* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Auditory Pathways
Survey
Document related concepts
Noise-induced hearing loss wikipedia , lookup
Calyx of Held wikipedia , lookup
Sound from ultrasound wikipedia , lookup
Evolution of mammalian auditory ossicles wikipedia , lookup
Auditory processing disorder wikipedia , lookup
Sensorineural hearing loss wikipedia , lookup
Transcript
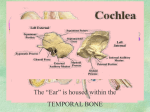
Neuroanatomy: Auditory Pathways (Pan) AUDITORY SYSTEMS AND SOUND WAVES: Auditory System: transmits information about sound waves in the environment to the CNS Sound Waves: alternating air pressure o Properties of Sound: Frequency (Hz): determines the pitch of the sound Human range of hearing is 20-20,000 Hz Most sensitive in the 1000-3000 Hz range Females can hear higher frequencies than males Amplitude (dB): determines the loudness of sound; decibels is a logarithmic scale dB= 10 log [(intensity of sound)/(intensity of standard sound)] dB= 20 log [(pressure of sound)/(pressure of standard sound) 0 dB is the threshold for human hearing At 140 dB, sounds are both felt and heard TRANSDUCTION OF SOUND INTO ELECTRICAL EVENTS: Three Components to the Auditory Apparatus: 1. External Ear: Separated from middle ear by tympanic membrane (eardrum) Tympanic membrane receives airborne vibrations External auditory canal acts like a resonator (natural frequency of about 3000 Hz) 2. Middle Ear: Chain of 3 ossicles: malleus, incus and stapes o Transmit vibration movement of the tympanic membrane to the movement of the face plate of the stapes (attached to oval window of cochlea- inner ear) Amplification and Impedance-Matching Device: o Differences in the amplitude of the movement and the surface area between tympanic membrane and face plate of the stapes cause 22 times more pressure to be placed on the cochlear fluid as was exerted by the sound wave on the tympanic membrane Attenuation Reflex: o Loud sounds being transmitted through CNS result in this reflex (10 ms latency) o Reflex causes contraction of the tensor tympani and stapedius muscles which oppose one another, causing rigidity in ossicular system- dampens movements (decreases sensitivity) Natural Resonant Frequency of Ossicular Chain: between 700 and 1400 Hz o Combined with the external auditory canal, transmission of sound from air to cochlea is good between 600-6000 Hz (fades above and below these limits) 3. Inner Ear: Cochlea: auditory portion of the inner ear o Fluid-filled coiled tube that is 3cm long (coiled 2.5 times around the modiolus) o Scala Media: central cavity containing endolymph (like ICF- high K+, low Na+) Contains the Organ of Corti o Scala Vestibuli: in contact with the oval window; contains perilymph (like ECF- high Na+, low K+) Separated from the scala media by Reissner’s membrane Connected to the scala tympani by a small opening at the apex called the helicotrema o Scala Tympani: in contact with the round window; contains perilymph Separated from the scala media by the basilar membrane o Movements: Inward movement of stapes increases fluid pressure in the scala vestibuli Displaces the basilar membrane and causes a subsequent increase in the pressure of the scala tympani Causes bulging of the round window into the middle ear Basilar Membrane: o Contains cross striations- narrow and stiff at the base (high frequencies resonate here), wide and more flexible at the apex (low frequencies resonate here) Organ of Corti: o Rests on the basilar membrane o Receptor organ that generates nerve impulses in response to vibrations of the basilar membrane Hair Cells: sensory receptor cells located in the Organ of Corti o o Two Types: Inner Hair Cells: single row, responsible for processing sound Outer Hair Cells: 3-4 rows, responsible for amplification/moderating the inner hair cells; separated from inner hair cells by a supporting arch Generation of Sound Impulses: Minute hairs project from hair cells and contact tectorial membrane Bases of hair cells associated with endings of cochlear nerve fibers (cell bodies in spiral ganglion of modiolus) Movements of basilar membranes causes shearing of hairs resulting in either depolarization or hyperpolarization Movement of hairs towards kinocilium results in the opening of K+ channels and depolarization; results in influx of Ca++ and release of NT onto afferent cochlear nerves (initiates action potential) Movement of hairs away from kinocilium results in closing of K+ channels and hyperpolarization MAJOR NUCLEAR CENTERS AND PATHWAYS: Spiral Ganglion: located in the modiolus of the cochlea Peripheral processes of ganglion cells receive inputs from Organ of Corti hair cells Central processes of the ganglion form the cochlear nerve o Enters the brainstem at the cerebellopontine angle along with vestibular nerve (together, form the vestibulocochlear nerve or CNVIII even though they have distinct ganglia and central connections) Cochlear Nuclei: located in the rostral medulla on the lateral surface of the inferior cerebellar peduncle (ICP) Receive all primary auditory fibers from the cochlear nerve Fibers