* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Abacavir Regimen - WHO archives
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of HIV-protease inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
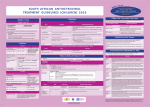
1 (22 April 2002) Application for Inclusion of abacavir on WHO Model List of Essential Medicines Drug is a member of the therapeutic class of HIV nucleoside analogue reverse transcriptase inhibitors Summary of Proposal Since the first clinical evidence of AIDS was reported over twenty years ago, an estimated 25 million people have died as a result of HIV infection. Current estimates suggest that around 40 million persons world-wide are infected with HIV and more than 90% of infected persons live in the developing world. Growing experience of the provision of anti-retroviral therapy in resource-limited settings (eg. Brazil, Côte d’Ivoire, Senegal, Haiti, India) indicates that treatment can be provided in an effective and safe manner. The delivery of anti-retroviral treatment in low-income countries has been aided by the development of fixed drug combinations and substantial reductions in the prices of certain products. The nucleoside reverse transcriptase inhibitor abacavir is proposed for listing on the WHO Model List of Essential Medicine. Other members of this class of drugs may serve as alternatives, depending on quality, price and local availability. A search of several data-bases, including the Cochrane Library, Medline and Embase, retrieved systematic reviews and articles supporting the use of HIV-1 RNA levels and CD4 cell counts as valid surrogate measures for changes in the rates of clinical outcomes during treatment of HIV-infected subjects. The literature search also provided evidence that combinations of 3 or 4 anti-retroviral drugs are superior to dual or single drug therapy. The latter are no longer regarded as satisfactory treatment, because of low efficacy rates and the development of resistance. Extensive library searches compiled by the Cochrane Review Group for HIV/AIDS resulted in the retrieval of a total of 7 randomised controlled trials of abacavir (ABC) and 5 uncontrolled single arm studies that provided insights into the efficacy and safety of this drug for different indications. As initial therapy in antiretroviral-naïve subjects (3 trials), abacavir (ABC) in combination with two nucleoside reverse transcriptase inhibitors (zidovudine and lamivudine), was superior to two nucleoside reverse transcriptase inhibitors alone. Abacavir-containing regimens appeared equivalent to protease inhibitor-containing regimens in achieving viral suppression (with the possible exception of subjects with high baseline viral loads), and there was some evidence of better adherence to treatment than with the PI -containing regimens. One trial studied the addition of ABC (or placebo) in patients receiving dual and triple-drug 2 regimens with detectable viral loads (above 400c/mL) (intensification therapy). Overall, patients receiving abacavir were significantly more likely than those on placebo to have a viral load (VL)<400c/mL at 48 weeks. However, only 13% of patients in the ABC arm had VL<50c/mL (vs. 0% of patients in the placebo arm). Abacavir has also been tested (3 trials) as an alternative to protease inhibitors (replacement therapy) in patients who were receiving stable combined drug therapy. All three trials showed high rates of continued viral suppression in patients randomized to abacavir-based regimens. Overall abacavir was quite well tolerated. Overall rates of adverse reactions were similar to, or less than, what was seen with Pi-containing regimens and adherence rates were similar or higher. However hypersensitivity reactions with ABC were observed in several trials with reported rates between 2% and 10%. Abacavir can be administered as twice daily treatment. It is presently available as a fixed dose combination with ZDV and 3TC from one manufacturer (GSK - TrziverTM) at an annual treatment cost of $US 2409. The costs of a year’s treatment with ABC alone varies from $US 1387 (GSK) to $US 2628 (Hetero). 1. Summary statement of the proposal for inclusion, change or deletion. Abacavir is proposed for inclusion on the WHO Model List of Essential Medicines, as part of a multi-drug antiretroviral regimen for the treatment of HIV/AIDS within an appropriately monitored program. Abacavir should be viewed as an example of the class of nucleoside analogue reverse transcriptase inhibitors. Other examples of this group may sometimes be preferred when local factors such as availability and price are taken into account. Antiretroviral therapy is recommended for HIV-infected children, adolescents, and adults with symptomatic disease, and also for asymptomatic patients with CD4+ cell counts at or below 200/mm3. Where CD4+ cell testing is unavailable, clinicians can use the presence of a total lymphocyte count below 1200/mm3, but only in symptomatic patients.1,2 2. Name of the focal point in WHO submitting the application: HIV/AIDS Department at WHO; the person responsible is Dr Dr Bernhard Schwartländer, Director of Evidence and Policy. 3. Name of the organization(s) consulted and/or supporting the application: Supporting letters may be submitted – please contact Dr Robin Gray (WHO/EDM) at [email protected] 4. International Nonproprietary Name: abacavir sulfate 5. Listing Type Requested: Listing is requested on the Model List of Essential Medicines as an example of the therapeutic class of HIV nucleoside analogue reverse transcriptase inhibitors. Other 3 members of this class of drugs may serve as alternatives, depending on quality, price and local availability. 6. Information supporting the public health relevance of the submission: Since the first clinical evidence of AIDS was reported over twenty years ago, an estimated 25 million people have died as a result of HIV infection. Current estimates suggest some 40 million persons worldwide are infected with HIV and more than 90% of infected persons live in the developing world3. In 2001, 5 million persons worldwide became infected with HIV, and 3 million others died from HIV/AIDS-related causes. In sub-Saharan Africa, the region most severely affected by HIV, 28.1 million individuals are living with this infection. Eastern Europe — especially the Russian Federation — continues to experience the fastest-growing epidemic in the world. In 2001, there were an estimated 250 000 new infections in this region, bringing to 1 million the number of people living with HIV. In Asia and the Pacific, an estimated 1 million people became infected in 2001; about 7.1 million people in this region are now living with HIV/AIDS 3. More than 1.8 million people in Latin America and the Caribbean are living with HIV/AIDS, including the 190,000 adults and children who became infected in 2001 In countries often already burdened by huge socio-economic challenges, HIV/AIDS threatens human social welfare, developmental progress, and social stability on an unprecedented scale. HIV/AIDS cripples the economic development of entire countries, because it often strikes people during their most productive working years. Of the 14,000 persons who became infected each day in 2001, about 12,000 were aged 15 to 49 years 3. Left untreated, HIV infection results in a period of clinical latency that may last a median of 3 to 10 years. Once symptomatic disease or AIDS develops, without access to antiretroviral treatment, death results within an average of two years. In high-income countries, an estimated 1.5 million people live with HIV, many of them productively, thanks to antiretroviral therapy. In the USA, the introduction of triple combination antiretroviral therapy in 1996 led to a decline of 42% in deaths attributable to HIV/AIDS in 1996-973. The feasibility efficacy and adherence with antiretroviral therapy has been demonstrated in a number of national and smaller pilot programs in middle- and low-income countries. In Brazil, the policy of universal access to antiretroviral drugs has reduced the number of AIDS-related deaths by nearly 50% and cut the incidence of opportunistic infections by 60 - 80%4. Between 1997 and 2000, Brazil saved approximately US $677 million in averted hospitalisations and treatment of HIV-related infections. In Argentina a program similar to that of Brazil provides even greater coverage. A special fund has been established to pay for antiretroviral drugs for those not covered by social security (such as street vendors, small business people, the unemployed, low-income pregnant women) 5. 