathogens) 50 % of blood cultures S.epidermidis S.aureus 50 % of blood cultures S.aureus S.epidermidis 50 % of blood cultures S.epidermidis 0% of blood cultures 6% of Blood cultures: All Candida species 11% of blood cultures: All Candida species 11% of bacteremias 6% in heart transplants Fungi (6% of positive blood cultures) Polymicrobial (10% of positive blood cultures) 7% in Kidney transplants Wagener et al. AJIC 1992;20: 239-47 Bacteremia in transplant recipients Survival Severity of illness Microbilogy Community acquired Nosocomial 19/21 (90%) 78/104 (75%) Lower APACHE II Score Higher APACHE II Score E.coli S.aureus Enterobacteriaciae S.aureus P.aeruginosa Enterobacter sps S.epidermidis Wagener et al. AJIC 1992;20: 239-47 Comparative Risk of Bloodstream Infection in Organ Transplant Recipients • Purpose: – Determine the relative rates of BSI in solid organ transplant recipients • Method – Data collected on 277 consecutive patients over a 33 month period in a Canadian, Tertiary Care Medical Center McClean et al. Infect Control Hosp Epi. Vol 15.No 9, September 1994 Comparative Risk of Bloodstream Infection in Organ Transplant Recipients Transplant Total patients Patients Infected Episodes Liver 50 14 (28%) 20 Kidney 175 9 (5%) 13 Heart or Heart/Lung 50 5 (10%) 7 Total 275 28 (10%) 40 McClean et al. Infect Control Hosp Epi. Vol 15.No 9, September 1994 Comparative Risk of Bloodstream Infection in Organ Transplant Recipients Transplant Primary (CVC) WND PN GI UTI Liver 11 (55%) 4 2 2 1 Kidney 7 (54%) 0 1 1 4 Heart or Heart/Lung 6 (86%) 0 0 1 0 Total 25 (60%) 4 3 4 5 •The majority of BSIs were Primary •The majority of Primary BSIs were attributable to intravascular lines McClean et al. Infect Control Hosp Epi. Vol 15.No 9, September 1994 Comparative Risk of Bloodstream Infection in Organ Transplant Recipients Organism Gram Positive aerobes Liver Kidney Heart Total 13 (62%) 7 (47%) 6 (75%) 26 (59%) 5 (24%) 5 (33%) 2 (25%) 12 (27%) 3 (14%) 3 (20%) 0 6 (13%) 21 15 8 44 S.aureus S.epidermidis Gram negative aerobes E.coli, Klebesiella, Enterobacteriaciae P.aeruginosa Other Candida Bacteriodes Total McClean et al. Infect Control Hosp Epi. Vol 15.No 9, September 1994 Nosocomial Bloodstream Infections, 1995-2002 Rank N= 20,978 Pathogen Percent 1 Coagulase-negative Staph 31.3% 2 S. aureus 20.2% 3 Enterococci 9.4% 4 Candida spp 9.0% 5 E. coli 5.6% 6 Klebsiella spp 4.8% 7 Pseudomonas aeruginosa 4.3% 8 Enterobacter spp 3.9% 9 Serratia spp 1.7% 10 Acinetobacter spp 1.3% Edmond M. SCOPE Project. Preventive Measures for Nosocomial BSI The risk factors interact in a dynamic fashion El Host The CVC is the greatest risk factor for Nosocomial BSI The CVC: Subclavian, Femoral and IJ sites The intensity of the Catheter Manipulation As the host cannot be altered, preventive measures are focused on risk factor modification of catheter use, duration, placement and manipulation Risk Factors for Nosocomial BSIs • Heavy skin colonization at the insertion site • Internal jugular or femoral vein sites • Duration of placement • Contamination of the catheter hub Nosocomial Bloodstream Infections • 12-25% attributable mortality • Risk for bloodstream infection: BSI per 1,000 catheter/days Subclavian or internal jugular CVC 5-7 Hickman/Broviac (cuffed, tunneled) 1 PICC 0.2 - 2.2 Catheter type and expected duration of use should be taken into consideration Prevention of Nosocomial BSIs • Limit duration of use of intravascular catheters – No advantage to changing catheters routinely • Maximal barrier precautions for insertion – Sterile gloves, gown, mask, cap, full-size drape – Moderately strong supporting evidence • Chlorhexidine prep for catheter insertion – Significantly decreases catheter colonization; less clear evidence for BSI – Disadvantages: possibility of skin sensitivity to chlorhexidine, potential for chlorhexidine resistance Putting BSI preventive strategies into practice…. Eliminating catheter-related bloodstream infections in the intensive care unit – Purpose: – To determine whether a multifaceted systems intervention would eliminate catheter-related bloodstream infections (CR-BSIs) – Method: – Prospective cohort study in a surgical intensive care unit (ICU) with a concurrent control ICU. –Patients: – All patients with a central venous catheter in the ICU Pronovost et al. Crit Care Med. 2004 Oct;32(10):2014-20. Eliminating catheter-related bloodstream infections in the intensive care unit Interventions Staff Education Creation of a catheter insertion cart Example •all physicians or physician extenders who insert central catheters were required to complete a Webbased training module and successfully complete a ten-question test before they were allowed to insert a central venous catheter. hand hygiene •central catheter insertion cart that contains the equipment and supplies needed • reduced the number of steps required for compliance Pronovost et al. Crit Care Med. 2004 Oct;32(10):2014-20. Eliminating catheter-related bloodstream infections in the intensive care unit Promotion of daily Catheter Removal Evidence based checklist CVC insertion and for BSI risk reduction Nurses empowered to stop the catheter insertion procedure if a violation of the guidelines occurred •Asked daily during patient rounds whether any catheters or tubes could be removed. •This was added it to the rounding form, called the daily goals form, which is used to develop daily care plans for patients in our SICU •Hand hygiene prior to procedure •chlorhexidine skin preparation •Full-barrier precautions during central venous catheter insertion •Subclavian vein placement as the preferred site, maintaining a sterile field while inserting the catheter •Use of antiseptic impregnated catheter Procedure aborted if they observed a violation in compliance with the evidence-based guidelines. The nurse paged the SICU attending physician if the resident/operator violated the procedure Pronovost et al. Crit Care Med. 2004 Oct;32(10):2014-20. Eliminating catheter-related bloodstream infections in the intensive care unit Pronovost et al. Crit Care Med. 2004 Oct;32(10):2014-20. Eliminating catheter-related bloodstream infections in the intensive care unit • Results: – During the first month nursing completed the checklist for 38 procedures: • eight (24%) for new central venous access, • 30 (79%) for catheter exchanges over a wire, • three (8%) were emergent. – nursing intervention was required in 32% (12/38) of central venous catheter insertions Pronovost et al. Crit Care Med. 2004 Oct;32(10):2014-20. Eliminating catheter-related bloodstream infections in the intensive care unit Study ICU BSI Rate 1st quarter 1998 BSI Rate 4th quarter 2002 January 2003April 2004 11.3/1,000 catheter days 0/1,000 catheter days 0.54/1,000 catheter days No crBSI over 9 month s Control ICU 5.7/1,000 catheter days 1.6/1,000 catheter days Multifaceted, comprehensive program requiring CVC insertion education, with safety checks for proper hand hygiene, aseptic insertion procedure and operator responsibility can result in reduction of nosocomial BSI in an ICU setting. Pronovost et al. Crit Care Med. 2004 Oct;32(10):2014-20. Hospital Acquired Pneumonia in Solid Organ Transplant Recipients Nosocomial Pneumonia (non-transplant) • Cumulative incidence = 1-3% per day of intubation • Early onset (first 3-4 days of mechanical ventilation) – Antibiotic sensitive, community organisms (S. pneumoniae, H. influenzae, S. aureus) • Late onset – Antibiotic resistant, nosocomial organisms (MRSA, Ps. aeruginosa, Acinetobacter spp, Enterobacter spp) Hospital Acquired Pneumonia Infections after Liver Transplantation Bacterial Pneumonia N=15 Hospital Acquired N=10 Community Acquired N=5 Pathophysiology Nosocomial Organisms (episodes) 7 (70%) where ventilator associated 3 aspiration S.aureus (1) P. Aeruginosa (4) Enterobacter cloacae (2) Acinetobacter (2) E.coli (1) 2 aspiration Kusne et al. Medicine, Vol 67, No.2, 132-153. 