* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hemolysis-a.v.
Survey
Document related concepts
Nutriepigenomics wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
X-inactivation wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Transcript
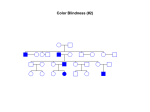
Hemolysis Increased cell destruction Rate of destruction exceeds the capacity of the bone marrow to produce red blood cells (RBC) Normal RBC survival time is 110-120 days Approximately 1% of RBC are removed each day and replaced by the marrow to maintain the RBC count Hemolysis During hemolysis RBC survival is shortened and increased marrow activity results in a heightened reticulocyte percentage Hemolysis can be divided into two Intravascular hemolysis Extravascular hemolysis Hemolysis Extravascular hemolysis The degradation of Hb results in the biliary excretion of heme pigments and increased fecal urobilinogen Gallstones composed of calcium bilirubinate may be formed in children as young as 4 years of age Hemolysis Intravascular hemolysis Hb binds to haptoglobin and hemopexin both of which are reduced Oxidized heme binds to albumin to form methemalbumin which is increased When the capacity of these binding molecules is exceeded, free Hb appears in the plasma (evidence of intravascular hemolysis) When the tubular reabsorbtive capacity of kidneys for Hb is exceeded free Hb appears in the urine Hemolytic anemia Hemolysis A feature of hemolytic anemia is a reduction in the normal red cell survival of 120 days The premature destruction of RBC may result from corpuscular abnormalities such as Increased cell destruction Hb defects, abnormalities of RBC enzymes or defects of RBC membrane Other defects may result from extracorpuscular abnormalities and may be due to immune or non-immune mechanisms Hemolytic anemia The approach to the diagnosis of hemolytic anemia should include Consideration of the clinical features suggesting hemolytic disease Demonstration of the presence of hemolytic process by laboratory means Establishment of the presice cause of the hemolytic anemia by special hematologic investigations Hemolytic anemia-Clinical features(1) The following clinical features suggest hemolysis Age: anemia and jaundice in an Rh(+) infant born to a Rh(-) mother or a group A or B infant born to a group O mother History of anemia, jaundice or gallstones in family Persistent/ recurrent anemia associated with reticulocytosis Anemia unresponsive to hematinics Intermittent/persistent indirect hyperbilirubinemia Hemolytic anemia-Clinical features(2) Splenomegaly Hemoglobinuria Presence of multiple gallstones Chronic leg ulcers Development of anemia or hemoglobinuria after exposure to certain drugs Dark urine Hemolytic anemia-laboratory findings Reduced cell survival and evidence of accelerated Hb catabolism Evidence of increased erythropoiesis Hemolytic anemia-laboratory findings Accelerated Hb catabolism Extravascular Raised unconjugated bilirubin Raised fecal and urinary urobilinogen Intravascular Hemoglobinuria Low/absent plasma haptoglobin Raised plasma methemalbumin Hemolytic anemia-laboratory findings Increased erythropoiesis (response to a reduction in Hb) Reticulocytosis Increased MCV Increased normoblasts in peripheral blood Spesific morphological abnormalities Sickled cells, target cells, spherocytes Erhytroid hyperplasia of bone marrow Expansion of marrow space Prominence of frontal bones, broad cheek bones, widened intratrabecular spaces, hair-on-end appearance of skull radiographs normal Hypochromic, microcytes macrocytes Target cells schistocytes Tests used to establish a spesific cause of hemolytic anemia (1) Membrane defects (Hereditary spherocytosis, elliptocytosis, stomatosis, acantocytosis) Blood smear Increased RBC osmotic fragility (spherocytes lyse in higher concentrations of saline than normal RBC) Autohemolysis at 24 and 48 hours Enzyme defects (G6PD and pyruvate kinase) Heinz body preparation Autohemolysis test Screening tests for enzyme deficiencies Tests used to establish a spesific cause of hemolytic anemia (2) Hemoglobin