* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Preventing hospitalizations for respiratory syncytial virus infection
Gastroenteritis wikipedia , lookup
Influenza A virus wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
2015–16 Zika virus epidemic wikipedia , lookup
Schistosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Orthohantavirus wikipedia , lookup
Ebola virus disease wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Herpes simplex virus wikipedia , lookup
West Nile fever wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hepatitis B wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Henipavirus wikipedia , lookup
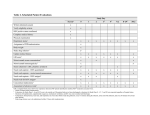
POSITION STATEMENT Preventing hospitalizations for respiratory syncytial virus infection Joan L Robinson, Nicole Le Saux; Canadian Paediatric Society Infectious Diseases and Immunization Committee Paediatr Child Health 2015;20(6):321-26 Posted: Sep 8 2015 Updated: May 12 2016 Abstract Respiratory syncytial virus infection is the leading cause of lower respiratory tract infections in young children. Palivizumab has minimal impact on RSV hospitilization rates as it is only practical to offer it to the highest risk groups. The present statement reviews the published literature and provides updat ed recommendations regarding palivizumab use in children in Canada. Key Words: At-risk infants; Chronic lung disease; Congenital heart disease; Palivizumab; Prematurity; Prophylaxis; RSV Epidemiology Respiratory syncytial virus (RSV) is the most common cause of lower respiratory tract infections (LRTIs) in young children worldwide, with almost all experiencing their first RSV infection by two years of age. In devel oped countries, 1% to 3% of all infants are hospitalized with RSV infection. In Canada, the RSV season typi cally begins in November or December and persists for four to five months. The present statement replaces four previous position statements from the Canadian Paediatric Society on this topic[1]-[4] because there is evidence that the risk of RSV hospitalization does not warrant the use of palivizumab in many children for whom it was previously recommended. Preventing RSV hospitalizations Instructions for parents Young infants (and their siblings) should not be in con tact with individuals with respiratory tract infections whenever practical. A Cochrane review suggests that hand hygiene in the home decreases the spread of respiratory tract infections in children.[5] Breastfeeding and avoidance of cigarette smoke are also presumed to decrease the incidence and/or severity of viral respi ratory tract infections. Palivizumab Palivizumab, a humanized murine monoclonal im munoglobulin G-1 directed against an epitope on the F glycoprotein of RSV, is produced by recombinant DNA technology, and has 95% human and 5% murine amino acid sequences. Rare cases of anaphylaxis are the only recognized serious adverse event. Standard dosing is 15 mg/kg administered intramuscularly every 30 days during RSV season for a maximum of five doses. Some Canadian programs administer the sec ond dose 20 days after the first dose to prevent a low trough level;[6][7] however, there are no data showing an increased RSV hospitalization rate before the sec ond dose. Palivizumab is available in 50 mg or 100 mg vials. Drug costs for five doses of palivizumab for an infant with a mean weight of 5 kg are approximately $5,600, assuming no waste. Palivizumab use in Canada is directed by provincial or territorial programs. When practitioners have questions about eligibility, they should contact their local pro gram; contact information is available through neonatal care units. Some programs routinely begin prophylaxis in November or December. Others use laboratory sur veillance from local laboratories or from the national Respiratory Virus Detection Surveillance System (http://www.phac-aspc.gc.ca/bid-bmi/dsd-dsm/rvdi-divr/ index-eng.php) to determine when to start palivizumab. The latter strategy is more complicated to organize than having a uniform start and stop date, but has been demonstrated to save drug costs in a recent Canadian study.[8] INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 1 Efficacy of palivizumab Table 1 summarizes the results of randomized con trolled trials (RCTs) investigating palivizumab, demon strating a reduction in hospitalizations of approximately 80% in infants with prematurity but without chronic lung disease of prematurity (CLD), of 40% in infants with CLD, and of 45% in children with congenital heart disease (CHD). Efficacy was not demonstrated in the CHD subgroup with cyanotic heart disease.[9]-[11] Observational studies demonstrate effectiveness in the ‘real world’, where clinicians, in conjunction with par ents, decide who should receive palivizumab and where compliance is often lower than in RCTs. A re cent systematic review summarized 20 published ob servational palivizumab studies. Estimates of effective ness were generally in the range predicted by the RCTs.