* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Exotoxins
Neonatal infection wikipedia , lookup
Germ theory of disease wikipedia , lookup
Lyme disease microbiology wikipedia , lookup
Infection control wikipedia , lookup
Marine microorganism wikipedia , lookup
Triclocarban wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Magnetotactic bacteria wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Disinfectant wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Trimeric autotransporter adhesin wikipedia , lookup
Schistosoma mansoni wikipedia , lookup
Molecular mimicry wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
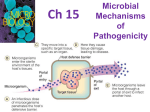
Summary of Lecture 20 • Microbe: human interactions on and within the body are normal. • Human body is a good habitat for suitable bacteria (nutrients, temperature, pH, etc.) • Normal microbe flora is important for general well-being (e.g. vitamin synthesis). • But bacteria sometimes do invade (pathogens). Some parts of human body colonised by bacteria (normal flora) • • • • Skin (Staphylococcus) Mouth (Streptococcus) Respiratory tract (Streptococcus) Gastrointestinal tract – Diverse flora – Largest number in large intestine • Urogenital tract (Lactobacillus) Infection and Disease • Infection is any situation leading to establishment of microbial growth with or without causing damage to the host. • Disease results in damage to the host. • Not all infections cause disease. BS104 Lecture 21 Entry of the pathogen into the host. Colonisation and growth. Toxins. Entry of the pathogen into the host • Pathogens must gain access to host tissue. • They use various strategies to establish virulence. • Virulence - the relative ability of a pathogen to cause damage to the host - disease • In order to cause damage, the pathogen needs to penetrate – Mucous membranes. – The skin (through wounds). – Intestinal epithelium. • Pathogen is often selective for tissue and host. – E.g. Neisseria gonorrhoeae adheres to urogenital epithelial cells. • Adherence to is often very important for pathogenesis. EXPOSURE to pathogens Microorganisms and Pathogenesis ADHERENCE to skin or mucosa Further exposure at local sites •Virulence factors •Invasiveness •Toxicity •Tissue damage INVASION through epithelium COLONIZATION and GROWTH Production of virulence factors TOXICITY: toxin effects are local or systemic Brock: Figure 28.12 Further exposure INVASIVENESS: further growth at original site and distant sites TISSUE DAMAGE, DISEASE Adherence of pathogens to the host • Extracellular macromolecules facilitate bacterial adherence. • Protein: protein interactions (pathogen: host). • Pathogens are selective when adhering to cells. N. gonorrhoeae – urogenital epithelia. • Polysaccharides produced by bacteria: • Dense polymer coat (capsule) • Loose network of polymer fibres (glycocalyx). • Diffuse network of polymer fibres (slime) • Attachment and defence against host immune response • (a) Vibrio cholerae attaching to brush border of rabbit villi. • (b) Escherichia coli infecting calf brush border villi. Note capsule Brock: Figure 28.13 Bacillus anthracis colonies can be mucoid (slimy) in appearance Bacillus anthracis with stained capsule (bright green) – note how capsule extends about 1m From actual cell (cell is about 0.5 m diameter) Fimbriae and Pili • Fimbriae and pili – facilitators of bacterial adherence. • Important bacterial cell surface structures. • They initiate attachment by binding to glycoproteins on the cell surface. • Fimbriated Escherichia coli often cause urinary tract infections. • One of the best characterised fimbriae are the type I fimbriae of enteric bacteria (Escherichia, Klebsiella, Salmonella and Shigella). • Type I fimbriae -uniformly distributed on the cell surface. Escherichia coli EM showing type P fimbriae. Cell is 0.5 m wide Brock: Figure 28.15 Fimbriae and Pili •Pili are longer than fimbriae. •There are less pili found on the surface of the cell. •Both structures bind to host cell surface glycoproteins: leads to adherence to animal cells. Major adherence factors • E.g. Pathogenic forms of Escherichia coli make fimbrial proteins called colonization factor antigens (CFA). • These specifically adhere to the small intestine cells. • Pathogenic E. coli colonizes and makes enterotoxin – a protein released extracellularly –causes damage to the small intestine. Invasion Invasion: Penetration of the microorganism