* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download approved
Survey
Document related concepts
Transcript
Ministry of Health of Ukraine
BUKOVINIAN STATE MEDICAL UNIVERSITY
“APPROVED”
on methodical meeting of the Department of
Anatomy, Topographical anatomy and Operative
Surgery
“………”…………………….2008 р. (Protocol №……….)
The chief of department
professor ……………………….……Yu.T.Achtemiichuk
“………”…………………….2008 р.
METHODICAL GUIDELINES
for the 3d-year foreign students of English-spoken groups of the Medical Faculty
(speciality “General medicine”)
for independent work during the preparation to practical studies
THE THEME OF STUDIES
“Topographical anatomy
of the regions and triangles of the neck”
MODULE I
Topographical Anatomy and Operative Surgery
of the Head, Neck, Thorax and Abdomen
Semantic module
Topographical Anatomy and Operative Surgery of the Head and Neck
Chernivtsi – 2008
1. Actuality of theme:
The topographical anatomy and operative surgery of the neck are very
importance, because without the knowledge about peculiarities and variants of
structure, form, location and mutual location of their anatomical structures, their agespecific it is impossible to diagnose in a proper time and correctly and to prescribe a
necessary treatment to the patient. Surgeons usually pay much attention to the
topographo-anatomic basis of surgical operations on the neck.
2. Duration of studies: 2 working hours.
3. Objectives (concrete purposes):
To know the definition of regions and triangles of the neck.
To know classification of surgical operations on the neck.
To know the topographical anatomy of the neck.
4. Basic knowledges, abilities, skills, that necessary for the study themes
(interdisciplinary integration):
The names of previous disciplines
1. Normal anatomy
2. Physiology
3. Biophysics
The got skills
To describe the structure and function of the
different organs of the human body, to determine
projectors and landmarks of the anatomical
structures. To understand the basic physical
principles of using medical equipment and
instruments.
5. Advices to the student.
5.1. Table of contents of the theme:
The Neck
The neck is a tube providing continuity from the head to the trunk. It extends anteriorly from
the lower border of the mandible to the upper surface of the manubrium of sternum, and posteriorly
from the superior nuchal line on the occipital bone of the skull to the intervertebral disc between the
CVII and TI vertebrae (Fig. 3-1). Within the tube four compartments provide longitudinal
organization:
the visceral compartment is anterior and contains parts of the digestive and
respiratory systems, and several endocrine glands;
the vertebral compartment is posterior and contains the cervical vertebrae, spinal
cord, cervical nerves, and muscles associated with the vertebral column;
the two vascular compartments are lateral and contain the major blood vessels and
the vagus nerve (CN X).
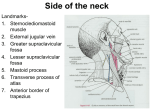
Landmarks of the neck
The laryngeal prominence ("Adam's apple") is the important surface feature of the anterior
part of the neck. It is produced by the thyroid cartilage, the largest part of the laryngeal skeleton.
The thyroid cartilage is located at the level of the 4-5th cervical vertebrae.
There are three superficial muscles in the neck: platysma, sternocleidomastoid, trapezius.
The skin of the neck is thin and pliable. The subcutaneous connective tissue contains
cutaneous nerves and superficial veins. The flat platysma muscle, ascending on the face from the
anterior aspect of the neck, is superficial to the main parts of these veins and nerves.
Areas of the Neck
The anterior edges of the trapezius muscles are demarcate by the neck on the anterior and
posterior areas.
Left and right anterior areas of the neck are subdivided on the suprahyoid, infrahyoid and
sternocleidomastoid regions as well as on two big triangles - medial and lateral. The medial, or
anterior, triangle is limited by inferior border of the mandible, sternocleidomastoid muscle and the
anterior midline of the neck. The lateral (or posterior) triangle is limited by superior edge of
clavicle, back edge of the sternocleidomastoid muscle and trapezoid muscle.
Within the limits of the medial triangle are allocated four more triangles: submandibular,
submental, carotid and omotracheal, or muscular. Within the borders of the lateral triangle
omoclavicular, or occipital, and omotrapezoid, or subclavian, triangles are allocated.
Fascias of the Neck
Whereas there are only three fascias of the human body is known (the superficial, the
investing, the visceral) according to theirs origin from the three germinal layers (ectoderm,
mesoderm and endoderm) bat Shevkunenko distinguished there are five cervical fascias (the
superficial, three leafs of the investing and the visceral). It is convenient for the applied medicine.
