* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download a study of the variation of the popliteal artery branching pattern
Survey
Document related concepts
Transcript
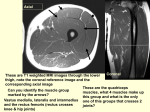
A STUDY OF THE VARIATION OF THE POPLITEAL ARTERY BRANCHING PATTERN AMONG MALE MEDICAL UNDERGRADUATE STUDENTS IN IIUM KUANTAN BY AHMAD RUZAIN SALEHUDDIN A dissertation submitted in fulfilment of the requirement for the degree of Master of Medical Sciences Kulliyyah of Medicine International Islamic University Malaysia JUNE 2016 ABSTRACT A wide range of variations can be seen in the vascular system of an adult human lower limb. One of the important blood vessels that has been mentioned in the literature is popliteal artery. Popliteal artery injury is frequently associated with lower limb trauma or surgical procedures involving the knee joint and popliteal fossa. Therefore, knowledge regarding the branching patterns of popliteal artery is essential because any damage to its branches can be life- or limb-threatening. This study aimed to measure the prevalence of popliteal artery variations in healthy subjects. Furthermore, we would also like to determine the symmetrical characteristic of variations in the same individual, and the correlation between luminal diameter of popliteal artery and specific parameters. This is the first study done in Malaysia on popliteal artery variations in vivo using colour Doppler ultrasonography. One hundred and fifty four lower limbs (77 subjects of male medical undergraduate students of International Islamic University Malaysia) were examined during this study. The area of interest was the popliteal fossa. Among them, 4.5% (seven cases) were found to possess variants. The two variants encountered in this study were Type I-B or trifurcation of popliteal artery 1.9% (three cases), and Type II-A or high-origin anterior tibial artery 2.6% (four cases). With regard to the variants of popliteal artery branching pattern, two subjects had Type II-A occurred bilaterally while three other subjects had unilateral characteristic of Type I-B in combination with Type I-A. It was found that luminal diameter of popliteal artery increased with body surface area and calf circumference in both dominant and non-dominant legs respectively (p<0.001). In conclusion, popliteal artery showed variations in branching pattern, and its diameter increases with body surface area and calf circumference. ii خالصة البحث هناك جمموعة واسعة من االختالفات ميكن أن ينظر إليها يف األوعية الدموية من االطراف السفلى لالنسان البالغ .واحدة من األوعية الدموية اهلامة اليت مت ذكرها يف األدب هو الشراين املأبضي .وكثريا ما يرتبط إصابة الشراين املأبضي مع إصاابت األطراف السفلى أو العمليات اجلراحية اليت تتضمن مفاصل الركبة واملبأبضية .ولذلك،فان أمناط معرفه تفرع الشراين املأبضي ضروري ألن أي ضرر يف فروعها ميكن أن يكون هتديدا حلياة االنسان أو هتديدا ألطرافة .هدفت هذه الدراسة إىل قياس مدى انتشار إختالفات الشرايني املأبضية يف االشخاص األصحاء .وعالوة على ذلك ،نود أيضا لتحديد اخلصائص املتناررة من االختالفات يف نف الفرد والعالقة بني قطر الشراين املأبضي مع معايري حمددة .هذه هي الدراسة األوىل من نوعها اليت أجريت يف ماليزاي على إختالفات الشرايني املأبضية يف اجلسم احلي ابستخدام دوبلر املوجات فوق الصوتية امللونة ) .(colour Doppler ultrasonographyمت فحص مائة وأربعة ومخسون طرف سفلى ( 77شخص ابلغ ذكر من طالب البكالوريوس يف كليه الطب ابجلامعة اسإسالمية العاملية مباليزاي) خالل هذه الدراسة .كانت املنطقة ذات االهتمام هي املأبضية .من بينهم ،مت العثور على 7 ( ٪4.5حاالت) من األطراف السفلية وجدهبا إختالفات .وكان اخليارين اليت مت مواجهتها يف هذه الدراسة هو النوع االول-ب أو كما يطلق عليها االنفراق الثالثي من الشراين املأبضي ( ٪1.9ثالث حاالت) ،والنوع الثاين-أ أو كما يطلق عليها ارتفاع نقطة تفرع الشراين عظام الساق األمامية (( ٪2.6 )high-origin anterior tibial arteryأربع حاالت) .وفيما يتعلق ابالختالفات يف طرق تفرع الشراين املأبضي ،كان شخصني من النوع الثاين-أ حيملوهنا يف كال الطرفيني السفليني ,بينما وجد يف ثالثة أشخاص أخرين يف طرف واحد النوع االول-ب مع النوع االول-أ .