defects (sickle cell disease, thalassemias) Blood smear, sickle cell, target cell Sickling test Hemoglobin electrophoresis HbF determination Tests used to establish a spesific cause of hemolytic anemia (3) Immune hemolytic anemia Isoimmune Autoimmune Mismatched blood transfusion Hemolytic disease of the newborn Action of Ig Idiopathic, secondary to number of conditions Coombs’ test (+) Tests used to establish a spesific cause of hemolytic anemia (4) Non-immune hemolytic anemia Infections, drugs, underlying hematologic disease- microangiopathic HA, hypersplenism Coombs’ test (-) Congenital hemolytic anemias Membrane defects Enzyme defects G6PD deficiency Hemoglobin defects Hereditary spherocytosis(HS) ıntracorpuscular - thalassemia (quantitative hemoglobinopathies) HbS (qualitative hemoglobinopathies) Hemolytic disease of the newborn (isoimmune) Hereditary spherocytosis Familial hemolytic disorder Marked heterogenicity of clinical features Asymptomatic condition Fulminant hemolytic anemia The morphologic hallmark of HS Microspherocyte Caused by loss of membrane surface area Abnormal osmotic fragility Hereditary spherocytosis HS usually is transmitted as an autosomal dominant trait An autosomal recessive mode of inheritance also occurs 20-25% of all HS cases HS is encountered worldwide Hereditary spherocytosis An intrinsic genetic defect causes defects in membrane proteins The major complications Aplastic or megaloblastic crisis Hemolytic crisis Cholecystitis and cholelithiasis Severe neonatal hemolysis Hereditary spherocytosisPathophysiology HS erythrocytes are caused by membrane protein defects resulting in cytoskeleton instability Four abnormalities in red cell membrane proteins have been identified Spectrin deficiency alone (most common) Combined spectrin and ankyrin deficiency Band 3 deficiency(10-20% of patients) Protein 4.2 defects (common in Japan) Hereditary spherocytosisPathophysiology Spectrin deficiency Loss of erythrocyte surface Spherical RBC Hemolysis primarily confined to the spleen Culled rapidly from the circulation by the spleen Splenomegaly Extravascular hemolysis Biochemical spectrin deficiency and the degree of spectrin deficiency are reported to correlate with the extent of spherocytosis, the degree of abnormality on osmotic fragility test results and the severity of hemolysis Hereditary spherocytosisPathophysiology Ankyrin defects Ankyrin is the principal binding site for spectrin on RBC membrane A proportional decrease in spectrin content occurs although spectrin synthesis is normal 75-80% of patients with autosomal dominant HS have combined spectrin and ankyrin deficiency Deletion of chromosome 8 are shown to have a decrease in RBC ankyrin content Hereditary spherocytosisClinical findings Anemia Jaundice Splenomegaly Clinical features of HS Hereditary spherocytosisClinical findings(2) Anemia or hyperbilirubinemia may be of such magnitude as to require exchange transfusion in the neonatal period Anemia is mild to moderate Sometimes severe/not present In patients with mild HS cholelithiasis may be the first sign of underlying disease Moderate HS (most common, 60-75%) Mild HS (20-30%) Severe HS (5%, requires RBC transfusions) Hereditary spherocytosisLaboratory findings Minimal or no anemia Reticulocytosis Increased MCHC Spherocytes on the peripheral blood smear Hyperbilirubinemia Abnormal osmotic fragility test Howell-Jolly bodies may be seen hemolysis of HS cells may be complete at a solute concentration that causes little or no lysis of normal cells LDH increased Increased unconjugated bilirubin Looking for abnormalities in spectrin, ankyrin, band 3 (not routine) Hereditary spherocytosisTreatment Neonates Aplastic crisis Phototherapy/exchange transfusion RBC transfusion Folic acid supplementation to prevent megaloblastic crisis Splenectomy (after 6 years of age) Increased Hb level Decreased reticulocyte count Appereance of Howell-Jolly bodies and target cells Thrombocytosis Glucose 6 phosphate dehydrogenase deficiency (G6PD) X-linked disorder Homozygous women are found in populations in which the