* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download visual field defects in optic chiasm lesions
Survey
Document related concepts
Transcript
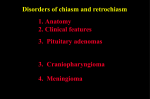
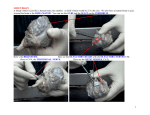
CLINICAL ASPECTS VISUAL FIELD DEFECTS IN OPTIC CHIASM LESIONS MARIETA DUMITRACHE1, RODICA LASCU2 1 Ophthalmological Emergency Clinical Hospital, Bucureşti, 2Emergency Clinical County Hospital, Sibiu Keywords: bitemporal defect-quadrantic or hemianopic, Wilbrand’knee, junctional scotoma, bitemporal hemianopic scotomas, arcuate defect Abstract: Temporal visual field defects result from the compression of the optic chiasm medially involving the crossing of nasal retinal fibres, while nasal visual field defects occur with lateral optic chiasm compression involving the temporal retinal fibres. The visual field defects reported with optic chiasm compression include nasal visual field loss, arcuate visual field defects, scotomatous visual field defects and homonymous visual field loss, in addition to the typical temporal visual field loss. Cuvinte cheie: defect bitemporal-cvadrantic sau hemianopic, genunchiul lui Wilbrand, scotom joncţional, scotoame hemianopice bitemporale, defect arcuat Rezumat: Defectele câmpului vizual temporal rezultă de la compresiunea chiasmei optice implicând medial încrucişarea fibrelor retiniene nazale, în timp ce defectele câmpului vizual nazal apar cu compresia chiasmei optice laterale implicând fibrele retiniene temporale. Defectele câmpului vizual raportate cu compresia chiasmei optice includ pierderea câmpului vizual nazal, defecte ale câmpului vizual arcuat, defecte câmp vizual scotoame şi pierderea câmpului vizual omonim, pe lângă pierderea câmpului vizual temporal tipic. „Rules of the road” for the optic chiasm: Three rules describe the course of major fibres bundles in the chiasm: • The nasal retinal fibres (including the nasal half of the macula) of each eye cross in the chiasm to the contralateral optic tract. Temporal fibres remain uncrossed. Thus, a chiasmal lesion will cause a bitemporal hemianopia due to interruption of decussating nasal fibres. • Lower retinal fibres project through the optic nerve and chiasm to lie laterally in the tracts; upper retinal fibres will lie medially (there is a 90-degree rotation of fibres from the nerves through the chiasm into the tracts) • Inferonasal retinal fibres cross into the chiasm and cross anteriorly approximately 4 mm in the contralateral optic nerve (Wilbrand ́s knee) then redress back in to opposite optic tract. The existence of Wilbrand ́s knee is controversial. • „Macular” crossing fibres are distributed throughout the chiasm and if primarily affected, cause a „central” bitemporal hemianopia. • Clinical “pearl”: if a patient comes in with poor vision in the left eye, the important eye for visual examination is the right due to the involvement of Wilbrand‘s knee. The lesion is now intracranial at the junction of the left optic nerve and chiasm. The field defects constitute a junctional scotoma. Although there are many variations in the visual field defects caused by the damage to the optic chiasm, the essential feature is some type of bitemporal defect, the hallmark of damage to fibres that cross within the chiasm. The bitemporal defects may be superior, inferior, or complete, and they may be peripheral, central, or both. Many lesions that arise in the region of the chiasm affect not only the entire chiasm but also the intracranial optic nerves. Most visual field defects produced by lesions that damage the optic chiasm seem to result from the damage at one of three locations: (a) the anterior angle of the chiasm, (b) the body of the chiasm, or (c) the posterior angle of the chiasm. Lesions that damage the body of the optic chiasm The lesions that damage the body of the optic chiasm produce a bitemporal defect that may be quadrantic or hemianopic and that may be peripheral, central, or both, with or without the so-called „splitting of the macula”. In most cases, visual acuity is normal. In some patients, however, visual acuity is diminished and a bitemporal hemianopia is present. When the lesion compresses the chiasm from below, such as occurs with a pituitary adenoma, the field defects are typical. When the peripheral fibres are principally affected, the field defects usually commence in the outer upper quadrants of both eyes. In the field of the right eye, the defect usually progresses in a clockwise direction and in the left eye in a counterclockwise direction. Alternatively, suprasellar, suprachiasmal compressive lesions-such as tuberculum sellae meningiomas, craniopharyngiomas, aneurysms, and dolichoectatic anterior cerebral arteries-may damage the superior fibers of the optic chiasm, as may infiltrating lesions such as benign and malignant gliomas, and cavernous angiomas. The defects in the visual fields in such cases are still bitemporal, but are located in the inferior rather than the superior fields of both eyes. Papilledema, which is quite unusual in patients with suprasellar, infrachiasmal lesions, is somewhat more common in suprachiasmal lesions because such lesions can extend into the 3rd ventricle. Lesions that damage the posterior angle of the optic chiasm 1 Corresponding author: Rodica Lascu, Str. Aleea Infanteriştilor, Bloc I, Scara B, Etaj III, Ap.25, Sibiu, România; e-mail: [email