into the host cell (through the epithelium) and subsequently inflicting damage. Broken skin or mucosal surfaces can be points of entry for pathogens. Once growth is established at these sites, colonisation and invasion begin. May also spread throughout the host via the circulatory or lymphatic systems. Colonization and growth • Invasion of pathogen followed by growth leads to colonisation. • Microbial growth requires available nutrients and environmental conditions. – Carbon source, nitrogen source, trace metals. – trace metals are scarce (bound to host cell proteins). – bacteria may make metal chelating compounds so they can scavenge trace metals. – Temperature, pH and oxygen affect microbial growth, but the availability of nutrients is most important. • Localized (focal) infection – Boil (Staphylococcus) • Spread through blood and lymphatic vessels is a general (systemic) infection. – Lymphatic vessels lymph nodes containment by the immune system (?) – Blood distribution throughout the body • Bacteraemia often starts as a localized infection. Infections in sport • Tetanus - Clostridium tetani. – C. tetani spores often contaminate sports fields. – Spores can enter deep wounds and then germinate – Production of exotoxin (neurotoxin) that travels to CNS that can cause death • Other recreational infections: Scrumpox (Herpes gladitorium, impetigo - Staphylococcus); Wound infections (sepsis); Waterborne (giardiasis – Giardia lamblia, leptospirosis); Vectorborne (Lyme disease). Impetigo http://www.healthhype.com/staphskin-infections.html Scrumpox http://www.sciencedaily.com/release s/2008/09/080928210041.htm Scanning EM of the spiral-shaped bacteria of the genus Leptospira – causative agents of leptospirosis. – Janice Carr (CDC –Image no:138) Lyme disease infection; (a) deer tick attached to skin, (b) circular rash associated with lyme disease (Madigan et al., 2009. Brock Biology of Microorganisms. pp.1012. Virulence • Relative ability of a pathogen to cause disease. • LD50 ; The dose (number of bacteria) required to kill 50% of a test group. Virulence •Attenuation: Decrease or loss of virulence. An attenuated (weakened) microorganism would have lost the ability to cause serious illness, but still able to trigger an immune response. These microorganisms may cause a mild or subclinical form of the illness. •Used in vaccine production. Toxicity and Invasiveness Toxicity • Ability of an organism to kill by a preformed toxin that kills host cells. • Tetanus is a disease caused by exotoxin produced by Clostridium tetani. • Bacteria stay in localized wound but toxin spreads through the body. Invasiveness • Growth of bacterium in large enough numbers to inhibit cell function. • Streptococcus pneumoniae produces no toxin but grows in large numbers in the lung. • Polysaccharide capsule of the pathogenic strains prevent phagocytosis. • Host responses lead to pneumonia. Virulence Factors and Toxins • Salmonella virulence factors: – Enterotoxin – Endotoxin – Cytotoxin – kills the cells – Siderophores (iron-chelation, sequestering iron to aid in growth) – Attachment (fimbriae) – Defense (capsule) Virulence Factors and Toxins Injectosome (inv and prg products form complex) Endotoxin in LPS layer (fever) Siderophores Enterotoxin (diarrhea) Virulence plasmid Anti-phagocytic proteins induced by oxyR O antigen (inhibits phagocyte killing) Brock: Figure 28.17 Type 1 fimbriae (adherence) Cytotoxin (inhibits host cell protein synthesis; calcium influx into host; adherence) Vi capsule antigen; Inhibits complement binding Flagellum (motility) H antigen (adherence; inhibits phagocyte killing) Fibrin clots • Produced by host at wound sites. • Some pathogens (e.g. Streptococcus) dissolve clots by production of hyaluronidase (breaks down hyaluronic acid in cell cement). • Other pathogens (e.g. Staphylococcus aureus) promote clots (e.g. by a coagulase). • Fibrin then coats bacteria affording protection to the bacterium. Boils and pimples are the result. • S. aureus strains that are coagulase-positive are more virulent than the ones that are negative. Bacterial toxins Exotoxins • Proteins released (secreted) by bacterium to outside of cell during its growth. • Special secretion machinery often used • Highly toxic • Specific targets usually distant from the site of infection. – Generally no fever Endotoxins • Toxic lipopolysaccharides that are part of the gram negative bacterial cell wall. • Released when bacteria lyse (burst open) • Large bacterial numbers needed for toxic effect. • Weakly toxic • General targets – Fever, diarrhoea Exotoxins • Proteins that are released by bacteria. • Soluble and may travel throughout body of infected person. • See table 28.4 (next 2 slides). Three major categories of exotoxins 1. 