* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File - Kamilan Aurielle Lowery
Survey
Document related concepts
Transcript
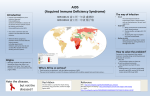
HIV/AIDS and Nutrition Source: http://hiv.health.gov.tt/ Ali Aziz, Aurielle Lowery, Sarah Vacher, Tessa Englund, and Xiaolu Hou Objectives ■ Examine HIV’s history, etiology, & effects on the human body ■ Explain the impact of HIV on nutritional status & vice versa ■ Discuss nutrition assessment methods for an HIV patient ■ Identify nutrition diagnoses for the case patient & other common diagnoses for HIV/AIDS patients ■ Identify nutrition interventions for HIV/AIDS patients ■ Discuss common goals/outcomes as well as time frames for nutrition monitoring & evaluation ■ Use a male case patient with AIDS-Stage 3 with oral thrush to facilitate more detailed exploration of the topics above Case Patient T.L. ■ 32-year-old African American male, 6’1”, 151# CBW, and 160165# UBW ■ HIV diagnosed 4 years ago but had never been treated for it PTA ■ Admitted with very sore mouth/ throat, likely PNA & progression to AIDS, mild malnutrition, & 8.5% weight loss compared to UBW. ■ Diagnosis of AIDS-Stage 3 with thrush & no clinical evidence of PNA. HAART initiated with Atripla. Sources: http://remediesforthrush.blogspot.com/2013/09/oral-thrush-infection-and-solution.html http://recommendpills.com/candidiasis-symptoms-and-treatment/04/11/2012/ HIV/AIDS and Nutritional Status Epidemiology and Trends ◻ The first cases of AIDS were described in 1981. Soon after, HIV was identified as leading to AIDS. ◻ At the end of 2008 an estimated 33.4 million people lived with either AIDS or HIV. Acquired immune deficiency syndrome (AIDS) is caused by Human Immunodeficiency virus (HIV) . HIV affects the body’s ability to fight off infection and disease. Nutritional status plays an important role in maintaining a healthy immune system. HIV Transmission • HIV is transmitted via direct contact with infected fluids – Blood, semen, pre-seminal fluid, vaginal fluid, breast milk – Cerebrospinal fluid, synovial fluid, amniotic fluid • Sexual transmission is most common • Saliva, tears, and urine do NOT contain enough HIV for transmission Source: http://www.prideglv.org/how-do-you-get-hiv/ HIV-1 vs HIV-2 • HIV-1 infection is what we are referring to unless specified otherwise • HIV-2 is endemic in West Africa – Lower viral loads, longer asymptomatic period, lower mortality rates than HIV-1 – Rarely seen outside of Africa or areas with strong ties to affected areas in Africa Sources: http://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv-guidelines/24/hiv-2infection Stages of HIV Infection • HIV progresses through four clinical stages – – – – Acute HIV infection Clinical Latency Symptomatic HIV infection* Progression of HIV to AIDS* • Two main biomarkers to assess disease progression – HIV RNA (viral load) – CD4 (T-helper cell) count 1: Acute HIV Infection • Time from transmission of HIV to the host until production of detectable antibodies – This is called seroconversion • Non-specific clinical features and very short diagnostic window – Acute HIV infection is rarely discovered 2: Clinical Latency • Also called asymptomatic HIV infection • Further evidence of illness might not show for as long as 10 years post-infection • Virus is active and replicating at a slow rate • Long-term non-progression – Here CD4 count levels remain WNL and viral loads can be undetectable for years – Not everyone experiences clinical latency for so long 3: Symptomatic HIV infection • Over time HIV breaks down the immune system and the body is incapable of fighting off the virus • Here CD4 counts fall below 500 cells/mm3 • Pt likely to develop s/s – Persistent fevers, chronic diarrhea, unexplained weight loss, recurrent fungal or bacterial infections 4: Progression of HIV to AIDS • Immunodeficiency continues to worsen and CD4 counts fall lower • Increased risk of opportunistic infections (OIs) • CDC defines AIDS as: – Lab confirmation of HIV infection in person with a CD4+ count below 200 cells/mm3 (or less than 14%) – Documentation of an AIDS-defining condition • Krause, pg 866, Box 38-1 Case Study Patient Pt believes HIV has progressed to AIDS because he is experiencing: ● exhaustion ● sore mouth and throat (thrush) ● unintended weight loss ● possible pneumonia diagnosis Source: http://www.cell.com/cms/attachment/531402/3640755/gr2.jpg Opportunistic Infections ● Candidiasis of bronchi, trachea, esophagus, or lungs infection caused by yeast (commonly known as thrush) ● Cryptococcosis - parasitic infection in small intestine ● Cryptosporidiosis - chronic intestinal infection (greater than 1 month's duration) ● Tuberculosis - bacterial lung infection ● Pneumonia, recurrent ⬜ PCP - form of PNA caused by fungus These typically present themselves during Source: Mahan LK, Escott-Stump S, Raymond JL. Krause's Food & the Nutrition Care Process. 13th ed. St. Louis, MO: Saunders; 2012. Other Common Complications AIDS-Defining Conditions HALS - HIV-associated lipodystrophy syndrome Wasting - unintentional weight loss Obesity Kaposi’s sarcoma - cancerous connective tissue tumor (pictured) Lymphoma - blood cell tumors HIV encephalopathy - neurodegenerative disorders (also called HIV-associated dementia) Chronic liver disease Source: http://www.dermis.net/dermisroot/en/1270069/image.htm Impact on Nutritional Status ■ Vitamin and mineral deficiencies are common ■ Resultant of: ⬜ malabsorption ⬜ drug-nutrient interactions ⬜ altered metabolism ⬜ altered gut & gut barrier function ■ Commonly low: Vitamin A, zinc, and selenium Impact on Nutritional Status ■ Low levels of vitamin A, vitamin B12, and zinc are associated with faster disease progression ■ Higher intakes of vitamins B and C have been associated with increased CD4 counts and slower disease progression ■ No evidence that megadosing is helpful Case Study Patient - Vitamins Pt diet should be assessed to ensure that he is receiving DRI’s, especially for: ➢ ➢ ➢ ➢ ➢ ➢ ➢ Vitamin B12 Vitamin A Vitamin E Vitamin D Selenium Zinc Iron Because pt is a “picky eater” and has mouth sores that make eating uncomfortable, RD needs to work with him to get adequate nutrients while being sensitive to preferences/pain. CD4 Count ■ Indicator of immune function & stage of HIV infection ■ Used to determine whether to initiate antiretroviral therapy (ART), which suppresses viral loads to increase quality of life and reduce M&M Case patient has low T-helper cell counts (CD4) indicating immune suppression and progression to AIDS. Source: Treatment Types: HAART HAART = Highly Active Antiretroviral Therapy (also commonly referred to as ART) Goals: ● Reach and maintain viral suppression ● Reduce HIV related M & M ● Increase quality of life ● Gain and maintain immune function Classes of Antiretroviral Drugs ■ Nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs) ■ Nonnucleoside reverse transcriptase inhibitors (NNRTIs) ■ Protease inhibitors (PIs) ■ Fusion inhibitors ■ CCR5 (chemokine receptor 5) antagonists ■ Integrase strand transfer inhibitors (INSTIs) Most common treatment is the combination of NRTIs + NNRTI or PI Predictors of Adherence ■ Patients must have the ability and commitment to a lifelong treatment ■ Understanding of the pros and cons of therapy and importance of adherence ■ Barriers include: ⬜ ⬜ ⬜ ⬜ ⬜ homelessness low literacy level depression dementia/psychosis illicit drug use ART Side Effects ART medications commonly cause the following side effects: ■ ■ ■ ■ ■ ■ ■ diarrhea fatigue gastroesophageal reflux nausea vomiting dyslipidemia insulin resistance Many ART drugs must be taken on a strict schedule, with or without food. Consider this when evaluating patient lifestyle, willingness to take medication, and access to health care. Source: http://www.pwnfitness.com/harmful-dangerous-side-effects-zinc/ Drug-Nutrient Interactions Be aware of patient’s