وقد تبني أن قطر الشراين املأبضي يزداد مع مساحة سطح اجلسم ومنتصف الساق يف كال الساقني ( .)p<0.001ويف اخلتام ،أرهر الشراين املأبضي اختالفات يف منط التفرعات ،ويزيد قطرها مع حميط الساق ومساحة سطح اجلسم. ABSTRACT IN ARABIC iii APPROVAL PAGE I certify that I have supervised and read this study and that in my opinion, it conforms to acceptable standards of scholarly presentation and is fully adequate, in scope and quality, as a dissertation for the degree of Master of Medical Sciences. ………………………………….. Zunariah Buyong Supervisor ………………………………….. Siti Kamariah Che Mohamed Co-Supervisor ………………………………….. Radhiana Hassan Co-Supervisor I certify that I have read this study and that in my opinion it conforms to acceptable standards of scholarly presentation and is fully adequate, in scope and quality, as a dissertation for the degree of Master of Medical Sciences. ………………………………….. Emad Mohamed Nafie AbdelWahab Internal Examiner This dissertation was submitted to the Department of Basic Medical Sciences and is accepted as a fulfilment of the requirement for the degree of Master of Medical Sciences. ………………………………….. Zunariah Buyong Head, Department of Basic Medical Sciences This dissertation was submitted to the Kulliyyah of Medicine and is accepted as a fulfilment of the requirement for the degree of Master of Medical Sciences. ………………………………….. Azmi Md. Nor Dean, Kulliyyah of Medicine iv DECLARATION I hereby declare that this dissertation is the result of my own investigations, except where otherwise stated. I also declare that it has not been previously or concurrently submitted as a whole for any other degrees at IIUM or other institutions. Ahmad Ruzain Salehuddin Signature ........................................................... v Date ......................................... COPYRIGHT PAGE INTERNATIONAL ISLAMIC UNIVERSITY MALAYSIA DECLARATION OF COPYRIGHT AND AFFIRMATION OF FAIR USE OF UNPUBLISHED RESEARCH A STUDY OF THE VARIATON OF THE POPLITEAL ARTERY BRANCHING PATTERN AMONG MALE MEDICAL UNDERGRADUATE STUDENTS IN IIUM KUANTAN I declare that the copyright holders of this dissertation are jointly owned by the student and IIUM. Copyright © 2016 Ahmad Ruzain Salehuddin and International Islamic University Malaysia. All rights reserved. No part of this unpublished research may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without prior written permission of the copyright holder except as provided below 1. Any material contained in or derived from this unpublished research may only be used by others in their writing with due acknowledgement. 2. IIUM or its library will have the right to make and transmit copies (print or electronic) for institutional and academic purpose. 3. The IIUM library will have the right to make, store in a retrieval system and supply copies of this unpublished research if requested by other universities and research libraries. By signing this form, I acknowledged that I have read and understand the IIUM Intellectual Property Right and Commercialization policy. Affirmed by Ahmad Ruzain Salehuddin ….……………………………. Signature ……..……………….. Date vi ACKNOWLEDGEMENTS Alhamdulillah, all praises to ALLAH, The Sustainer and Provider for all universe, Who has given me good health, strength and enough time for me to finish this study and guided me in my life as a Muslim. May all the blessings and peace be upon our beloved Prophet Muhammad, his family and companions. First and foremost, I would like to take this opportunity to express my sincere gratitude and appreciation to my supervisor, Asst. Prof. Dr. Zunariah Buyong for her continuous support and patience during my study. I would also like to thank my cosupervisors, Assoc. Prof. Dr. Siti Kamariah Che Mohamed and Assoc. Prof. Dr. Radhiana Hassan for their advices and encouragements. I am also grateful to acknowledge the unreserved help and assistance offered by several individuals: Dr. Ye Tun, Dr. Yi Yi Myint, Assoc. Prof. Dr. Jamalludin Ab. Rahman, Dr. Nurul Asyiqin Yusof, Dr. Che Anuar Che Mohamad and Bander S. Ali Binjaabaan Al-Qahtani. I wish to express my appreciation and thanks to the Postgraduate Office of Kulliyyah of Medicine, IIUM including Assoc. Prof. Dr. Kamarul Ariffin Khalid (Deputy Dean Postgraduate and Research) and his supporting staffs; IIUM Research Ethics Committee and Research Management Centre for their continuous support and advice during this study. Thank you also to the Director of IIUM Breast Centre for the permission to use the facilities and the supporting staffs for their technical support. Special thanks also forwarded to Madeleine Eng Jiun Yi (Clinical Application Specialist US Ultrasound from Healthcare