2. Cytolytic toxins (e.g. hemolysin – degradation of cytoplasmic membrane leading to cell lysis) AB toxins 1. 2. 3. 4. 3. Diphtheria toxin (Corynebacterium diphtheriae) Botulinum toxin (Clostridium botulinum) Tetanus toxin (Clostridium tetani) Cholera enterotoxin (Vibrio cholerae) Superantigen toxins – stimulate the immune system leading to inflammation Exotoxins Hemolysis by Streptococcus pyogenes • Blood agar plate. • Zones of clearing surrounding bacterial colonies caused by hemolysin that is secreted by bacteria in colonies. • Cytolytic toxin. • Attack host cell wall Exotoxins Diptheria toxin • Produced by Corynebacterium diptheriae. • Rats and mice are insensitive, but humans, rabbits, birds are sensitive. • One toxin molecule can kill a host cell. • Called an AB toxin. • Blocks protein synthesis by ADP ribosylation of elongation factor 2 (EF-2), leading to cell death. • Only made in strains lysogenized by phage (therefore toxicity determined by horizontal gene transfer). • Phage injection converts non-toxic, non-pathogenic strains to pathogenic ones – phage conversion. Exotoxins Cytoplasmic membrane Out Receptor protein Key Diphtheria toxin Amino acid ADP ribosylation of EF-2 Ribosome Normal protein synthesis Protein synthesis stops Diphtheria toxin: Blocks protein synthesis by ADP ribosylation of EF-2. Brock Figure 28.20 In Exotoxins Tetanus and Botulinum toxins are also A-B toxins • Produced by Clostridium tetani and Clostridium botulinum respectively. • Both microbes are obligate anaerobes. • Neither microbe is very invasive – pathogenic effects are due to neurotoxicity. • C. botulinum grows in badly preserved food. • Botulism causes death by muscle paralysis resulting in respiratory failure. • C. tetani grows in deep body wounds. • Toxins spread throughout body via the neural cells, causing spastic paralysis. Tetanus toxin: blocks glycine release – constant Exotoxins acetylcholine release. Inhibitory interneuron Inhibition Excitation signals from the central nervous system Tetanus toxin Muscle Normal Glycine (G) release from inhibitory interneurons stops acetylcholine (A) release and allows relaxation of muscle Tetanus Tetanus toxin binds to inhibitory interneurons, preventing release of glycine (G) and relaxation of muscle Brock: Figure 28.22 Botulinum toxin:Blocks neurotransmitter acetylcholine release Excitation signals from the central nervous system Muscle Normal Acetylcholine (A) induces contraction of muscle fibers Brock: Figure 28.21 Botulism Botulinum toxin, , blocks release of A, inhibiting contraction Exotoxins Clostridium tetani Large gram negative rod with terminal endospores (looks like drumsticks) A soldier dying from tetanus. Painting by Charles Bell in the Royal College of Surgeons, Edinburgh. Exotoxins Enterotoxins • • • • • Exotoxins that act on small intestine. Result in excessive fluid secretion. Cause vomiting and diarrhoea. Food poisoning (Staphylococcus aureus). Intestinal pathogens (Vibrio cholerae, Salmonella enteriditis). Exotoxins Cholera toxin • AB toxin, produced byVibrio cholerae. • The B fragment directs the toxin to the intestinal epithelium.The A fragment crosses the cytoplasmic membrane and activates adenyl cyclase resulting in an increase of cellular cAMP. • cAMP is an important mediator in diverse regulatory systems, including ion balance. • Increased cAMP levels induce chloride and bicarbonate ions to be secreted into the intestinal lumen, leading to an imbalance. This results in excessive amounts of water production into the intestinal lumen and subsequently water loss into the small intestine. • Treatment is by oral solutions containing electrolytes and other solutes to reverse the ion imbalance. Endotoxins • Endotoxins stimulate host to release endogenous pyrogens (leads to fever). • Also cause diarrhoea, inflammation etc. • Large doses can cause death due to haemorrhagic shock and tissue necrosis. • Lower in toxicity than exotoxins. • Endotoxins are the lipopolysaccharides of gramnegative bacteria outer membrane. Further reading • Madigan et al., 2009. Brock: Chapter 28.6 to 28.12