1988 Hospital Acquired Pneumonia Risk Factor Risk Factors for Nosocomial Pneumonia Approx. Magnitude of Increased Risk Gastric aspiration 10.6 Intubation 6.7 Decreased consciousness 5.8 Thoracic or abdominal surgery 4.7 Chronic Lung Disease 3.7 Age>70 2.3 Alterable NonAlterable Prevention of VAP • Semirecumbent position of ventilated patients (head of bed at 45°) is the most effective measure for decreasing bronchoaspiration Prevention of Nosocomial Pneumonia Head of bed elevation at 30-45 degrees This Intervention is : •Easy •Simple •cheap Semi-elevated position prevents bronchoaspiration Nosocomial Pneumonia in Lung Transplantation Transplant Type Lung Transplant Heart/Lung Transplant (anastamotic colonization) Organisms S.aureus P.aeruginosa B.Cepacia GNR Prophylaxis IDSA(A-III) Rec. CF Patients: Culture specific (targeted therapy) for 2 weeks post transplant or until purulent secretions disappear Soave R. Clinical Infectious Diseases, 2001;33 (supplement):S26-31 Nosocomial UTI Nosocomial Urinary Tract Infections • Most common hospital-acquired infection (40% of all nosocomial infections) – 1 million cases of nosocomial UTI per year in the US • Of nosocomial infections, lowest mortality & cost • >80% associated with urinary catheter Nosocomial Urinary Tract Infections • 25% of hospitalized patients will have a urinary catheter for part of their stay • Incidence of nosocomial UTI is ~5% per catheterized day • Virtually all patients develop bacteriuria by 30 days of catheterization – Of these: 3% will develop bacteremia Safdar N et al. Current Infect Dis Reports 2001;3:487-495. The principal risk factor is duration if urinary catheterization Table 3. Risk factors for catheter-associated urinary tract infection, based on prospective studies and use of multivariable statistical modeling. Factor Relative risk Prolonged catheterization >6 days 5.1-6.8 Female gender 2.5-3.7 Catheter insertion outside operating room 2.0-5.3 Urology service 2.0-4.0 Other active sites of infection 2.3-2.4 Diabetes 2.2-2.3 Malnutrition Azotemia (creatinine >2.0 mg/dL 2.4 2.1-2.6 Ureteral stent 2.5 Monitoring of urine output 2.0 Drainage tube below level of bladder and above collection bag 1.9 Dennis G. Maki* and Paul A. Tambyah, Emerging Infectious Diseases, 2001 Prevention of Nosocomial UTIs • Avoid catheter when possible & discontinue ASAP • Aseptic insertion by trained HCWspreferably in OR • Maintain closed system of drainage • Ensure dependent drainage • Minimize manipulation of the system • Silver coated catheters Nosocomial UTI: Silver Impregnated Urinary Catheters Nosocomial UTI: Silver Impregnated Urinary Catheters Dennis G. Maki* and Paul A. Tambyah, Emerging Infectious Diseases, 2001 Nosocomial Urinary Tract Infections: Silver Alloy Catheters • Advantages: – Most studies have demonstrated a significant decrease in incidence of UTI – Insertion, care no different than for 1st generation catheter • Disadvantage: – Cost • Supporting evidence: reasonably strong (high strength of evidence for impact & effectiveness at low cost & complexity) • Primary goal should still remain avoiding the use of catheters when possible & discontinuing as soon as possible UTI in Kidney Transplantation Transplant Type Incidence Organisms Prophylaxis/Treatment IDSA-Recommendations Kidney Transplantation - Early infections associated with pyelonephritis