Sector of Siemens Malaysia Sdn. Bhd.) for the intensive workshop and calibration of the ultrasound machine used in this study. Finally, a million thanks to the medical undergraduate students who participated in this study for without them none of this would have been possible. It is my utmost pleasure to dedicate this work to my dear parents, Rozana Mudzir and Salehuddin Shamsuddin, thank you is not enough for all the sacrifices you both made to ensure that I achieve success in my life. Not forgetting my dearly wife, Zahrah Humaira Hii, for your unfailing love and support especially when I needed it the most. My lovely daughter, Nur Sofiya Mardhiyah, you are the pride and joy of my life. All my brothers, Ahmad Dzulkarnain, Ahmad Shamsuddin and Ahmad Suleiman for always supporting me through good and bad times. All my dearest friend, Ahmed Nuri, Raed and Raihana; for their advice, support and happy moment together during this postgraduate study. Last but not least, I dedicate this work to my colleagues and future students in the field of anatomy. vii TABLE OF CONTENTS Abstract .................................................................................................................... …..ii Abstract in Arabic .................................................................................................... ….iii Approval Page .......................................................................................................... ….iv Declaration ............................................................................................................... …..v Copyright Page ......................................................................................................... ….vi Acknowledgements .................................................................................................. …vii List of Tables ........................................................................................................... …..x List of Figures .......................................................................................................... ….xi List of Abbreviations...................................................................................................xiv CHAPTER ONE: INTRODUCTION .................................................................. …..1 1.1 Background ............................................................................................. …..1 1.1.1 Normal Anatomy of Lower Limb Arterial System ..................... …..2 1.1.1.1 Femoral Artery .................................................................. …..2 1.1.1.2 Popliteal Artery ................................................................. …..4 1.1.1.3 Anterior Tibial Artery........................................................ …..8 1.1.1.4 Posterior Tibial Artery ....................................................... …..9 1.1.1.5 Peroneal Artery .................................................................. …10 1.1.2 Embryology of Vascular System in Lower Limb ........................ …11 1.1.3 Physics of Ultrasound in Determining the Anatomy of Lower Limb Arterial System ....................................................... …13 1.1.3.1 Ultrasound Instrumentation ............................................... …14 1.1.3.1.1 Real-time Ultrasound Units .................................... …14 1.1.3.1.2 Doppler Instruments ............................................... …17 1.1.3.2 Sonographic Findings of Lower Limb Arteries ................. …19 1.1.3.2.1 Gray-scale Image Characteristics of a Normal Artery ........................................................ …19 1.1.3.2.2 Doppler Colour Flow Image Characteristics of a Normal Artery ................................................. …20 1.1.3.2.3 Doppler Spectral Waveform Image Characteristics of a Normal Artery ........................ …20 1.2 Justification ............................................................................................. …20 1.3 General Objective ................................................................................... …21 1.4 Specific Objectives ................................................................................. …21 CHAPTER TWO: LITERATURE REVIEW 2.1 Embryological Justification of Arterial Variations in Adult Lower Limb 2.2 Classification of Lower Limb Arterial Variations in Popliteal Region 2.2.1 Popliteal Artery Branching Pattern (Type I) 2.2.2 Popliteal Artery Branching Pattern (Type II) 2.2.3 Popliteal Artery Branching Pattern (Type III) 2.3 Clinical Significance of High-origin Anterior Tibial Artery and Trifurcation of Popliteal Artery viii 22 22 24 25 29 32 35 2.4 Other Studies Regarding Popliteal Artery 2.5 Concept of Lower Limb Dominance (Leg Dominance) 38 41 CHAPTER THREE: METHODOLOGY 3.1 Study Design 3.2 Population 3.3 Subjects 3.3.1 Inclusion Criteria 3.3.2 Exclusion Criteria 3.3.3 Subjects Recruitment Work Flow 3.3.4 Anthropometric Measurements 3.3.5 Ultrasound Examination Protocol of Lower Limb Arterial System in Popliteal Region 3.4 Statistical Analysis 42 42 42 43 43 43 43 44 CHAPTER FOUR: RESULTS 4.1 Baseline Subjects Background 4.2 Descriptive Analysis of Popliteal Artery Branching Patterns 4.2.1 Type I-A (Usual Pattern) 4.2.2 Type I-B (Variant 1) 4.2.3 Type II-A (Variant 2) 4.3 Statistical Analysis of Popliteal Artery Branching Patterns 4.3.1 Percentage of Popliteal Artery Branching Patterns 4.3.2 Percentage of Popliteal Artery Branching Patterns In Relation with Leg Dominance 4.3.3 Percentage of Subjects Having the Same (Symmetrical) or Different (Non-symmetrical) Popliteal Artery Variants in Both Lower Limbs 4.3.4 Luminal Diameter of Popliteal Artery and Anterior Tibial Artery 4.3.5 Luminal Diameter of Other Arteries (Tibial-peroneal Trunk, Posterior Tibial Artery and Peroneal Artery) 4.3.6 Correlation between Luminal Diameter of Popliteal Artery and Body Surface Area, Calf Circumference in Dominant and Non-dominant Legs 53 53 54 54 58 62 66 66 CHAPTER FIVE: DISCUSSION 5.1 Overall Prevalence of Popliteal Artery Variations 5.2 Recommendations and Conclusion 73 73 75 REFERENCES 76 APPENDIX A: ETHICAL APPROVAL (IREC) APPENDIX B: INFORMED CONSENT FORM (ENGLISH AND MALAY) APPENDIX C: INFORMATION SHEET (ENGLISH AND MALAY) APPENDIX D: LIST OF PRESENTATION 80 82 84 86 ix 46 52 66 67 68 68 69 LIST OF TABLES Table 2.1 Normal level of division of popliteal artery (below the tibial plateau) 26 Table 2.2 High division of popliteal artery (above the tibial plateau) 30 Table 2.3 Hypoplastic-aplastic infrapopliteal vessels with altered arterial supply to the foot 33 Frequency of popliteal arterial variations among different studies 41 Table 4.1 Baseline parameters of 77 subjects recruited in this study 53 Table 4.2 Popliteal artery branching patterns in 154 lower limbs 66 Table 4.3 Popliteal artery branching patterns in dominant and nondominant legs 67 Unilateral and bilateral occurrence of popliteal artery variants in 77 subjects 67 Mean, standard deviation for luminal diameter of popliteal artery and anterior tibial artery 68 Frequency of tibial-peroneal trunk, posterior tibial artery and peroneal artery in 77 subjects 68 Mean, standard deviation for luminal diameter of tibialperoneal trunk, posterior tibial artery and peroneal artery 69 Table 2.4 Table 4.4 Table 4.5 Table 4.6 Table 4.7 x LIST OF FIGURES Figure 1.1 Left thigh region showing femoral artery common stem from where profunda femoris artery and medial circumflex femoral artery arise 3 Right thigh region showing femoral artery and its branches in the femoral triangle 3 Dissection of right popliteal region showing adductor hiatus where femoral artery continues downward as popliteal artery and femoral vein becomes popliteal vein after passing through the hiatus 5 Figure 1.4 Structures in the right popliteal fossa (popliteal vein omitted) 6 Figure 1.5 Dissection of right popliteal region showing the bifurcation of popliteal artery 7 Course of the popliteal artery genicular branches in right popliteal region 8 Dissection of right popliteal region showing the origin and course of posterior tibial artery and peroneal artery 10 Figure 1.8 Development of the arterial system in the lower limb 13 Figure 1.9 Various types of ultrasound transducer 16 Figure 1.2 Figure 1.3 Figure 1.6 Figure 1.7 Figure 1.10 Two basic real-time scanning formats for cross-sectional imaging 16 Figure 1.11 Image of A-mode and M-mode with real-time sector B scanning 17 Figure 1.12 Triphasic spectrum at rest 18 Figure 1.13 Bifurcation of a normal brachial artery (red) with parallel running vein (blue) in colour duplex sonography 19 Figure 2.1 Embryologic