The following classification of the rather complicated fascias of the neck follows the work
of several investigators:
1. Superficial fascia.
2. Investing, or Deep, fascia.
a. Anterior, or superficial layer of investing f.;
b. Middle layer of investing f., or fascia of infrahyoid muscles, because it is in front and
below hyoid bone only;
c. Prevertebral layer (posterior, or deep, layer of investing f.);
3. Visceral fascia, or endocervical (pretracheal and buccopharyngeal layers).
1. Superficial fascia
The superficial fascia lies beneath the skin and is composed of loose connective tissue, fat,
the platysma muscle, and small unnamed nerves and blood vessels (Fig. ). The surgeon should
remember that the cutaneous nerves of the neck and the anterior and external jugular veins are
between the platysma and the deep cervical fascia. If these veins are to be cut, they must first be
ligated. Because of their attachment to the platysma above and the fascia below, they do not retract;
bleeding from them may be serious. For practical purposes, there is no space between this layer and
the deep fascia.
2. Investing, or Deep, fascia.
a. Anterior, or superficial layer of investing f., (Fig. ) is envelops two muscles (trapezius and
sternocleidomastoid), two glands (parotid and submaxillary) and forms two spaces (supraclavicular
and suprasternal). It forms the roof of the anterior and posterior cervical triangles and the midline
raphe of the strap muscles.
These fascia is attached superiorly to the superior nuchal line of the occipital bone (Fig. ),
the mastoid process, the zygomatic arch, the inferior border of the mandible, the hyoid bone, and
the spinous processes of the cervical vertebrae. Inferiorly, the layer of investing fascia is attached to
the manubrium of the sternum, the clavicle, and the acromion and spine of the scapula. Just superior
to the sternum, the superficial layer of these fascia divides into two sheets, which are attached to the
anterior and posterior surfaces of the manubrium of the sternum, respectively. The superficial layer
of the investing fascia also forms the roof of the anterior and posterior triangles of the neck.
b. Middle layer of investing f., or fascia of infrahyoid muscles, splits into an anterior portion
that envelops the strap muscles and a posterior sheet that envelops the thyroid gland, forming the
false capsule of the gland. Together with superficial fascia and superficial layer of investing fascia
forms the white line of the neck, an aponeurotic narrow strip, a place of joining fascias and
aponeurosis of the superficial muscles along the medial sagittal line of the neck.
c. Prevertebral, or posterior, layer of investing f. lies in front of the prevertebral muscles. It
originates from the posterior surface of the sternocleidomastoid and, together with the pretracheal
layer of the visceral fascia, forms the carotid sheath. The fascia divides to form a space in front of
the vertebral bodies, the anterior layer being the alar fascia and the posterior layer retaining the
designation of prevertebral fascia.
The prevertebral fascia forms part of a tubular sheath (fascial sleeve) for the prevertebral
muscles that surrounds the vertebral column. It is also continuous with the investing fascia covering
the muscular floor of the posterior triangle of the neck. The prevertebral fascia extends from the
base of the skull to the third thoracic vertebra, where it fuses with the anterior longitudinal ligament
in the posterior mediastinum. The prevertebral fascia extends inferiorly and laterally as the axillary
sheath, which surrounds the axillary vessels and brachial plexus.
Pus from an abscess located posterior to the prevertebral fascia is likely to extend into the
lateral parts of the neck, deep to this fascia on the floor of the posterior triangle. Here, it forms a
swelling, posterior to the sternocleidomastoid muscle.
3. Visceral fascia
The pretracheal layer envelops the some organs of the cervical cavity and lines the wall of it.
This thin layer of visceral cervical fascia is anterior to the trachea and limited to the anterior aspect
of the neck; however, it is more extensive than its name implies. It extends inferiorly from the
thyroid cartilage and the arch of the cricoid cartilage into the thorax. The pretracheal layer lies deep
to the infrahyoid muscles. It splits to enclose the thyroid gland, trachea, esophagus and blends
laterally with the carotid sheath. The main vessels of the thyroid gland are located deep to this layer.
The visceral fascia descends into the thorax where it blends with the fibrous pericardium in the
middle mediastinum.
The buccopharyngeal layer covers the lateral and posterior surfaces of the pharynx and binds
the pharynx to the alar layer of the prevertebral fascia.