medications, vitamins & supplements, and recreational substances consumed/used in order to prevent interactions with ART. Ex: Grapefruit juice and protease inhibitors (PIs) both compete for cytochrome P450 enzyme. Grapefruit consumption can lead to either increased or decreased blood levels of the drug. Tables 38-2 through 38-5 in the Krause textbook break down specific drugs, interactions, and side effects. Source: Cost of Therapy ■ According to the CDC treatment usually costs $2000 - $5000 a month ■ About half of those diagnosed with HIV do not have regular health care ■ 42% are on Medicaid & 24% are uninsured ■ For the uninsured many will qualify for the AIDS Drug Assistance Program ⬜ Many states have an income cutoff of about $22,000/year ■ Estimated survival time of 24.2 years after HIV diagnosis yields the following costs: ⬜ Lifetime on discounted treatment: $385,200 ⬜ Lifetime without discount: $618,900 Source: http://blogs.scientificamerican.com/observations/2011/01/12/cost-of-cancer-care-projected-to-jump-nearly-40-percent-by-2020 Cost Breakdown Just FYI...HIV/AIDS costs the US about $12 billion annually in health care-related expenses! ■ ART Drugs 73% ■ Inpatient Costs 13% ■ Outpatient Costs 9% ■ Other HIV-related Medication & Lab Costs 5% Nutritional Implications RDs need to take into consideration: ■ ■ ■ ■ ■ ■ ■ Medications Disease Complications & Combinations Immunity Quality of Life Altered Metabolism Dietary Habits Health Care Access Energy Expenditure ■ Research suggests that patients may have up to a 10% increase in resting energy expenditure in asymptomatic HIV patients. That number can rise to up to 20 - 50% after an opportunistic infection (OI). ▪ Opportunistic Infections: These infections take advantage of a weakened immune system. Those with immuno-deficiencies can face serious threats from viruses and other microbes that healthy individuals would not even experience symptoms from. Source: http://www.healthline.com/health-slideshow/hiv-opportunistic- Nutrient Breakdown ■ PROTEIN: DRI of 0.8 g/kg IBW is recommended for healthy or asymptomatic individuals, however it should increase if REE is calculated at an increased rate. ⬜ Also increase by 10% after an OI ■ FAT/CHO: Keep intake relative to total calories. There is evidence to support increasing Omega-3 fatty acids in the diet and keeping saturated fats low. ■ MICRONUTRIENTS: There is NO evidence to support doses of micronutrients above the DRI. ■ It is important to monitor individual nutrients and to do so on a patient-by-patient basis Special Considerations: Wasting, Obesity, & HALS Wasting: unintentional weight loss and loss of LBM which are associated with disease acceleration and mortality. ■ Caused by a combination of possible factors such as poor dietary intake, nutrient malabsorption, increased metabolic rate, or various other metabolic complications. ■ Case Pt: Recent undesired weight loss of 6-9% UBW (9-14 lb.) Obesity: some ART medications increase risk of hyperlipidemia, insulin resistance, and diabetes. Monitor these values and encourage both aerobic and resistance training activities. HALS: HIV-Associated Lipodystrophy Syndrome ■ HALS refers to the abnormalities in fat distribution similar to metabolic syndrome. Fat accumulation in the abdominal or dorsocervical region are common. Fat atrophy in the extremities, face, and buttocks are also common. Nutritional Implications of HALS Common problems associated with HALS include: ■ Insulin Resistance ■ Hyperglycaemia ■ Dyslipidemia ■ high total cholesterol and triglycerides, lowered HDL cholesterol, elevated LDL cholesterol ■ Type II diabetes mellitus Nutritional interventions should be targeted towards patients individual symptoms and problems. There are no current major nutritional treatments for the lipodystrophy itself, but increasing fiber intake and physical activity may offer slight benefit. Examples of HALS Source: http://www.nature.com/nrendo/journal/v8/n1/images/nrendo.2011.151-f2.jpg