[12] Exceptions included one study with higher and two with lower efficacy. A study from Korea showed a very high 82% efficacy in children with CLD. [13] A study from Sweden showed no efficacy, with RSV hospitalization in 11 of 151 children (7.3%) with CLD who were given palivizumab versus three of 44 (6.8%) who were not (P=0.91). For infants born at <33 weeks’ gestational age (GA) without CLD, hospitalization rates were two of 75 (2.7%) with palivizumab and 22 of 567 (3.9%) without (P=0.61).[14] A study from Japan also showed no efficacy, with RSV hospitalization rates of 39 of 2806 (1.4%) and 45 of 3496 (1.3%) with and without palivizumab in preterm infants, although testing for RSV was not widely available.[15] False-negative results for the detection of RSV in the presence of palivizumab have been described;[16] thus, the efficacy of palivizumab may be lower than that demonstrated in studies. TABLE 1 A summary of findings on the efficacy of palivizumab for preventing respiratory syncytial virus (RSV) hospitalizations in randomized controlled trials Risk group Illustrative comparative Relative effect Participants, n risks of RSV hospitalization (95% CI) (studies, n) (95% CI) Assumed risk Corresponding risk Quality of the evi dence (GRADE)* Comments Control Palivizumab Infants born at <36 weeks’ GA with no CLD who are <6 months of age at the start of RSV season – RCT (1998)[9] 81 per 1000 18 per 1000 (8 to 39) RR 0.22 (0.1 to 740 (1 study) 0.48) ++++ high NNTI=16 (9– 32) Children with CLD diagnosed clinically and treated with steroids, bronchodilators, diuretics or supplemental oxygen in the past 6 months who are <24 months of age at the start of RSV season – RCT (1998)[9] 128 per 1000 78 per 1000 (51 RR 0.62 (0.4 to 762 (1 study) to 122) 0.95) ++++ high NNTI=20 (10–198) Children with hemodynamically significant CHD who are <24 months of age at the start of RSV season – RCT (2003)[10] 97 per 1000 53 per 1000 (36 RR 0.55 (0.37 to 80) to 0.82) 1287 (1 study) ++++ high NNTI=23 (95% CI 14– 66) Children with CF – RCT (2005)[11]† 11 per 1000 11 per 1000 (1 to 177) 186 (1 study) ++−−low RR 1.02 (0.06 to 16.09) *GRADE Working Group grades of evidence: High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Fur ther research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very like ly to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the esti mate. CF Cystic fibrosis; CHD Congenital heart disease; CLD Chronic lung disease of prematurity; GA Gestational age; NNTI Number needed to vaccinate to prevent one case; RCT Randomized controlled trial; †Only ever published in abstract form, so many details are unclear Cost-effectiveness of palivizumab Reports concerning the cost-effectiveness of palivizumab have varied, owing in large part to dis parate estimates of its short- and long-term benefits.[17] [18] In terms of short-term benefits, there is no evidence that palivizumab prevents mechanical ventilation or death or that breakthrough RSV hospitalizations are less severe than hospitalizations in controls. With re 2 | PREVENTING HOSPITALIZATIONS FOR RESPIRATORY SYNCYTIAL VIRUS INFECTION gard to longer-term benefits, one RCT showed that palivizumab administered to infants 33 to 35 weeks’ GA without CLD decreased days with parent-reported wheezing in the first year from 4.5% to 1.8% (P<0.001; number needed to treat = 38) and decreased recurrent wheezing from 21% to 11% (P=0.01).[19] Prophylaxis must be provided to many infants to pre vent one hospitalization (Table 1), while the cost to provide prophylaxis to a single infant (approximately $5,600) exceeds that of a typical RSV hospitalization (three or four days). Therefore, given the paucity of ev idence that palivizumab prevents severe outcomes, palivizumab is unlikely to be cost-effective in children with prematurity, CLD or CHD, and can only be poten tially cost-effective in settings where RSV hospitaliza tions are exceedingly common and very expensive (such as Inuit infants in rural Baffin Island).[20] Challenges of identifying the children at highest risk CHD and CLD Higher rates and durations of hospitalization and more intensive care unit admissions occur in RSV-infected children with CHD or CLD compared with healthy term infants. A common recommendation has been to offer palivizumab to children up to 24 months of age at the start of RSV season when they have hemodynamically significant CHD or are still receiving therapy for CLD. A 24-month cut-off applies simply because this age limit was used in the original studies.[9][10] One study from Switzerland showed that only two of 10 RSV admis sions in children with CHD occurred in the second year of life,[21] while a study from Norway showed a mean admission age of 9.5 months in children with CHD.