frequency of G6PD is high Heterozygous carrier women can develop hemolytic attacks Polymorphic with more than 300 reported variants The highest prevalance rates are found in tropical Africa, the Middle East, some areas of Mediterranean (severe forms) Glucose 6 phosphate dehydrogenase deficiency- Pathophysiology G6PD enzyme catalyzes the oxidation of glucose-6-phosphate to 6phosphogluconate while reducing the oxidized form of nicotinamide adenine dinucleotide phosphate (NADP+) to nicotinamide adenine dinucleotide phosphate (NADPH) Glucose 6 phosphate dehydrogenase deficiency- Pathophysiology NADPH Protects the cells against oxidative stress Required cofactor in many biosynthetic reactions Maintains glutathion in its reduced form Glutathion acts a scavanger for dangerous oxidative metabolites in the cell Converts harmful hydrogen peroxide to water with the help of glutathion peroxidase Glucose 6 phosphate dehydrogenase deficiency- Clinical findings The most common clinical feature is no symptoms Symptomatic patients Neonatal jaundice Acute hemolytic anemia Appears by age 1-4 days Often requires exchange transfusion Results from stress factors such as oxidative drugs or chemicals, infection or ingestion of fava beans Jaundice and splenomegaly may be present during crisis Glucose 6 phosphate dehydrogenase deficiency- Laboratory findings Anemia Reticulocytosis Activity of G6PD is low (after hemolysis) Indirect hyperbilirubinemia Serum haptoglobin levels will be decreased Formation of bodies which consist of denaturated hemoglobin Heinz body Glucose 6 phosphate dehydrogenase deficiency- Treatment Avoid oxidant drugs Antimalarial drugs, nitrofurantoin, nalidixic acid, ciprofloxacin,methylene blue, chloramphenicol, phenazopyridine, vit K analogs, sulfonamides, acetanilid, doxorubicine, isobutyl nitratre, naphtalene, phenylhydrazine, pyridoxin Exchange transfusion RBC transfusion Thalassemia (Cooley’s anemia, Mediterranean Anemia) Genetically determined defect in Hb synthesis An inability to manufacture sufficient quantities of globin chains In the adult there are 3 Hb types normally present Hb A 22 (95% of total) Hb A2 22 (3% of total) HbF 22 (2% of total) During fetal life the majority of Hb During embryonic life at least 2 different Hbs are produced Gowers 2 22 chains Gowers 1 4 chains The manufacture of each of these chains is controlled by spesific genes Thalassemia In thalassemia there is a genetic failure in the production of globin chains Failure of production of and chains is the most common thalassemia a failure of beta chain production thalassemia a failure of alpha chain production Beta Thalassemia The genes controlling beta chain production are located on chromosome 11 thalassemia major If both genes fail thalassemia minor If only one gene fails Beta Thalassemia minor (Heterozygous) (B+) Most common of thalassemias Beta chain production is less than normal Alpha chain production continues at a near normal rate Decreased level of HbA Excess alpha chains stimulates the increased production of delta chains Increased amount of HbA2 Rate of gamma chain production is greater Increased amount of HbF Beta Thalassemia minor These patients are not severely anemic These patients can be provided appropriate genetic counselling Hb, Hct are decreased RBC count is not as low as the Hb and Hct Bone marrow produce the cells but cannot fill them with Hb RBCs are microcytic and hypochromic Normal RDW Beta Thalassemia minor MCV is slightly decreased MCH is decreased MCHC is normal WBC count is normal Reticulocyte count is relatively increased Bone marrow is either normal or undergoes slight erythroid hyperplasia Serum iron,ferritin is normal Bilirubin slightly increase due to intramedullary hemolysis Beta Thalassemia minor Hb studies HbA decreased HbA2 increased HbF slightly increased to normal Beta Thalassemia major (homozygous)(B0) Complete failure of beta chain production Raised levels of HbA2 and HbF HbF has a very high affinity for oxygen (poor oxygen deliverer) Only functional Hb is HbA2 The patient is hypoxic İncreased erythropoietin