* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Teitelbaum Science 2000 MULTIPLE MYELOMA: Clinical Picture
Behçet's disease wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Osteochondritis dissecans wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
IgA nephropathy wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
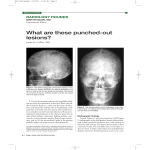
Multiple Myeloma By Dr Sameh Shamaa Multiple Myeloma Epidemiology: • 1% Of all malignant diseases. • Annual incidence: 3-4/100 000. • Age: - Median age: 65y. - The diagnosis of MM in a patient < 30y should only be made after careful evaluation of all data. OC precursor OAF receptor (RANK) OSTEOCLAST ACTIVATION OPG/OCIF Osteoclast RANKL/OAF Osteoblast/ stromal cell /tumour cells/ myeloma Teitelbaum Science 2000 MULTIPLE MYELOMA: Clinical Picture MM Monoclonal Protein Renal Failure Hyperviscosity Marrow Infiltration Amyloidosis Anaemia Immune Deficiency Release of Cytokines Infections LL 6 Bone Destruction Bone Pains Hypercalcaemia Bone Marrow Failure: *Anemia:usually normocytic normochromic :due to marrow infiltration and plasma volume expansion. *Neutropenia is frequent(++ susceptibility to infection). *Thrombocytopenia is rare. Bone Disease: Skeletal lytic lesions,with or without osteoperosis,wedging or collapse of vertebral bodies or pathological fractures. Renal Failure: In 20-40% of cases,due to: -BJP,and/0r hypercalcemia (in 95% of cases). -Other causes: hyperuricemia,hypeviscosity,sepsis& nephrotoxic drugs. Hypercalcemia: Secondary to osteolysis----->polyurea,and polydypsia may lead to severe dehydration Hyperviscosity: usually associated with IgM M-protein----ocular,hemostatic,and neurological disturbances. Coagulopathy: either: -Hemorrhage: due to interference with action of clotting factors and platelets. -Thrombosis: due to acquired protein C deficiency. Immune Paresis: -In 70% of patients with IgG MM, 40% of IgA MM and 20% of acses with BJP MM but cell mediated immunity is intact. So----- incresed risk of bacterial sepsis. Amyloidosis: In less than 5% of MM cases: more common with BJP and IgA MM-- deposition of amyloid material--congesive heart failure, Carpal tunnel syndrome, macroglossia, gastrointestinal disturbances and europathies., renal amyloidosis. MULTIPLE MYELOMA : Lab investigation •ESR: very high. •Serum protein electrophoresis: M-band. •Immunofixation or immunoelectrophoresis: are confirmatory studies to define M-protein heavy and light chain classes. MULTIPLE MYELOMA : Lab investigation •Serum Ca: often . •Serum creatinine: often . •Anaemia (not obligatory): (rouleaux formation of RBCs). • In uninvolved immunoglobulins. • +BJP in 24 hr urine collection (monoclonal light chains). MULTIPLE MYELOMA BM PICTURE: (Aspirate & Trephine Biopsy) • >10 % myeloma cells.. • More basophilic cytoplasm. • Increased mitotic figures or multiple nuclei. • Coarse chromatin. • Plasma cell nests. MULTIPLE MYELOMA Immunophenotyping: • CD 38 +ve. • CD 19, 20, 22 -ve. • Intracytoplasmic Ig +ve. • sIg -ve. MULTIPLE MYELOMA RADIODIAGNOSIS: •Radiological survey of the entire skeleton: is mandatory. •MRI: is superior to CT for screening the vertebral column for osteolytic lesions. •Bone scan: is not indicated (cold lesions). •REMEMBER!! Iodine-containing contrast media may cause acute renal failure in case of paraproteinaemia. MM: SWOG Criteria for Diagnosis: (At least 1 major + 1 minor or 3 minors) Major Criteria: (1) Plasmacytoma on tissue biopsy (2) Marrow plasmacytosis > 30 %. (3) Monoclonal protein: Ig G > 3.5 g / dl. Minor Criteria: Ig A > 2 g / dl. BJP > 1 g / 24 hr. (1) Marrow plasmacytosis 10-29 %. (2) Monoclonal protein present but less than the above levels (3) Lytic bone lesions (4) Decrease in uninvolved Ig: Ig M < 50 mg / dl. Ig A < 100 mg / dl. Ig G < 600 mg / dl. MULTIPLE MYELOMA Prognostic Factors (1) Staging (2) -2 microglobulin most significant) (3) CRP (reflect IL-6 activity) (4) PCLI (5) Cytogenetics (6) LDH MM: Prognostic Factors Risk Group 2M & CRP Level M.S. (mg/l) (mo) Low-risk Both <6 54 Intermediate 2M <6 27 High-risk Both >6 6 or CRP MM: Prognostic Factors Cytogenetics: • Cytogenetics abnormalities occur in 80-90% of patients. • FISH is the best technique to discover them. • Del 13 (partial or complete) & t involving 11q are associated with poor prognosis in ABMT patients only. • Hypodiploidy is associated with drug resistance. • Any abnormal karyotype leads to inferior outcome with standard therapy. MM Treatment Options • • • • • Chemotherapy High dose-therapy with transplant Radiation Maintenance therapy (e.g. alpha interferon, prednisone) Supportive care for – Anaemia – Pain – Bone disease (Bisphosphonates) – Hypercalcemia – Antibiotics – Emergency care (e.g. dialysis, plasmapheresis, surgery) • Management of drug-resistant or refractory disease • New and emerging treatments Treatment of MM Use of Bisphosphonate in MM: Mechanism of action: 1. Decrease IL-6 release 2. Direct effect on Myeloma (may slow tumor growth) 3. Effect of angiogenesis Treatment of MM Radiotherapy: Indications: • Big osteolytic lesions. • Significant osteolytic lesions in weight-bearing bone (for fear of pathological fracture). • Cord compression. • Extramedullary plasmacytoma. TREATMENT PLAN IN MM Patients < 60 yrs of Age 3 courses of VAD CR PR HLA-Typing Another 3 courses of VAD No HLA-Identical Sibling HLA-Identical Sibling ABMT Mini-Transplant CR TREATMENT PLAN IN MM Patients > 60 yrs Asymptomatic Symptomatic or PD No treatment MP till CR or Max. Response Progression < 6 months Progression >6 months VAD Repeat MP PD PD 2nd line VAD Survival of Multiple Myeloma patients • • • • • • • No treatment: 3-6 months Conventional chemotherapy: 3 years Chemotherapy + IFN-α: 3 years ± 6 months Auto transplant: 5 years 25% dies within 1st year 25% survival 8 years No cure by conventional chemotherapy