4 Through the UNAIDS Drug Access Initiative Pilot Program, 6 treatment centres in Abidjan, Côte d’Ivoire, offer antiretroviral therapy. Of the patients who received therapy, 72% were heavily symptomatic upon initiation. Nonetheless, the overall survival rate of was 93% at 6 months, 90% at 12 months, and 86% at 18 months. When survival rates are re-calculated using a worst-case scenario in which patients lost to follow-up are assumed to have died immediately after their last clinic visit, 75% survived at 6 months, 64% at 12 months, and 55% at 18 months6. The Senegal Initiative on Antiretroviral Therapy was launched in August 1998. A partnership between the Senegalese government and the International Therapeutic Solidarity Fund, it aims to have 7,000 patients on triple combination therapy by the end of 2007. At the end of 2001, an estimated 550 adults and children had received treatment. A prospective observational cohort study was undertaken to assess the feasibility, effectiveness, adherence, toxicity and viral resistance of antiretroviral therapy. The clinical and biological results of the study were comparable to those seen in western cohorts, despite differences in HIV-1 subtype and an advanced disease stage when treatment was initiated. Fifty-eight patients with advanced HIV disease demonstrated by CDC staging (16 patients in CDC Stage B, 42 in CDC Stage C) and CD4+ cell count (median CD4+ cell count = 108.5, IQR = 34 - 217) were given triple combination antiretroviral therapy (2 nucleoside analogues + 1 protease inhibitor). After 18 months of treatment, participants gained a median of 180 CD4+ cells and showed a median drop in plasma viral load of 2.8 log10 copies/ml. During the study period, there were 7 clinical AIDS-defining events with 6 deaths from HIV-related infections7. The antiretroviral regimen was complex: indinavir, the protease inhibitor used in the study, had to be taken in a fasting state every 8 hours, with maintenance of hydration; didanosine (DDI), the nucleoside analogue given to 86% of participants, is a buffered preparation which also had to be taken while fasting 1 to 2 hours after any other medication. Despite the complexity of the regimen, 80% of patients (IQR 72-87%) showed adherence 80% at 18 months. In Cange, a Haitian village, the non-profit organization Partners in Health has introduced antiretroviral therapy to a small number of seriously ill AIDS patients, based on their Directly-Observed Therapy (DOT) programme for multiple-drug resistant tuberculosis. This DOT programme has been successful, with 90% of all registered TB cases in the Cange catchment area considered cured, compared with just 26% in other regions of Haiti. Sixtyfive patients were selected to receive triple combination antiretroviral therapy on the basis of clinical indicators of severe HIV disease (e.g. wasting, recurrent opportunistic infections, severe neurological complications, etc.). Shortly after initiating treatment, most patients showed clinical improvement. To counter critics and test the effectiveness of the programme, blood samples were sent to Boston for viral-load analysis. The results showed that 83% of patients on triple therapy had unquantifiable viral load measures. For the most part, side effects have been minimal and easily managed and there are support groups to encourage adherence.8 At HIV clinics in Pune and Ahmedabad, India, a recent study demonstrated the benefit of triple combination antiretroviral therapy (nevirapine + 2 nucleoside analogue RTs) in 347 patients with advanced HIV disease. At 12 months, 64.6% of the study participants experienced an increase of more than 20% in CD4+ cell counts. Twenty-three secondary 5 clinic events during the study were reported, including 6 deaths (4 TB-related, 1 cryptococcal meningitis, 1 non-Hodgkin’s lymphoma) — an AIDS-associated mortality rate of 5.7% at six months. This program was also significant for the fact that it relied on generic drugs supplied by Indian pharmaceutical manufacturers.9 Thus, in addition to the large amount of clinical data from high-income countries, there is a small but growing body of clinical evidence to support the use of ARVs in developing countries. Significant price reductions have also been achieved in many developing countries and new funding and delivery mechanisms are being developed to expand their availability. These factors warrant the addition of this class of drugs to the Model List of Essential Drugs (with appropriate consideration of their use in resource-limited settings). 7. Treatment details: Recommended Dosage: Adults: 300 mg twice daily, in combination with at least two other antiretroviral drugs. There are no food restrictions. Children and adolescents 3 months to 16 years of age: 8 mg/Kg twice daily, to a maximum of 300 mg twice daily, in combination with at least two other antiretroviral drugs. Formulations: Abacavir 300mg tablets; Abavacir 300mg + Zidovudine 300mg + Lamivudine 150mg fixed dose combination tablets (“Trizivir”TM). Concomitant Antiretroviral Therapy: Abacavir must be given in combination with other antiretroviral medications. Duration: Antiretroviral treatment is usually regarded as life-long with the exceptions of post-exposure prophylaxis and for the prophylaxis of infants of HIV-infected mothers. Guidelines: The draft “WHO Antiretroviral Guidelines for Resource Limited Settings”10 indicates abacavir (in combination with two other antiretroviral medicines) is a preferred first-line regimen for the treatment of HIV/AIDS. Special Requirements: Adequate resources for monitoring and specialist oversight are a pre-requisite for the introduction of this class of drugs. Familiarity with the diagnosis of and response to Abacavir hypersensitivity reaction is of particular importance. 