production Stimulates the marrow to maximum Typical facial appereance Splenomegaly Extramedullary hemopoiesis Beta Thalassemia major Patients develop a life threatening anemia by one or two months (mostly often 6 months) Severe anemia (Hb:2-3 mg/dl) MCV, MCH, MCHC are all decreased RDW is increased Hypochromic microcytic RBC Hct and RBC count are also decreased Anisocytosis, poikilocytosis, target cells Reticulocytosis WBC is increased at the beginning Beta Thalassemia major Bone marrow undergoes erythroid hyperplasia Serum Fe increased/normal Ferritin increased/normal Hb electrphoresis HbA decreased HbA2 variable HbF increased Beta Thalassemia major The patients must be supported with blood transfusions which result in iron overload Unless iron is removed with appropriate chelation therapy these patients die of hemosiderosis Splenectomy When the yearly transfusion requirement of packed red cells exceeds 200-250 ml/kg Bone marrow transplantation Alpha thalassemia Four genes coding for alpha chain production These genes are located on chromosome 6 There are at least five forms of alpha thalassemia depending on the number and location of abnormal genes Hydrops fetalis- Homozygous alpha thalassemia All genes are abnormal There is no alpha chain production No HbF production and death in utero At autupsy the cord blood shows severe anemia There is no HbA and HbF on electrophoresis most of the Hb is HbBart’s which consists of 4 gamma chains Hemoglobin H disease Three genes are abnormal and one gene is coding for alpha chains Limited production of HbF in utero and HbA after birth The excess gamma chains form HbBart’s and the excess beta chains form HbH Unstable hemoglobins precipitate in the cell Premature destruction in the marrow and spleen with splenomegaly Infant is anemic at birth RBC and hct count are also decreased Hemoglobin H disease MCV, MCHC, MCH decreased RDW is increased Microcytosis, hypochromia Reticulocyte count is slightly increased Bone marrow undergoes erythroid hyperplasia Serum iron,ferritin increased Hb electrophoresis Hb Bart’s increased at birth Hb Bart’s 2-10% later HbH 5-40% HbA and A2 decreased Heterozygous alpha thalassemia (minor) Depends on whether or not the two deleted genes are on the same chromosome In alpha th O, both genes are absent from the same chromosome In alpha th +, one gene is missing from each chromosome In both forms Minor changes Mild anemia MCV and MCHC are borderline low Hb electrophoresis is normal with increased levels of HbBart’s if the cord blood is electrophoresed Alpha thalassemia silent Only one of the four genes is abnormal There is a near normal production of alpha chains with very few if any clinical or laboratory changes Beta thalassemia variants Delta/beta th Similar to beta th Symptoms are milder HbA decreased HbF 5-15% HbA2 normal HbLepore No normal beta or delta chain HbF 80-90% HbA absent (Homozygous) clinical and lab.findings are identical to Beta th HbA2 absent HbLepore 10% Beta thalassemia variants HbLepore HbA decreased HbA2 decreased HbLepore 10% (Heterozygous) clinical and lab.findings are identical to Beta th minor Sickle cell anemia Qualitative hemoglobinopathy Valine is substituted instead of glutamine in the sixth position on the globin molecule Sickle cell anemia is caused by homozygosity for the sickle cell gene and is the most common form of sickle cell disease The charge at this site is altered and allows for polymerization of Hb under conditions of hypoxia Sickle cell anemia Polymerization of sickle Hb distorts erythrocyte morphology causing a marked reduction in RBC life span increases blood viscosity predisposes to episodes of vasoocclusion Sickle cell anemiaclinical findings Children are normal at birth Onset of symptoms is unusual before 3-4 months of age High levels of HbF inhibits sickling Moderately severe hemolytic anemia is often present by age 1 year Pallor,fatigue, jaundice Predispozition to the development of gallstones Sickle cell anemiaclinical findings Intense congestion of the spleen with sickled cells may cause splenomegaly in early