* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Circulatory System
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
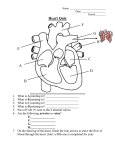
The Circulatory System What does our heart do? Monitoring your pulse • Find pulse in your wrist (the pulse you feel is blood rushing through the brachial artery in your arm) – Count the number of heartbeats in 30 seconds. Multiply this number by 2 to calculate your heart rate for 1 min. • Find pulse on side of your neck (the pulse you feel is blood rushing through the carotid artery – the one that carries blood to your head) – Calculate heart rate for 1 min. Compare the strength of the pulse in your carotid artery with your brachial artery. What do you notice? Why? Pulse: change in the diameter of the arteries following heart contractions • Run on the spot for 2 minutes. • Take your pulse immediately for 30 seconds after exercise using either the carotid or brachial artery. Calculate your heart rate for 1 min. • Compare your heart rate before and after exercise. What do you notice? • Do you think the difference between resting heart rate and the heart rate after exercise would be greater for athletes? Why or why not? The Circulatory System • Consists of the heart, blood vessels, and blood • Fundamental purpose is to transport substances from place to place in the body via the blood • Blood vessels ensure the proper routing of blood to its destinations • Heart is the pump that keeps the blood flowing Functions of the Circulatory System • 3 main functions – Transport – Protection – Regulation Transport • Blood carries oxygen from the lungs to all of the body’s tissues, while it picks up carbon dioxide from those tissues and carries it to the lungs to be removed from the body • It picks up nutrients from the digestive tract and delivers them to all of the body’s tissues • Carries metabolic wastes to the kidneys for removal • Carries hormones from endocrine cells to their target organs Protection • The blood plays several roles in inflammation, a mechanism for limiting the spread of infection • White blood cells destroy microorganisms and cancer cells • Antibodies and other blood proteins neutralize toxins and help to destroy pathogens • Platelets secrete factors that initiate blood clotting and other processes for minimizing blood loss Regulation • Controls body temperature – homeostasis • By absorbing or giving off fluid under different conditions, the blood capillaries help to stabilize fluid distribution in the body • By buffering acids and bases, blood proteins neutralize toxins and help to destroy pathogens • Platelets secrete factors that initiate blood clotting and other processes for minimizing blood loss So.. Why is an excessive loss of blood quickly fatal? • We need our blood to efficiently transport nutrients, wastes, hormones and especially oxygen from place to place Components and Properties of Blood • Adults generally have about 4 to 6 litres of blood • It is a liquid connective tissue composed of cells and an extracellular matrix – the matrix is the blood plasma which is a clear, light yellow fluid making up a little over half of our blood volume • Suspended in the plasma are the formed elements (RBCs, WBCs, and platelets) Components of Blood Hematocrit: Ratio of red blood cell volume to the total blood volume Formed Elements • Erythrocytes (red blood cells, RBCs) – Densest of the elements, constitute about 37% to 53% of total blood volume – Contain hemoglobin, which increases the capacity of oxygen that can be carried in the blood – Two principal functions: 1) to pick up oxygen from the lungs and deliver it to tissues elsewhere, and 2) to pick up carbon dioxide from the tissues and unload it in the lungs Formed Elements • Leukocytes (white blood cells, WBCs) – 5 types of leukocytes • Granulocytes- Neutrophils, Eosinophils, Basophils • Agranulocytes- Lymphocytes, Monocytes – Total 1% or less of total blood volume (ratio of 700 RBCs to 1 WBC) – Form special proteins, called antibodies, which interfere with invading microbes and toxins – Important part of the immune system Formed Elements • Platelets – Included with WBCs in the total 1% or less of blood volume – Component of blood responsible for initiating blood clotting • Blood will not clot unless blood vessel is broken • Substances released by the broken blood vessel will attract platelets Anemia • A condition in which an individual does not have enough healthy red blood cells to carry adequate oxygen to the tissues • Causes weakness and fatigue • Can be temporary or long-term, and can range from moderate to severe • Prevention: eating a healthy, varied diet • Treatment: supplements Blood Groups • Blood types A, B, AB and O are determined by the hereditary presence or absence of antigens A and B on the RBCs • Universal Donor Type O blood • Universal Acceptor Type AB blood Table 1: Antigens and Antibodies Found in Blood Groups p. 247 in textbook Rhesus Factor • During the 1940s , scientists discovered another antigen on the red blood cell: the Rh group (named after the rhesus monkey) • Rh group is also inherited – Individuals who have this special antigen (approx. 