[22] In the original palivizumab CHD trial, RSV admissions in controls declined from 12% in infants <6 months of age to 7% at six to 12 months, and to 4% at 12 to 24 months.[10] Admission rates in one Canadian prospec tive CHD trial were 16% at <6 months of age (n=42), 0% at six to 12 months of age (n=26), and 1% at 12 to 24 months of age (n=105).[23] A study involving children on Medicaid with CLD showed an estimated RSV ad mission rate (extrapolated from the incidence of bron chiolitis) of 38.8% in year one (95% CI 30.4% to 49.0%) falling to 7.3% (95% CI 4.2% to 11.9%) in year two, and 1.3% (95% CI 0.2% to 4.6%) in year three.[24] Figures 1 and 2[9][10][13][21][23][25]-[33] summarize the inci dence of RSV hospitalization in studies that investigat ed proven RSV infection in children with CHD or CLD who did not receive palivizumab. They show rates of approximately 10% with CHD and 15% to 20% with CLD. One limitation is that most studies were conduct ed in the 1990s and very few were population-based. Hospitalized infants were not uniformly tested for RSV and most studies were from the premolecular era of RSV testing; thus, RSV hospitalizations may have been missed. There have been major advances in therapy for CHD and CLD such that children with these conditions now have less severe disease than children born in the 1990s. At the same time, however, increas es in infant survival rates mean that there are still med ically fragile children with severe CHD and CLD. Prematurity without CLD Since palivizumab was licensed in 2002, most Canadi an infants born before 32 weeks’ GA without CLD were offered prophylaxis if they were <6 months of age at the start of RSV season. Programs have offered pro phylaxis to selected infants born up to 35 weeks, 6 days’ GA who were believed to be at higher risk for RSV hospitalization, typically based on a scoring sys tem.[34] Despite the fact that the efficacy of palivizumab is higher in healthy preterm infants than in those with CHD or CLD, use in healthy premature infants has re cently come into question[35] based on the following in formation: • Although RSV hospitalization rates correlate with GA, the magnitude of difference between preterm infants without CLD and term infants does not war rant routine use of palivizumab, except possibly in very preterm infants. Figure 3[9][30][36]-[43] shows RSV hospitalization rates without palivizumab that are significantly lower than for infants with CHD (Figure 1) or CLD (Figure 2). Even in infants born before 30 weeks’ GA, admission rates were <10% in all but one study.[37] The main limitation of Figure 3 is that, as with Figures 1 and 2, case findings were incomplete in some studies, but this proviso should have applied equally to all GAs. • There have been significant advances in neonatol ogy, such that infants with or without CLD are now healthier and have less residual lung damage than did infants of the same GA in the past. • The parents of fragile infants are now more aware of the principles of infection transmission than in decades past. Parental leaves are longer and there are fewer young infants in child care settings, where the risk of RSV acquisition is higher. INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 3 Figure 1) Percentage of proven respiratory syncytial virus (RSV) hospitalizations in children with congenital heart disease who were not given palivizumab arranged according to the year that data collection ended. At study entry, children were up to 12 months [26], 24 months[10][21][25][27] or 36 months[23] of age. For the study from Sweden,[26] the number of children with congenital heart disease was estimated 4 | PREVENTING HOSPITALIZATIONS FOR RESPIRATORY SYNCYTIAL VIRUS INFECTION Figure 2) Incidence of proven respiratory syncytial virus (RSV) hospitalizations per 1000 children with chronic lung disease of prematurity who were not given palivizum ab, presented according to age at the time of the study. The bars represent 95% CIs (except for refer ence 29, in which raw data were not provided). For the study from Sweden,[26] the number of children with chronic lung disease of prematurity was estimated Figure 3) Incidence of proven respiratory syncytial virus (RSV) hospitalizations per 1000 preterm children without chronic lung disease of prematurity who were not given palivizumab, arranged according to gestational age. The bars represent 95% CIs. RSV testing was not performed in 38 of 118 admissions in reference 36. *The upper limit of the 95% CI is 42.9 Aboriginal infants High rates of hospitalization due to LRTIs have been described in isolated Inuit populations: 484 per 1000 infants <6 months of age in the Qikiqtaaluk (Baffin) re gion of Nunavut in 1997/1998,[44] and 202 per 1000 in fants <12 months of age in 2009/2010.