8. Comparative effectiveness in clinical settings: In compiling the evidence for this and related submissions for anti-retroviral drugs we have created a common ‘stem’ in the form of information that is relevant to all of the antiretroviral group. This is followed by information that is relevant to use of this class of drug under the conditions described in this application, followed by information which is specific to the individual agent under consideration. Because of time constraints and the growing acceptance of the efficacy of highly active anti-retroviral drug regimens in the last 5 years, we have relied in part on secondary data 6 sources – systematic reviews of randomised and non-randomised studies conducted by the Cochrane Collaboration, or by independent groups who have generally met standards that are considered appropriate to this type of work. We have relied on individual trials where these provided data and insights not available from systematic reviews. Details of literature searches conducted The principal data-bases maintained by the WHO that were searched were: o The Cochrane Data-base of Systematic Reviews o The ACP Journal Club reviews of published trials o The data-base of reviews of abstracts of reviews of effectiveness (DARE) o The Cochrane controlled trials register (CCTR) o Medline o Embase o o o AIDSLINE AIDSTRALS AIDSDRUG Search terms included: o o o o o o o Anti-retroviral or antiretroviral Nucleoside reverse transcriptase inhibitors Non-nucleoside reverse transcriptase inhibitors Protease inhibitors Randomised clinical trial (exploded and as text word) Individual drug names: eg abacavir (ABC) Study selection: o o Randomised comparative parallel-group controlled clinical trials Examined the performance of abacavir when included in combinations comprising 3 or more drugs, involving concomitant use of NRTIs, other NNRTIs or PIs. Categorisation of levels of evidence The following rating scheme was used11: Level 1 – evidence from relevant high quality systematic reviews of unbiased randomised comparative clinical trials Level 2 – evidence from at least one relevant unbiased randomised comparative clinical trial. Level 3 – evidence from relevant controlled observational studies Additional considerations for use in resource-poor settings Co-morbidity Simplicity (frequency of dosing, number of tablets) 7 Tolerability Cost Prior exposure to ARVs General therapeutic issues: (common to the therapeutic category of anti-retroviral drugs) 1. What is the validity of surrogate markers as predictors of morbidity and mortality in patients with HIV/AIDS? 2. What evidence is there that triple (or quadruple) ARV therapy is superior to single or dual therapy? Class specific questions 3. Which combinations of drug classes have the best evidence in relation to benefits and harms? Agent-specific questions 4. What is the evidence for the efficacy and toxicity of anti-retroviral drug combinations that include abacavir? Results 1. What is the validity of surrogate markers as predictors of morbidity and mortality in patients with HIV/AIDS? (Level 3 evidence) Trials of anti-retroviral compounds have relied heavily on measuring the effects of drugs on surrogate markers, usually CD4 cell counts and plasma HIV-1 RNA levels. The validity of these markers depends on showing that they are correlated with clinical outcomes, and that they should be able to capture the effects of treatment on the major clinical outcomes12. Both of these markers may be viewed as being on the ‘causal pathway’ between viral infection and disease outcomes, but more directly in the case of viral measures. The viral end-point has come to be regarded as superior to a measure as a prognostic marker, although results have not been entirely consistent. A meta-analysis of trials of 2 NRTIs (plus NNRTI or PI), which included 36 treatment arms, found that baseline CD4 counts were significantly correlated with virologic suppression at 6 and 12 months, whereas a similar correlation was not found with baseline viral load and subsequent viral suppression13. The authors concluded that baseline CD4 cell count was a better predictor of drug induced viral suppression than baseline viral load. In the other meta-analysis of surrogate measures uncovered by the literature search, Hill et al reviewed results from 15 randomised trials that used surrogate markers and also included measures of disease progression14. This review included data from 15038 patients, of whom 3532 patients progressed to clinical outcomes. The analyses documented that there were significant correlations between the relative hazards for clinical progression and changes in both HIV-1 RNA levels and CD4 cell counts. The authors concluded that these markers, together, were useful in monitoring treatment responses. However the data also indicate the value of using CD4 cell counts alone. Another meta-analysis has quantified the relationship between changes in surrogate measures and development of AIDS or death. In an analysis based on 16 randomised trials of NRTIs, Babiker et al. estimated that the average hazard reduction was 51% (95% CI 41, 59%) for each reduction in HIV 8 RNA levels of 1*log10, and 20% (95% CI 17, 24%) for each increase of 33% in CD4 cell count15. These studies are supported by a wealth of observational data from developed countries, showing that the use of highly active anti-retroviral therapy, tested on the basis of surrogate markers in many trials, has profoundly influenced the outcomes for patients with HIV infection. 2. What evidence is there that triple (or quadruple) ARV therapy is superior to single or dual therapy? (Level 1 evidence) There is extensive clinical experience suggesting that multiple drugs with different modes of action are necessary to achieve sustained viral suppression (induction). Such combination treatments are standard recommendations in clinical practice guidelines. 16,17,18 There is insufficient space and time to present all of the relevant studies documenting the success of multi-drug induction therapy to the Expert Panel. However, a smaller number of trials have documented the value of various maintenance regimens introduced after successful induction therapy and these studies are relevant. Four trials that compared 3 or 4 drug maintenance regimens with 2 drug regimens were included in a Cochrane Review19. Use of a two-drug maintenance regimen was associated with an odds ratio for virologic failure (loss of HIV suppression) of 5.55 (95% CI 3.14, 9.80). These results complement an earlier systematic review, which synthesised data from 6 trials that compared the results of zidovudine monotherapy with treatment combinations comprising ZDV with DDI or DDC20. Although mainly of historical interest now, the review studies clinical outcomes and showed that the addition of DDI to ZDV resulted in a reduced odds of disease progression and death (OR 0.74, 95% CI 0.67, 0.82) and (0.72, 95% CI 0.64, 0.82) respectively. The addition of DDC gave similar results: disease progression, 0.86 (95% CI 0.78, 0.94); and death, 0.87 (95% CI 0.77, 0.98). After 3 years the rates of mortality were ZDV 59%, ZDV+DDC 63% and ZDV+DDI 68%. The reviewers concluded that the combination of ZDV and DDI was probably superior to ZDV plus DDC. The most recent review of the importance of multiple drugs in treatment of HIV/AIDS was recently published in the BMJ21. These investigators pooled data from 54 randomised clinical trials. The odds ratio for disease progression with 3 drugs compared with 2 drugs was 0.62 (95% CI 0.50, 0.78), but data were considered inadequate to determine if a general advantage was achieved by addition of a fourth drug. 3. Which combinations of drug classes have the best evidence in relation to benefits and harms? (Level 2 evidence) Unfortunately this is a question that is not yet addressed in published systematic reviews. Enquiries directed to the AIDS/HIV review group in the Cochrane Collaboration revealed that relevant reviews are underway but results are not yet available. Some of the data from the limited number of trials comparing different combinations of 3 or more anti-retroviral drugs will be reviewed in relation to the individual drugs (see below). However there are broad questions about which combinations should be used as first line treatment, and in what sequence should they be employed. The clinical practice guidelines mentioned