* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download outline27890
Survey
Document related concepts
Transcript
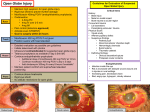
A “Sticky” Case of Endophthalmitis Lecture Outline By Jeff Cohen, O.D. Abstract: Endophthalmitis is a serious ocular infection that warrants prompt medical attention. This case discusses an atypical presentation of endophthalmitis and reviews the current management and treatment of this condition. I. Case History: A. 80 year old white male B. Chief complaint: pain, photophobia, tearing, and yellow discharge OD since corneal suture removed 3 days prior C. Past Ocular History: PKP OD in 10/2005 secondary to pseudophakic bullous keratopathy, superior bleb with iris prolapse OS, pseudophakia ou D. Family history: unremarkable E. Past medical history: Basal cell carcinoma (currently receiving chemotherapy),colon carcinoma, h/o H. Pylori infection, colon polyps, angina, hypertension, GERD, hyperlipidemia, low back pain, COPD, hernia F. Active Medications: Albuterol, Amlodipine, Ammonium Lactate lotion, Aspririn, Diphenhydramine, Docusate, Fluoxetine, Hydrocortisone cream, Ipratropium Bromide inhalant, Ketoconazole cream, Levothyroxine, Lisinopril, Loperamide, Metoprolol Tartrate, Moxifloxacin HCL, Omeprazole, Oxycodone prn, Prednisolone 1% ophth susp QD OD, Prochlorperazine, Sennosides, Simvastatin, Terazosin, Trazodone. G. No medical allergies II. Pertinent Findings: A. Clinical: i. BCVA HM OD and 20/20-2 OS ii. Current Spec Rx: OD: -6.00+3.00x131, OS: -2.00+0.50x010 iii. Pupils: OD unable to view, OS peaked vertically, reactive to light, no APD. iv. Intraocular pressures: 26 mm Hg OD and 19 mm Hg OS v. Slit Lamp Exam: 1. LLL: mild debris OU 2. Conj/Sclera: 2-3+ inj OD; iris prolapsed covered with conj superior nasal OS. 3. K OD: hazy corneal, corneal graft with intact sutures, 3mm x 3mm ulcer superotemporally with indistinct borders encompassing graft-host interface, with mucous surrounding ulcer. Early pterygium nasally. K OS: arcus 4. AC: deep/with 1.3mm high hypopyon inferiorly OD; d/q OS 5. I: flat/intact ou 6. Lens: ACIOL OD, PCIOL OS vi. Fundoscopy – unable to view secondary to corneal haze B. Ancillary testing: i. B-scan ii. Corneal cultures with blood, chocolate, Sabourad, and thioglycolate agars. Gram and Giemsa smears, too. iii. Vitreous tap for Gram stain, culture, and sensitivities. III. Differential Diagnoses: a. Chronic Postoperative Uveitis b. Fungal Keratitis c. Acanthamoeba Keratitis d. Bacterial Keratitis e. Endophthalmitis IV. Results of testing: A. Corneal culture positive for Staph Aureus (Methicillin Sensitive) B. B-scan: Dense vitreous debris, no retinal detachment appreciated V. Diagnosis: A. Endophthalmitis OD s/p PKP suture removal VI. Discussion: A. Endophthalmitis is a serious intraocular infection. Generally reserved for bacterial or fungal pathogens, but any organism can cause it. B. Three types of endophthalmitis i. Traumatic ii. Postoperative 1. Early 2. Late iii. Endogenous C. Epidemiology i. Traumatic- between 3% and 44% of all cases, but most sources say 20%-30% ii. Postoperative- more than half of all cases; most common form iii. Endogenous- between 6% to 14% of all cases; least common form, more prevalent in ill patients and IV drug users D. Organisms i. Traumatic- mostly Bacillus; usually associated with high pathogenicity ii. Postoperative- mostly Staphylococcus epidermidis, from the patient’s own flora. iii. Endogenous- mostly a fungal infection like Candida species E. Diagnosing i. Symptoms- decreased VA (usually 5/200 or worse), redness, and pain ii. Signs- conjunctival hyperemia, AC cell and flare, vitreous cells and opacities, hypopyon, lid edema, chemosis, corneal edema, reduced red reflex; possible APD and corneal ring infiltrate iii. Onset 1. Traumatic- acutely; at time of incident 2. Postoperative- median of 6 days after surgery, but can be up to 6 weeks. If it’s due to a low pathogenicity organism, it can be >6 weeks. 