85% of Canadians) are said to be Rh-positive • Individuals who are Rh-negative may donate blood to Rh-positive individuals, but should not receive their blood Blood Vessels • Arteries – Carry oxygenated blood away from heart • Capillaries – Connect the smallest arteries to the smallest veins • Veins – Carry deoxygenated blood to heart Blood Vessels • Arteries – Every time the heart contracts, blood surges from the heart and enters the arteries – The arteries stretch to accommodate the inrush of blood – Blood from the arteries passes into smaller arteries, called arterioles Blood Vessels • Walls of the arteries become narrow when fat deposits along the artery wall • Arterial size can also change during warm and cold temperatures winter weather constricts the arterial size while hot weather causes dilation of artery wall • Blood flow through arteries is affected by changes in arterial wall diameter • Decreasing arterial size causes elevation of blood pressure levels and strains the heart to do more work, thus increasing the risk for a heart attack Blood Vessels • Capillaries – Materials such as nutrients, wastes, hormones and leukocytes pass between the blood and the tissue fluids, through the walls of capillaries – Capillaries are sometimes called exchange vessels Blood Vessels • Veins – Unidirectional blood flow back to heart • Valves- open in one direction, steering blood toward the heart – they do not allow blood back in the other direction – Diameter of veins increases as blood returns to the heart – As much as 50% of total blood volume can be found in the veins Atherosclerosis • Growth of lipid deposits in the arterial walls • Deposits can become calcified plaques, giving the arteries a hard, bonelike consistency • As a result of these degenerative changes, blood pressure rises with age Predict-Observe-Explain How does the size of blood vessels affect blood pressure? Blood Pressure • The force that the blood exerts against a vessel wall • Fluctuations can be created due to increased demands on the body – how readily the body reverts back to a normal level is indicative on one’s overall fitness • Systolic pressure is the peak arterial BP attained during ventricular contraction • Diastolic pressure is the minimum arterial BP occurring during the ventricular relaxation between heartbeats • Arterial BP is written as a ratio of systolic over diastolic pressure: 120/75 mm Hg is normal average – measured using a sphygmomanometer Hypertension • Chronic high blood pressure – Causes: • Physical inactivity • A salt-rich diet through processed and fatty foods • Alcohol and tobacco use • Plaque build up in arteries can cause damage to platelets and can start to lead to a blood clot (embolism) • Treatment: – Exercise, better diet and medications (Asprin: helps prevent platelets from sticking to one another) – Surgery: Angioplasty- fine plastic tube inserted into artery and when a constricted region is identified a balloon is blown up to force the vessel open. Coronary bypass - involves removing a segment of healthy blood vessel from one part of your body and using it to go around a blockage near the heart. (The term double or triple refers to the number of blood vessels containing blockages that must be bypassed. (p.258, fig. 3) Discoveries • Ancient Greeks – Heart was seat of intelligence • Galen (Greek physician) – In second century theorized that blood and veins were separate and blood flowed out of each to the body • William Harvey – In seventeenth century theorized that we have a cyclic circulatory system. He was never able to find the point where blood stopped travelling away from the heart and travelled back • Marcello Malpighi – In 1657 identified capillaries to back Harvey’s findings The Mammalian Heart • The Pulmonary and Systemic Circuits – The two major divisions of the cardiovascular system Pulmonary Circuit- carries blood to the lungs for gas exchange and returns it to the heart Systemic Circuit- supplies blood to every organ of the body, including other parts of the lungs and the wall of the heart itself heart arteries capillaries veins heart The Mammalian Heart • Right side – Supplies the pulmonary circuit – Receives blood that has circulated through the body, unloaded its oxygen and nutrients, and picked up a load of carbon dioxide and other wastes – Pumps oxygen-poor blood into a large artery, the pulmonary trunk, which immediately divides into right and left pulmonary arteries – These transport blood to the air sacs (alveoli) of the lungs, where carbon dioxide is unloaded and oxygen is picked up – The oxygen –rich blood then flows by way of the pulmonary veins to the left side of the heart • Left side – – – – Supplies the systemic circuit Blood leaves it by way of another large artery, the aorta The aortic arch gives off arteries that supply the head, neck and upper limbs After circulating through the body, the now deoxygenated systemic blood returns to the