earlier address some of these issues and point out that choice is determined not only by direct evidence of comparative clinical efficacy, but also by tolerability and toxicity, 9 presence of co-morbidity, concern about the development of viral resistance, and more pragmatic considerations such as pill burden and adherence to therapy. With recognition that none of the available regimens eradicates the virus, but suppression is desirable, HIV infection has come to be regarded as a chronic disease, which requires long-term (albeit sometimes intermittent) drug therapy. An additional consideration is a wish to ‘preserve’ more active anti-retroviral regimens for later in the course of therapy. This has led to recommendations to conserve PI-containing regimens, using those based on combinations of NRTIs and NNRTIs early in therapy. These considerations are reflected in the advice contained in the draft WHO Antiretroviral Guidelines for Resource Limited Settings. The summary of regimens recommended in this document is reproduced as Table 1. Table 1. Recommended First-Line Antiretroviral Regimens in Adults Regimen ZDV/3TC plus EFV* or NVP* ZDV/3TC/ABC* ZDV/3TC** plus RTV enhanced PI or NFV Pregnancy Considerations - Substitute NVP for EFV in pregnant women or women for whom effective contraception cannot be assured - ABC safety data limited - LPV/r safety data limited - NFV: most supportive safety data Major Toxicities - ZDV-related anemia - EFV-associated CNS symptoms - Possible teratogenicity of EFV - NVP-associated hepatotoxicity and severe rash - ZDV-related anemia - ABC hypersensitivity - ZDV-related anemia - NFV-associated diarrhoea - IDV-related nephrolithiasis - PI-related metabolic side effects *ZDV/3TC is listed as the initial recommendation for dual NsRTI component based on efficacy, toxicity, clinical experience and availability of fixed dose formulation. Other dual NsRTI components can be substituted including d4T/3TC, d4T/ddI and ZDV/ddI depending upon country-specific preferences. ZDV/d4T should never be used together because of proven antagonism. ** RTV-PI includes IDV/r, LPV/r, and SQV/r. 4. What is the evidence for the efficacy and toxicity of anti-retroviral drug combinations that include abacavir? (Level 2 evidence) Abacavir is a fairly well-studied and widely used NRTI. It is the most potent single NRTI currently available, reducing HIV viral load (VL) by 1-5-2.0 logs when studied as monotherapy. Abacavir requires a minimal pill burden (one pill BID); the combination of abacavir with zidovudine and lamivudine can be given as a single tablet BID. Abacavir is 10 associated with a rare but potentially lethal toxicity, however: 3-5% of patients treated with abacavir in clinical studies have developed a severe hypersensitivity reaction, including fever, rash, malaise, nausea, vomiting, abdominal pain, and cough/dyspnea, that resolves with immediate discontinuation of the drug, but proves rapidly fatal with each successive dose. Once abacavir is stopped due to suspicion of this reaction, it should never be restarted. Most trials of abacavir have used the 300mg BID dosage in combination with at least two additional antiretroviral agents. This formulation has been studied in several different clinical settings: (1) as initial therapy; (2) as substitute for a protease inhibitor in simplifying an antiretroviral regimen that is successfully suppressing viral replication; (3) as intensification of a failing antiretroviral regimen; and (4) as part of rescue therapy in patients with viral rebound after numerous antiretroviral regimens. The antiretroviral efficacy of Abacavir in combination therapy has been studied in three randomized controlled trials involving treatment-naïve subjects (Spreen, 199922; Staszewski 200123; Jordan 200224). These trials are summarised in Attachment 1. Spreen randomized treatment-naïve patients to triple-NRTI therapy with ABC+ZDV+3TC vs. dual NRTI therapy with ZDV+3TC for 48 weeks, with the option adding open label ABC or other agents to failing regimens at 16 weeks. At week 16, 75% of pts in the ABC arm had undetectable viral loads vs. 35% in the dual-NRTI arm (p<0.001); 74% of pts in the ABC arm maintained suppression at week 48. To compare the potency of ABC-based triple NRTI therapy to that of PI-based therapy, Staszewski randomized 562 treatment-naïve patients to ABC+ IDV-placebo or IDV+ABCplacebo for 48 weeks. All patients also received open label Combivir (AZT+3TC). When antiretroviral efficacy was analyzed, regardless of baseline patient viral load, ABC+2NRTI was equivalent to IDV+2NRTI: 51% of each group had HIV VL<400 copies/mL at 48 weeks. A slightly higher proportion of patients randomized to indinavir vs abacavir had VL<50 c/mL (46% vs. 40%). Most notably, however, was the finding that patients with a baseline VL>100,000 copies/mL were less likely to have a VL<50c/mL at 48 weeks if randomized to Abacavir (31%) than if randomized to indinavir (45%). There was little difference in prevalence of clinical side effects, lab abnormalities, discontinuations, or study withdrawals between the abacavir-based and indinavir-based arms. Jordan conducted a randomized trial of open label ABC vs. IDV, each with ZDV+3TC, to study viral efficacy and adherence in 329 treatment-naïve patients (see Attachment 1). This study found a greater probability of 95% adherence with ABC vs. IDV (72% vs. 45%, p=0.001), as well as a dose response relationship between adherence and probability of VL<400c/mL at 48 weeks. In an intensification study, Katlama et al (2001)25 randomized 185 patients with detectable viral loads (above 400c/mL) on dual and triple-drug regimens to abacavir vs. placebo plus their stable background therapy for 48 weeks. Overall, patients receiving abacavir were significantly more likely than those on placebo to have a VL<400c/mL at 48 weeks (25% vs. 5% p,<0.001). However only 13% of patients in the Abacavir arm had VL<50c/mL (vs. 0% of patients in the placebo arm). Here, too, the magnitude of baseline VL played a role: in the Abacavir arm, 41% of patients with a baseline VL<5000c/mL had a VL<400c/mL at 11 week 48, vs. 9% of patients with a baseline VL>5000c/mL. Taken together, these three trials suggest that triple NRTI-therapy with ABC is (a) superior to dual-NRTI therapy in ART-naïve patients; (b) possibly equivalent to PI-based triple drug therapy in ART-naïve patients with moderate baseline VL; and (c) only modestly successful in intensifying a failing regimen. There are three open-label, randomized trials of abacavir as replacement for protease inhibitors in stable, suppressive triple-drug regimens (Clumeck, 200126; Katlama-TRIZAL, 200127; Martinez, 200228) (see Attachment 1). All three trials showed high rates of continued viral suppression in patients randomized to abacavir-based regimens; the study by Martinez showed the efficacy of abacavir to equal that of the non-nucleoside reversetranscriptase inhibitors efavirenz and nevirapine, when used to simplify successful, PIbased combination therapy. Three single-arm, retrospective studies (Khanna, 200029; Moyle, 200030; Tenorio, 200031) (see Table 1) examined the use of abacavir in treating patients with extensive antiretroviral experience and viral rebound on their current regimen (rescue therapy). The studies by Khanna and Tenorio showed disappointingly modest rates of viral suppression in highly antiretroviral-experienced patients. Moyle, by contrast, studied NNRTI-naïve patients failing PI-based regimens; 58% of those who received rescue therapy including efavirenz and abacavir demonstrated VL<500c/mL at 24 weeks, with a mean rise in CD4 count of 97 cells. In a prospective, open label, single arm study of ABC+ZDV+3TC given to PI-naïve, patients experiencing viral rebound on dual-NRTI therapy, Henry et al32 demonstrated moderately successful viral suppression at 48 weeks, with higher likelihood of failure among patients with a higher VL at study entry. Finally, two additional, open-label, single-arm, prospective studies examined novel uses of abacavir (see Attachments 1). Kirkland33 found a high rate of viral suppression among incarcerated, ART-naïve patients treated with ABC+ZDV+3TC given as two pills BID in directly-observed therapy (DOT). Chapuis34 treated 41 ART-naïve patients early in infection (antibody-positive with mean CD4 count 756/mm3 and mean VL 28,000c/mL ) for 72 weeks with a two-drug, NRTI+PI regimen consisting of abacavir + amprenavir, and found 70% of patients to have a VL<50c/mL at 72 weeks. 