[45] Rates were 590 per 1000 infants in the first year of life in the Kitik meot region of Nunavut between 2000 and 2004[46] and 389 per 1000 in 2009/2010.[45] Approximately onehalf of LRTIs are due to RSV. There is a high incidence of complications when infants from remote Northern communities are hospitalized with LRTIs.[46] Morbidity from LRTIs appears to be far lower in non-Inuit Aborig inal children. Whether palivizumab should be offered to term Inuit in fants in high-incidence communities is controversial. Palivizumab would have saved costs in term infants during the 2002 RSV season in rural Baffin Island Inuit communities, where hospitalization requires air evacu ation,[20] with similar findings from the same communi ties in the 2009 RSV season.[47] It appears to be likely that other measures to reduce LRTIs, such as im proved housing, prevention of exposure to smoke, and optimal use of influenza and other vaccines, would be more cost-effective than palivizumab in the long term. [48] Immunocompromised children There are no population-based data for this population, but severe disease and prolonged viral shedding are well-recognized risks.[49] A 2010 to 2013 Canadian Paediatric Surveillance Program study estimated an RSV hospitalization rate of five of 488 (1.0%) for hematopoietic stem cell transplant recipients and 13 of 274 (4.7%) for solid organ transplant recipients within two years post-transplant, with two deaths and one child requiring prolonged ventilation.[50] Under-report ing of cases is suspected and a validation study is on going. Lymphopenia, young age, and use of corticos teroids also appear to be risk factors for severe RSV in the immunocompromised child.[35] INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 5 Children with upper airway obstruction or pulmonary disease not related to prematurity The risk of hospitalization due to RSV is increased but not well quantified in children with neuromuscular dis orders, recurrent aspiration, pulmonary malformations, upper airway conditions such as Pierre Robin syn drome, and for conditions requiring a tracheostomy or noninvasive mechanical ventilation. Results of two small, [11][51] and one large[52] study of palivizumab in children with cystic fibrosis were inconclusive. RSV ad mission rates were low. Children with Down syndrome One non-population-based study showed that 39 of 395 children with Down syndrome (9.9%) experienced RSV hospitalization in the first two years of life, at a median age of six months, with the rate being 7.6% for term infants without CHD, 9.4% for preterm infants, and 11.9% for those with CHD.[53] There was no in creased risk of recurrent wheezing in individuals hospi talized with RSV infections.[54] Decisions regarding prophylaxis are complicated by the fact that another study showed a much older median age (1.3 years) at the time of RSV hospitalization with Down syndrome. [55] A Canadian study demonstrated only a small num ber of palivizumab breakthrough infections in children with Down syndrome.[56] Pharmacokinetics of palivizumab The level of palivizumab postulated to prevent RSV hospitalization is based on the fact that a trough of 25 mg/mL to 30 mg/mL decreased RSV titres by an aver age of 99% in the lungs of cotton rats,[57] with all achieving a 99% drop at 40 mg/mL.[58] Lower doses, less frequent doses or a smaller number of total doses have the potential to protect children throughout RSV season,[59] because the trough remains >40 mg/mL for >30 days following the third dose.[60][61] A recent study demonstrated that a presumed therapeutic level of 30 mg/mL to 40 mg/mL can be maintained for the typical duration of the RSV season with only four doses, if doses 2, 3 and 4 are given 38 rather than 30 days apart.[62] Furthermore, a lower trough than 30 mg/mL to 40 mg/mL may be sufficient. Based on these premises, the British Columbia program administers <5 doses. A maximum of three doses are provided to infants born at 29 to 34 weeks’ GA without CLD, and they have reported no RSV admissions >35 days after the third dose in 514 infants over four RSV seasons.[63] A maximum of four doses are provided to higher-risk infants, and they have reported only two admissions >35 days after the fourth dose in 666 infants over two RSV seasons.