and urospepsis 5%-36 % Majority within the first 3 months Enterbacteriaciae Enterococci S.aureus P.aeruginosa Salmonella •Treatment of asymptomatic UTI and surveillance urine culture (BII) recommendation –Prolonged prophylaxis reduces rates of UTI/Bacteremia but no impact on patient and graft survival •TMP/Sulfa or Ciprofloxacin •Salmonelluria- 6 weeks of Rx (BII) • Asymptomatic Candiduria Rx recommended (A-II) Soave R. Clinical Infectious Diseases, 2001;33 (supplement):S26-31 Special Concerns: Liver Transplantation Transplant Type Liver Transplantation Infections •Intrahepatic and extrahepatic abscesses •Cholangitis •Peritonitis •SSI •BSI Organisms Prophylaxis/treatment Selective Bowel Decontamination (SBD) •Non-absorbable/topical antibiotics Enterbacteriaciae Enterococci –Decreased bacterial VRE infections in 2 randomized, S.aureus controlled trials OLT recipients Anaerobes •Antibiotic prophylaxis Candida warranted before/after each post transplant cholangiogram , liver biopsy (IDSA A1) Badger et al, Transplant Proceedings. 1991;23:1460-1 Smith SD et al, Transplantation. 1993;55:1306-9 30%-40% of all Nosocomial Infections are Attributed to Cross Transmission The inanimate environment is a reservoir of pathogens X represents a positive Enterococcus culture The pathogens are ubiquitous ~ Contaminated surfaces increase cross-transmission ~ Abstract: The Risk of Hand and Glove Contamination after Contact with a VRE (+) Patient Environment. Hayden M, ICAAC, 2001, Chicago, IL. The inanimate environment is a reservoir of pathogens Recovery of MRSA, VRE, C.diff CNS and GNR Devine et al. Journal of Hospital Infection. 2001;43;72-75 Lemmen et al Journal of Hospital Infection. 2004; 56:191-197 Trick et al. Arch Phy Med Rehabil Vol 83, July 2002 Walther et al. Biol Review, 2004:849-869 The inanimate environment is a reservoir of pathogens Recovery of MRSA, VRE, CNS. C.diff and GNR Devine et al. Journal of Hospital Infection. 2001;43;72-75 Lemmen et al Journal of Hospital Infection. 2004; 56:191-197 Trick et al. Arch Phy Med Rehabil Vol 83, July 2002 Walther et al. Biol Review, 2004:849-869 The inanimate environment is a reservoir of pathogens Recovery of MRSA, VRE, CNS. C.diff and GNR Devine et al. Journal of Hospital Infection. 2001;43;72-75 Lemmen et al Journal of Hospital Infection. 2004; 56:191-197 Trick et al. Arch Phy Med Rehabil Vol 83, July 2002 Walther et al. Biol Review, 2004:849-869 Transfer of VRE via HCW Hands 16 transfers (10.6%) occurred in 151 opportunities. •13 transfers occurred in rooms of unconscious patients who were unable to spontaneously touch their immediate environment Duckro et al. Archive of Int Med. Vol.165,2005 Alcohol based hand hygiene Easy to use Quick solutions Very effective antisepsis due to bactericidal properties of alcohol Impact of alcohol based hand sanitizers at VCU: can this improve hand hygiene? Study Algorithm Incremental Increase in Alcohol Dispensers Hand Hygiene Educational Program Implemented Direct Observation of Hand Hygiene Arch Intern Med. 2000;160:1017-1021. Results Hand hygiene practice can be improved with education and greater accessibility of alcohol hand sanitizers •Improvement in Hand Hygiene Compliance Arch Intern Med. 2000;160:1017-1021. Hand Hygiene • Single most important method to limit cross transmission of nosocomial pathogens • Multiple opportunities exist for HCW hand contamination – Direct patient care – Inanimate environment • Alcohol based hand sanitizers are ubiquitous – USE THEM BEFORE AND AFTER PATIENT CARE ACTIVITIES How are we improving compliance with IC recommendations for your patients in the ICU? Measurement and feedback of infection control process measures in the intensive care unit: impact on compliance. Mezgebe Berhe MD1, Mike