9. Comparative evidence on safety (See attachment 1 for results from clinical trials of abacavir): b. Adverse effects/reactions: Adults: nausea, malaise and/or fatigue, vomiting, diarrhoea, anorexia, insomnia and other sleep disorders, fever and/or chills, headache, severe sensitivity reactions (see below). Laboratory abnormalities (Grade 3 or 4): anaemia, neutropaenia; elevated liver function tests, and CPK elevations; elevations of blood glucose; elevated triglyceride elevations. Paediatric: nausea and vomiting, fever, headache, diarrhoea, rashes, anorexia. Laboratory abnormalities (Grade 3 or 4): anaemia, neutropenia; elevations in liver function tests, creatine kinase. 12 Warnings: Abacavir must not be used as a single agent to treat HIV or added on as a sole agent to a failing regimen. Fatal hypersensitivity reactions have been associated with therapy with abacavir. Patients developing signs or symptoms of hypersensitivity (which include fever; skin rash; fatigue; gastrointestinal symptoms such as nausea, vomiting, diarrhoea, or abdominal pain; and respiratory symptoms such as pharyngitis, dyspnoea, or cough) should discontinue abacavir as soon as a hypersensitivity reaction is suspected. To avoid a delay in diagnosis and minimize the risk of a life-threatening hypersensitivity reaction, abacavir should be permanently discontinued if hypersensitivity cannot be ruled out, even when other diagnoses are possible (e.g., acute onset respiratory diseases, gastroenteritis, or reactions to other medications). Abacavir must not be restarted following a hypersensitivity reaction because more severe symptoms will recur within hours and may include life-threatening hypotension and death. Severe or fatal hypersensitivity reactions can occur within hours after reintroduction of abacavir in patients who have no identified history or unrecognised symptoms of hypersensitivity to abacavir therapy. In clinical studies, approximately 5% of adult and paediatric patients receiving abacavir developed a hypersensitivity reaction. This reaction is characterized by the appearance of symptoms indicating multi-organ/body system involvement. Symptoms usually appear within the first 6 weeks of treatment with abacavir, although these reactions may occur at any time during therapy. Frequently observed signs and symptoms include fever; skin rash; fatigue; and gastrointestinal symptoms such as nausea, vomiting, diarrhoea, or abdominal pain. Other signs and symptoms include malaise, lethargy, myalgia, myolysis, arthralgia, oedema, pharyngitis, cough, dyspnoea, headache, and paraesthesia. Some patients who experienced a hypersensitivity reaction were initially thought to have acute onset or worsening respiratory disease. The diagnosis of hypersensitivity reaction should be carefully considered for patients presenting with symptoms of acute onset respiratory diseases, even if alternative respiratory diagnoses (pneumonia, bronchitis, pharyngitis, or flu-like illness) are possible. Physical findings include lymphadenopathy, mucous membrane lesions (conjunctivitis and mouth ulcerations), and rash. The rash usually appears maculopapular or urticarial but may be variable in appearance. Hypersensitivity reactions have occurred without rash. Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including abacavir and other antiretrovirals. A majority of these cases have been in women. Obesity and prolonged exposure to antiretroviral nucleoside analogues may be risk factors. Particular caution should be exercised when administering abacavir to any patient with known risk factors for liver disease; however, cases have also been reported in patients with no known risk factors. Treatment with abacavir should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations). Precautions: 13 Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and “cushingoid appearance” have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established. Drug Interactions: An increased methadone dose may be required in a small number of patients receiving abacavir. c) Variation in safety due to health systems and patient factors: Antiretroviral therapy cannot be successfully introduced in a healthcare system vacuum. However, facilities and personnel infrastructure can be expanded in parallel with the implementation of antiretroviral agent delivery programmes. Health care provider and patient education, an essential health care package, and the ability to do at least limited clinical and laboratory monitoring are all necessary to try to insure programmatic success. [WHO Draft Antiretroviral Guidelines for Resource Limited Settings, p. 2.] It is well established that the introduction of any antimicrobial therapy for an infectious disease is association with the induction and spread of drugs resistance as an inevitable consequence. Although an obvious concern, this is not a reason to delay introduction of large-scale antiretroviral therapy programmes. Rather, education of providers and patients, attention to drug adherence, monitoring the population for drug resistance, and institution of strategies to try to limit drug resistance are the components of an appropriate response. It is possible that the risk of the spread of resistant viral strains in the population may be balanced by the potential for the reduction of HIV transmission by the introduction of antiretroviral therapy. [WHO Draft Antiretroviral Guidelines for Resource Limited Settings, p. 15.] 10. Summary of available data on comparative cost and cost-effectiveness within the pharmacological class or therapeutic group: Cost of therapy The most recent list of price offers compiled by MSF lists two suppliers of abacavir: GlaxoSmithKline (UK) annual cost of treatment $US 1387 and Hetero (India), $US 2628. By comparison, zidovudine costs range from $US 180 (Ranbaxy) to $US 584 (GSK), lamivudine from $US 91 to 248; stavudine from $US 44 to $US 137; and didanosine from $US 190 to 891. However, it may be more appropriate to compare the price of abacavir with other drugs that are combined with dual nucleoside therapy, for instance nevirapine ($US 166 – 438), nelfinavir ($US 1380 – 3139) and efavirenz ($US 438 – 1040). 