Infections in the head or cervical region of the vertebral column can spread inferiorly,
posterior to the esophagus, into the posterior mediastinum. They can also spread inferiorly, anterior
to the trachea, and enter the anterior mediastinum. Air from a ruptured trachea, bronchus, or
esophagus can pass superiorly in the neck. An unusual source of air in the face and neck may be
caused by a dentist's drill passing through an alveolus (tooth socket). Similarly a small slit in the
buccal mucosa, followed by hard blowing with the mouth closed, may result in subcutaneous
cervicofacial emphysema. This unusual kind of swollen neck has been reported in glass blowers and
in those who play wind instruments.
Spaces of the Neck
There are many spaces in the neck defined by the fasciae, but the visceral compartment is
the most important. The boundaries of the visceral compartment of the neck are:
- anterior: fascia of infrahyoid muscles;
- posterior: prevertebral fascia;
- lateral: carotid sheath;
- superior: hyoid bone and thyroid cartilage;
- posteroinferior: posterior mediastinum;
- anteroinferior: bifurcation of the trachea at the level of the 4th thoracic vertebra;
- contents: part of esophagus, larynx, trachea, thyroid gland and parathyroid glands.
The retropharyngeal space consists of loose connective tissue between the prevertebral
fascia and the buccopharyngeal layer of the visceral fascia. The buccopharyngeal layer surrounds
the pharynx superficially. This "space" permits movement of the pharynx, larynx, trachea, and
esophagus during swallowing. It is closed superiorly by the base of the skull and on each side by the
carotid sheath. It opens inferiorly into the superior mediastinum, which contains the thymus, great
vessels of the heart, trachea, and esophagus. The retropharyngeal space is of considerable surgical
interest because of the structures related to it. Pus located posterior to the prevertebral fascia may
perforate this layer and enter the retropharyngeal space. This produces a bulge in the pharynx
known as a retropharyngeal abscess, which causes difficulty in swallowing and speaking (i.e.,
dysphagia and dysarthria). Infections in the retropharyngeal space may also extend inferiorly into
the superior mediastinum.
Carotid Sheath
Beneath the sternocleidomastoid muscle, the investing fascia, the pretracheal fascia, and the
prevertebral fascia contribute to a fascial tube, the carotid sheath. Within this tube lie the common
carotid artery, the internal jugular vein, the vagus nerve, and the deep cervical lymph nodes.
The sac of submandibular gland is pair, contains a submandibular gland, loose cellulose,
lymph nodes, facial vessels. Limited by the sheets of the superficial layer of investing fascia and
periosteum of lower edge of the mandible. It is connects only through openings formed by vessels.
Suprasternal space. It is the interval between two layers of investing fascia. It encloses the
sternal heads of the sternocleidomastoid muscles, the inferior ends of the anterior jugular veins, the
jugular venous arch, and a few lymph nodes. Space is opened from sides, contains a loose fatty
tissue.
Retrosternocleidomastoid cul-de-sac is pair. This space is limited: the back wall of vagina
of the sternocleidomastoid muscle, fascia of infrahyoid muscle, periosteum of superioposterior edge
of clavicle. It is connected with the suprasternal space.
Previsceral space is located between the leaves of internal fascia from the level of hyoid
bone to the manubrium of sternum. Part of this space is selected as pretracheal space. There are
lymph nods, thyroid imae artery (8-12%), part of impar thyroid venous plexus.
Retrovisceral space is located between the visceral fascia (buccopharyngeal layer of it) and
prevertebral fascia of neck, behind a gullet and trachea. Infections in these space can spread into the
posterior mediastinum. There are internal carotid artery, vagus, glossopharyngeal and accessory
nerve, hyoid bone locates in the back department of the space.
Space of lateral triangle of the neck is pair, situated between the investing and the
prevertebral fascias. It is limited outside by the carotid sheath and trapezoid muscle.
Prevertebral space is a crack bedding between prevertebral fascia and neck vertebrae and
spreading downward to the 3rd thoracic vertebra. This space includes of the sympathetic trunk,
phrenic and spinal nerves, deep cervical, levator scapulae, longus colli, anterior, middle and
posterior scalene muscles.
Sternocleidomastoid region
Borders of the region are correspond to muscle.
The layers are:
- skin thin, mobile;
- hypodermic fat is expressed moderately;
- the superficial fascia forms the vagina for the platysma muscle;
- deep fascia forms the vagina for the sternocleidomastoid muscle. On its surface passes
the external jugular vein running into subclavian vein. The innervation of the muscle is carried out
by accessory nerve (CN XI), and the blood supply from the sternocleidomastoid vessels.