Edmond MD, MHA, MPH1,2, Gonzalo Bearman MD, MPH1,2 Divisions of Infectious Diseases1 and Quality Health Care2 Department of Internal Medicine Virginia Commonwealth University School of Medicine Richmond, VA, USA Conferencia anual de SHEA, Los Angeles, California Measurement and feedback of infection control process measures in the intensive care unit: impact on compliance. - • To measure selected infection control process measures • To feedback the results of process indicator measurement to ICU leadership • To assess the impact of feedback on compliance with infection control process measures Mezgebe Berhe MD1, Mike Edmond MD, MHA, MPH1,2, Gonzalo Bearman MD, MPH1,2 Measurement and feedback of infection control process measures in the intensive care unit: impact on compliance. • Selected Infection Control Process Measures: – Hand Hygiene – Femoral Catheter use as proportion of CVC days – Proportion of Head of bed (HOB) elevations in medical (MRICU) and Surgical (STICU) Intensive Care Units • All Data Collected by ICPs – Baseline data- April-June 2004 – Follow up- 3rd, 4th quarters of 2004, 1st quarter 2005 – Baseline and follow up data presented to ICU nurses and Physician staff • Differences in proportions analyzed for significance by Chi-Square Method Mezgebe Berhe MD1, Mike Edmond MD, MHA, MPH1,2, Gonzalo Bearman MD, MPH1,2 Measurement and feedback of infection control process measures in the intensive care unit: impact on compliance. MRICU STICU Baseli ne Q22004 Q3 (2004 Q4 (2004) Q1 (2005) P value* Process Measure Baseline Q2-2004 Q3 (2004) Q4 (2004) Q1 (2005) P value* HH % Opp 14/44 (32%) 31/91 (37%) 33/91 (36%) 50/108 (46%) 0.101 19/38 (50%) 42/80 (53%) 40/80 (50%) 49/100 (49%) 0.916 HOB % Opp 28/51 (55%) 320/333 (96%) 450/45 4 (99%) 551/556 <0.001 20/43 (47%) 229/30 7 (75%) 389/48 8 (79%) 275/36 1 (76%) <0.001 Fem. CVC % of Days 195/1093 (18%) 130/769 (16%) 80/879 (9.1%) 51/951 (5.4% <0.001 93/110 9 (8.4%) 49/970 (5.1%) 14/107 7 (1.3%) 26/920 (2.8%) 0.01 (99%) Mezgebe Berhe MD1, Mike Edmond MD, MHA, MPH1,2, Gonzalo Bearman MD, MPH1,2 Measurement and feedback of infection control process measures in the intensive care unit: impact on compliance. • Feedback of process measures: • lowered the use of femoral catheters • Improved the proportion of elevated HOBs in both ICUs • There was no significant improvement in hand hygiene. • System level changes such as catheter placement and HOB elevation appears to be impacted by feedback whereas individual level practices such as hand hygiene were not affected Mezgebe Berhe MD1, Mike Edmond MD, MHA, MPH1,2, Gonzalo Bearman MD, MPH1,2 Conclusion • Much like other critically ill patients, solid organ transplant recipients are prone to nosocomial infections. • Even in solid organ transplant recipients, the NI risk factors, pathogens and the preventive measures are the same as for non-transplant recipients • The major nosocomial infections are: – BSI – Hospital acquired pneumonia – Hospital acquired UTI • The principal NI pathogens are bacterial and represent colonizing or nosocomial pathogens – – – – S.aureus Enterococci- VRE Enterobacteriaciae P.aeruginosa Conclusion • Risk reduction strategies are well defined in the literature – Lack of adherence to IC measures is recognized as important in the pathogenesis of NIs • System level changes involving the measurement and feedback of adherence to IC measures are needed to implement risk reduction strategies consistently – BSI: comprehensive catheter use/care – VAP: HOB elevation – UTI: catheter insertion, care and silver impregnated catheters – Hand Hygiene- alcohol based sanitizers • Selective antibiotic prophylaxis may be warranted in certain cases involving: • Lung transplants, Liver Transplants, Kidney Transplants