* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Incorporating Heart Failure Patients into Cardiac
Survey
Document related concepts
Transcript
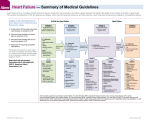
Lynne Hamilton Weir, PT, CYT List risk factors/causes of HF and discuss treatment List key self care skills for the heart failure patient/family/caregiver to learn for self management of HF Develop an exercise prescription for the heart failure patient Identify the CMS HF eligibility criteria necessary for HF participation and reimbursement Heart Failure Facts and Guidelines CR in HF Disease Management Staff Training CMS HF Criteria Core Components for CR HF ITP Self Care Behaviors Exercise Training and Prescription CR Session Boarding Pass and Red Flags Heart failure is “a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill or eject blood.” The main manifestations of HF are dyspnea, fatigue, limited exercise tolerance and fluid retention which may lead to pulmonary, and/or splanchnic congestion, and/or peripheral edema. HFrEF HFpEF Stage Definition A At high risk for later HF but without current structural heart disease B Structural heart disease but without signs or symptoms of HF C Structural heart disease with current or prior symptoms of HF D Refractory HF HF Stage Patients with the following: A • Risk Factors – smoking, HTN, HLD, DM, obesity, Metabolic Syndrome, known CAD • Exposure cardiotoxins – cocaine, some chemotherapies • Hx of familial cardiomyopathy B • Known structural heart changes-MI, valve, CM, LVH,<EF • No signs or symptoms of HF C • Known structural heart disease – MI, CM, Valve disease PLUS • Signs and symptoms of Heart Failure: HFPEF or HFREF D • Marked HF signs and symptoms even at rest, hospitalizations despite GDMT HF Stage Treatment A Risk factor modification • therapeutic lifestyle changes • drug therapies as indicated B • Drug therapy – ACEI or ARB, BB as indicated • Revascularization or valve surgery if indicated C • Drug therapy - ACEI/ARB plus BB, diuretics Aldosterone antagonists Hydralazine/nitrates – African Americans • ICD, CRT, revascularization, valvular surgery as indicated D • Drug therapy, LVAD, transplant, palliative care, hospice NYHA Functional Capacity Classification I No limitation of physical activity. Ordinary physical activity does not cause symptoms. II Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in symptoms. III Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes symptoms. IV Inability to carry on any physical activity without symptoms. Symptoms may be present even at rest. HF Stage Cardiac Rehabilitation A CR for Primary Prevention for at risk population-self pay B CR for MI, angina, PCI, CABG, Valve C CR for HF < 35% EF Medicare/Medicaid CR for all other HF covered by private carriers D Cardiac Rehabilitation for LVAD, transplant >5.1 Million in US have HF Incidence of HF is increasing By 2050 - 1 in 5 individuals will have HF Primary diagnosis for Medicare hospital admissions High rate of hospital all cause 30 day readmissions – average 25% Cost of HF care in US >$30 billion/year with>50% due to hospitalizations Individual treatment plan creation Provider assessment What’s missing? Hospital •Diet non adherence •RX non adherence •Failure to seek care •Care not readily available •Socioeconomic factors •Inappropriate RX or ED Patient education on treatment plan Patient non-adherence 14 Every patient with HF should have an evidence based plan of care that ensures GDMT goals, management of comorbid conditions, timely FU with health care team, dietary instruction and physical activities - updated regularly and made available to each patient’s healthcare team. Effective systems of care coordination should be deployed for every patient with chronic HF to achieve GDMT and prevent hospitalizations. HF pts. should receive specific education to facilitate self-care Cardiac Rehabilitation can be useful in clinically stable patients with HF to improve functional capacity, exercise duration, HR- QOL