* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download BLOOD CIRCULATION
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
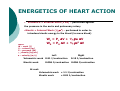
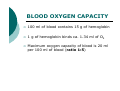
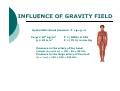
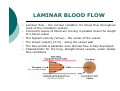
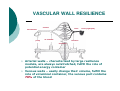
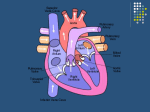
BLOOD CIRCULATION Department of Biomedical Sciences Medical University of Lodz CONSTRUCTION OF THE CIRCULATORY SYSTEM Circulatory System VESSELS CONSTRUCTION HEART The primary function of the heart is blood pumping Pumping is done by the rhythmic contractions of different batches of the heart Factors causing contractions - are periodically passing through the heart muscle cells membranes - waves of depolarization and repolarization of cells to the resting phase THE RHYTHM OF THE HEART It is relatively constant. At rest, the number of heartbeats per 1 minute depends on age (in children is higher), gender (in women is higher than man) and level of physical strenght In an adult an average value is 60-80 beats/min. Heart rhythm accelerates under the influence of emotional factors, elevated ambient temperature and physical effort During each contraction of the heart, the main artery is extruded to a certain amount of blood called the ejection fraction (in the systemic circuit). The average value for healthy adults in rest is 50-70 ml. Thus, the total amount of blood extruded per minute through the left ventricle into the circulatory system is defined as a minute or cardiac output – it is the product of the rhythm and the level of the systol In adults and healthy people, with an average level of fitness, at rest, 4-5 liters of blood is pumped by the heart per one minute (the cardiac output) ENERGETICS OF HEART ACTION • Volumetric = External Work (P dV) – performed against the pressure in the aorta and pulmonary artery •Kinetic = Internal Work (½ ρν2) – performed in order to introduce kinetic energy to the blood (to move blood) were: W – work [J] V – volume [m3] P – pressure [Pa] ρ − density [kg/m3] ν – velocity [m/s] WL = PL ∆V + ½ ρν2 ∆V WR = PR ∆V + ½ ρν2 ∆V Left Right Volumetric work 0.91 J/contraction 0.15 J/contraction Kinetic work 0.006 J/contraction 0.006 J/contraction At rest: Volumetric work = 1.1 J/contraction Kinetic work = 0.01 J/contraction HEART ACTION The heart is a pump where energy is used not to fill the atrium and the ventricle with blood, but for emptying it It is not a lift-and-force pump, the vacuum is not produced during its filling The pressure in the heart chambers is always positive The efficiency energy of the heart is: at rest - 15% in stress conditions - 40% BLOOD FUNCTIONS: Transport - atmospheric oxygen from the lungs to the tissues and CO2 from the tissues to the lungs; of nutrients from the digestive tract and removal of metabolic products; of hormones, enzymes and antibodies. Maintaining a relatively constant H2O content in the tissues through the exchange of fluids (with lymph or urine). Control of body temperature - blood moves towards the skin to cool us down, as excess heat can escape easier. Protection - in the form of our immune system. Blood carries white blood cells which help fight disease. Platelets also clot the blood to stop us from bleeding. BLOOD COMPOSITION BLOOD OXYGEN CAPACITY 100 ml of blood contains 15 g of hemoglobin 1 g of hemoglobin binds ca. 1.34 ml of O2 Maximum oxygen capacity of blood is 20 ml per 100 ml of blood (ratio 1:5) PRESSURE GRADIENT IN LARGE AND SMALL CIRCULATION Aorta Caval vein 100 hPa (70 mm Hg) 160 hPa (120 mm Hg) 0 Pulmonary artery 10 hPa (8 mm Hg) 30 hPa (15 mm Hg) Pulmonary vein 9 hPa (7 mm Hg) diastole systole diastole systole MOVEMENT OF BLOOD IS CAUSED BY PRESSURE DIFFERENCE BETWEEN ARTERIAL AND VENOUS SYSTEMS AND THAT IS SUSTAINED BY HEART WORK INFLUENCE OF GRAVITY FIELD Hydrostatic blood pressure P = ρ x g For ρ ≈ 103 kg/m3 g ≈ 10 m/s2 x h P = (100h) in hPa P = (75 h) in mm Hg Pressure in the artery of the head: (height (h) =0.5 m) = 130 – 50 = 80 hPa Pressure in the large artery of the foot: (h = 1 m) = 130 + 100 = 230 hPa LAMINAR BLOOD FLOW Laminar flow - the normal condition for blood flow throughout most of the circulatory system Concentric layers of blood are moving in parallel down the length of a blood vessel The highest velocity (Vmax) - the center of the vessel. The lowest velocity (V=0) - along the vessel wall The flow profile is parabolic once laminar flow is fully developed Characteristic for the long, straight blood vessels, under steady flow conditions TURBULENT FLOW Laminar flow – a fluid flows in parallel layers Turbulent flow – only immediately after the semilunar valves close (heart sounds) Re η νk = rρ Re – Reynolds’ number (approx. 