- There is main neurovascular fascicle of the neck under the muscle. It consist of common
carotid artery, internal jugular vein and vagus nerve (CN X).
- In the middle of the back edge of the muscle leave branches of the cervical plexus
(transverse cervical, supraclavicular, great auricular, lasser occipital, phrenic, accessory nerves).
Structures beneath the sternocleidomastoid muscle:
- Ansa cervicalis is on the surface of the carotid sheath
- Carotid sheath containing vagus nerve, internal jugular vein, and common carotid artery.
- Cervical sympathetic trunk is embedded in dorsomedial wall of carotid sheath.
Triangles of the neck
Submandibular Triangle
The submandibular triangle is demarcated by the inferior border of the mandible above and
the anterior and posterior bellies of the digastric muscle below. The largest structure in the triangle
is the submandibular salivary gland. A number of vessels, nerves, and muscles also are found in the
triangle.
The contents of the triangle are best described in four layers, or surgical planes, starting
from the skin.
The Roof of the Submandibular Triangle
It is composed of skin, superficial fascia enclosing platysma muscle and fat, and the
mandibular and cervical branches of the facial nerve (CN VII) (first surgical plane).
It is important to remember that (1) the skin should be incised 4 to 5 cm below the
mandibular angle; (2) the platysma and fat compose the superficial fascia; and (3) the cervical
branch of the facial nerve (CN VII) lies just below the angle, superficial to the facial artery.
The marginal mandibular branch of facial nerve passes approximately 3 cm below the angle
of the mandible to supply the muscles of the corner of the mouth and lower lip. The cervical branch
of the facial nerve divides to form descending and anterior branches. The descending branch
innervates the platysma and communicates with the anterior cutaneous nerve of the neck. The
anterior branch, the ramus colli mandibularis, crosses the mandible superficial to the facial artery
and vein and joins the mandibular branch to contribute to the innervation of the muscles of the
lower lip.
Injury to the mandibular branch results in drooling at the corner of the mouth. Injury to the
anterior cervical branch produces minimal drooling that will disappear in 4 to 6 months.
The Contents of the Submandibular Triangle
The structures of the second surgical plane, from superficial to deep, are the anterior and
posterior facial veins, part of the facial (external maxillary) artery, the submental branch of the
facial artery, the superficial layer of the submaxillary fascia (deep cervical fascia), the lymph nodes,
the deep layer of the submaxillary fascia (investing cervical fascia), and the hypoglossal nerve
(XII).
The facial artery pierces the stylomandibular ligament and so it must be ligated before it is
cut to prevent bleeding after retraction. Also, it is important to remember that the lymph nodes lie
within the vagina of submandibular gland in close relationship with it. Differentiation between
gland and lymph node sometimes is difficult.
The anterior and posterior facial veins cross the triangle in front of the submandibular gland
and unite nearby the angle of the mandible to form the common facial vein, which empties into the
internal jugular vein near the greater cornu of the hyoid bone. It is necessary to identify, separate,
clamp and ligate both these veins.
The facial artery, a branch of the external carotid artery, enters the submandibular triangle
under the posterior belly of the digastric muscle and under the stylohyoid muscle. From the
beginning, it is under the submandibular gland. After crossing the gland posteriorly, the artery
passes over the mandible, lying under the platysma. It can be ligated easily.
The Floor of the Submandibular Triangle
The structures of the third surgical plane, from superficial to deep, include the mylohyoid
muscle with its nerve, the hyoglossus muscle, the middle constrictor muscle covering the lower part
of the superior constrictor, and part of the styloglossus muscle.
The mylohyoid muscles are considered to form a true diaphragm of the floor of the mouth.
They arise from the mylohyoid line of the inner surface of the mandible and insert on the body of
the hyoid bone into the median raphe. The nerve, a branch of the mandibular division of the
trigeminal nerve (CN V), lies on the inferior surface of the muscle. The superior surface is in
relationship with the lingual and hypoglossal nerves.
The Basement of the Submandibular Triangle
The structures of the fourth surgical plane, or basement of the triangle, include the deep
portion of the submandibular gland, the submandibular (Wharton's) duct, the lingual nerve, the
sublingual artery, the sublingual vein, the sublingual gland, the hypoglossal nerve (CN XII), and the
submandibular ganglion.