bifurcate and distribute to two nuclei: o Dorsal Cochlear Nucleus: gives rise to dorsal acoustic stria (secondary auditory fibers) Cross midline ventral to medial longitudinal fasciculus (MLF) Ascend in the auditory pathways (lateral lemniscus) o Ventral Cochlear Nucleus: gives rise to intermediate acoustic stria and the ventral acoustic stria Intermediate: from dorsal part of ventral cochlear nucleus; runs dorsal to ICP, crosses midline and enters lateral lemniscus on the opposite side Ventral (Trapezoid Body): from ventral part of ventral cochlear nucleus; runs ventral to ICP, crosses the midline and enters lateral lemniscus of opposite side Some fibers of this pathway also terminate in the superior olivary complex and the nuclei of the trapezoid body Superior Olivary Nuclear Complex: Consists of a principal and accessory nucleus Receives binaural input (from both ears) comparing timing and intensity of auditory signals (sound localization) Gives rise to 3rd order (tertiary) fibers that mostly cross the midline and enter the medial lemniscus on the opposite side o Some fibers can also ascend without crossing the midline (enters medial lemniscus on the same side) Lateral Lemniscus (Ascending Auditory Pathways): Located in the lateral part of the tegmentum and ascends through the pons to terminate at the inferior colliculus at caudal midbrain levels Made up of the following fibers: o Crossed secondary fibers from the cochlear nuclei o Crossed and uncrossed tertiary fibers from the superior olivary nuclear complex Nucleus of the lateral lemniscus: small relay center that receives and contributes fibers to the main bundle Inferior Colliculus: at lower midbrain levels Receives connections from lateral lemniscus Communicates with the IC of the other side via the commissure of the IC Sends auditory fibers to the medial geniculate nucleus via the brachium of the inferior colliculus Medial Geniculate Nucleus: part of the diencephalon Receives fibers from the IC and sends auditory fibers to the transverse temporal gyri of Heschl located in the temporal cortex Transverse Temporal Gyri: Anterior Gyrus: primary auditory area (Brodman’s area 41) Posterior Gyrus: auditory association area (Brodman’s area 42) CLINICAL CORRELATIONS: Deafness: Conductive Deafness: impaired passage of sound waves through external or middle ear o Causes: wax, thickening of windows, ankylosis of ossicles, otosclerosis (new bone formation causing them to be immobile), otitis media (most common cause in children) Sensorineural Deafness: nerve deafness o Causes: degeneration of hair cells, tumors of auditory nerve, multiple sclerosis (loss of myelin), damage to auditory nerve with streptomycin Central Deafness: interference with the pathway in the brain Important Notes: o Lesions above cochlear nuclei results only in partial deafness o Ipsilateral deafness in one ear only results when there is conduction deafness, destruction of the cochlea, cochlear nerve or BOTH of the cochlear nuclei o Lesions of the lateral lemniscus will cause bilateral partial deafness due to extensive crossing (will be greater in the contralateral ear) Clinical Tests: Rinne Test: compares air conduction and bone conduction o Place the butt of the vibrating fork on the mastoid process until the patient can no longer hear it (bone conduction); then place it near the ear without touching it (air conduction) o Normal/Sensorineural Deafness: air better than bone (should hear the vibration longer in the air) o Conduction Deafness: bone is better than (or equal to) air Weber Test: test for lateralization o Normal: vibrating fork heard equally well in both ears when placed on top of the patient’s head at midline o Conduction Deafness: lateralizes to the bad ear (louder on that side) o Sensorineural Deafness: lateralizes to the good ear Presbycusis: gradual hearing loss with aging; higher tones lost early, with declines at each successive frequency above 2000 Hz Auditory Evoked Potentials (AEP): electrophysiological tool which can establish evidence of abnormality when clinical signs and symptoms are equivicol Peaks of AEP correspond to successive anatomic way stations along the auditory pathway: o Peak I: generated by CNVIII o Peak II: generated at or near the cochlear nuclei o Peak III: generated at the lower pons as impulses travel through the superior olive and trapezoid body o Peak IV and V: generated in upper pons or lower midbrain as impulses travel through lateral lemniscus and IC (may be one peak) Uses: o Examine hearing in newborns o Preoperative diagnoses such as acoustic neuromas and coma o Neurosurgical manipulations involving the brainstem and/or CNVIII Preservation of wave V with relatively unchanged latencies and amplitudes is a good predictor of gross postoperative hearing o Transient changes of AEP occur frequently during surgery and are of little clinical significance If detected changes return to normal within 15 minutes, there is usually no serious post-op impairment of function Surgeon can monitor transient changes and use them as a guide to regulate surgical procedures