* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 眼科计算机课件
Survey
Document related concepts
Vision therapy wikipedia , lookup
Retinal waves wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
Macular degeneration wikipedia , lookup
Diabetic retinopathy wikipedia , lookup
Transcript
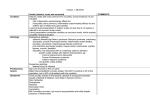
Uveal Tract Diseases UVEAL TRACT DISEASES U-1 Associated anatomic structure U-2 Uveitis U-3 congenital anomaly & tumor Ciliary body lens pupil Zonule retina choroid iris sclera U-1 Anatomy anatomy: iris, ciliary body, choroid physiology: vasular layer of the eye blood supply and flow speed retaining of the immunity cells is very easy similar to lymph node , “immune center” “antigen bank” : anterior & posterior uveal tract, lens, vascular, pigment epithelium, optic nerve… the incidence of the immunity diseases ↑ Inflammations ( uveitis) and uveal tumors comprised the vast majority of diseases affecting uveal tract Some associated with systemic diseases U.2. Uveitis “Uveitis” denotes inflammation of the choroid (choroiditis), ciliary body (intermediate uveitis), or iris (iritis). etiology 1.infections: bacteria, virus, fungi, parasites… 2.non-infections (1) exogenous: physical or chemical injury allergic reactions to external antigens (2) endogenous: classification of uveitis according to anatomy location (clinical) (1)anterior (2)intermediate (3)posterior (4)panuveitis cause of diseases : infections and noninfections pathology : granulomatous and nongranulomatous U.2-1. Anterior uveitis most common, usually unilateral and acute in oneset Acute iritis and iridocyclitis last for two to six weeks . Some patients have only one or two attacks in a lifetime, and others have multiple episodes. 1.symptoms (1) pain (2) photophobia (3) blurred vision 2.signs (1)ciliary or mixed congestion (2)aqueous flare: blood-aqueous barrier high concentration of plasma proteins Tyndall's sign particularly severe hypopyon (3) keratic precipitates (KP) small ( dust, nongranulomatous); large (mutton fat, granulomatous); pigment; stellate ( translucency). (4) Pupil may be small (miosis) or irregular (5) iris nodule Koeppe's nodules at iris margin Busaca nodules at iris stroma Berlin’s nodules in the anterior chamber angle (6) Anterior or posterior synechiae (7) corneal sensation (8) intraocular pressure Koeppe nodules Multiple bussaca nodules arrows (large) showing the ciliary congestion typical of acute anterior uveitis Smaller arrows show areas of the iris adherent to the lens (posterior synechiae differential diagnosis (1)acute conjunctivitis (2)acute angle-closure glaucoma (3)keratitis How can differentiate the acute conjunctivitis from acute angle-closure glaucoma, and acute iridocyclitis Table 1 acute conjunctivitis acute iridocyclitis acute angle-closure G. incidence extremely common common uncommon discharge moderate to copious none none vision no effect slightly blurred markedly blurred pain none moderate severe Conjunctival more toward fornics injection mainly circumcorna mainly circumcorna cornea clear usually clear steamy pupil size normal small moderately dilated and fixed pupilary light normal response poor none IOP normal elevated normal treatment of iridocyclitis corticosteriods and cycloplegics: topical therapy 0.1% dexamethasone; 1% prednisolone acetate, or systemic therapy prednisone homatropine 5% anti-prostaglandins : aspirin or indomethacine anti-infective therapy: virus, tuberculosis, syphilis complications: secondary G; complicated cataract. U.2-2. Intermediate Uveitis Also called pars planitis cause is unknown, infection, allergy, or autoimmunity? Commonly occurred in youth (late teens or early adult years), often bilateral, men commonly than women Intermediate uveitis Symptoms: floaters, blurred vision pain, photophobia, and redness are usually absent Signs: vitritis vitreous condensates,free-floating as “snowballs” layered over the pars plana and ciliary body as “snowbank” Comlications cystoid macular edema, retinal vasculitis optic nerve head neovascularization Macular edema diagnosis and differentiation treatment posterior sub-Tenon injection of triamcinolone oral prednisone steroid-sparing agents concurrent therapy for specific infectious cause U.2-3. posterior uveitis