* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download pneumonia
Gastroenteritis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Neonatal infection wikipedia , lookup
Typhoid fever wikipedia , lookup
Anaerobic infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Influenza A virus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
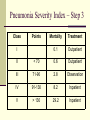
Pneumonia Danielle M Hansen, DO, MS PNEUMONIA Definition: Infection of Lung Parenchyma 1/6 of All Deaths in USA Most Common Infectious Cause of Death Pneumonia Defense Mechanisms Defense Mechanism Cough Reflex Things that Impair the Defense Mechanism Anesthesia Neuromuscular Disorder Coma Mucociliary Apparatus Cigarette Smoke Corrosive Gases Phagocytic Action of Alveolar Macrophages Alcohol Secretion Clearance Cystic Fibrosis Innate, Humoral, Cell-Mediated Immunity Tobacco Classification of Pneumonia Community-Acquired, Acute S. pneumoniae H. influnzae M. catarrhalis Staph aureus Enterobacteriacea Community-Acquired, Atypical Mycoplasma Chlamydia Legionella Coxiella burnetti Viruses Nosocomial Enterobacteriacea Pseudomonas S. Aureus (MRSA) Aspiration Anaerobic oral flora Aerobic bacteria Immunocompromised Host CMV PCP MAC Aspergillosis Candidiasis Classification of Pneumonia Community-Acquired, Acute S. pneumoniae H. influnzae M. catarrhalis Staph aureus Enterobacteriacea Community-Acquired, Atypical Mycoplasma Chlamydia Legionella Coxiella burnetti Viruses Nosocomial Enterobacteriacea Pseudomonas S. Aureus (MRSA) Aspiration Anaerobic oral flora Aerobic bacteria Chronic Nocardia Actinomyces Granulomatous Necrotizing and Abscess Anaerobic Staph aureus Klebsiella Strep pyogenes Immunocompromised Host CMV PCP MAC Aspergillosis Candidiasis CAP - ACUTE Clinical Presentation: High Fever, Shaking Chills Cough Productive of Mucopurulent Sputum Pleuritic Chest Pain, Pleural Friction Rub Clinical Course: Marked Improvement in Symptoms after 48-72 Hours of Antibiotics <10% Mortality Pathogenesis of Acute CAP Invasion of Lung Parenchyma Normal Alveoli Inflammatory Exudate Fills Alveoli Consolidation Pneumonia Morphology of Acute CAP Bronchopneumonia Patchy Consolidation Lobar Pneumonia Fibrinosuppurative Consolidation of Entire Lobe or Large Portion of Lobe Pathogens of Acute CAP S. pneumoniae H. influnzae M. catarrhalis Staph aureus Enterobacteriacea <10 epi’s/lpf Streptococcus Pneumoniae = Pneumococcus Most Common Cause of CAP Up to 50% Colored Sputum False Positive Sputum Cultures Normal Flora of Nasopharynx Blood Cultures More Specific 30% Mortality if Bacteremic Treatment: Fluoroquinolones, Amoxil, PCN, Macrolides Some Resistant Strains Immunization Staphylococcus Aureus Follows Influenza or ABX Colored Sputum Treatment: 1st Generation Cephalosporin or PCN Vanco (if MRSA suspected) High Incidence of Complications Lung Abscess Empyema Glomerulonephritis Pericarditis Enteric Gram-Negatives Klebsiella, E. Coli, Proteus Most Frequent Cause of GN Pneumonia Debilitated and Malnourished Chronic Alcoholics Sputum Treatment: Fluoroquinolones Pip+Tazo ECF Haemophilus Influenzae Gram-Negative Coccobacilli Encapsulated Form > Unencapsulated Form Infections from Unencapsulated Forms Elderly, COPD Bronchopneumonia Treatment: Ampicillin, Augmentin, Doxycycline, 3rd Generation Cephalosporins, Fluoroquinolones, TMP/SMX