development of arteries to leg 23 Figure 2.2 Arterial supply to the left lower limb 24 Figure 2.3 Normal level of popliteal arterial branching 26 Figure 2.4 Normal termination of popliteal artery in the right lower limb 27 Figure 2.5 Normal branching pattern of popliteal artery 27 xi Figure 2.6 Trifurcation of popliteal artery in the right lower limb 28 Figure 2.7 Trifurcation of popliteal artery 28 Figure 2.8 Dissection of both popliteal regions in the same cadaver showing high-origin anterior tibial artery proximal to the upper border of popliteus muscle 29 Embryological pattern of arteries near the knee shows that 30 Figure 2.9 Figure 2.10 High division of popliteal artery 31 Figure 2.11 High-origin anterior tibial artery 31 Figure 2.12 High-origin posterior tibial artery 32 Figure 2.13 Hypoplastic or aplastic branching with altered distal supply 33 Figure 2.14 Aplastic posterior tibial artery 34 Figure 2.15 Hypoplastic anterior tibial artery 34 Figure 2.16 Hypoplastic or aplastic posterior tibial artery and anterior tibial artery 35 Figure 2.17 Example of a high-origin anterior tibial artery 37 Figure 2.18 Levels of osteotomy for 37 Figure 2.19 Diagram shows the posterior view of the new patterns 40 Figure 3.1 Measuring tape was used to record the calf circumference 45 Figure 3.2 Colour doppler ultrasound machine used in this study 49 Figure 3.3 Surface marking of the popliteal fossa on the right lower limb 49 Figure 3.4 Sagittal scan from a posterior approach 50 Figure 3.5 Transverse scan from a posterior approach 50 Figure 3.6 Landmark for each peripheral pulses of the right lower limb 51 Figure 3.7 Flowchart for measurement of arteries luminal diameter at the level of popliteus muscle 51 Figure 3.8 Luminal diameter measurements in bifurcation of popliteal artery 52 Figure 3.9 Luminal diameter measurements in trifurcation of popliteal artery 52 xii Figure 4.1 Type I-A, branching pattern of the right popliteal artery in sagittal view 55 Figure 4.2 Popliteal artery and its branches in transverse view 56 Figure 4.3 Sagittal view of Type I-A, branching pattern of the right popliteal artery 57 Doppler spectral waveform image and schematic diagram of the right popliteal artery 58 Type I-B, branching pattern of the right popliteal artery in sagittal view 59 Sagittal view of Type I-B, branching pattern of the right popliteal artery 60 Doppler spectral waveform image and schematic diagram of the right 61 Type II-A, branching pattern of the left popliteal artery in sagittal view 63 Sagittal view of Type II-A, branching pattern of the left popliteal artery 64 Figure 4.4 Figure 4.5 Figure 4.6 Figure 4.7 Figure 4.8 Figure 4.9 Figure 4.10 Doppler spectral waveform image and schematic diagram of the left 65 Figure 4.11 Luminal diameter of popliteal artery in relation to body surface area in dominant and non-dominant legs 70 Figure 4.12 Luminal diameter of popliteal artery in relation to calf circumference in dominant legs 71 Figure 4.13 Luminal diameter of popliteal artery in relation to calf circumference in non-dominant legs 72 xiii LIST OF ABBREVIATIONS ASIS Anterior superior iliac spine ATA Anterior tibial artery BSA Body surface area CTA Computed tomography angiography DPA Dorsalis pedis artery DSA Digital subtraction angiography FA Femoral artery IIUM International Islamic University Malaysia IREC IIUM Research Ethics Committee LEA Lower extremity artery MDCT Multidetector computed tomography PA Popliteal artery PAES Popliteal artery entrapment syndrome PM Popliteus muscle PRA Peroneal artery PTA Posterior tibial artery PV Popliteal vein SPSS Statistical Packaged for the Social Sciences SS Sample size TKA Total knee arthroplasty TPT Tibial-peroneal trunk xiv CHAPTER ONE INTRODUCTION 1.1 BACKGROUND A wide range of anatomical variations can be seen in the vascular system of adult human lower limb. The knowledge of these variations which is determined by embryonic vascular development is rather interesting not only for radiologists, but also for surgeons who are responsible to plan the correct management (Ozgur, Ucerler & Ikiz, 2009; Lappas, Stavropoulos, Noussios, Sakellariou & Skandalakis, 2012). Vascular injury is frequently associated with lower limb trauma involving the knee joint and popliteal fossa (Cross, Hall, Howdieshell, Colborn & Gale, 2000). In