* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Evaluation of myocardial ischemia in coronary artery disease with
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
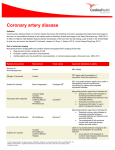
Dextro-Transposition of the great arteries wikipedia , lookup
ORIGINAL ARTICLE Evaluation of myocardial ischemia in coronary artery disease with cardiac MR perfusion method: comparison with the results of catheter or CT angiography Mehmet Sait Doğan1, Erkan Yılmaz2, Sümeyra Doğan3, Bahri Akdeniz4, Nezihi Barış4, Uygar Teomete5, Leyla İyilikçi6 Radiology Clinic, Mardin State Hospital, Mardin, 2Department of Radiology, Dokuz Eylül University School of Medicine, İzmir, 3Radiology Clinic, Mardin Women’s and Children’s Hospital, Mardin, 4Department of Cardiology, Dokuz Eylül University School of Medicine, İzmir, Turkey, 5Department of Radiology, University of Miami Miller School of Medicine, Miami/Florida, USA, 6Department of Anesthesi- 1 ology and Reanimation, Dokuz Eylül University School of Medicine, İzmir, Turkey ABSTRACT Aim To evaluate the eficacy of the Cardiac Magnetic Resonance Perfusion (CMRP) method in detection of Coronary Artery Disease (CAD) by comparing CMRP indings with the results of Coronary Computed Tomography Angiography (CCTA) or Catheter Coronary Angiography (CCA). Corresponding author: Mehmet Sait Doğan Radiology Clinic, Mardin State Hospital, Mardin Nur Mahallesi, Diyarbakır Bulvarı Yan Yolu, 47200, Mardin, Turkey Phone: +90-480-2121048 ; Fax: +90-480-2125865 ; Email: [email protected] Original submission: 21 August 2012; Accepted: 19 September 2012. Methods Thirty one patients in whom CMRP was performed along with CCTA or CCA within a month after CMRP between December 2009 and November 2010 were selected for the study. In CMRP, after adenosine administration as a stress agent Balanced TFE sequences were used to gather dynamic images that include the myocardial irst pass of contrast media. Image analysis was performed visually. CMRP indings were compared to CCTA or CCA results for each coronary artery territories and for all territories. Results Sensitivity, speciicity, accuracy, positive predictive value, and negative predictive value of CMRP test in the identiication of patients with signiicant (≥70%) coronary artery stenosis were 94.7%, 83%, 90.3%, 90%, and 90.9% for all coronary arteries, respectively; 94.4%, 84.6%, 90.3%, 89.4%, and 91.6% for left anterior descending artery, respectively; and 100%, 100%, 100%, 100%, and 100% for circumlex and right coronary artery, respectively. There was no statistically signiicant difference between angiography methods (CCTA/CCA) and CMRP (p>0.05). Methods had good to perfect consistency (ĸ = 0.79-1.00). Conclusion CMRP test seems to be a reasonable alternative for catheter angiography, which is considered the gold standard for evaluation of CAD and exclusion of signiicant coronary artery obstruction. Key words cardiac catheterization, computed tomography, coronary angiography, perfusion magnetic resonance imaging Med Glas Ljek komore Zenicko-doboj kantona 2013; 10(1):63-69 63 Medicinski Glasnik, Volume 10, Number 1, February 2013 INTRODUCTION The major cause of Ischemic Heart Disease (IHD) is reduction of blood low through coronary arteries due to atherosclerosis. Detection of coronary atherosclerosis and evaluation of myocardial hypoperfusion is important for decisions regarding an appropriate and effective therapeutic approach, including catheter based interventions or surgical options (1). Myocardial perfusion, deined as blood volume lowing through a given myocardial area in a determined time, is one of the irst steps of the ischemic cascade and may be detected prior to electrocardiogram (ECG) alterations, clinical symptoms, or myocardial wall motion abnormalities (2). The most common clinical method performed for detecting perfusion abnormalities is single photon emission computerized tomography (SPECT) (2). The validity of this method is evident in a number of multi-center trials, however, low spatial and temporal resolution, exposure to ionising radiation, and attenuation artifacts are its signiicant limitations (2). In contrast, stress Cardiac Magnetic Resonance Perfusion (CMRP) does not emit ionising radiation, has high spatial and temporal resolution, is able to evaluate subendocardial perfusion, and is a non-invasive modality; therefore it is the preferred method for myocardial perfusion evaluation (2,3). In 2006, a consensus panel from the American College of Cardiology Foundation (ACCF) deemed the following indications as appropriate uses of stress perfusion MRI: evaluating chest pain syndromes in patients who have intermediate probability of coronary artery disease (CAD) and ascertaining the physiologic signiicance of indeterminate coronary artery lesions (4). Recent studies have shown that stress CMRP has high sensitivity and speciicity for IHD diagnosis, and negative stress CMRP was considered a perfect test for ruling out a major cardiac event (2,3,5). In light of this information, the present study aims to compare the indings of CMRP with the results of CCTA or CCA and to evaluate the eficacy of CMRP in detection of CAD. PATIENTS AND METHODS Patients Thirty one patients were selected at the Department of Radiology, Dokuz Eylül University Hospital between December 2009 and November 64 2010 in whom CMRP, as well as CCA or CCTA, were performed within one month after CMRP. All patients were investigated for the criteria that are contraindicated for the Magnetic Resonance Imaging (MRI) including claustrophobia, cardiac pacemaker, and inappropriate surgical and prosthetic materials for MRI. Perfusion MRI was performed after 12-hour fasting. For maximum response to vasodilatory effect of adenosine, if patients were using calcium channel blockers, beta-blockers and nitrates these were discontinued 24 hours before the procedure. Also consumption of foods and beverages containing caffeine was discontinued 12 hours prior to the procedure. Patients with conditions that are contraindicated for adenosine administration including signiicant valvular stenosis, unstable angina, obstructive pulmonary disease, severe arterial hypertension, and history of myocardial infarction within 3 days prior to the procedure were excluded. An anesthesia team was ready during the procedure in order to address any potential adverse effects of adenosine. All patients provided written informed consents before the procedure. This retrospective study was approved by the Ethics Committee of Dokuz Eylül University School of Medicine. Cardiac MR perfusion techniques Although the present study was retrospective, the standard sequences of adenosine-stress CMRP imaging were used in each patient. Cardiac Magnetic Resonance Perfusion imaging was performed with 1.5 Tesla MRI device (Philips Intera Achieva; Philips Medical Systems, Holland) with ECG, respiratory pad and 5-phased array cardiac coil that was applied to the anterior chest of the patient in the supine position. In stress perfusion imaging, 140 microgram/kg/ min dosing of adenosine was administered for 4 minutes via IV infusion as a vasodilator (Adenosin-L.M., Apoteket AB, Sweden). At the end of the 4th minute, 0.08 mmol/kg gadobutrol (Gadovist, Bayer Schering, Germany) followed by 20-50 ml saline (4-5 ml/sec) IV bolus was administered. In the mean time, through the short axis perpendicular to the long axis of left ventricle, 3-4 slices with slice thickness of 10 mm and interval of 10 mm from the left ventricle basal, midventricular layer, and apex were displayed at each heart beat. From these slices, 60 heart beat long dynamic images were gathered that included myocardial irst pass of con- Doğan et al. MR perfusion in coronary artery disease trast media with Balanced Turbo Field Echo (TFE) sequence. Imaging parameters for Balanced TFE sequences were as follows TR: 2.4 msec; TE: 1.2 msec, Flip Angle: 50 degrees, FOV: 350-400 mm; matrix: 128x256, Sense factor: 2, Slice width: 10 mm and Slice Interval: 10 mm. For higher quality images, patients were asked to hold breath at the end of the expirium during dynamic assessment. In rest perfusion imaging, after waiting 10 minutes for clearance of gadolinium from the blood pool, dynamic images were taken with the same parameters that were used before without adenosine infusion. During this 10-minute waiting period, dynamic images including the