childhood and results in functional asplenia as early as age 3 months Acute splenic sequesteration Sudden enlargement of spleen with pooling of red cells Great risk for infection with encapsulated bacteria Acute exacerbation of anemia, shock, death Aplastic crisis Caused by infection with human parvovirus Sickle cell anemiaclinical findings Vasoocclusive crisis Hand-foot syndrome Abdominal pain Musculoskletal pain Stroke Acute chest syndrome Fever, pleuritic chest pain, acute pulmonary infiltrates Sickle cell anemialaboratory findings Decreased Hb (7-10 g/dl) with normal MCV Reticulocytosis Characteristic sickle cells Hb electrophoresis HbS (SCA with 0 th; HbF and S) (sickle +th;HbS with lesser HbA) Most infants with sickle hemoglobinopathies born in USA are now identified by neonatal screening Sickle cell anemia-treatment Patient and family education Prevention of complications and optimization of health All children should be immunized with the conjugate pneumococcal vaccine At the age of 2 months all children should begin penicillin prophylaxis At least at 5 years of age Sickle cell anemia-treatment Treatment of painful vaso-occlusive episodes RBC transfusion Adequate hydration Correction of acidosis if present Administration of analgesics Maintenance of normal oxygen saturation Treatment of associated infection In acute exacerbation Exchange transfusion Hydroxyurea Bone marrow transplantation Sickle cell trait Individuals who are heterozygous for the sickle gene Hb electrophoresis HbA 60% HbS 40% Normal levels of A2 and F No anemia, no hemolysis Sickle cell trait Exposure to environmental hypoxia may precipitate splenic infarction or sequestration Sudden death during exercise? Hematuria Bacteriuria Intraocular bleeding Genetic counselling is important HbE Hemoglobinopathy (not a thalassemia) Production of abnormal globin chains Beta chain variant in which lysine is substituted for glutamic acid in position 26 Mild anemia Reticulocyte count slightly increased Serum iron, ferritin increased/normal The catabolism of 1 gr Hb yields 35 mg of bilirubin Red blood cell of the newborn has a shortened life span= 70-90 days Significant bilirubin load Albumin binding of unconjugated bilirubin may be important in the prevention of toxicity (kernicterus) In the hypoglycemic infant, glucuronide production may be limited and thus conjugation is impaired The presence of β-glucuronidase in the bowel lumen during fetal life enables bilirubin to be reabsorbed and transported across the placenta for excretion by the maternal liver Overproduction of bilirubinHemolytic disease of the newborn Blood group incompatibilities such as Rh, ABO or minor blood groups exist between a mother and her fetus Rh(-) mother can become sensitized to the Rh Antigen Improperly matched blood transfusion Occurance of fetal-maternal blood transfusion During pregnancy, delivery, abortion, amniocentesis Hemolytic disease of the newborn Rh antigen Maternal antibody production IgG crosses placenta into the fetal circulation Reacts with the Rh Ag on fetal erythrocytes These antibody coated cells are recognized as abnormal and are destroyed by the spleen Production of bilirubin Hemolytic disease of the newborn Mild hemolysis Severe anemia, erythroblastosis fetalis Cardiac decompensation, massive anasarca, circulatory collapse Hydrops fetalis (abnormal fluid in two or more fetal compartments) The use of anti-D gammaglobulin (rhoGam) including antenatal administration at 26-28 weeks’ gestation ABO incompatibility ABO incompatibility is limited to mothers of blood group O and affects infants of blood group A or B All group O individuals have naturally occurring anti-A and anti-B antibodies, previous sensitization is not necessary Clinical disease is milder spherocytosis poikilocytosis acanthocytosis eliptocytosis stomatocytosis Fragmentation hemolysis Sickle cell anemia; target cells and sickled cells Target cells Thalassemia; severe hypochromia Normal RBC Heinz body anemia Anisopoikilocytosis, target cells normal Hypochromic, microcytes macrocytes Target cells schistocytes