and mortality. Ex. training (or regular physical activity) is recommended as safe and effective for pts. with HF who are able to participate to improve functional status. CR has a unique opportunity to provide HF disease management significantly impacting clinical outcomes. • Facilitate self care skills leading to self management – Health Care 90% Self Care • Health coaching and motivational interviewing • Support families/caregivers Identify barriers – comorbidities (cognition/depression), financial, transportation, education Identify resources Medication reconciliation Track and communicate clinical variances with physician Facilitate obtaining office visits with fast track intervention Medication adjustment according to diuretic protocol if authorized by physician And importantly…. Collect data and track outcomes with AACVPR Report tracking HF admissions/discharge Inpatient visits Automatic CR referrals at discharge Heart Failure Clinic and Provider Offices Transitions/Home Health HF patients…. Clinically stable, HFrEF <35% On optimal medical therapy for at least 6 wks Cannot have had a recent (<6wk) and does not have a planned major CV hospitalization or procedure in the next 6 mo. 6 week waiting period is an opportunity for CR to impact HF care at their facility 6 Weeks of ENGAGEMENT • Enrollment telehealth program • Follow up patient/family calls • Self care education/disease management skills – telephone, internet, 1:1 or classes • Schedule appointment to begin CR in 6 weeks Obtain a reliable scale, record weight daily, monitor for excessive change in body weight – + 3 lb from baseline “dry” weight Observe changes in signs/symptoms of SOB, lightheadedness, swelling, fatigue, cough, nocturia, pillow count Contact health care provider promptly for unexpected weight change or increasing symptoms Develop a system for taking mediation as prescribed-pill organizer, timely refills Limit dietary sodium intake (<2.0-2.3g/d in most cases) Avoid excess fluid intake (<1.5-2 L/d in most cases) Do not use dietary supplements or herbal medicines unless approved by HCP or pharmacist Avoid all tobacco products/2nd hand smoke Restrict alcohol intake <2/d M;<1/d F Avoid recreational toxins, especially cocaine Seek treatment for depression/anxiety Discuss sleep disturbances w/HCP such as heavy snoring Achieve and maintain physical fitness by engaging in regular exercise Visit HCP at regular intervals as advised Monitor coexisting conditions, such as HBP, DM, cholesterol levels, obesity, renal disease Maintain current immunizations, especially influenza and pneumococcal pneumonia Follow prescribed nutrition plan Patient Assessment – Hx, Medication, Symptom Management, Physical Nutrition Counseling Weight Management Blood Pressure Management Lipid Management Diabetes Management Tobacco Cessation Psychosocial Management Physical Activity/Training Medical Record – hospital and provider Medical History from patient/caregiver Cardiac – ischemic or idiopathic, valve related, HTN Paced, CRT, ICD Comorbidities and Risk Factors Complex Patients: pulmonary disease, CKD, anemia, depression, sleep apnea, DM, musculoskeletal, neurological, cognitive Medication Reconciliation- dose/frequency ◦ Have patient bring in list/bottles – compare DC instructions and physician OV list ◦ Any problems accessing medications? – financial, transportation, refills ◦ Medication compliance – taking regularly what % of the time? Morinsky Survey ◦ Medication schedule ◦ What system do they have for taking – who manages? Is your patient on optimal GDMT?? HFrEF Stage C NYHA Class I – IV Treatment: Class I, LOE A ACEI or ARB AND Beta Blocker For all volume overload, NYHA class II-IV patients For persistently symptomatic African Americans, NYHA class III-IV For NYHA class II-IV patients. Provided estimated creatinine >30 mL/min and K+ <5.0 mEq/dL Add Add Add Class I, LOE C Loop Diuretics Class I, LOE A Hydral-Nitrates Class I, LOE A Aldosterone Antagonist LCZ696 from Novartis ………may