[64] 6 | PREVENTING HOSPITALIZATIONS FOR RESPIRATORY SYNCYTIAL VIRUS INFECTION Recommendations Good hand hygiene in the home and avoiding contact of high-risk children with people with RTIs, where prac tical, remain paramount for RSV prevention. Breast feeding and avoidance of exposure to cigarette smoke should be encouraged. Given that the efficacy of palivizumab is <50% in the highest-risk groups (CLD or CHD), and that most hospitalizations occur in healthy term infants, more education should be direct ed at such prevention strategies. Use of palivizumab in different risk groups • Children with hemodynamically significant CHD or CLD (defined as a need for oxygen at 36 weeks’ GA) who require ongoing diuretics, bronchodilators, steroids or supplemental oxygen, should receive palivizumab if they are <12 months of age at the start of RSV season. Because the incidence of RSV decreases in the second year of life, palivizumab is not indicated during the second RSV season for infants with CHD or for the vast majority of children with CLD (with the exception of those still on or weaned off of supplemental oxygen in the past three months). • In preterm infants without CLD born before 30 + 0 weeks’ GA who are <6 months of age at the start of RSV season, it is reasonable (but not essential) to offer palivizumab. Infants born after 30 + 0 weeks’ GA have RSV admission rates that are con sistently ≤7% (Figure 3), yielding a minimum num ber needed to treat of 18 (90 doses of palivizumab to prevent one RSV admission) if one assumes 80% efficacy and five doses per infant. Therefore, palivizumab should not be prescribed for this group. • Infants in remote communities who would require air transportation for hospitalization born before 36 + 0 weeks’ GA and <6 months of age at the start of RSV season should be offered palivizumab. It is not clear whether this recommendation should ap ply only to Inuit infants, to all Aboriginal infants or to all infants in remote communities. The incidence of RSV hospitalization in a remote community in pre vious years should be taken into account when making this decision. A practical issue is that the onset and duration of RSV season is unpredictable in the Far North. A logical option is to delay admin istering palivizumab until RSV is detected in the Far North. The attendant risk is that significant spread may have already occurred. Consideration may be given to administering palivizumab during RSV season to term Inuit infants until they reach six months of age only if they live in communities with documented persistent high rates of RSV hospital ization. However, the first priority should be to pro vide palivizumab to infants with prematurity, CLD or CHD. • Children with immunodeficiencies, Down syn drome, cystic fibrosis, upper airway obstruction or a chronic pulmonary disease other than CLD should not routinely be offered palivizumab. However, pro phylaxis may be considered for children <24 months of age who are on home oxygen, have had a prolonged hospitalization for severe pulmonary disease or are severely immunocompromised. • Continuation of monthly palivizumab is not recom mended for children hospitalized with break through RSV infection. Repeat RSV infections in one season are not common. Although recom mended on the product monograph, the number needed to treat is no doubt very high if one contin ues palivizumab following RSV infection. Optimization of program Each jurisdiction should optimize processes to imple ment these recommendations in the most cost-effec tive manner, ensuring that health care providers who administer palivizumab are prepared to monitor for and treat anaphylaxis. Well-organized palivizumab clinics decrease drug wastage. • For eligible infants being discharged home for the first time during RSV season, palivizumab should be started just before discharge. Use before dis charge to prevent nosocomial RSV is an expensive strategy that is not recommended. • Programs should administer a maximum of three to five doses, with four doses probably being sufficient in all risk groups if palivizumab is started only when there is RSV activity in the community, especially if doses 2, 3, and 4 are given 38 days apart. • There is no evidence to support giving >5 doses in one RSV season, administration to any child >24 months of age at the start of RSV season, or using palivizumab as RSV therapy. Annual program review A panel of experts should be convened in each province or territory to review annually the palivizumab program guidelines and outcomes. People serving on these panels should not have conflicts of interest, in cluding research funding, participation in a speaker’s bureau or financial links, with the pharmaceutical firm that makes palivizumab. Acknowledgements This position statement has been reviewed by the Acute Care, Community Paediatrics, and Fetus and Newborn Committees of the Canadian Paediatric Soci ety. References 1. Tan B; Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Palivizumab and respira tory syncytial virus globulin intravenous for the prophy laxis of respiratory syncytial virus infection in high risk infants. Paediatr Child Health 1999;4(7):474-80. 2. Langley JM; Canadian Paediatric Society, Infectious Dis eases and Immunization Committee. Use of palivizumab in children with congenital heart disease. Paediatr Child Health 2003;8(10):631-3. 