* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Anterior Segment Optical Coherence Tomography as a Diagnostic
Vision therapy wikipedia , lookup
Visual impairment wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Mitochondrial optic neuropathies wikipedia , lookup
Corneal transplantation wikipedia , lookup
Diabetic retinopathy wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
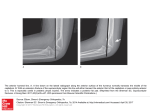
LETTERS RESEARCH LETTERS Anterior Segment Optical Coherence Tomography as a Diagnostic Tool for Cyclodialysis Clefts A nterior segment optical coherence tomography (OCT) is a noninvasive, painless, noncontact technique that provides accurate and reproducible images. This technique correlates well with ultrasound biomicroscopy, allows observation of iridocorneal angle abnormalities in the presence of opaque media, and is easier to perform than ultrasound biomicroscopy. A cyclodialysis cleft results from separation of the longitudinal ciliary muscle fibers from the scleral spur and establishes a new drainage pathway for aqueous humor between the anterior chamber and the suprachoroidal space. This new drainage channel increases uveoscleral outflow and may result in chronic ocular hypotonia; it is sometimes complicated by decreased visual acuity, a shallow anterior chamber, ciliochoroidal effusion, optic disc edema, retinal folds, hypotonus maculopathy, and engorgement and stasis of retinal veins.1 Slitlamp examination using a gonioscope has been the most common method used to confirm the existence of clefts. However, it cannot be used in patients with hyphema, corneal opacity, and excessive hypotonia after trauma or surgery. In these patients, ultrasound biomicroscopy (UBM) has been a useful tool for visualizing the anterior eye segment.2-5 We demonstrate the use of OCT as a new technique that provides anterior segment imaging and allows identification of cyclodialysis clefts in correlation with clinical examination and UBM. Report of a Case. A 38-year-old man was initially seen after having been hit in the left eye with a heavy bungee cord. He noted severe pain and blurred vision. Distance visual acuity was 20/20 OD and 20/80 OS. The right eye was unremarkable. Eyelid ecchymosis was seen in the left eye, and anterior segment examination revealed diffuse conjunctival hyperemia, Descemet folds, grade 1 hyphema (less than one-third of the anterior chamber), iritis, and an atonic pupil. The lens was clear, and there was no evidence of phacodonesis. Applanation intraocular pressure (IOP) was 14 mm Hg in each eye. Funduscopy revealed a healthy optic disc, macula, and peripheral retina in each eye. The patient was treated with topical prednisolone acetate, 1%; scopolamine hydrobromide; and bed rest with elevation of the head of the bed 30° to 45°. He was examined daily. After a week, visual acuity was 20/120 OS. There was resolution of the hyphema, persistent mild iritis, a shallow anterior chamber, and atrophy of the inferior iris. His left eye IOP was 5 mm Hg. Ophthalmos- Figure 1. A cyclodialysis cleft (arrow) revealed by gonioscopy. Figure 2. A cyclodialysis cleft (arrow) revealed by ultrasound biomicroscopy. copy revealed optic disc edema, radiating retina folds around the macula, and mild vascular tortuosity. Gonioscopy revealed a cyclodialysis cleft at the 7- to 8-o’clock position (Figure 1). A diagnosis of hypotonus maculopathy secondary to a posttraumatic cyclodialysis cleft was made. Both UBM (Figure 2) and anterior segment OCT (Figure 3) demonstrated the cyclodialysis cleft at the 7- to 8-o’clock position. Anterior segment OCT also provided high-resolution images that identified the disinsertion of the ciliary body from the scleral spur and an associated ciliary body detachment, confirming the diagnosis (Figure 3). Since the iritis was almost completely resolved and there is some literature that suggests that corticosteroid therapy should be limited in patients with cyclodialysis6 because of the possibility of a secondary increased IOP and inhibition of scar formation, administration of prednisolone acetate was stopped and only scopolamine hydrobromide therapy was continued. Six months later, distance visual acuity was 20/20 OS and near visual acuity was 20/20 with a correction of ⫹3 diopters (REPRINTED) ARCH OPHTHALMOL / VOL 127 (NO. 1), JAN 2009 109 WWW.ARCHOPHTHALMOL.COM ©2009 American Medical Association. All rights reserved. Downloaded From: http://jamanetwork.com/ on 05/06/2017 Correspondence: Dr Mateo-Montoya, Ophthalmology Clinic, Department of Clinical Neurosciences, Geneva University Hospital, 22 rue Alcide-Jentzer, CH-1211 Geneva 14, Switzerland ([email protected]). Financial Disclosure: None. Figure 3. A cyclodialysis cleft (arrows) confirmed by anterior segment optical coherence tomography. Disinsertion of the ciliary body from the scleral spur and an associated ciliary body detachment were also revealed. in that eye. This result suggested that the patient had lost his accommodation, probably because of the ciliary body detachment. The IOP in the left eye was 10 mm Hg, and macular folds were less marked. Repeated UBM and anterior segment OCT showed persistence of the cyclodialysis cleft and an even larger ciliary body detachment. The patient’s vision status was excellent compared with that of other patients with cyclodialysis clefts described in the