protected]; tel +40-720547341 Article received on 26.01.2012 and accepted for publication on 23.03.2012 ACTA MEDICA TRANSILVANICA June 2012;2(2):185-187 AMT, v. II, no. 2, 2012, p. 185 CLINICAL ASPECTS Lesions that damage the posterior aspect of the optic chiasm produce characteristic defects in the visual fields: bitemporal hemianopic scotomas. Such defects may be cecocentral scotomas and attributed to a toxic, metabolic, or even hereditary process rather than to a tumour. True bitemporal hemianopic scotomas are almost always associated with normal visual acuity and colour perception, whereas cecocentral scotomas are invariably associated with reduced visual acuity and dyschromatopsia. Lesions that damage the posterior aspect of the optic chiasm may also damage one of the optic tracts, thus producing an homonymous field defect that is combined with whatever field defect has occurred from damage to the optic chiasm. Bitemporal homonymous scotomas are important in localizing a lesion. Visual Field Defects Caused by Lesions That Damage the Optic Chiasm after Initially Damaging the Optic Nerve or Optic Tract If there is extension of a lesion from the optic nerve or the optic tract to the optic chiasm, the blind eye usually is on the side of the lesion. When there is extension of a lesion from an optic nerve or optic tract to the optic chiasm, the blind (or nearblind) eye is always on the side of the original lesion, and when there is extension of a lesion from the optic chiasm to the optic nerve or to the optic tract, the blind (or near-blind) eye is always on the side of the extension of the lesion. The degree of visual field loss is usually asymmetrical. Optic atrophy is only present in 50% of cases with visual field defects. For this reason, it is extremely important to perform careful examination of the visual fields in all patients with unexplained visual loss. Compression of the optic chiasm may be symmetrical or asymmetrical relating to the size of lesion and its degree of involvement of the optic chiasm, optic nerve and optic tract. Symmetrical or asymmetrical compression is reflected by the presence of bilateral or unilateral visual field defects. At the junction of the optic nerve and optic chiasm, the crossed and uncrossed retinal nerve fibres are separated; consequently, a small lesion of the optic nerve at this level affecting either the crossed or the uncrossed fibres may give rise to a unilateral hemianopic defect. The involvement of the ipsilateral optic nerve close enough to the optic chiasm (to impair selectively conduction in crossing nasal retinal fibres from the ipsilateral eye, but too anterior to affect the crossing nasal retinal fibres from the contralateral eye) produces monocular temporal hemifield loss. Junctional scotoma: temporal hemianopsic central scotoma associated with deficiency in opposite superior temporal quadrant, situation described by Traquir. Junctional scotoma presents a lesion placed in inside angle, anterior of chiasm. The junction scotoma is met particularly in tumours of the anterior angle of chiasm at the junction between the optic nerve and the chiasm. The suffering of these fibres at the junction between the optic nerve and chiasm, that is the suffering of the „anterior knee”, produces a superior temporal peripherial deficiency, to the opposite eye. The fibres from the nasal inferior quadrant of the retina go through the anterior part of the chiasm, those coming from the superior nasal quadrants go through the posterior side of the chiasm. That is why pituitar tumours produce initially deficiencies in the superior temporal quadrant, and the craniopharyngiomas produce initially deficiencies in the inferior temporal field. Arcuate visual field defects have been proposed to result from vascular changes in the optic nerve rather than at the optic chiasm. Compression of the optic nerve at the anterior optic chiasm level might also explain the presence of an arcuate defect. Trobe (1974) described hemianopic temporal arcuate visual field defects due to a lesion in the anterocentral optic chiasm, where crossing and non-crossing portions of the nerve fibre bundles separate; the lesion would selectively impair crossing fibres. Bitemporal hemianopic central scotomas (heteronimous) are caused by a lesion strictly placed at chiasm, particularly on its posterior edge. The unilateral central scotoma sometimes expresses a compression lesion: tumour of sellar area, meningioma of olfactory ditch. The bilateral central scotoma is mentioned among different types of visual troubles during the optochiasma arachnoid. Hemianopia is a bilateral deficiency of visual field, representing an alteration of the pathways from the optic chiasm up to occipital cortex. With reference to the place of lesion, hemianopic deficiencies present different aspects which have a very important significance if neuropathological diagnosis. Bitemporal hemianopia is met in sagittal lesion of chiasm, in pituitary adenoma, craniopharyngiomas, gliomas of optic chiasm, optochiasmal arahnoid, tubersellar meningiomas, obstructive hydrocephalus with chiasmatic compression by the bottom of the third ventricle, carotid aneurysms situated in sellar, anterior cerebral aneurysms, craniocerebral trauma with chiasm involvement. When we come across a temporal hemianopic deficiency to an eye and blindness to the other, it is difficult