the management of peripheral vascular disease and in surgery involving the knee joint, it is important to know the course and termination of popliteal artery (PA). Knowledge regarding the branching patterns of popliteal artery is essential because any damage to its branches can be life- or limb-threatening (Tindall, Shetty, James, Middleton & Fernando, 2006). According to literature review, the earliest study pertaining to popliteal artery variations was done by Quain and Maclise in 1844. This study was observed in Europeans. The incidence of popliteal artery variations among American Whites and Negroes was studied by Trotter in 1940. In 1989, Kim, Orron and Skillman introduced a revised classification of popliteal artery branching patterns based on previous study done by Lippert and Pabst (1985). The importance of popliteal artery branching patterns in surgery had been previously evaluated by different techniques such as cadaveric method, angiographic 1 studies and Doppler ultrasonography. Those reports were studied in many other countries, but not in Malaysia. Therefore, this study is aimed to evaluate the popliteal artery branching patterns and related measurements using Doppler ultrasonography in healthy subjects. It is hoped that this study will be beneficial and add up to the existing knowledge of vascular anatomy of lower limb. 1.1.1 Normal Anatomy of Lower Limb Arterial System 1.1.1.1 Femoral Artery Femoral artery (FA) is the chief artery which provides the main arterial supply to the lower limb (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). Femoral artery which is the continuation of external iliac artery, begins deep to inguinal ligament, midway between anterior superior iliac spine (ASIS) and pubic symphysis, descends on the adjacent borders of iliopsoas and pectineus forming the floor of femoral triangle, passes deep to sartorius and enters through the adductor (subsartorial) canal, then exits through an opening in adductor magnus (adductor hiatus) near the junction of middle and distal thirds of the thigh before entering the popliteal fossa as popliteal artery (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). In the femoral triangle, femoral artery gives off three superficial and three deep branches (Figure 1.1 and Figure 1.2). Superficial branches are superficial epigastric artery which supplies the skin and fasciae at the lower part of anterior abdominal wall; superficial circumflex iliac artery which supplies the skin along iliac crest; and superficial external pudendal artery which supplies the skin of external genital organs. Deep branches are profunda femoris, the chief artery which supplies all 2 the three compartments of the thigh (anterior, medial & posterior); deep external pudendal artery which supplies the external genital organs; and muscular branches which supply the sartorius, vastus medialis and adductors (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). Figure 1.1 Left thigh region showing femoral artery common stem from where profunda femoris artery and medial circumflex femoral artery arise (Modified from Suthar, Patil, Mehta, Patel, Prajapati & Bhatt, 2013). SUPERFICIAL EPIGASTRIC ARTERY SUPERFICIAL CIRCUMFLEX ILIAC ARTERY FEMORAL ARTERY PROFUNDA FEMORIS ARTERY Figure 1.2 Right thigh region showing femoral artery and its branches in the femoral triangle (Modified from Pradip, Alpa, Monika, Ashish, Ankit & Suresh, 2015). 3 1.1.1.2 Popliteal Artery Popliteal artery, which is the continuation of femoral artery, enters the popliteal fossa through an opening (adductor hiatus) in adductor magnus (Figure 1.3). Popliteal artery is the deepest structure in the popliteal fossa and runs close to the articular capsule of the knee joint. It ends by dividing into anterior tibial artery (ATA) and posterior tibial artery (PTA) at the level of inferior border of popliteus muscle (PM) (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). In popliteal artery surgery, radiologists and surgeons prefer to use another description of popliteal artery and its main branches where anterior tibial artery arising first followed by tibial-peroneal trunk (TPT), which then gives rise to the posterior tibial artery and the peroneal artery (PRA) (Day & Orme, 2006) (Figure 1.4 and Figure 1.5). Popliteal artery has genicular and