replace ACEI Current and recent: ◦ Dyspnea ◦ Fatigue ◦ Angina ◦ Lightheadedness Current and recent: ◦ Edema – LE’s and abdominal ◦ Cough ◦ Orthopnea -how many pillows ◦ Cachexia ◦ Sleep Apnea – Berlin Sleep Apnea Questionnaire Determine the following: ◦ ACCF/AHA - Heart Failure Stage (C or D) ◦ NYHA Functional Class I-IV ◦ ACCF/AHA Risk Stratification – High based on EF Weight and height BP - symptomatic hypotension or orthostatic hypotension EKG – HR, BBB, pacing, ectopy, atrial fib O2 Sat % - undiagnosed pulmonary component Waist circumference - abdominal edema? Edema LE 1+ to 4+ Lung sounds – baseline rales ? Gait, strength and balance Fall risk, frailty index Assessments ◦ Dietary habit assessment tool ◦ Daily Caloric Intake- undernourished? ◦ Daily Sodium Intake Assessments HR-QOL – Minnesota Living with HF Questionnaire Kansas City Cardiomyopathy Questionnaire Depression - Beck Depression Inventory Patient Health Questionnaire-9 ◦ Assessments ◦ Anxiety, anger/hostility ◦ Social isolation, marital/family distress ◦ Substance abuse ◦ Psychotropic medications and provider Assessment ◦ Duke Activity Survey ◦ Days per week of exercise, minutes per day ◦ Occupational and recreational needs ◦ Activity of Daily Living needs ◦ Exercise Stress Test or 6 Min Walk Test ◦ MET level of 1st exercise session Types ◦ Cardiorespiratory Endurance Training ◦ Resistance Training ◦ Flexibility ◦ Balance Type - Cardiorespiratory Endurance Training ◦ Frequency 2-3 (CR) progressing to 5+ days/week ◦ Intensity ETT (recommended) 55% progressing to 80% HRR=THR Without ETT/Beta Blocker/ Afib Initial rest HR + 20/ RPE 10-12 …Progressing to RPE 13-14 = THR Afib – use RPE only High Intensity Interval Training- selected pts 30 sec-4 min HII followed by LII, 3-5 min ◦ Time/Duration – 16-20 min progressing to 40 min-50 min Deconditioned pts. may need rest periods ◦ Mode – cardio equipment, walking +++ Type – Resistance Training ◦ Utilize fixed weight machines, hand held weights, body weight for 4-6 primary muscle groups ◦ Post 2-4 weeks of cardio training ◦ Intensity – UE - 40% 1 rep max progressing to 70% LE – 50% 1 rep max progressing to 70% ◦ Frequency 1-2 days/wk, 1-2 sets/day Duration 12-20 min total Type – Flexibility Training ◦ Stretching exercises for major muscle groups ◦ End of warm up and/or during cool down at least 3 x per week ◦ Purpose to maintain joint flexibility Type – Balance Training ◦ Fall risk patients ◦ 1-2 days per week 1. 2. 3. 4. 5. 6. 7. 8. Rate SOB – Dyspnea Scale 0-4 More swelling? 0 to 4 Difficulty breathing at night/sleeping? Need more pillows? Take all medications? Out of any? Daily weight – chart, morning, trending Lightheadedness? Pain/discomfort? (angina or other) Where and rating Lab work? Next physician appt? Weight Gain > 2-3 lb in a day or 5 lb within a week Worsening dyspnea (on exertion or rest) Excessive fatigue, lack of energy Increased edema legs, abdomen Increased urination at night, nocturia Productive cough Increased orthopnea or nocturnal dyspnea Lightheadedness/dizziness- hypotension Shock from ICD Disease Management Review of 2013 ACCF/AHA Heart Failure Guidelines Clinical health coaching and motivational interviewing LVAD and Transplant Specific Training Palliative care, hospice and EOL decisions Heart Failure Facts and Guidelines CR in HF Disease Management CMS HF Criteria Self Care Behaviors Core Components for CR HF ITP Exercise Training and Prescription CR Session Boarding Pass and Red Flags Staff Training Yancy, CW, et al. ACCF/AHA Guideline for the Management of Heart Failure. JACC, 2013; 62:e147-e239. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins: 2014. American College of Sports Medicine. ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription, 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins: 2014. SJ Keteyian, SJ, et al. Incorporating Patients With Chronic Heart Failure Into Outpatient Cardiac Rehabilitation. JCRP, 2014:Volume 34, Number4 Lynne Hamilton Weir, PT, CYT [email protected]