1000) νk – critical velocity [m/s] η – viscosity coefficient [Ns/m2] r – vessel radius [m] ρ – blood density [kg/m3] CHANGE IN VESSEL LUMEN LAWS REGULATING BLOOD FLOW 1) FLOW CONTINUITY PRINCIPLE ∆t ∆V ∆t ∆V ν1 J= Flow rate S1 ν x 1 = S2 x S – area [m2] ν- velocity [m/s] t – time [s] V – volume [m3] ν2 ν2 ∆V [m3] ∆t [s] J1 = J2 Accounting for vessel ramification J = ∑ Jn S = ∑ Sn S capillary Saorta = 750 Not accounted for: • vessel pulsation • exchange of blood with the surroundings 2) BERNOULLI’S LAW p + hρ ρg + ½ ρv2 = const where: p – static pressure [Pa] h – hight [m] ρ – density [kg/m3] v –velocity [m/s] g – acceleration of gravity [m/s2] For horizontal vessel: p + ½ ρv2 = const THE TOTAL SUM OF STATIC PRESSURE (p), HYDROSTATIC PRESSURE (hrg) AND HYDRODYNAMIC PRESSURE (½ ρv2) IS CONSTANT DURING THE FLOW FOR ANY CROSS-SECTION OF THE TUBE 3) POISEUILLE’S LAW For non-turbulent, non-pulsatile fluid flow through a uniform straight pipe, the volume flow rate (J) is: 1) directly proportional to the pressure difference (∆P) between the ends of the tube, 2) inversely proportional to the length (l) of the tube, 3) inversely proportional to the viscosity (η) of the fluid, 4) proportional to the fourth power of the radius (r4) of the tube. π 1 r4 ∆V J= = 8ηl ∆t 1 J= ∆P R 8 R= η l4 r π ∆P [m3/s] R – resistance of the vessel blood inflow [Pa s/m3] 2-FOLD INCREASE IN RADIUS DECREASES RESISTANCE BY 16-FOLD! I.E. RESISTANCE VERY SENSITIVE TO RADIUS VASCULAR WALL RESILIENCE left ventricle pump arteries veins air chamber heart (right part) container resistance Arterial walls – characterized by large resilience module, are always outstretched, fulfill the role of potential energy container Venous walls – easily change their volume, fulfill the role of voluminal container, the venous part contains 70% of the blood VASCULAR RESISTANCE VOLUME veins RESISTANCE venules arteries arterioles arteries Capillaries Capillaries veins venules arterioles Volume Resistance vessels vessels GEOMETRIC FACTOR OF VASCULAR RESISTANCE TO BLOOD FLOW L r4 = geometric factor F L = spring tension The effect of spring tension is spring pressure of the wall in accordance with the law of Laplace : T P= r where: P – wall spring pressure on blood [Pa] T – spring tension in the wall [N/m] r – vessel radius [m] Small deformations (elastin fibers) Large deformations (collagen fibers) PULSE Every 0,8 s 70 cm3 of blood is ejected (ejection volume at rest) Loop resistance causes bulge in aorta, i.e. blood kinetic energy is changed into potential energy of the aorta wall resilience Pulse wave occurs – a wave of spring deformations in the wall of artery vessels C=F √ Εd 2 ρr C – pulse wave velocity [m/s] F – empirical coefficient ρ – density [kg/m3] E – Young module [Pa = N/m2] d – artery wall thickness [m] r – vessel radius [m] BLOOD VISCOSITY F= ηA ∆ν ∆H [N] F A - shear stress [N/m2] ν H - shear rate [1/s] shear stress η = shear rate Viscosity coefficient [Ns/m2] is the ratio of the shearing stress to the shear rate in a fluid. where: A – area [m2] H – hight [m] v –velocity [m/s] η – viscosity coefficienty [Ns/m2] FACTORS AFFECTING BLOOD VISCOSITY diameter of blood vessels - below 0.3mm viscosity is lower (Magnus Effect) temperature – in 0°C viscosity is 2.5-times higher concentration of plasma proteins flow rate – diameter 0.1-0.2mm: velocity increases but viscosity decreases presence of cellular components of blood, particularly hematocrit (% of content of erythrocytes in the blood volume) size (7µm) and deformability of erythrocytes AXIAL ACCUMULATION OF BLOOD CELLS (MAGNUS EFFECT) VISCOELASTICITY Vessels smaller tham 3 µm – viscosity increases, but elasticity occurs