11. Summary of regulatory status of the medicine (in country of origin and preferably in other countries as well): TBA 12. Availability of pharmacopoieal standards: TBA 14 Attachment 1: Results of the trials of abacavir Pages 14 - 19 15 ATTACHMENT 1 RESULTS OF CLINICAL TRIALS OF ABACAVIR AUTHOR METHODS STUDY DETAILS Staszewski et al. 200123 CNAAB3005 RCT of safety, equivalence Open: combivir (ZDV+3TC) + Blind: IDV/placebo Q8h or ABC/placebo BID N= 562 ARV-naïve; HIV VL>10,000c/mL; CD4>100/mm3. Equivalence= 95% CI between –12% and +12% ‘Abacavir* Regimen BENEFITS Comparator Regimen % all pts w/HIV VL<400 copies/mL at 48 weeks: 51% --Similar rise in CD4 count between groups. --No difference in time to viral rebound regardless of baseline VL. % all pts w/HIV VL<50 copies/mL at 48 weeks: 40% 46% 95% CI (-15% ,+2%) 51% 95%CI (-9%, +8%) % of pts with baseline HIV VL>100,000 c/mL and HIV VL<50 c/mL at 48 weeks: 31% 45% 95% CI (-27% , 0%) TOLERABILITY AND ADVERSE EFEFCTS ‘Abacavir* Comparator Regimen Regimen No difference in most prevalent side effects (nausea, vomiting, malaise, headache), except for renal side effects: <1% for ABC group, 5% for IDV group Severe lab abnormalities: --ABC+ZDV+3TC: 16% --IDV+ZDV+3TC: 19% Discontinued study drug:: --ABC+ZDV+3TC: 17% --IDV+ZDV+3TC: 22% Deaths: --ABC+ZDV+3TC: 3 (1 hypersensitivity, 2 MI) --IDV+ZDV+3TC: 1 (heroin/cocaine overdose) Drop-outs: --ABC+ZDV+3TC: 99 (41 w/adverse events) --IDV+ZDV+3TC: 96 (50 w/adverse events) 16 Staszewski et al. 199835 CNAB2002 2 phase dose ranging study: Randomized, double-blind: ABC 100mg, 300mg, or 600mg BID to 24 weeks, then Open-label: ABC 300mg+ZDV 300mg+3TC 150mg BID to 48 weeks. N=60 ARV-naïve patients; VL>30,000 c/mL; CD4 >100/mm3. NB: based on interim analysis showing less ABC potency at 100mg, at four weeks, pts randomized to ABC 100mg BID were offered open-label ABC at higher doses; by 24 weeks, only 3 pts remained on 100mg dose. Katlama et al. 200125 CNA3002 RCT Of open-label stable background therapy (SBG) + blinded ABC vs. Placebo x 48 weeks.. N= 185 pts on >12 weeks SBG with HIV VL 400-50,000c/mL; CD4 >100/mm3 Most common SBG: ZVD/3TC (36%) 2NRTI + PI or NNRTI (21%) % of pts on ABC+ZDV+3TC with HIV VL<400 c/mL at 48 weeks (pooled from --Withdrawals due to adverse events during randomized phase: 4 (1 MI; 1 rhabdo; 2 all ABC doses) 65% No comparison arm % of pts on ABC+ZDV+3TC with HIV VL<50 c/mL at 48 weeks (pooled from all ABC doses) 43% No comparison arm --At four weeks, decrease in log10 VL among pts receiving 300mg or 600mg ABC (-1.55 and -1.61 respectively), were significantly greater than that achieved by 100mg ABC, but not significantly different from each other. --Differences between 300mg and 600mg doses of ABC remained insignificant at 24 weeks. --CD4+ cell counts increased a median of 118/mm3 over 48 weeks (range 62-186 cells). % Pts with HIV VL<400c/mL at 48 weeks 25% (p<0.001) 5% % Pts with HIV VL<50c/mL at 48 weeks 13% 0% hypersensitivity). --Grade 3-4 lab abnormalities during randomized phase: 6. --Withdrawals during open-label phase: 2 (nausea/vomiting and depression/skin rash). --Similar nature/frequency of adverse events in all dose groups; trend towards increased nausea and malaise with increased dose. 13 pts quit study due to 12 pts quit study due to AE AE 12% switch to open-label 37% switch to open by 48 weeks label by 48 weeks 52% complete 48 weeks 15% complete 48 as randomized weeks as randomized Overall 25% of participants prematurely discontinue study. 17 d4T/3TC (19%) ZDV/ddI (10%) --41% of pts on SBG+ABC with baseline VL<5000c/mL had VL<400 at 48 weeks vs. 9% of pts on SBG+ABC with BL VL>5000c/mL. --CD4 cells increased a median of 102/mm3 in pts on SBG+ABC vs. 57 in pts on SBG alone. 18 Author Spreen et al. 199922 CNAA3003 Clumeck et al. 200126 CNA30017 Study details RCT: Double blind ABC+ZDV+3TC vs. ZDV+3TC x 16 weeks; option to add open label ABC at 16 weeks, or to unblind, add other ART if VL>400 confirmed. Followed to 48 weeks. N= 173 ART-naïve. Open label, randomized trial of continued (2NRTI+PI) vs. 2NRTI+ ABC replacing PI N= 211 pts with HIV VL<50c/mL since starting stable ART consisting of NRTI+PI >6 months prior to entry. Abacavir regimen Comparator regimen % pts with HIV VL<400c/mL at 16 weeks: Tolerability and adverse events Trial reported in abstract form; no adverse event data. 75% (p<0.001) 35% 74% remain <400c/mL at 48 weeks. --No significant difference in median CD4 rise over 48 weeks between pts who received ABC and those who did not (150 and 152 /mm3 respectively). Treatment Failure (HIV VL>400c/mL or premature discontinuation of therapy) over 48 weeks 12% (p<0.03) failure due to AE: 8 virologic failure: 4 other failure: 0 23% failure due to AE: 14 virologic failure: 2 other failure: 8 --No significant difference in grade 3-4 lab abnormalities. --2% incidence of hypersensitivity in ABC group --Pts in ABC arm experienced significantly higher incidence of nausea, malaise, fatigue. 19 Khanna et al. 200029 (Swiss HIV Cohort Study) Single arm retrospective study of heavily pre-treated patients switched to salvage therapy with ABC+NNRTI+1 or 2 new PIs. N= 23 pts on HAART (2NRTI+PI), w/o exposure to ABC or NNRTI, with HIV VL>1000c/mL, and hx of median 4 drug changes since starting ART. --At six months, 2 patients (9%) had HIV VL<500c.mL, and 10 pts (43%) had decrease in HIV VL>0.5 log10. --Seven pts increased CD4 count >30% above baseline. --Of 20 pts analyzed, 18 harbored multiple PR and RT resistance mutations. No comparator arm. Eight pts dropped out of study (35%) -Five pts quit study due to adverse events (4 rash, 1 neuropathy) --Three pts quit due to non-response, including one with clinical progression (KS, CMV retinitis). 20 Author Study Details Benefits Abacavir Regimen Kirkland et al. 200233 (NZTA4007) Moyle et al. 200030 (from CNA3008 study) Open-label clinical trial (Single arm) of ZDV+3TC+ABC, given as 2 pills BID, as DOT for 24 weeks. N= 108 incarcerated, ARTnaïve pts with VL>400c/mL and CD4>50/mm3. Retrospective analysis of pts experiencing virologic failure on PI-based regimen, switched to salvage therapy including ABC+(EFV or NVP)+2, 3, or 4 additional drugs. N= 31 pts naïve to NNRTI and ABC, with detectable HIV VL and CD4<100/mm3 with a history of ART with at least 2 NRTI and PI. Comparator Regimen % of pts with HIV VL<400 c/mL at 24 weeks: 85% 68% (missing=failure) No comparator group. % of pts with HIV VL<50 c/mL at 24 weeks: 75% No comparator group. 62% (missing=failures) --Pts w/BL VL<100,000 c/mL were more likely to reach undetectability at 24 weeks. --Median CD4 increase 111/mm3 at 24 weeks % of Pts with HIV VL<500c/mL at 24 weeks: --ABC+EFV: 58% --ABC+NVP:11% Mean change in CD4 at 24 weeks: --ABC+EFV: +97.4 --ABC+NVP:+25.7 No comparator arm. --90% received 2 additional drugs; baseline characteristics similar between pts receiving EFV vs NVP; virologic response unrelated to BL CD4, VL, # drugs received, or sensitivity of virus to drugs received. Tolerability/Adverse Effects Abacavir Regimen Comparator Regimen 18 pts withdrew: --6 LTFU --4 virologic failure --4 adverse events (2 hypersensitivity) --2 withdrew consent --2 other --No difference in adverse events in EFV vs NVP group. --No ABC hypersensitivity reactions. --Five deaths, due to HIV progression 21 Henry et al 200132 (TARGET) Open label prospective Single arm 48 week trial of ABC+ZDV+3TC given as 2 pills BID to NRTIexperienced,PI-naïve pts with virologic failure. N=87 pts w/HIV VL<50,000c/mL; CD4>50/mm3 not currently receiving ZDV. Most common Baseline ART: 3TC+d4T (61%); d4T+ddI (19%) Tenorio et al. 200031 Retrospective analysis of salvage regimens including both ABC+EFV (grouped into a single arm) in heavily ARTexperienced clinic pts. N= 37 pts identified; only the 29 who remained on meds for >4 weeks analyzed. Mean CD4 115/mL; VL 5.14 log10 c/mL;Mean # prior regimens 5; mean # new drugs started 3. Abacavir Regimen Comparator Regimen % of pts with undetectable HIV VL at 48 weeks: <400c/mL: --82% (ITT=observed) --52% (ITT M=F) --Median change inCD4 at 48weeks: +66/mm3 No