http://1.bp.blogspot.com/-ewQ6BFHZA6o/T-UahEZ-KFI/AAAAAAAAfwA/-4HonrykycM/s640/collage1.jpg Case Patient Information for Nutrition Diagnoses ■ 32-year-old African American male, 6’1”, 151# CBW, and 160165# UBW ■ HIV diagnosed 4 years ago but had never been treated PTA ■ Admitted with very sore mouth/ throat, difficulty eating, likely PNA & progression to AIDS, mild malnutrition, & recent 6-9% (914 lb.) weight loss from UBW. ■ Diagnosis of AIDS-Stage 3 w/ oral thrush & no evidence of PNA. HAART initiated. Sources: http://remediesforthrush.blogspot.com/2013/09/oral-thrush-infection-and-solution.html http://recommendpills.com/candidiasis-symptoms-and-treatment/04/11/2012/ Case Patient Information for Nutrition Diagnoses ■ 32-year-old AA male 151# (69 kg) CBW, 160-165# (73-75 kg) UBW, 6’1” (185 cm) ■ Family hx of CAD & HTN ■ EEN: 2360-2740 kcal/d (MSJx1.4-1.5, rebuild LBM/infection) 100-125 g protein/d (1.2-1.5 g/kg IBW) 2,398 mL fluid (35 ml/kg/d) ■ 24-hr recall shows intake of ~2,000 kcal & 71 g protein ■ HAART regimen Atripla w/ side efx including N/V/D; anorexia; dysgeusia; increased cholesterol & TG; & known interaction w/ alcohol, SJW, garlic, & milk thistle ■ PTA took MVI, vit C & E, ginseng, milk thistle, & echinacea supplements ■ 2-3 beers 3-4 times/week Nutrition Diagnoses for Case Patient ■ Sample PES Statements for Patient T.L. ⬜ Unintended weight loss (NC-3.2) r/t inadequate oral intake and mouth pain AEB caloric intake ~73-85% of EEN according to 24-hr recall; mild malnutrition (82% IBW); and recent undesired significant weight loss of 6-9% (9-14 lb.). ⬜ Predicted food-medication interaction (NC 2.4) r/t concurrent use of Atripla, alcohol, milk thistle, and St. John’s wort AEB pt report of regular alcohol consumption and herbal supplementation along with recent initiation of HAART using Atripla (which has known DNIs with alcohol, milk thistle, SJW). ⬜ Food and nutrition-related knowledge deficit (NB-1.1) r/t lack of prior nutrition-related education AEB self-reported usual dietary intake (before mouth sores) high in processed foods and low in fresh nutrient-dense foods; high alcohol consumption; and excessive vitamin C and E supplementation. Common Nutrition Diagnoses for HIV/AIDS Patients ■ Inadequate oral intake (NI-2.1) ■ Inadequate protein-energy intake (NI-5.3) ■ Increased energy expenditure (NI-1.1) ■ Increased nutrient needs (NI-5.1) ■ Malnutrition (NI-5.2) ■ Unintended weight loss (NC-3.2) ■ Swallowing difficulty (NC-1.1) ■ Altered GI function (NC-1.4) ■ Predicted / Food-medication interaction (NC-2.4 or NC-2.3) ■ Altered nutrient-related laboratory values (NC-2.2) ■ Food and nutrition-related knowledge deficit (NB-1.1) ■ Limited access to food or water (NB-3.2) Nutrition Interventions for Case Patient Adjust meals to a texture modified diet (ND- 1.2) to ease pain from oral thrush and mouth sores by recommending soft foods (prepared mashed, pureed, or cooked until very soft). Refer pt to another provider (ND-1.5) for treatment of oral thrush, likely with antifungal medication. Promote a general/healthful diet (ND-1.1) with small, frequent meals to prevent further weight loss and promote weight regain to achieve IBW of 184# or at least UBW of 160-165#. Nutrition Interventions for Case Patient Refer pt to another provider (or community program if necessary) (ND-1.5; ND-1.6) if necessary to decrease alcohol intake & receive more education on living with AIDS. Instruction intended to lead to nutrition-related knowledge. Purpose of nutrition education (E-1.1) should be to improve pt’s food choices to improve PO intake toward meeting EEN; minimize DNIs w/ current medications; and stop excessive supplementation & alcohol consumption. Nutrition Interventions ■ Highly individualized: Very important to tailor intervention to pt needs using clinical judgment & collaborating w/ team of healthcare providers! ■ Energy/nutrient needs: NO specific nutrition therapy