right side of the heart, mainly by way of two large veins: the superior vena cava (draining the upper body) and inferior vena cava (draining everything below the diaphragm) Heart Chambers • 4 chambers – The two superior chambers are the right and left atria: they are thin-walled receiving chambers for blood returning to the heart by way of the great veins – The two inferior chambers are the right and left ventricles: they are the pumps that eject blood into the arteries and keep it flowing around the body Heart Valves • To pump blood effectively, the heart needs valves that ensure a one-way flow • There is a valve between each atrium and its ventricle and another at the exit from each ventricle into its great artery • The atrioventricular (AV) valves regulate the openings between the atria and ventricles • The semilunar valves (pulmonary and aortic valves) regulate the flow of blood from the ventricles into the great arteries • The Lub-Dub sound your heart makes is due to these valves opening and closing in the heart – Lub AV valves – Dub Semilunar valves The Mammalian Heart Control of the Heart – The impulse that causes the heart to beat is actually in the heart itself • A bundle of special muscle tissue, located in the right atrium, stimulates muscle fibers to contract and relax rhythmically. • This tissue is called the sinoatrial (SA) node AKA the pacemaker • SA node gives electrical impulse to both atria and causes them to contract simultaneously • The pulse will then reach the atrioventricular (AV) node located between the two ventricles to start their contraction Recording a Heart Rate – Electrocardiograph (ECG) shows the duration of a single beat – Small voltage increase as the electrical depolarization that accompanies contraction of the atria (P) – Large spike accompanies the contraction of the ventricles • Ventricular depolarization (QRS) – As the ventricles recover another small spike shows the electrical repolarization that precedes the next firing of the SA node (T) – Ventricular fibrillation – ventricles contract randomly • Can be sometimes stopped. A strong electrical current to the heart and SA node can take over again. Electrocardiogram- ECG Heart Rate & Fitness • • Maximum heart rate is the fastest your heart can possibly beat during activity, which decreases as you get older Fitness relation is not in how many beats but in the length of time it takes your heart to go from maximum to resting level after activity Stroke Volume & Fitness 1. How easily the heart fills with blood • Depends on volume of blood returning in veins and the distensibility or “stretchiness” of the ventricles 2. How readily the heart empties • Depends on strength of ventricular contraction and pressure exerted by artery walls • Cardiovascular exercise enlarges the ventricular chambers, increases distensibility of ventricles and strengthens ventricular walls • Strength training may simply increase thickness of ventricular walls and limit stroke volume by reducing elasticity Heart Defects • Septal defect- hole in the septum (separates right and left ventricles) – Oxygenated and deoxygenated blood are able to mix Heart Defects • Murmurs- one or more of heart valves not closing properly • Arrhythmias- irregular heartbeat – When a coronary artery is blocked, it delivers less blood and causes the heart to beat in an irregular pattern • Too slow heart rate (bradycardia) • Too fast heart rate (tachycardia) Lymphatic System • Consists of a network of vessels that penetrate nearly every tissue of the body, and a collection of tissues and organs that produce immune cells • 3 main functions; – Fluid recovery – Immunity – Lipid absorption Lymphatic System • Fluid Recovery – Fluid continually filters from blood capillaries into the tissue spaces – Lymphatic system reabsorbs excess water that blood capillaries do not absorb and returns it to the blood – Even partial interference with lymphatic drainage can lead to severe edema Lymphatic System • Immunity – As the lymphatic system recovers tissue fluid, it also picks up foreign cells and chemicals from the tissues – On its way back to the blood stream, the fluid passes through lymph nodes, where immune cells stand guard against foreign matter – When they detect anything potentially harmful, they activate a protective immune response Lymphatic System • Lipid absorption – In the small intestine, special lymphatic vessels called lacteals absorb dietary lipids that are not absorbed by the blood capillaries Lymphatic System Components of the Lymphatic System • 1) Lymph, the recovered fluid • 2) Lymphatic vessels, which transport the lymph • 3) Lymphatic tissue (lymph nodes are round masses of tissue that supplies lymphocytes to the bloodstream and remove bacteria and foreign particles from the lymph) • 4) Lymphatic organs – Spleen: acts as a reservoir for blood and a filtering site for lymph – Thymus gland: where lymphocytes mature, multiply and differentiate (lymphocytes are WBCs that produce antibodies) Elephantiasis A disease caused by lymphatic obstruction