entire left ventricle through the short axis with Steady-state Free Precession (SSFP) sequence were taken (functional imaging). The myocardial perfusion MRI protocol used in our study is summarized in Figure 1. Image analysis For each coronary artery territory, CMRP indings were evaluated retrospectively by two radiologists separately (one of them was experienced on cardiac imaging) and they were blinded to the results of CCTA and CCA assessment of perfusion defect. Perfusion defect is deined as hypointense subendocardial regions in comparison with the normal myocardium at early myocardial signal enhancement. If discordance occurred in the results, the radiologists re-examined the indings and reached a consensus. Then, CMRP results were compared to that of angiography techniques (CCTA or CCA). Obstructions of 70% or greater detected at angiography were considered positive for signiicant stenosis. between analyses. For the Kappa test, ≤ 0.20, 0.21 - 0.40, 0.41 - 0.60, 0.61 - 0.80 and 0.81 - 1.00 values were considered bad, weak, moderate, good and perfect harmonization, respectively. RESULTS Twenty ive of 31 patients were males (80.6%) and six of 31 (19.4%) were females (age range, 22-88 years). All patients had chest pain. The interval between CMRP imaging and angiography methods varied 0 to 18 days (mean 4.2 days). Two patients had a history of coronary artery bypass surgery, nine had coronary artery stents. Five patients with stent had obstruction or occlusion. Figure 1. Illustration of study protocol A total of 93 coronary artery territories consisting of left anterior descending artery (LAD), circumlex artery (Cx) and right coronary artery (RCA) territories were evaluated and it was revealed that 32 of these included perfusion defects. Twenty of 31 patients had perfusion defect in at least one of the coronary artery territories. Five patients had perfusion defects at all three LAD, Cx and RCA territories (Figure 2), one patient A) B) C) D) E) F) Statistical analysis Cardiac Magnetic Resonance Perfusion imaging results of 31 patients were compared to those of angiography (CCTA or CCA) according to the coronary artery territories. Angiography indings were considered as gold standard, and then CMRP indings were compared to angiography with respect to perfusion defects for each case and also each coronary artery perfusion territory. Then sensitivity, speciicity, accuracy, positive predictive value and negative predictive value were calculated. Analysis of diagnostic differences for all comparisons mentioned above was performed using the McNemar test. P<0.05 value was considered signiicant for the McNemar test. The Kappa test was used for harmonization G) H) Figure 2. A) wide perfusion defects at each of three coronary artery territories of the left ventricle (stress-CMRP test images,) A-C) no perfusion defect was detected in rest perfusion images, D-F), an obstruction of 95% at Cx artery (long arrow) and occlusions at LAD artery (short arrow) and G,H) at RCA (thick arrow) (CCA) 65 Medicinski Glasnik, Volume 10, Number 1, February 2013 A) B) C) D) had perfusion defects at LAD and RCA territories, one had perfusion defects at LAD and CX territories. One patient had a perfusion defect at the Cx artery territory and the remainder (12 patients) had perfusion defect at LAD artery territory (Figures 3, 4). Angiography studies (CCTA or CCA) revealed that 18 of 20 patients with perfusion defects had 70% or greater obstruction in at least one of the three coronary arteries (LAD, Cx or RCA) or their branches. One patient had no coronary artery obstruction in CCA, the other patient had no coronary artery obstruction in CCTA, however, there was myocardial bridging at the middle segment of LAD artery (Figure 4). During the evaluation of both coronary arteries and perfusion territories, angiography detected signiicant luminal narrowing (≥70%) or occlusion in LAD arteries of 17 of 19 patients who had perfusion defect in LAD artery territory, and in all RCA and/or Cx arteries who had a perfusion defect in RCA and/or Cx artery territories. Stenosis of 90% was detected at the D1 branch of LAD artery in one of 11 patients who did not have perB) 66 Figure 5. Normal findings