to state the chiasmatical origin of the lesion. It is possible that, by means of a big index or by using a candle in an obscure room, we can observe the presence of temporal retinal sensitivity of the atrophy of the eye and the absence of it in the nasal retinal area. Binasal heteronymous hemianopia is the loss of both nasal half fields, corresponding to the lesion of the fibres of temporal half retinas. The lesion focuses on the temporal uncrossed direct bundle at the chiasm level (in lateral lesion of the chiasm). CRANIOPHARYNGIOMA Sometimes hemianopia appears as a result of the compression of the optic pathway by tumour of sellar area (craniopharyngiom).Visual field defects with craniopharyngiomas are frequently asymmetric bitemporal hemianopias or a homonymous pattern with reduced acuity. The craniopharyngiomas will not only cause inferotemporal field defects but also bitemporal hemianopic scotomas. Situations starting with homonim hemianopic central scotomas and paradoxal situations of homonim hemianopic with sparing of the macula are quoted. Figure no. 1. Humphrey perimeter visual field assessment: craniopharyngioma. Bitemporal hemianopia is present with some superior nasal visual field impairment also present bilaterally. AMT, v. II, no. 2, 2012, p. 186 CLINICAL ASPECTS directly above the sella. As the tumour grows upwards it splays GLIOMA AND MENINGIOMA the anterior chiasmal notch and compresses the crossing Meningiomas compressing the junction of the optic inferonasal fibres, causing a defect in the upper visual field. chiasm and optic nerve will interfere with the anterior knee of With further tumour extension, the defect progresses in an Wilbrand. A lesion at this site will therefore give rise to an anticlockwise direction in the left eye and clockwise in the right ipsilateral central scotoma and a contralateral upper temporal eye to involve the lower visual field. field defect (junctional scotoma). For this reason, it is very important to test the visual field of the opposite eye in all patients who present unexplained unilateral visual impairment, Figure no. 3. Humphrey perimeter visual field assessment: particularly including a central visual field defect. pituitary adenoma. There is superior temporal visual field Visual deficits due to meningiomas and gliomas impairment (left greater than right) due to involvement of usually take the form of slowly progressive monocular loss of the inferior retinal nerve fibres first. Note the decibel values vision. When both fields are involved, there is a distinct and probability plots. tendency toward marked asymmetry. HYDROCEPHALUS The optic chiasm is situated in the anteroinferior region of the third ventricle. An enlarged third ventricle due to raised intracranial pressure may press on the superior aspect of the chiasm resulting in a visual deficit of the inferior quadrants initially. Figure no. 2. Humphrey perimeter visual field assessment: hydrocephalus. There is severe impairment of visual field, but particularly loss in the temporal visual field as evident on the pattern deviation plot and corrected pattern standard deviation plot. Note the decibel values for the bitemporal areas of the visual fields. VASCULAR ABNORMALITIES Nasal visual field defects may also be caused by arterial aneurysms. A dilatation of an internal carotid aneurysm may cause lateral compression of the optic chiasm. The field defect is usually unilateral, but may be bilateral with large aneurysms or bilateral carotid aneurysms. 1. 2. 3. MULTIPLE SCLEROSIS This may commence with a central scotoma which progresses to hemianopic scotoma. PITUITARY ADENOMA Bitemporal visual field defects are classically associated with optic chiasm compression. The inferonasal retinal nerve fibres cross low and anteriorly, and therefore are most vulnerable to damage from expanding sellar lesions, typically pituitary adenomas. Compression of the optic chiasm may be asymmetrical, thus causing an asymmetrical visual field defect such that temporal visual field loss is present in one eye but the other eye can have very little involvement. With extensive compression of the optic chiasm, there can be substantial loss of visual field. In approximately 10% of normal subjects, the optic chiasm is situated more anteriorly over the tuberculum sellaeprefixed (Walsh and Hoyt 1982). In this situation, pituitary tumours may compress the optic tract first, resulting in homonymous defects (Trobe1974). Elkington (1968) reported that homonymous hemianopia is uncommon, but is particularly associated with large and extensive tumours. In about 80% of normal subjects, the optic chiasm lies 4. 5. 6. BIBLIOGRAPHY Arseni C, David M, Chiliman M, et al. Neurooftalmologie, Editura Didactică şi Pedagogică. Bucureşti; 1981. p.61-66, p. 154-157, p. 174-177. Biousse V, Newman JN. Neuro-Ophthalmology Illustrated. Thieme. New York; 2009. p. 60-75. Kidd PD, Newman JN, Biousse V. Neuro-Ophthalmology, Butterworth-Heinemann. Oxford; 2008. p. 7-8, p. 243-249. Kline BL, Bajandas JF. Neuro-Ophthalmology. SLACK Incorporated, Torofare, NJ, USA; 2008. p. 10-11. Miller NR, Newman NJ, Biousse V et al. Walsh and Hoyt’s ̉Clinical Neuro-Ophthalmology: The Essentials. Lippincott Williams & Wilkins, Philadelphia; 2008. p. 224227. Rowe F. Visual fields via the visual pathway. Blackwell Publishing, Oxford; 2006. p. 160-177. AMT, v. II, no. 2, 2012, p. 187