Include retinitis, choroiditis, retinal vasculitis, and optic neuritis Most associated with some form of systemic disease by infectious or noninfectious posterior uveitis symptoms floaters, reduced vision, scotomas Ocular injection: Redness of the eye is absent in conditions that affect only the posterior segment. Thus, it is rare in toxoplasmosis and absent in histoplasmosis. Pain: atypical, but can occur in endopthalmitis, posterior scleritis and optic neuritis. posterior uveitis signs Anterior uveitis: granulomatous nongranulomatous Vitritis : Vitreous opacity, cells may be seen with sliplamp microscope. Morphology and location of lesions: retina, choroid, optic nerve Mode of onset: acute and sudden slow and insidious Trauma: history of trauma is important in patients with uveitis to rule out intraocular foreign body posterior uveitis complications detachment of the retina treatment a) Corticosteroids b) Concurrent therapy for specific infectious cause c) Vitrectomy d) immunosuppressant Female, 56 ys Female, 31 ys U.2-4 panuveitis ( diffuse uveitis) Uniform cellular infiltration of both the anterior and posterior segments Tuberculosis, sarcoidosis, syphilis, sympathetic ophthalmia, Vogt-Koyanagi-Harada syndrome, Behcet’s disease Endophthalmitis U.3.Some special types of uveitis U.3-1.sympathetic ophthalmia rare but devastating bilateral granulomatous uveitis that comes on 10 days to many years following a perforating eye injury. injured , or exciting eye becomes inflamed first; the fellow, or sympathizing eye secondarily interval : 2 weeks--2 years symptoms photophobia, redness, blurred vision signs diffused uveitis Severely injured sightless eye is enucleation within 10 days after injury U.3-2.Vogt-Koyanagi-Harada syndrome age: 30-50; bilateral eyes; pigment epithelial disturbance acute or sub-acute headache, meningitis, dysaudia, vitiligo, alopecia -Koyanagi: anterior ; -Harada: posterior segment treatment In acute stage, ectrosis with a large dosage of corticosteroid should be used, 2~3days intravenous drop can almost inhibit choroidal exudation, then to diminish dosage gradually, a week later to change to oral administration; the method is to select intermittent administrationwhich may lighten the reduction of adrenocortical function, the lowering velocity should be decided according to the ill state of each case after careful observation, commonly till 3~6months to stop administration; White Choroidal Infiltrates (Arrow) Seen in VKH Syndrome with Very Pink Optic Nerve Head Localised Retinal Detachment Total Retinal Detachment, Where Whole Retina is Grey in Colour Scarring When Choroidal Granulomas Subside vitiligo U.3-3.Behcet’s disease recurrent uveitis, bilateral eyes; orogenital ulcerations and skin lesions, age: 20-40 years, sex: male>female U.4-3-2.clinical featurs of Behce't disease 1.ocular sign : *posterior ( more common ): retinal vasculitis hemorrhage ; edema; focal areas of retina necrosis; ischemic optic neuropathy; complicated cataract, secondary G. , and optic atrophy *anterior: acute iritis or chronic ; iridocyclitis with a transient hypopyon 2.recurrent orogenital ulceration; 3.multi-morpho lesions of the skin 4.arthritis 5.damage in the nerve system Fig-U.8 U.3-4.acute retinal necrosis syndrome U.4-4-2.clinical featurs of ARN Herpes simples virus periorbit pain, scleritis, anterior uvitis vitreous exudate necrosis retinitis: multifocal yellow patches from peripheral to posterior polar active retinal vasculitis after 4-6 weeks, 75% retinal detachment Cytomegalovirus retinitis prognosis of ARN may be blindness due to retinal detachment diagnosis and differential diagnosis (1)clinical features (2)laboratary examination treatment of ARN (1)acyclovir 5mg/kg /d in V. tid, 7-10 days (2)anti-coagulation agents: heparin (3)corticosteroids (4)laser photocoagulation (5)Chinese herbs U.3-5.Fuch's heterochromic iridocyclitis U.4-5-1.clinical features : chronic, young or middle-aged, M>F (1)iris: diffuse atrophy; (2)KP: fine, whiteness; (3)light aqueous flare (4)fundus: normal (5)complicated cataract and secondary G. U.4-5-2.treatment of the complications Fuchs U.4.congenital anomaly and tumors of the Uveal tract Iris Melanoma Choroidal Melanoma Choroidal naevus Malignant Melanoma