The submandibular duct lies below the lingual nerve (except where the nerve passes under
it) and above the hypoglossal nerve.
The Lymphatic Drainage of the Submandibular Triangle
The submandibular lymph nodes receive afferent channels from the submental nodes, the
oral cavity and the anterior parts of the face. Efferent channels drain primarily into the
jugulodigastric, jugulocarotid and juguloomohyoid nodes of the chain accompanying the internal
jugular vein (deep cervical chain). A few channels pass by way of the subparotid nodes to the spinal
accessory chain.
Lingual triangle (of Pyrogov)
For the purpose of lingual artery ligation in case of bleeding from a tongue or before the
some operations on it the boundaries of lingual triangle must be defined. This triangle locates within
the submandibular triangle and demarcated by the lingual nerve above and the anterior and posterior
bellies of the digastric muscle below.
Submental Triangle
The boundaries of this triangle are:
- lateral: anterior belly of digastric muscle
- inferior: hyoid bone
- medial: midline
- floor: mylohyoid muscle
- roof: skin and superficial fascia
- contents: lymph nodes
The floor of this unpaired suprahyoid area is formed by the two mylohyoid muscles, which
meet in a median fibrous raphe. The apex of the submental triangle is at the symphysis menti (Fig.
3- ) and its base is formed by the hyoid bone. The submental triangle contains the submental lymph
nodes, which receive lymph from the tip of the tongue, the floor of the mouth, the mandibular
incisor teeth and associated gingivae, the central part of the lower lip, and the skin of the chin.
Lymph from the submental lymph nodes drains into the submandibular and deep cervical lymph
nodes. The submental triangle also contains small veins that unite to form the anterior jugular vein.
Carotid triangle
The boundaries are:
- posterior: sternocleidomastoid muscle
- anterior: anterior belly of omohyoid muscle
- superior: posterior belly of digastric muscle
- floor: hyoglossus muscle, inferior constrictor of pharynx, thyrohyoid muscle, longus
capitis muscle, and middle constrictor of pharynx
- roof: investing layer of deep cervical fascia
- contents: bifurcation of carotid artery; internal carotid artery (no branches in neck);
external carotid artery branches (superficial temporal, internal maxillary, occipital, ascending
pharyngeal, sternocleidomastoid, lingual (occasional), external maxillary (occasional) arteries;
jugular vein tributaries (superior thyroid, occipital, common facial, pharyngeal veins; vagus nerve,
spinal accessory nerve, hypoglossal nerve, ansa hypoglossi and sympathetic nerves (partially).
The posterior belly of the digastric muscle - which is between the submandibular and carotid
triangles - is a reliable landmark in a dangerous area. Deep to the posterior belly, the following
anatomic entities will be found: internal and external carotid arteries, internal jugular vein,
glossopharyngeal nerve (CN IX), spinal accessory nerve (CN XI), hypoglossal nerve (CN XII),
sympathetic trunk.
Lymph is received by the jugulodigastric, juguiocarotid, and juguloomohyoid nodes, and by
the nodes along the internal jugular vein from submandibular and submental nodes, deep parotid
nodes, and posterior deep cervical nodes. Lymph passes to the supraclavicular nodes.
Muscular triangle (omotracheal)
The boundaries are:
- superior lateral: anterior belly of omohyoid muscle
- inferior lateral: sternocleidomastoid muscle
- medial: midline of neck
- floor: prevertebral fascia and prevertebral muscles
- roof: investing layer of deep fascia, strap muscles, sternohyoid muscle, and cricothyroid
muscle
- contents: thyroid and parathyroid glands, trachea, esophagus, and sympathetic nerve trunk
Sometimes the strap muscles must be cut during of approach to thyroid gland. They should
be cut across the upper third of their length to avoid sacrificing their nerve supply.
The posterior cervical triangle
The posterior cervical triangle is usually considered to be two triangles, omotrapezoid, or
occipital, and omoclavicular, or subclavian, divided by the posterior belly of the omohyoid muscle,
or perhaps by the spinal accessory nerve.
The boundaries of the posterior triangle are:
- anterior: sternocleidomastoid muscle
- posterior: anterior border of trapezius muscle
- inferior: clavicle
- floor: splenius capitis muscle, levator scapulae muscle, and three scalene muscles
This muscular floor is covered with investing and prevertebral fascia, between which lie the
accessory nerve (CN XI) and a portion of the external jugular vein.