in stress-cardiac MR perfusion study (A-D) in a patient, with obstructive CAD. There was no perfusion defect at short axis views obtained from the apex of left ventricule (A) to the basal layer (D). CCA (E) revealed a high-grade (90%) stenosis of the diagonal 1 branch of LAD artery (It was also reported as a thin vessel at CCA). fusion defects (Figure 5). In this case, stenosis of 60% at the distal LAD artery and 30% obstruction at the RCA were also observed. No signiicant stenosis (≥70%) was detected in the coronary arteries of 10 patients who did not have perfusion defect. Similarly, coronary arteries associated with normal perfusion areas of the patients with perfusion defect were not signiicantly narrowed. Only ive patients had stenosis with up to 50% obstruction in coronary arteries or branches. The overall sensitivity, speciicity, accuracy, positive predictive value and negative predictive value of CMRP imaging in detecting signiicant coronary artery stenosis (≥70%) at angiography were 94.7%, 83%, 90.3%, 90% and 90.9%, respectively. There was no statistical difference between the two methods (p>0.05). Harmonization between the two groups was “good” (ĸ=0.79). When evaluating each separate coronary artery territory; sensitivity, speciicity, accuracy, positive Table 1. Sensitivity, specificity, accuracy, positive predictive value and negative predictive value of Cardiac MR perfusion test in detecting significant (70% or greater) obstruction at CCA-CCTA Diagnostic Sensi- Speci- Accu- Positive Negative difference Consitivity icity racy predictive predictive between stency (%) (%) (%) value (%) value (%) methods C) Figure 4. In stress perfusion test (A), short axis image through left ventricular basal layer showed hypointensitiy at anteroseptal wall in concordance with subendocardial perfusion defect, whereas, there was no perfusion defect at the same level at rest perfusion image (B). In CCTA (C), no stenosis was detected in coronary arteries. However, it was revealed that there was myocardial bridging at the middle segment of LAD artery (arrow). E) D) C) Figure 3. In stress perfusion test, short axis images obtained from apical (A) and midventricular (B) layer of the left ventricule showed hypointensities at inferoseptal wall in concordance with perfusion defects, whereas, there was no perfusion defect at the same levels at rest perfusion images (C,D). In CCA (E), RCA was reported to be non-dominant and an obstruction of 80% at the origin of diagonal 1 branch of LAD artery was detected (arrow). Because of non-dominant RCA, perfusion defects at inferoseptal wall were thought to be at LAD artery territory and to be associated with the obstruction of LAD artery A) B) A) E) LAD AT 94.4 84.6 90.3 89.4 91.6 none good CX AT 100 100 100 100 100 none perfect RCA AT 100 100 100 100 100 none perfect All ATs 94.7 83 90.3 90 90.9 none good CCA, catheter coronary angiography; CCTA, coronary computed tomography angiography; LAD, left anterior descending artery; CX, circumlex artery; RCA, right coronary artery; AT, artery territory. Doğan et al. MR perfusion in coronary artery disease and negative predictive value of CMRP imaging for detecting signiicant obstruction in associated coronary artery indicated at angiography (CCTA or CCA) were 94.4%, 84.6%, 90.3%, 89,4% and 91.6% respectively for LAD; 100%, 100%, 100%, 100% and 100% respectively for Cx; and 100%, 100%, 100%, 100% and 100% respectively for RCA. There was no diagnostic difference between methods (p>0.05). Harmonization of two methods resulted in ĸ values of 0.80, 1.00 and 1.00 for LAD artery, Cx and RCA territories, respectively and harmonization was “good”, “perfect” and “perfect”, respectively (Table 1). DISCUSSION This study evaluates the eficacy of CMRP imaging in detecting CAD in comparison to CCTA or CCA results, revealing high sensitivity and speciicity. This is the irst adenosine-stress CMRP study on this subject in Turkey. Hamon et al. (6) completed a meta-analysis of articles that had been published up to July 2009. This analysis included 20 trials and a total of 1678 patients in whom CMRP imaging was performed with adenosine as the pharmacological stress agent and another 5 trials with a