3. Endogenous- depending on the organism, can be fulminant (acutely) or insidious (latent) F. Imaging Studies i. B-scan ultrasound- can show vitreous opacities, choroidal thickening, retinal or choroidal detachment. Also useful in following the response of endophthalmitis to treatment ii. Computed tomography (CT) - useful in traumatic cases when an intraocular foreign body is suspected. Also, can identify sinus infections if the organism spread to periorbital sites. G. Cultures i. Need immediate culturing on blood, chocolate, Sabouraud, and thioglycolate agars as well as Gram and Giemsa stains. VII. Treatment/Management: A. Initial management included: i. Topical fortified Tobramycin 1.4% every hour, Vancomycin 2% every hour (alternating the two), Prednisilone Acetate 1% BID, and Vigamox 6x/day. ii. Intravitreal injections of Ceftazadime, Vancomycin, and Dexamethasone were given the same day. B. Follow-up Treatment i. Corneal gluing for dehiscence at graft-host interface with overlying bandage contact lens. ii. The patient’s medications were slowly decreased as the infection and inflammation resolved. VIII. Conclusion: A. Endophthalmitis is an infection within the eye caused from intraocular surgery, trauma, or from an infection somewhere else in the body. B. Most cases are diagnosed on clinical appearance and treatment is initiated empirically while awaiting results from culture tests. C. Rapid diagnosis and treatment is necessary to prevent irreversible damage from a case of endophthalmitis. IX. References 1. Lemley, Craig and Han, Dennis. “Endophthalmitis: A Review of Current Evaluation and Management.” Retina 27.6 (2007): 662-680. 2. Bhatia, Subir. “Ocular Surface Sealants and Adhesives.” The Ocular Surface 4.3 (2006) 146-154. 3. Nagra P, Hammersmith K, et al. “Wound Dehiscence After Penetrating Keratoplasty.” Cornea 25.2 (2006) 132-135 4. Culbert RB, and Devenyi RG. “Bacterial endophthalmitis after suture removal.” Journal of Cataract and Refractive Surgery 25 (1999): 725-727 5. Krause L, Bechrakis NE, et al. “Incidence and outcome of endophthalmitis over a 13year period.” Canadian Journal of Ophthalmology 44 (2009) 88-94 6. Major JC, Engelbert M, et al. “Staphylococcus aureus Endophthalmitis: Antibiotic Susceptibilities, Methicillin Resistance, and Clinical Outcomes.” American Journal of Ophthalmology Nov. 2009: 1-7 7. Kokolaris S, Zafirakis P, et al. “Endophthalmitis After Suture Removal.” Journal of Cataract and Refractive Surgery 26 (2000) p.632. 8. Ehlers, Justis P. and Shah, Chirag P. The Wills Eye Manual. 5th ed. Pp 62-69, 358364. 9. MacCumber, Matthew W. Management of Ocular Injuries and Emergencies. Pp. 275282 10. Fan, Jennifer C. et.al. Infectious endophthalmitis: clinical features, management, and visual outcomes. Clinical and Experimental Ophthalmology 2008. Vol 36, pp. 631-636 11. Christo CG, Van Rooij J, et al. “Suture-Related Complications Following Keratoplasty: A 5 year Retrospective Study.” Cornea 20(8): 816-819, 2001. 12. Jun and Chung. “Toxic Anterior Segment Syndrome after Cataract Surgery”. Journal of Cataract and Refractive Surgery 36, 314-316, 2010