Immunization for b Serotype Moraxella Catarrhalis Gram Negative Cocci COPD, DM, CA Treatment: Doxycycline Macrolide Cephalosporin Augmentin CAP - ATYPICAL Clinical Presentation: Symptoms out of Proportion to PE Findings Less Sputum No Consolidation Moderate WBCs Clinical Course: Sporadic Form < 1% Mortality Interstitial Form has been Epidemic Secondary Bacterial Infections Pathogenesis of Atypical CAP Organism Attaches to Upper Respiratory Tract Epithelium Cell Necrosis and Inflammatory Response Interstitial Inflammation Morphology of Atypical CAP Patchy or Lobar No Pleural Involvement Pathogens of Atypical CAP Mycoplasma Chlamydia Pneumoniae Legionella Coxiella Burnetti (Q Fever) Viruses: Influenza Respiratory Syncytial Virus Adenovirus Rhinovirus Rubeola Varicella Mycoplasma Pneumoniae Most Common Cause of Atypical CAP Children and Young Adults Sporadic or Epidemic 2-3 Week Incubation Period Extrapulmonary Manifestations: Hemolytic Anemia Splenomegaly Erythema Multiforme Arthritis Myringitis Bullosa Pharyngitis Tonsillitis Mental Status Change Diagnosis: Complement Fixation to Measure IgM Antibody Treatment: Macrolide, Doxycycline Up to 6 Months Recovery Legionella Pneumophila Artificial Aquatic Environments Transmitted by Inhalation or Aspiration Associated Diarrhea, Neuro Sx Na and Phos Fatality Rate 50% in Immunosuppressed Diagnosis: Antigen in Urine +Fluorescent Antibody Test on Sputum Culture is Gold Standard Treatment: Macrolides or Quinolones Chlamydophilia Pneumoniae Young Adults Laryngitis precedes Pneumonia by 2-3 Wks Diagnosis: IgM titer > 1:16 Positive Culture PCR 4x Increase in IgG Treatment: x 3 Wks Doxycycline Macrolides Influenza Virus 8 Helices of Single-Stranded RNA Encodes Nucleoprotein Determines Type (A, B, C) Lipid Bilayer = Envelope Containing Hemagglutinin and Neuraminidase Determines Subtype (H1-3, N1-2) Type A is Major Cause of Human Infections Epidemics Antigenic Drift (Mutations of Hemagglutinin and Neuraminidase) Pandemics Antigenic Shift (Hemagglutinin and Neuraminidase Replaced with Animal Virus RNA Segments) Type B, C Infect Children Treatment: Oseltamir (Tamiflu) and Zanamivir (Relenza) Severe Acute Respiratory Syndrome Pandemic of 2002 started in China > 8,000 Cases 774 Deaths Coronavirus from Animals Diffuse Alveolar Damage, Multinucleated Giant Cells Clinical Presentation: Incubation Period 2-10 Days Dry Cough, Malaise, Myalgias, Fever, Chills Clinical Course: 1/3 Resolve 2/3 Progress to SOB, Tachypnea, Pleurisy 10% Mortality NOSOCOMIAL PNEUMONIA Types: Hospital Acquired (HAP) >48 hours after Admission Ventilator Associated (VAP) >48 hours after Intubation Healthcare Associated (HCAP) Hospitalized >2 Days within 90 Days Resident of ECF IV ABX, Chemo, Wound Care within 30 Days Hemodialysis Pathogens: GNR (Enterobacteriaceae and Pseudomonas) Staph Aureus (MRSA) Life-Threatening Pseudomonas Aeruginosa Risk Factors: ICU Steroids ABX > 7 Days in Past Month CHF Malnutrition Cystic Fibrosis Extrapulmonary Spread Hematogenously Treat with 2 Antipseudomonals Aminoglycoside + Antipseudomonal Beta-Lactam ASPIRATION PNEUMONIA Abnormal Gag and/or Swallowing Reflex Pneumonia from Oral Flora Aerobes > Anaerobes Chemical Pneumonitits from Gastric Acid Necrotizing, Fulminant Course Lung Abscess or Empyema are Common Complications Treatment: Augmentin or Clindamycin CHRONIC PNEUMONIA Localized Lesion with/without Nodes Immunocompetent Granulomatous Inflammation Fungal Histoplasma Capsulatum Blastomyces Dermatitidis Coccidioides Immitis Histoplasmosis Ohio and Mississippi Rivers and Caribbean Inhalation of Bird and Bat Droppings Contaminated with Spores Primary Stage: Self-Limited or Latent Coin Lesion on Chest X-Ray Secondary Stage: Chronic, Progressive Cough, Fever, Night Sweats Lung Apices Extrapulmonary Manifestations: Adrenals Liver Meninges No Treatment Indicated unless Disseminated Blastomycosis Central and SE U.S., Canada, Mexico, Africa, India, and the Middle East Male : Female 10:1 Clinical Presentation: Abrupt Onset Productive Cough Headache Chest Pain, Abdominal Pain Weight Loss, Anorexia Fever, Chills, Night Sweats May Resolve, Persist, or Progress to Chronic Treatment: Itraconazole Coccidioidomycosis SW and Far West U.S. and Mexico Deserts >80% of Population in Endemic Areas are Infected Only 10% are Symptomatic Lung Lesions Fever Cough Pleuritic Pain Erythema Nodosum or Multiforme Treat if Hemoptysis or Abnormal CXR with Fluconazole or Amphotericin B IDSA/ATS CAP Guidelines 2007 Pneumonia Severity Index – Step 1 Lab & x-ray PE PMHx Demographics Pneumonia Severity Index – Step 2 Risk Factors Points Age (M) Years Age (F) Years-10 ECF 10 Active Neoplasm 30 Chronic Liver Dz 20 CHF 10 Cerebrovascular Dz 10 CKD 10 Altered Mental Status 20 Resp > 30 20 SBP < 90 20 Temp < 35 or > 40 15 Pulse > 125 10 pH < 7.35 30 BUN > 30 20 Na < 130 20 Glucose > 250 10 Hematocrit < 30 10 PaO2 < 60 10 Pleural Effusion 10 Pneumonia Severity Index – Step 3 Class Points I Mortality Treatment 0.1 Outpatient II < 70 0.6 Outpatient III 71-90 2.8 Observation IV 91-130 8.2 Inpatient V > 130 29.2 Inpatient CURB-65 Confusion (disorientation to person, place, or time) Urea (blood urea nitrogen) >7 mmol/L (20 mg/dL) Respiratory rate >30 breaths/minute Blood pressure (systolic <90 or diastolic <60) Age >65 years Score 0-1 2 >3 Mortality 0.7-2.1 Treatment Outpatient 9.2 >14.5 Inpatient ICU Indications for Etiology Testing Empiric Outpatient Treatment Healthy and No ABX within 3 months: Macrolide Or Doxycycline Comorbidities (chronic heart, lung, liver or renal disease; diabetes mellitus; alcoholism; malignancies; asplenia; immunosuppressing conditions or use of immunosuppressing drugs) or ABX within 3 months Fluoroquinolone Or B-Lactam Plus Macrolide For Macrolide-Resistant Streptococcus pneumoniae Fluoroquinolone Or B-Lactam Plus Macrolide Empiric Inpatient Treatment Non-ICU: Fluoroquinolone Or B-Lactam Plus Macrolide ICU: B-Lactam (cefotaxime, ceftriaxone, or ampicillin-sulbactam) Plus Azithromycin Or Fluoroquinolone For Penicillin-Allergy: Fluoroquinolone and Aztreonam Special Circumstances For Pseudomonas: Piperacillin-tazobactam, cefepime, imipenem, or meropenem Plus Ciprofloxacin or Levofloxacin Or Aminoglycoside and Azithromycin Or Aminoglycoside and Fluoroquinolone For Penicillin-Allergy, Substitute Aztreonam for B-Lactam For CA-MRSA: Vancomycin or Linezolid Extras First Dose of ABX in ER IV to PO when: Hemodynamically Stable Clinically Improving Able to Ingest RX Functioning GI Tract Length of Treatment: Minimum of 5 days Afebrile for 48–72 hours Clinically Stable Immunizations: Influenza Pneumococcal Smoking Cessation