total of 417 patients in whom dipiridamol was used as the pharmacologic stress agent in CMRP imaging. Sensitivity and speciicity for detecting CAD were 90% and 81% respectively in the irst group and 86% and 76% respectively in the latter. We used adenosine as the stress agent and found both high sensitivity (94.7%) and high speciicity (83%). Semi-quantitative analysis requires additional time; it is not appropriate for daily practice and there is no consensus in post-processing protocol. Therefore, we preferred the visual method. It is stated that as a stress test, CMRP imaging should be avoided in patients with signiicant valvular stenosis, unstable angina, obstructive pulmonary disease, recent myocardial infarction, and severe arterial hypertension because of the hemodynamic disruption and possible side effects of adenosine (7), whereas, Greenwood et al (8) suggest that adenosine-stress CMRP imaging is a safe method in early after ST elevated myocardial infarction (STEMI) patients. In our study, the patients in whom adenosine usage may be hazardous were excluded from MRI perfusion examination. Plein et al. (9) evaluated cardiac MRI tests that include 4 parameters: perfusion imaging, myocardial function, late enhancement, and coronary artery anatomy. In this study, CMRP imaging itself is suficient for detecting coronary artery stenosis with high sensitivity and speciicity (88% and 83%, respectively). But in cases of equivocal results or cases with insuficient evaluation resulting from artifacts (motion artifact, respiratory artifact, ring artifact) other cardiac MRI methods may be combined to increase sensitivity. Klem et al. (10,11) stated that the combination of CMRP imaging with late enhancement would increase speciicity and accuracy. Moreover, according to the results of another study this combination did not seem to affect sensitivity and speciicity. (12). We evaluate only the eficacy of CMRP in detecting signiicant coronary artery stenosis at angiography and found high sensitivity, speciicity and accuracy. These results are similar to that of literature, with the exception of the studies by Klem et al. (10,11). Merkle et al. (13) stated that CMRP imaging had low positive predictive value (59%) in the primary diagnosis of CAD. They thought that the higher rate of risk factors in these patients supported the idea that those patients more frequently had non-vascular conditions like hypertensive heart disease, syndrome X, or coronary endothelial dysfunction, which might be the cause of false positive results and ischemic pain. Burgstahler et al. (14) found severe myocardial hypertrophy in 2 patients with false positivity. Hamon et al. (6) stated that the reason for higher sensitivity than speciicity was the high rate of false positives. We also found that sensitivity was higher than speciicity. Our two cases had MR perfusion defects in the LAD artery territory, but there were no signiicant coronary artery stenosis. One had LIMALAD and AO-OM-SVG bypass grafts with patent vascular lumen and suficient low on CCA. In this case, perfusion defect is considered to be due to microvascular disease or persistent microvascular obstruction. The other case was not observed to have signiicant coronary artery stenosis in CCTA, however, there was myocardial bridging at the middle segment of LAD artery and this is thought to explain the perfusion defect. Cheng et al. (15) reported that 3 T CMRP imaging was superior to 1,5 T CMRP imaging. Meyer et 67 Medicinski Glasnik, Volume 10, Number 1, February 2013 al. (16) used 3 T MR device and performed adenosine-stress CMRP test. When they compared the results to those in the literature at 1.5 T based on a visual analysis, they found that their protocol was at least as eficacious as those at 1.5 T. Our results are similar to the study by Meyer et al. with 3 T MR Devices. Merkle et al. (13) found that the sensitivity of CMRP imaging for diagnosis of coronary artery stenosis was higher in LAD artery territory than that of Cx and RCA territories. They stated that a possible explanation might be the use of surface coil leading to lower signal intensities at lateral and inferior segments in especially obese population. In