3. Sampson L; Canadian Paediatric Society, Infectious Dis eases and Immunization Committee. Prevention of res piratory syncytial virus infection. Paediatr Child Health 2009;14(8):521-6. 4. Robinson JL; Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Preventing res piratory syncytial virus infections. Paediatr Child Health 2011;16(8):487-8. 5. Jefferson T, Del Mar C, Dooley L, et al. Physical inter ventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev 2010; (1):CD006207. 6. Mitchell I, Paes BA, Li A, Lanctôt KL; the CARESS in vestigators. CARESS: The Canadian Registry of Palivizumab. Pediatr Infect Dis J 2011;30(8):651-5. 7. Zaaijer HL, Vandenbroucke-Grauls CM, Franssen EJ. Optimum dosage regimen of palivizumab? Ther Drug Monit 2002;24(3):444-5. 8. Paes BA, Craig C, Pigott W, Latchman A. Seasonal res piratory syncytial virus prophylaxis based on predeter mined dates versus regional surveillance data. Pediatr Infect Dis J 2013;32(9):e360-4. 9. The Impact-RSV Study Group. Palivizumab, a human ized respiratory syncytial virus monoclonal antibody, re duces hospitalization from respiratory syncytial virus in fection in high-risk infants. Pediatrics 1998;102(3):531-7. 10. Feltes TF, Cabalka AK, Meissner HC, et al. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant heart disease. J Pediatr 2003;143(4):532-40. 11. Robinson KA, Odelola OA, Saldanha I. Palivizumab for prophylaxis against respiratory syncytial virus infection in children with cystic fibrosis. Cochrane Database Syst Rev 2014;(5):CD007743. 12. Homaira N, Rawlinson W, Snelling TL, Jaffe A. Effective ness of palivizumab in preventing RSV hospitalization in INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 7 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. high risk children: A real-world perspective. Int J Pediatr 2014;2014:571609. Chang SG, Park MS, Yu JE. Outcomes of palivizumab prophylaxis for respiratory syncytial virus infection in preterm children with bronchopulmonary dysplasia at a single hospital in Korea from 2005 to 2009. J Korean Med Sci 2010;25(2):251-6. Henckel E, Luthander J, Berggren E, et al. Palivizumab prophylaxis and hospitalization for respiratory syncytial virus disease in the Stockholm infant population, 1999 through 2002. Pediatr Infect Dis J 2004;23(1):27-31. Kusuda S, Koizumi T, Sakai T, Fujimura M, Nishida H, Togari H. Results of clinical surveillance during the Japanese first palivizumab season in 2002-2003. Pedi atr Int 2006;48(4):362-8. Deming DJ, Patel N, McCarthy MP, Mishra L, Shapiro AM, Suzich JA. Potential for palivizumab interference with commercially available antibody-antigen based res piratory syncytial virus diagnostic assays. Pediatr Infect Dis J 2013;32(10):1144-6. Smart KA, Lanctôt KL, Paes BA. The cost effectiveness of palivizumab: A systematic review of the evidence. J Med Econ 2010;13(3):453-63. Hampp C, Kauf TL, Saidi AS, Winterstein AG. Cost-ef fectiveness of respiratory syncytial virus prophylaxis in various indications. Arch Pediatr Adolesc Med 2011;165(6):498-505. Blanken MO, Rovers MM, Molenaar JM, Winkler-Sein stra PL, et al. Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. New Engl J Med 2013;368(19):1791-9. Tam DY, Banerji A, Paes BA, Hui C, Tarride JE, Lactôt KL. The cost effectiveness of palivizumab in term Inuit infants in the Eastern Canadian Arctic. J Med Econ 2009;12(4):361-70. Duppenthaler A, Ammann RA, Gorgievski-Hrisoho M, Pfammatter JP, Aebi C. Low incidence of respiratory syncytial virus hospitalisations in haemodynamically sig nificant congenital heart disease. Arch Dis Child 2004;89(10):961-5 Meberg A, Bruu AL. Respiratory syncytial virus infec tions in congenital heart defects – hospitalizations and costs. Acta Paediatr 2006;95(4):404-6. Wang EE, Law BJ, Robinson JL, et al. PICNIC (Pediatric Investigators Collaborative Network on Infections in Canada) study of the role of age and respiratory syncy tial virus neutralizing antibody on respiratory syncytial virus illness in patients with underlying heart or lung dis ease. Pediatrics 1997;99(3):E9. Boyce TG, Mellen BG, Mitchel EF Jr, Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid. J Pediatr 2000;137(6):865-70. Simões EA, Sondheimer HM, Top FH Jr, et al. Respira tory syncytial virus immune globulin for prophylaxis against respiratory syncytial virus disease in infants and children with congenital heart disease. The Cardiac Study Group. J Pediatr 1998;133(4):492-9. 8 | PREVENTING HOSPITALIZATIONS FOR RESPIRATORY SYNCYTIAL VIRUS INFECTION 26. Eriksson M, Bennet R, Rotzén-Ostlund M, von Sydow M, Wirgart BZ. Population-based rates of severe respi ratory syncytial virus infection in children with and with out risk factors, and outcome in a tertiary care setting. Acta Paediatr 2002;91(5):593-8. 