for HIV/AIDS except for meeting additional energy, protein, fluid, & micronutrient needs. ■ Specific diet/recommendations: Diet adjustments & nutrition counseling often needed to manage HIV/AIDS complications & comorbidities such as: ■ Cardiovascular disease/risk ■ Liver or renal disease (e.g., hepatitis B & C) ■ Diabetes, insulin resistance, and/or altered sex hormones Nutrition Interventions ■ Provide adequate nutrition/ reduce or eliminate malnutrition ⬜ ⬜ ⬜ ⬜ PRIORITY of treatment to prevent weight loss/wasting necessary for body to properly process meds & nutrients may significantly slow progression to AIDS decrease disease severity, maintain immune fxn, improve lifespan & quality of life ⬜ can be challenging to balance important health priorities ■ Minimize drug-nutrient interactions ⬜ many drugs need to be taken w/ regard to food ⬜ common HAART side efx of N/V/D, anorexia, dyslipidemia ⬜ potential interactions w/ alcohol, grapefruit, supplements Source: "Position of the American Dietetic Association: nutrition intervention and human immunodeficiency virus infection." JADA 110.7 (2010): 1105- Nutrition Interventions ■ Management of N/V/D ⬜ Small, frequent lower-fat meals w/ snacks ⬜ Replenish fluids & nutrients when lost ⬜ Avoid lying down within 1 hour of eating ⬜ Limit or avoid lactose, caffeine, & insoluble fiber ⬜ Nutrition supplements and medication as needed ■ Adjunct Therapies ⬜ Common Medications: antiemetic, antidiarrheal, appetitestimulating, lipid-lowering, antidiabetic, anabolic, & pain ⬜ Exercise: maintain/increase LBM, promote healthy BMI & body shape, & promote CV health Sources: http://coveville.com/how-to-get-rid-of-diarrhea/ Nutrition Care Manual Nutrition Interventions ■ Education & Counseling ⬜ ⬜ ⬜ ⬜ General nutrition & PA principles Food safety & access issues Meal preparation, timing, & content Medical adherence & potential DNIs ⬜ Micronutrient supplementation ⬜ Body image & changes to body weight/shape ⬜ Other psychosocial issues ■ Referral to Other Providers ⬜ Last but NOT least...this is key to any plan of care for HIV/AIDS patients! Sources: http://www.school-counselor.org/topics/new-school-counselor.html Nutrition Care Manual Nutrition Support ■ Enteral nutrition (EN) & parenteral nutrition (PN) support are both viable options for HIV/AIDS patients if needed. ■ Criteria for initiating either EN or PN remain the same as for other disease states & ASPEN Guidelines should be followed. ■ “If the gut works, use it!” still applies here...even when PN has been initiated, it is important to stimulate the gut regularly with water & a little food if at all possible to prevent GI dysfunction & reduce risk of bacterial translocation. ■ Catheter infection & refeeding syndrome are the primary risks of NS but minimized with proper monitoring & adjustment. ⬜ Especially for highly immunocompromised HIV/AIDS patients, additional sanitary precautions including the use of sterile water may be needed to reduce risk of infection. Nutrition Monitoring & Evaluation ■ Nutrition reassessments should generally be carried out at least every 3-6 months in HIV/AIDS patients. ■ Treatment for this population is highly individualized, so F/U may be appropriate sooner than 3 months depending on the initial nutrition assessment, diagnosis, & intervention. ■ During reassessments, it is important to monitor: ■ Food intake ■ Body weight, distribution, & composition ■ Anthropometric measurements can help identify HALS even when weight is stable! ■ Pertinent lab values ■ Medications ■ Supplements Nutrition M&E for Case Patient ■ Monitor weight over next 2 months ■ Encourage 0.5-1 lb. weekly weight gain ■ Target weight 184 lb. (acceptable range is 166-202 lb.) ■ With changes and disease progression, monitor & evaluate: ■ ■ ■ ■ ■ ■ Food intake Lab values Body composition Medications Supplements Ensure that education is continual and appropriate ■ M&E should take place at least semiannually after initial F/U