comparator regimen. --pts with virologic failure had higher baseline HIV VL than those who maintained suppression. --M184V mutation at BL not associated with virologic outcome; TAMs at BL more common in pts w/ virologic failure. Outcomes at one year: No comparator regimen <50c/mL: --56% (ITT=observed) --36% (ITT M=F) --2 pts w/ HIV VL<50 c/mL --11 pts (38%) had sustained virologic response (not specified) at one year; associated w/ fewer prior regimens, greater initial drop in viremia. --13 pts (45%) had increased CD4 count at one year (median +60/mm3). Abacavir Regimen Comparator Regimen --15% rate of withdrawal from study (nausea, malaise, fatigue, vomiting most common) --3.4% with ABC hypersensitivity. --Clinical failure in 20 pts (69%). --9 pts w/ clinical progression of disease (non-responders). --3 deaths due to disease. --31 pts w/ adverse rxns --8 pts (22%) discontinued at least one drug. --one ABC hypersensitivity. No comparator regimen 22 Chapuis et al. 200034 (CNAB2006) Virologic efficacy at 72 weeks: Nonrandomized, open label, observational, prospective trial Of ABC+AMP for 72 weeks in ART-naive pts. N= 41 pts with VL>5000c/mL; CD4 >400/mm3. At baseline, mean CD4 756/mm3; mean HIV VL 4.45 log10 c/mL. Author: Martinez et al. 200228 Study Details: Randomized open label Regimen simplification trial of pts with suppressed VL on PI+2NRTI randomized to replace PI with ABC, NVP or EFV for 12 months. N= 460 pts with HIV VL<200c/mL for >6 months on ART consisting of at least one PI+2NRTI.. --% pts w/ HIV VL < 50 c/mL: 70% No comparator regimen --% pts w/ HIV VL < 5 c/mL: 39%. --Mean change in CD4 count: +240/mm3 Benefits: Abacavir Regimen Comparator Regimen % of Pts with HIV VL<200c/mL at 12 months: ABC+2NRTI: 77% (p=0.7 for main comparison) NVP+2NRTI: 78% EFV+2NRTI: 74% Mean change in CD4 count at 12 months: +51/mm3. Mean change in CD4 count at 12 months: +41/mm3 (NVP); +51/mm3 (EFV). 7 pts (17%) withdrew prematurely: --4 w/ protocol defined adverse events (2 rash; 1 chemical pancreatitis; 2 ABC hypersensitivity). --3 voluntarily --2 LTFU @ 72 wks. --no clinical lipodystrophy Tolerability/Adverse Events: Abacavir Regimen Comparator Regimen % of pts who discontinued due to AEs: ABC+2NRTI: 6% (p=0.009 for main comparison) NVP+2NRTI: 16% EFV+2NRTI: 17% 23 Jordan et al. 200224 (CNA3014) Author: Katlama et al. 200127 (TRIZAL) Randomized open label viral efficacy and adherence trial Of ABC+ZDV/3TC vs. IND+ZDV/3TC in ART-naive pts for 48 weeks. N329 ART-Naïve Pts. Study Details: Randomized, open label trial Of Trizivir (combined ABC+ZDV+3TC) vs. continued HAART for 48 weeks. 209 pts with HIV VL<50 c/mL on HAART and no hx of prior virologic failure. Most common prestudy regimen: PI+2NRTI (63%). Abstract does not provide CD4, VL data from before pretrial ART was started. Efficacy and adherence at 48 weeks: Pts reporting difficulty taking regimen: pts w/ 95% adherence with HIV VL<400c/mL: 86%. pts w/ 95% adherence with HIV VL<400c/mL: 77%. 9% (p<0.001 for comparison) Pts w/95% adherence: 72% (P.001 for comparison). Pts w/95% adherence: 45% Benefits: Abacavir Regimen Comparator Regimen Pts with treatment failure (defined as 2 consecutive HIV VL>400c/mL or premature discontinuation of randomized therapy) at 24 weeks: 20% 36% 17% Tolerability/Adverse Events: Abacavir Regimen Comparator Regimen --Adverse events were most likely reason for treatment discontinuation in both arms. --10% incidence of ABC hypersensitivity in Trizivir arm. --Pts report Trizivir easier to take than continued HAART (p<0.0001). 24 Attachment 2 Characteristics of nucleoside reverse transcriptase inhibitors Two nucleoside analogue reverse transcriptase inhibitors (NRTIs) usually form the “backbone” of all currently recommended antiretroviral regimens. NRTIs were the first class of antiretroviral drugs to be introduced; consequently the most extensive clinical experience is recorded about these drugs. Presently ABC is usually ‘added on’ to the nucleoside core. Advantages Disadvantages *potent, durable antiretroviral activity when combined with a protease inhibitor or a nonnucleoside reverse transcriptase inhibitor * adverse events associated with long-term antiretroviral use, but a causal relationship has yet to be established * clinical benefit established, confirming validity of surrogate marker improvement * hypersensitivity reactions are severe and sometimes fatal * resistance profile of recommended dual NRTIs allows for 2nd line combination Non-proprietary name Cost p.a. US $ Advantages Disadvantages zidovudine $180 (Ranbaxy, India) to $584 (GlaxoSmith Kline, UK) * penetrates blood/brain barrier; * resistance profile allows for 2nd and possibly 3rd line NRTI combination; * twice-daily dosing; * can be taken with or without food; * compounded formulations with lamivudine; lamivudine and abacavir; and lamivudine and nevirapine available; * few drug interactions; * can be administered with rifampin *anaemia; *high level resistance to zidovudine usually confers resistance to abacavir; 25 lamivudine $66 (Aurobindo, India) to $234 (Glaxo SmithKline, UK) *very well tolerated; *twice-daily dosing and long half-life means potential for once-daily dosing; * can be taken with or without food; *active against hepatitis B virus; * resistance profile allows for 2nd and possibly 3rd line NRTI combination; * compounded formulations with zidovudine; zidovudine and abacavir; zidovudine and nevirapine available; * no significant drug interactions; * can be administered with rifampin *single mutation at codon 184 of reverse transcriptase can confer high-level resistance; didanosine $197 (Aurobindo, India) to $650 (GPO, Thailand) *twice-daily dosing but long half-life allows for once daily dosing; * delayed-release, enteric-coated formulation available; * can be administered with rifampin; * few drug interactions; * buffered formulation must taken on an empty stomach; * peripheral neuropathy; * fatal and nonfatal pancreatitis have occurred during therapy when didanosine was part of a combination regimen that included stavudine stavudine $31 (Aurobindo, India) to $137 (FarManguinh, Brazil) * well-tolerated; * twice daily dosing; * can be administered with rifampin; * few drug interactions; * peripheral neuropathy; * fatal and nonfatal pancreatitis have occurred during therapy when didanosine was part of a combination regimen that included stavudine abacavir $1387 (Glaxo SmithKline, UK) to $2628 (Hetero, India) * twice-daily dosing; *compounded formulation with zidovudine and lamivudine available; * penetrates blood/brain barrier; *can be used with rifampin; *no significant drug interactions; * serious, potentially fatal hypersensitivity reaction reported in 5% of clinical trials subjects; 26 1 Blatt SP et al. Total lymphocyte count as a predictor of absolute CD4+ count and CD4+ percentage in HIV-infected persons. JAMA 1993 Feb 3;269(5):622-6 2 French N, Mujugira A, Nakiyingi J, Mulder D, Janoff EN, Gilks CF. Immunological and clinical staging in HIV-1-infected Ugandan adults are comparable and provide no evidence of rapid progression but poor survival with advanced disease. J AIDS 1999;22:509-516 Joint United Nations Programme on HIV/AIDS. ‘AIDS epidemic update -- December 2001.’ Available at: http://www.unaids.org/epidemic_update/report_dec01/index.html 3 4 AIDS Drug Policy. Ministry of Health Brazil. Available at http://www.aids.gov.br/assistencia/aids_drugs_policy.htm 5 Improving access to antiretroviral therapy in Latin America. reference to Argentina program. Family Health International. Available at http://www.fhi.org/en/aids/impact/iohiv/ioh11/ioh16.html 6 Djomad G, Roels T, Chorba T, Diomandé F, Nkengasong J, Monga B, Maurice C, Wiktor SZ. HIV/AIDS Drug Access Initiative: Preliminary report covering the period August 1998-March 2000. Ministère de la Santé, Programme National de Lutte contre le SIDA/MST/TUB, République de Côte d’Ivoire, May 2000. Available at: www.unaids.org/publications/documents/care/UNAIDS_DAI/cote_ivoire_drug_access_initiative.doc 7 Source: Laurent C, Diakhaté N, Ngom Gueye NF, Touré MF, Sow PS, Faye MA, Gueye M, Lanièce I, Touré Kane TC, Liégeois F, Vergne L, Mboup S, Badiane S, Ndoye I, Delaporte E. The Senegalese government HAART initiative: an 18month follow- up study of feasibility, effectiveness, adherence, toxicity and viral resistance. [Abstract and Poster 460-W] 9th Conference on Retroviruses and Opportunistic Infections, Seattle, Washington, USA, February 24 - 28, 2002. d’Adesky A-C, HIV meds come to rural Haiti, The AmFAR Treatment Insider, October-November 2001 2(5):5-8. Available at: http://199.105.91.6/treatment/HIV+/insidermenu.html. 8 9 S. Pujari, E. Naik, A. Patel, and S. Bhagat. Safety, Tolerability, and Efficacy of Nevirapine-Based HAART amongst Antiretroviral Naïve HIV-1-Infected Patients in India. Paper presented at the 9th Retrovirus Conference, Washington State Convention and Trade Center, Seattle, February 24th-28th 2002. Available at www.retroconference.org World Health Organization. ‘Scaling up antiretroviral therapy in resource-limited settings: Guidelines for a public health approach’. WHO 2002. 10 11 National Health and Medical Researcg Council of Australia. How to use the evidence: assessment and application of scientific evidence. Available at: http://www.nhmrc.gov.au/publications/pdf/cp69.pdf 12 Gilbert, PB et al. Virologic and Regimen Termination Surrogate End Points in AIDS Clinical Trials. JAMA 2001; 285: 777-784 13 Skowron, G. Base Line CD4 Cell Count, Not Viral Load, Correlates with Virologic Suppression Induced by Potent Antiretroviral Therapy. Journal of Aquired Immune Deficiency Syndrome 2001; 28: 313-319 14 Hill, AM et al. Meta-Analysis of Antiretroviral Effects on HIV-1 RNA, CD4 Cell Count and Progression to AIDS or Death. Antiviral Therapy 1998; 3: 139-145. 15 Babiker A et al. Human immunodeficiency virus type I RNA level and CD4 count as prognostic markers and surrogate end points: a meta-analysis. AIDS Research and Human Retroviruses 2000; 16: 1123-1133. Carpenter, CCJ et al. Antiretroviral Therapy in Adults: Updated Recommendations of the International AIDS Society – USA Panel (Consensus Statement). JAMA: 2000; 283: 381-390 16 17 Gallant, JE. Strategies for Long-term Success in the Treatment of HIV Infection. JAMA 2000; 283: 1329-1334 27 18 World Health Organization. Safe and Effective Use of Antiretroviral Treatments in Adults with particular reference to resource limited settings. WHO/HSI/2000.04 19 Rutherford, GW et al. Three- or Four- versus Two-Drug Antiretroviral Maintenance Regimens for HIV Infection. Cochrane Database of Systematic Reviews. Issue 1, 2002 20 Darbyshire, J et al. (AZT) versus AZT plus didanosine (ddI) versus AZT plus zalcitabine (ddC) in HIV Infected Adults. Cochrane Database of Systematic Reviews. Issue I, 2002 21 Jordan et al. Systematic review and meta-analysis of evidence for increasing numbers of drugs in antiretroviral combination therapy. BMJ 2002;324: 1-10 22 Spreen B, Greenberg S, Lafon S, Clumeck N, Peters B, Fischl M, Rubio R, Gould J, Boone G, West M. Ziagen (abacavir, ABC, 1592) combined with 3TC & ZDV is highly effective and durable through 48 weeks in HIV-1 infected antiretroviral-therapy-naive subjects (CNAA3003). In: 6th Conference on Retroviruses and Opportunistic infections; 1999 Jan 31-Feb 4 1999; 1999. 23 Staszewski S, Keiser P, Montaner J, Raffi F, Gathe J, Brotas V, et al. Abacavir-lamivudine-zidovudine vs indinavirlamivudine-zidovudine in antiretroviral-naive HIV-infected adults: A randomized equivalence trial. Jama 2001;285(9):1155-63. 24 Jordan J, P. Cahn, and A. Vibhagool for the CNA3014 Study Team. Predictors of Adherence and Efficacy in HIV-1Infected Patients Treated with Abacavir/Combivir (ABC/COM) or Indinavir/Combivir (IDV/COM): Final 48-Week Data from CNA3014. In: 9th Conference on Retroviruses and Opportunistic infections; 2002 Feb 24-29, 2002; Seattle, WA; 2002. 25 Katlama C, Clotet B, Plettenberg A, Jost J, Arasteh K, Bernasconi E, et al. Intensification of stable background therapy with abacavir in antiretroviral therapy experienced patients: 48-week data from a randomized, double-blind trial. HIV Med 2001;2(1):27-34. 26 Clumeck N, Goebel F, Rozenbaum W, Gerstoft J, Staszewski S, Montaner J, et al. Simplification with abacavir-based triple nucleoside therapy versus continued protease inhibitor-based highly active antiretroviral therapy in HIV-1-infected patients with undetectable plasma HIV-1 RNA. Aids 2001;15(12):1517-26. 27 Katlama C, Clumeck N, Fenske S, Mallolas J, Lafeuillade A, Beauvais L. Use of Trizivir to simplify therapy in HAARTexperienced patients with long-term suppression of HIV-RNA: TRIZAL study (AZL30002)--24 week results. In: 8th Conference on Retroviruses and Opportunistic Infections; 2001 Feb 4-8, 2001; Chicago, IL; 2001. 28 Martinez I, D. Podzamczer, E. Ribera, P. Domingo, H. Knobel, D. Dalmau, M. Riera, E. Pedrol, L. Force, J. Llibre, F. Segura, C. Richart, C. Cortes, M. Javaloyas, M. Aranda, and J. M. Gatell. Switching Protease Inhibitors to Nevirapine (NEV), Efavirenz (EFA) or Abacavir (ABA): A Randomized, Multicenter, Open-Label, Simplification Trial. In: 9th Conference on Retroviruses and Opportunistic Infections; 2002 Feb 24-28, 2002; Seattle, WA; 2002. 29 Khanna et al. Salvage therapy with abacavir plus a non-nucleoside reverse transcriptase inhibitor and a protease inhibitor in heavily pre-treated HIV-1 infected patients. Swiss HIV Cohort Study. AIDS 2000;14:791-799. 30 Moyle et al. Salvage therapy with abacavir plus efavirenz or nevirapine in HIV-1-infected persons with previous nucleoside analogue and protease inhibitor use. AIDS 2000;14:1453-1454. 31 Tenorio AR, Irlanda IE, Narkiewicz E, Smith KY, Kessler HA, Sha BE. Efficacy and safety of the combination of efavirenz and abacavir in HIV- infected patients failing antiretroviral therapy. Aids 2000;14(10):1470-1. 32 Henry K, Wallace RJ, Bellman PC, Norris D, Fisher RL, Ross LL, et al. Twice-daily triple nucleoside intensification treatment with lamivudine- zidovudine plus abacavir sustains suppression of human immunodeficiency virus type 1: results of the TARGET Study. J Infect Dis 2001;183(4):571-8. 28 33 Kirkland LR, Fischl MA, Tashima KT, Paar D, Gensler T, Graham NM, et al. Response to lamivudine-zidovudine plus abacavir twice daily in antiretroviral-naive, incarcerated patients with HIV infection taking directly observed treatment. Clin Infect Dis 2002;34(4):511-8. 34 Chapuis A, Rizzardi, G.P., Pantaleo, G., Lazzarin, A., McDade, H., Spreen, W., Steel, H., Vafdis, I., Meylan, P., Bart, P.A., Meuwly, J.Y., Corpataux, J.M., Weibon, C., Graziosi, C., Chave, J.P., Gallant, S. Combination Ziagen (abacavir/ABC)/amprenavir(141, APV-USAN) therapy in HIV-1 infected antiretroviral naive subjects with CD4+ counts>400 cells/microliter and plasma HIV-1 RNA>5000 copies/mL. In: 6th Conference on Retroviruses and Opportunistic Infections; 1999 Jan 31-Feb 4, 1999; 1999. 35 Staszewski S, Katlama C, Harrer T, Massip P, Yeni P, Cutrell A, et al. A dose-ranging study to evaluate the safety and efficacy of abacavir alone or in combination with zidovudine and lamivudine in antiretroviral treatment-naive subjects. Aids 1998;12(16):F197-202.