27. Medrano López C, García-Guereta L; CIVIC Study Group. Community-acquired respiratory infections in young children with congenital heart diseases in the palivizumab era: The Spanish 4-season civic epidemio logic study. Pediatr Infect Dis J 2010;29(12):1077-82. 28. Thomas M, Bedford-Russell A, Sharland M. Hospitalisa tion for RSV infection in ex-preterm infants: Implications for use of RSV immune globulin. Arch Dis Child 2000;83(2):122-7. 29. Berner R, Schwoerer F, Schumacher RF, Meder M, Forster J. Community and nosocomially acquired respi ratory syncytial virus infection in a German paediatric hospital from 1988 to 1999. Eur J Pediatr 2001;160(9): 541-7. 30. Pedraz C, Carbonell-Estrany X, Figueras-Aloy J, Quero J; IRIS Study Group. Effect of palivizumab prophylaxis in decreasing respiratory syncytial virus hospitalizations in premature infants. Pediatr Infect Dis J 2003;22(9):823-7. 31. The PREVENT Study Group. Reduction of respiratory syncytial virus hospitalization among premature infants and infants with bronchopulmonary dysplasia using res piratory syncytial virus immune globulin prophylaxis. Pe diatrics 1997;99(1):93-9. 32. Greenough A, Cox S, Alexander J, et al. Health care utilisation of infants with chronic lung disease, related to hospitalisation for RSV infection. Arch Dis Child 2001;85(6):463-8. 33. Rietveld E, Vergouwe Y, Steyerberg EW, et al. Hospital ization for respiratory syncytial virus infection in young children: Development of a clinical prediction rule. Pedi atr Infect Dis J 2006;25(3):201-7. 34. Paes B, Steele S, Janes M, Pinelli J. Risk-Scoring Tool for respiratory syncytial virus prophylaxis in premature infants born at 33-35 completed weeks’ gestational age in Canada. Curr Med Res Opin 2009;25(7):1585-91. 35. American Academy of Pediatrics Committee on Infec tious Diseases; American Academy of Pediatrics Bron chiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young chil dren at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 2014;134(2):415-20. 36. Park HW, Lee BS, Kim AR, et al. Epidemiology of respi ratory syncytial virus infection in infants born at less than thirty-five weeks of gestational age. Pediatr Infect Dis J 2012;31(8):e99-104. 37. Grimaldi M, Gouyon B, Sagot P, et al. Palivizumab effi cacy in preterm infants with gestational age or = 30 weeks without bronchopulmonary dysplasia. Pediatr Pulmonol 2007;42(3):189-92. 38. Resch B, Pasnocht A, Gusenleitner W, Müller W. Re hospitalisations for respiratory disease and respiratory syncytial virus infection in preterm infants of 29-36 weeks gestational age. J Infect 2005;50(5):397-403. 39. Lacaze-Masmonteil T, Truffert P, Pinquier D, et al. Lower respiratory tract illness and RSV prophylaxis in very pre mature infants. Arch Dis Child 2004;89(6):562-7. 40. Figueras-Aloy J, Carbonell-Estrany X, Quero-Jiménez J, et al. FLIP-2 Study: Risk factors linked to respiratory syncytial virus infection requiring hospitalization in pre mature infants born in Spain at a gestational age of 32 to 35 weeks. Pediatr Infect Dis J 2008;27(9):788-93. 41. Wegner S, Vann JJ, Liu G, et al. Direct cost analyses of palivizumab treatment in a cohort of at-risk children: Evi dence from the North Carolina Medicaid Program. Pedi atrics 2004;114(6):1612-9. 42. Ambrose CS, Anderson EJ, Simões EA, et al. Respira tory syncytial virus disease in preterm infants in the U.S. born at 32-35 weeks gestation not receiving immunopro phylaxis. Pediatr Infect Dis J 2014;33(6):576-82. 43. Mitchell I, Tough S, Gillis L, Majaesic C. Beyond ran domized controlled trials: A “real life” experience of res piratory syncytial virus infection prevention in infancy with and without palivizumab. Pediatr Pulmonol 2006;41(12):1167-74. 44. Banerji A, Bell A, Mills EL, et al. Lower respiratory tract infections in Inuit infants on Baffin Island. CMAJ 2001;164(13):1847-50. 45. Banerji A, Panzov V, Robinson J, Young M, Ng K, Mam dani M. The cost of lower respiratory tract infections hospital admissions in the Canadian Arctic. Int J Circum polar Health 2013;72. 46. Young M, Kandola K, Mitchell R, Leamon A. Hospital ad mission rates for lower respiratory tract infections in in fants in the Northwest Territories and Kitikmeot region of Nunavut between 2000 and 2004. Paediatr Child Health 2007;12(7):563-6. 47. Banerji A, Young M, Bisson D et coll. Is an ounce of palivizumab worth a pound of cure? [résumé] Can J In fect Dis Med Microbiol 2010;21:189. 48. Banerji A, Greenberg D, White LF, et al. Risk factors and viruses associated with hospitalization due to lower res piratory tract infections in Canadian Inuit children: A case-control study. Pediatr Infect Dis J 2009;28(8): 697-701. 49. El Saleeby CM, Somes GW, DeVincenzo JP, Gaur AH. Risk factors for severe respiratory syncytial virus dis ease in children with cancer: The importance of lym phopenia and young age. Pediatrics 2008;121(2): 235-43. 