Deep to the fascia are the cervical nerves, the subclavian vessels, and the motor nerves to the
levator scapulae, the rhomboids, the serratus anterior muscles and the diaphragm.
- roof: superficial layer of the investing cervical fascia
- contents: subclavian vessels, cervical nerves, brachial plexus, phrenic nerve, accessory
nerve and lymph nodes
The external jugular vein courses deeply through the omoclavicular triangle.
The superficial occipital lymph nodes receive lymph from the occipital region of the scalp
and the back of the neck. The efferent vessels pass to the deep occipital lymph nodes (usually only
one), which drain into the deep cervical nodes along the spinal accessory nerve.
Scalenovertebral Triangle
It is a deep department of area (inferiomedial).
The boundaries are:
- lateral: scalene muscles
- medial: longus colli muscle
- inferior: apex of the pleura
- contents: subclavian artery (in close relationship with the apex of pleura), subclavian vein,
venous corner, between them vagus nerve and phrenic nerve. On bisectrix of the triangle passes
vertebral artery. Along the medial edge of the triangle, between the leafs of the prevertebral fascia is
located the cervical department of the sympathetic trunk.
5.2. Theoretical questions to studies:
1.
2.
3.
4.
5.
6.
7.
The structure of the facial region of the head.
The boundaries of the buccal region.
The blood supply of buccal region.
The nerve supply of buccal region.
The parotidomasseter region.
The parotid bed.
Profound facial region.
5.3. Materials for self-control:
DIRECTIONS: Each question below contains four or five suggested responses. Select the one best
response to each question.
31. Injury to the motor root of the mandibular division of the trigeminal nerve (CN V3) would incur
paralysis of all the following EXCEPT the
A anterior belly of the digastric muscle
B buccinator muscle
C mylohyoid muscle
D tensor tympani muscle
E tensor veli palatini muscle
32. The pterygomandibular raphe is a useful landmark in the oral cavity. This tendinous tissue
marks the juncture of two muscles that are innervated by which of the following cranial nerves?
A Maxillary (CN V2) and mandibular (CN V3)
B Mandibular (CN V3) and glosso-pharyngeal (CN IX)
C Mandibular (CN V3) and vagus (CN X)
D Facial (CN VII) and glossopharyngeal (CN IX)
E Facial (CN VII) and vagus (CN X)
33. A lesion involving the inferior salivatory nucleus would affect
A activation of neurons in the otic ganglion
B innervation of the superior tarsal muscle
C lacrimation
D mucous release in the nasal passages
E submandibular gland secretion
34. The cell bodies for the sensory nerve fibers that convey pain, touch, and temperature from the
posterior third of the tongue are lot cated in
A the geniculate ganglion
B the pterygopalatine ganglion
C the semilunar ganglion
D the submandibular ganglion
E none of the above
35. A 53-year-old banker develops paralysis on the right side of the face, which produces an
expressionless and drooping appearance. He is unable to close the right eye and also has difficulty
chewing and drinking. Examination shows loss of blink reflex in the right eye to stimulation of
either right or left conjunctiva. Lacrimation appears normal on the right side, but salivation is
diminished and taste is absent on the anterior right side of the tongue. There is no complaint of
hyperacusis. Audition and balance appear to be normal. The lesion is located
A in the brain and involves the nucleus of the facial nerve and superior salivatory nucleus
B within the internal auditory meatus
C at the geniculate ganglion
D in the facial canal just distal to the genu of the facial nerve
E just proximal to the stylomastoid foramen
36. In the course of administering a local anesthetic, a needle that is placed too far into the greater
palatine canal may paralyze an autonomic ganglion. In addition to dry nasal mucosa from loss of
nasal gland secretion, loss of function at this ganglion would result in
A dry eye from loss of lacrimal gland secretion
B dry mouth from loss of parotid gland secretion
C dry mouth from loss of submandibular and sublingual gland secretions
D pupillary constriction
E none of the above
Literature
1. Snell R.S. Clinical Anatomy for medical students. – Lippincott Williams &
Wilkins, 2000. – 898 p.
2. Skandalakis J.E., Skandalakis P.N., Skandalakis L.J. Surgical Anatomy and
Technique. – Springer, 1995. – 674 p.
3. Netter F.H. Atlas of human anatomy. – Ciba-Geigy Co., 1994. – 514 p.
4. Ellis H. Clinical Anatomy Arevision and applied anatomy for clinical
students. – Blackwell publishing, 2006. – 439 p.