muscular branches. Articular capsule and ligaments of the knee joint are supplied by five genicular branches of popliteal artery namely the lateral superior, medial superior, middle, lateral inferior and medial inferior genicular arteries (Figure 1.6). They participate in the formation of network of vessels around the knee joint which is called the genicular anastomosis (Moore & Dalley, 1999; Standring, 2004; Chaurasia, 2013; Nafis, 2013). Muscular branches of popliteal artery can be divided into superior muscular and inferior muscular or sural branches. Superior muscular branches supply the adductor magnus and hamstrings, and have clinically important anastomoses with the terminal part of deep femoral and gluteal arteries. Gastrocnemius, soleus and plantaris are supplied by the inferior muscular or sural branches (Moore & Dalley, 1999; Standring, 2004; Chaurasia, 2013). 4 Figure 1.3 Dissection of right popliteal region showing adductor hiatus where femoral artery continues downward as popliteal artery and femoral vein becomes popliteal vein after passing through the hiatus. 5 Figure 1.4 Structures in the right popliteal fossa (popliteal vein omitted) (O’Rahilly, Muller, Carpenter & Swenson, 1982). 6 Figure 1.5 Dissection of right popliteal region showing the bifurcation of popliteal artery. 7 Tibia Fibula Figure 1.6 Course of the popliteal artery genicular branches in right popliteal region (Modified from Chaurasia, 2013). 1.1.1.3 Anterior Tibial Artery The smaller terminal branch of popliteal artery which is anterior tibial artery, begins at the inferior border of popliteus muscle. It passes anteriorly through a gap in the superior part of interosseous membrane and descends on the anterior surface of this membrane between tibialis anterior and extensor digitorum longus (Figure 1.4 and Figure 1.5). Anterior tibial artery is the main arterial supply for anterior compartment of the leg (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). 8 Anterior tibial artery has muscular branches which supply adjacent muscles and anastomotic branches which are given to the knee and ankle joints. Anterior and posterior tibial recurrent branches take part in the anastomoses around the knee joint. Anterior medial malleolar and anterior lateral malleolar branches take part in the anastomoses around the ankle joint (Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). Anterior tibial artery ends at the ankle joint, midway between malleoli, where it becomes dorsalis pedis artery (DPA) or dorsal artery of the foot (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). 1.1.1.4 Posterior Tibial Artery Posterior tibial artery, which provides the main arterial supply to the posterior compartment of the leg and the foot, is the larger terminal branch of popliteal artery. It begins at the inferior border of popliteus muscle and passes downward deep to the gastrocnemius, soleus and deep transverse fascia of the leg (Figure 1.4 and Figure 1.7). After giving off peroneal artery, its largest branch, posterior tibial artery passes inferomedially on the posterior surface of tibialis posterior (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). During its descend in the leg, posterior tibial artery is accompanied by tibial nerve and veins. Posterior tibial artery runs downward and slightly medially, to reach the posteromedial side of the ankle, midway between medial malleolus and medial tubercle of calcaneum. Deep to the origin of abductor hallucis and flexor retinaculum, posterior tibial artery divides into lateral and medial plantar arteries (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). 9 Other important branches of posterior tibial artery are muscular branches which are distributed to the muscles in posterior compartment of the leg; anastomotic branches which join other arteries around the ankle joint and a nutrient artery which is given off to the tibia (Moore & Dalley, 1999; Standring, 2004; Snell, 2011; Chaurasia, 2013; Nafis, 2013). Figure 1.7 Dissection of right popliteal region showing the origin and course of posterior tibial artery and peroneal artery. 1.1.1.5 Peroneal Artery Peroneal artery is the largest branch and the most important branch of posterior tibial artery. It begins 2.5 centimetre (cm) below the inferior border of popliteus muscle and 10