50. Robinson JL, Grenier D, MacLusky I, Allen UD. Respira tory syncytial virus infections in paediatric transplant re cipients: A Canadian Paediatric Surveillance Program study. Pediatr Transplant 2015;19(6):659-62. 51. Giebels K, Marcotte JE, Podoba J, et al. Prophylaxis against respiratory syncytial virus in young children with cystic fibrosis. Pediatr Pulmonol 2008;43(2):169-74. 52. Winterstein AG, Eworuke E, Xu D, Schuler P. Palivizum ab immunoprophylaxis effectiveness in children with cystic fibrosis. Pediatr Pulmonol 2013;48(9):874-84. 53. Bloemers BL, van Furth AM, Weijerman ME, et al. Down syndrome: A novel risk factor for respiratory syncytial 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. virus bronchiolitis – a prospective birth-cohort study. Pe diatrics 2007;120(4):e1076-81. Bloemers BL, van Furth AM, Weijerman ME, et al. High incidence of recurrent wheeze in children with down syndrome with and without previous respiratory syncytial virus lower respiratory tract infection. Pediatr Infect Dis J 2010;29(1):39-42. Megged O, Schlesinger Y. Down syndrome and respira tory syncytial virus infection. Pediatr Infect Dis J 2010;29(7):672-3. Paes B, Mitchell I, Yi H, Li A, Lanctôt KL; CARESS In vestigators. Hospitalization for respiratory syncytial virus illness in Down syndrome following prophylaxis with palivizumab. Pediatr Infect Dis J 2014;33(2):e29-33. Johnson S, Oliver C, Prince GA, et al. Development of a humanized monoclonal antibody (MEDI-493) with potent in vitro and in vivo activity against respiratory syncytial virus. J Infect Dis 1997;176(5):1215-24. Subramanian KN, Weisman LE, Rhodes T, et al. Safety, tolerance and pharmacokinetics of a humanized mono clonal antibody to respiratory syncytial virus in prema ture infants and infants with bronchopulmonary dyspla sia: MEDI-493 Study Group. Pediatr Infect Dis J 1998;17(2):110-15. Zaaijer HL, Vandenbroucke-Grauls CM, Franssen EJ. Optimum dosage regimen of palivizumab? Ther Drug Monit 2002;24:444-5. Robbie GJ, Zhao L, Mondick J, Losonsky G, Roskos LK. Population pharmacokinetics of palivizumab, a human ized anti-respiratory syncytial virus antibody, in adults and children. Antimicrob Agents Chemother 2012;56(9): 4927-36. Solimano A, Kwan E. Revisiting palivizumab (PVZ) dos ing recommendations based on published pharmacoki netics data. [Abstract 4350.8]. Pediatric Academic Soci eties Meeting. Boston, April 28 to May 1, 2012. Gutfraind A, Galvani AP, Meyers LA. Efficacy and opti mization of palivizumab injection regimens against respi ratory syncytial virus infection. JAMA Pediatr 2015;169(4):341-8. Solimano A, Eastman P, Butler A, Taylor R, MacRae S. Three seasonal palivizumab doses over four seasons is perfectly adequate RSV prophylaxis for moderate risk infants. [Abstract 4159.437]. Pediatric Academic Soci eties Meeting. San Diego, April 25 to 28, 2015. Solimano A, Eastman P, Butler A, et al. The approval of four seasonal palivizumab doses provides cost-effective protection in infants at high risk of RSV admission dur ing the five-month British Columbia season – A multiseason analysis. [Abstract 4159.436]. Pediatric Acade mic Societies Meeting. San Diego, April 25 to 26, 2015. CPS INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE Members: Natalie A Bridger MD; Jane C Finlay MD (past member); Susanna Martin MD (Board Representative); Jane C McDonald MD; Heather Onyett MD; Joan L Robinson MD (Chair); Marina Salvadori MD INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE, CANADIAN PAEDIATRIC SOCIETY | 9 (past member); Otto G Vanderkooi MD Consultants: Noni E MacDonald MD Liaisons: Upton D Allen MBBS, Canadian Pediatric AIDS Research Group; Tobey Audcent MD, Committee to Advise on Tropical Medicine and Travel (CATMAT), Public Health Agency of Canada; Carrie Byington MD, Committee on Infectious Diseases, American Academy of Pediatrics; Charles PS Hui, Committee to Advise on Tropical Medicine and Travel (CATMAT), Public Health Agency of Canada; Nicole Le Saux MD, Immunization Monitoring Program, ACTive (IMPACT); Dorothy L Moore MD, National Advisory Committee on Immunization (NACI); Nancy Scott-Thomas MD, College of Family Physicians of Canada; John S Spika MD, Public Health Agency of Canada Principal authors: Joan L Robinson MD and Nicole Le Saux MD Also available at www.cps.ca/en © Canadian Paediatric Society 2017 The Canadian Paediatric Society gives permission to print single copies of this document from our website. For to reprint orHOSPITALIZATIONS reproduce multiple copies, please see our copyright policy. 10permission | PREVENTING FOR RESPIRATORY SYNCYTIAL VIRUS INFECTION Disclaimer: The recommendations in this position statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking in to account individual circumstances, may be appropriate. Internet addresses are current at time of publication.