our study, we evaluated eficacy of CMPR method for detection of signiicant coronary artery stenosis in each coronary artery territory separately. Sensitivity, speciicity, and accuracy were higher than the values in literature. These higher values, especially for Cx artery and RCA territories, are thought to be due to fewer perfusion defects in these territories in comparison to LAD artery territory, and relatively low number of patients with Cx artery and RCA obstruction. In our study, one of the patients without perfusion defects in CMRP imaging had an obstruction of 90% at D1 branch of LAD in CCA and it was noted as a thin vessel (Fig. 5). Lack of perfusion defect in this patient may be explained because of thin structure of obstructed artery and possible collateral blood low. One of the major limitations of our study is that we did not compare the CMRP method with an accepted test for evaluating perfusion defects such as SPECT. Another limitation was the use of angiography methods for comparison in a perfusion study. CCA is the standard diagnostic method for detecting signiicant coronary artery obstruction in daily practice. However, it is not appropriate to evaluate the hemodynamic signiicance of coronary artery obstruction and the functional signiicance of obstruction is more important than morphological obstruction in the prognosis of CAD. The invasive gold standard method in detecting functional signiicance of obstruction is measurement of pressure dependent fractional low reserve (FFR) (17). Rieber et al. (18) compared CMRP imaging to CCA and FFR in accordance 68 with detecting functional status of CAD and found a strong correlation between CMRP method and FFR measurement. FFR was not measured in patients included in our retrospective study. We considered angiography as the reference method, similar to most studies in the literature. Another limitation of our study was the absence of a single angiography method. Coronary artery evaluation was performed with CCA in 21 patients and CCTA in 10 patients in our study. However, recent advances in CCTA with the development of Multi-Detector Computed Tomography technology provide high sensitivity, speciicity, and accuracy for detection of CAD (19). Because of its high negative predictive value, we used CCTA as an alternative method to catheter angiography, especially in patients without perfusion defects. Small study sample and retrospective design are two additional factors that decrease statistical power. Further prospective studies with larger sample size are needed. Cardiac MR Perfusion test has high sensitivity and speciicity in detecting signiicant coronary artery stenosis when compared to catheter coronary angiography. We used adenosine as a pharmacologic stress agent in this technique. Sensitivity, speciicity, accuracy, positive predictive value, and negative predictive value in detecting 70% or greater obstructions of coronary arteries in catheter coronary angiography or coronary CT angiography were high, similar to literature. There was no signiicant diagnostic difference between these methods and the harmonization was good-to-perfect. In conclusion, cardiac MR perfusion test seems to be a reasonable alternative for catheter angiography, which is considered the gold standard for evaluation of CAD and exclusion of signiicant coronary artery obstruction. We suggest that as a non-invasive method, CMRP imaging could be used more commonly in clinical practice in order to decrease the use of invasive procedures like catheter angiography. FUNDING No speciic funding was received for this study. TRANSPARENCY DECLARATIONS Competing interests: none to declare. Doğan et al. MR perfusion in coronary artery disease REFERENCES 1. Silber S, Richartz BM. Impact of both cardiac-CT and cardiac-MR on the assessment of coronary risk. Z Kardiol 2005; 94:70-80. 2. Janssen CHC, Kuijpers D, Oudkerk M. MR Perfusion imaging for the detection of myocardial ischemia. Imaging Decisions 2004; 8:13–7. 3. Kim HW, Klem I, Kim RJ. Detection of Myocardial Ischemia by Stress Perfusion Cardiovascular Magnetic Resonance. Cardiol Clin 2007; 25:57-70. 4. Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC, Gerstad NA, Gillam LD, Hodgson JM, Kim RJ, Kramer CM, Lesser JR, Martin ET, Messer JV, Redberg RF, Rubin GD, Rumsfeld JS, Taylor AJ, Weigold WG, Woodard PK, Brindis RG, Hendel RC, Douglas PS, Peterson ED, Wolk MJ, Allen JM, Patel MR; American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group; American College of Radiology; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; American Society of Nuclear Cardiology; North American Society for Cardiac Imaging; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology. Appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group. J AmColl Cardiol 2006; 48:1475–1497. 5. Nagel E. Magnetic resonance perfusion imaging for detection of ischemic heart disease. Heart Metab 2008; 38:19–21. 6. Hamon M, Fau G, Née G, Ehtisham J, Morello R, Hamon M. Meta-analysis of the diagnostic performance of stres perfusion cardiovascular magnetic resonance for detection of coronary artery disease. J Cardiovasc Magn Reson 2010; 12:29. 7. Prasad SK, Lyne J, Chai P, Gatehouse P. Role of cardiac magnetic resonance in assessment of myocardial perfusion. Eur Radiol 2005; 15:B42-47. 8. Greenwood JP, Younger JF, Ridgway JP, Sivananthan MU, Ball SG, Plein S. Safety and diagnostic accuracy of stress cardiac magnetic resonance imaging vs exercise tolerance testing early after acute ST elevation myocardial infarction. Heart 2007; 93:1363-8. 9. Plein S, Greewood JP, Ridgway JP, Cranny G, Ball SG, Sivananthan MU. Assessment of non-ST-segment elevation acute coronary syndromes with cardiac magnetic resonance imaging. J Am Coll Cardiol 2004; 44:2173-81. 10. Klem I, Heitner JF, Shah DJ, Sketch MH Jr, Behar V, Weinsaft J, Cawley P, Parker M, Elliott M, Judd RM, Kim RJ. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging. J Am Coll Cardiol 2006; 47:1630-8. 11. Klem I, Greulich S, Heitner JF, Kim H, Vogelsberg H, Kispert EM, Ambati SR, Bruch C, Parker M, Judd RM, Kim RJ, Sechtem U. Value of cardiovascular magnetic resonance stress perfusion testing for the detection of coronary artery disease in women. J Am Coll Cardiol Img 2008; 1:436-45. 12. Klein C, Gebker R, Kokocinski T, Dreysse S, Schnackenburg B, Fleck E, Nagel E. Combined magnetic resonance coronary artery imaging, myocardial perfusion and late gadolinium enhancement in patients with suspected coronary artery disease. J Cardiovasc Magn Reson 2008; 10:45. 13. Merkle N, Wöhrle J, Grebe O, Nusser T, Kunze M, Kestler HA, Kochs M, Hombach V. Assessment of myocardial perfusion for detection of coronary artery stenoses by steady-state, free-precession magnetic resonance irst-pass imaging. Heart 2007; 93:13815. 14. Burgstahler C, Kunze M, Gawaz MP, Rasche V, Wöhrle J, Hombach V, Merkle N. Adenosine stress irst pass perfusion for the detection of coronary artery disease in patients with aortic stenosis: a feasibility study. Int J Cardiovasc Imaging 2008; 24:195200. 15. Cheng AS, Pegg TJ, Karamitsos TD, Searle N, Jerosch-Herold M, Choudhury RP, Banning AP, Neubauer S, Robson MD, Selvanayagam JB. Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol 2007; 49:2440-9. 16. Meyer C, Strach K, Thomas D, Litt H, Nähle CP, Tiemann K, Schwenger U, Schild HH, Sommer T. High-resolution myocardial stress perfusion at 3 T in patients with suspected coronary artery disease. Eur Radiol 2008; 18:226-33. 17. Pijls NH, Klauss V, Siebert U, Powers E, Takazawa K, Fearon WF, Escaned J, Tsurumi Y, Akasaka T, Samady H, De Bruyne B; Fractional Flow Reserve (FFR) Post-Stent Registry Investigators. Coronary pressure measurement after stenting predicts adverse events at follow-up: a multicenter registry. Circulation 2002; 105:2950–4. 18. Rieber J, Huber A, Erhard I, Mueller S, Schweyer M, Koenig A, Schiele TM, Theisen K, Siebert U, Schoenberg SO, Reiser M, Klauss V. Cardiac magnetic resonance perfusion imaging for the functional assesment of coronary artery disease: a comparison with coronary angiography and fractional low reserve. European Heart Journal 2006; 27:1465-71. 19. Herzog C, Zwerner P, Doll JR, Nielsen CD, Nguyen SA, Savino G, Vogl TJ, Costello P, Schoepf UJ. Signiicant coronary artery stenosis: comparison on per-patient and per-vessel or per-segment basis at 64-section CT angiography. Radiology 2007; 244:112-20. 69