literature.7 Because visual acuity was good and IOP was normal, continued follow-up was agreed on. However, the patient was informed of the risk of continued enlargement of the cyclodialysis cleft; if this were to happen, different treatment options would be proposed, such as suturing the ciliary body to the sclera, vitrectomy with pars plana cryopexy for the detached ciliary body, and gas tamponade8 or argon laser photocoagulation.9 Comment. Cyclodialysis clefts occur most commonly after trauma and sometimes after surgery. Intentional surgical cyclodialysis has been used for the treatment of glaucoma.2-6 Gonioscopy has been the classic method for visualizing a cyclodialysis cleft; however, cyclodialysis clefts could be missed in traumatized eyes with hazy media, distorted anatomy, or hypotonia. In these cases, UBM has been useful.2-5 We presented diagnostic images of a cyclodialysis cleft using a new technique, anterior segment OCT. This technique provided high-resolution images of the cyclodialysis cleft, showing its exact location and the extent of the disinsertion of the ciliary body from the scleral spur and an associated ciliary body detachment. These images served to confirm the clinical diagnosis. Anterior segment OCT is a noninvasive tool that provides accurate and reproducible images of the anterior segment. This technique has good correlation with UBM and allows observation of iridocorneal angle abnormalities in the presence of turbid media, hypotonia, and abnormal anterior segment anatomy. In addition, anterior segment OCT has some advantages compared with UBM: it does not require any contact with the patient’s eye, it does not require the use of topical gel, it is more comfortable for the patient, it is easier to perform, and it does not risk traumatizing or contaminating the cornea. Aránzazu Mateo-Montoya, MD Sylvain Dreifuss, MD Submitted for Publication: June 1, 2008; final revision received August 19, 2008; accepted August 25, 2008. 1. Aminlari A, Callahan CE. Medical, laser, and surgical management of inadvertent cylodialysis cleft with hypotony. Arch Ophthalmol. 2004;122(3):399-404. 2. Gentile RC, Pavlin CJ, Liebmann JM, et al. Diagnosis of traumatic cyclodialysis by ultrasound biomicroscopy. Ophthalmic Surg Lasers. 1996;27(2): 97-105. 3. Kaushik S, Arya SK, Kochhar S. Cyclodialysis cleft diagnosed by conventional ultrasonography. Ophthalmic Surg Lasers. 2000;31(4):346-349. 4. Park M, Kondo T. Ultrasound biomicroscopic findings in a case of cyclodialysis. Ophthalmologica. 1998;212(3):194-197. 5. González Martı́n-Moro J, Muñoz-Negrete FJ, Rebolleda G, Lara Medina J, Garcı́aFeijoó J. Ultrasonic biomicroscopic findings after spontaneous resolution of a traumatic cyclodialysis [in Spanish]. Arch Soc Esp Oftalmol. 2003;78(4): 211-214. 6. Brandonisio TM, Newman TL. Hypotonous maculopathy and normal visual acuity secondary to post-traumatic cyclodialysis cleft. Optometry. 2002;73 (10):620-625. 7. Chaudhry NA, Flynn HW Jr, Palmberg PF. Elastic cord-induced cyclodialysis cleft and hypotony maculopathy. Ophthalmic Surg Lasers. 1999;30(8): 678-680. 8. Takaya K, Suzuki Y, Nakazawa M. Four cases of hypotony maculopathy caused by traumatic cyclodialysis and treated by vitrectomy, cryotherapy, and gas tamponade. Graefes Arch Clin Exp Ophthalmol. 2006;244(7):855-858. 9. Joondeph HC. Management of postoperative and post-traumatic cyclodialysis clefts with argon laser photocoagulation. Ophthalmic Surg. 1980;11(3): 186-188. -3 Long-Chain Polyunsaturated Fatty Acid Intake Inversely Associated With 12-Year Progression to Advanced Age-Related Macular Degeneration A ge-related macular degeneration (AMD) is a leading cause of vision loss. Age-Related Eye Disease Study (AREDS) participants reporting the highest intake of -3 long-chain polyunsaturated fatty acids (LCPUFAs) were approximately half as likely as their peers reporting the lowest intake of these nutrients to have neovascular (NV) AMD1 at baseline or to progress across a 6-year period from bilateral drusen to central geographic atrophy (CGA).2 The Age-Related Eye Disease Study provides data that represent, to our knowledge, the largest longitudinal sample collected and classified with standardized methods as part of a natural history study on AMD. We now report that our baseline and 6-year findings persisted in 12-year AMD incidence models. These results are consistent with existing data.3,4 Methods. The Age-Related Eye Disease Study was a National Institutes of Health–sponsored and administered multicenter study designed to assess the clinical course, prognosis, and risk factors of AMD (http://www.nei.nih .gov/amd/). We examined the relationship of dietary intake of -3 LCPUFAs with progression to advanced AMD in 1837 AREDS participants who had a moderate risk for developing sight-threatening AMD (1211 participants in category 3a and 626 participants in category 4a). Participants in category 3a had bilateral visual acuity of 20/32 or better and bilateral large (ⱖ125-µm) drusen, extensive intermediate drusen, and/or geographic atrophy that did not involve the center of the macula in at least 1 eye. Category 4a participants had visual acuity of 20/32 or bet- (REPRINTED) ARCH OPHTHALMOL / VOL 127 (NO. 1), JAN 2009 110 WWW.ARCHOPHTHALMOL.COM ©2009 American Medical Association. All rights reserved. Downloaded From: http://jamanetwork.com/ on 05/06/2017