* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Acute Angle Closure Glaucoma
Mitochondrial optic neuropathies wikipedia , lookup
Contact lens wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Vision therapy wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Visual impairment wikipedia , lookup
Diabetic retinopathy wikipedia , lookup
Keratoconus wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Cataract surgery wikipedia , lookup
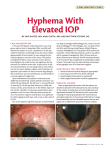
Acute Angle Closure Glaucoma Dr Tamara Al-Talib GP ST2 21st November 2013 Aims Definition Pathophysiology Epidemiology Presentation & Diagnosis DDx Management Follow-up Complications Prognosis Definition Glaucoma: Several ocular diseases that ultimately result in increased intraocular pressure (IOP) and decreased visual acuity. Acute angle-closure glaucoma (AACG) is an ocular emergency Defined as at least 2 of the following symptoms: ocular pain nausea/vomiting history of intermittent blurring of vision with halos and at least 3 of the following signs: IOP greater than 21 mm Hg conjunctival injection corneal epithelial edema mid-dilated nonreactive pupil and shallower chamber in the presence of occlusion. Pathophysiology Aqueous humor is produced by the ciliary body in the posterior chamber of the eye. It diffuses from the posterior chamber, through the pupil, and into the anterior chamber. From the anterior chamber, the fluid is drained into the vascular system via the trabecular meshwork and Schlemm canal contained within the angle. Several anatomic abnormalities lead to anterior chamber crowding and predispose individuals to AACG. a narrow angle has the most devastating consequences shallower anterior chambers thinner ciliary bodies a thinner iris anteriorly situated thicker lens and a shorter axial eye length. Precipitating factors Drugs (sympathomimetics, anticholinergics, antidepressants [SSRIs], anticonvulsants, sulfonamides, cocaine, botulinum toxin dim light rapid correction of hyperglycemia. Case reports have identified AACG associated with carotid-cavernous sinus fistula, trauma, prone surgical positioning, and giant cell arteritis Epidemiology Mortality/Morbidity Dependent on duration from onset to treatment, underlying ocular disease, and ethnicity. The degree of IOP elevation has been shown to have less impact on future visual acuity. Studies report that as many as two thirds of individuals with AACG had no visual field loss. Race AACG occurs in 1 of 1000 whites, about 1 in 100 Asians, and as many as 2-4 of 100 Eskimos. Sex AACG predominately affects females because of their shallower anterior chamber. Age Elderly patients in their sixth and seventh decades of life are at greatest risk. Presentation - History Periorbital pain-‟boring‟ Associated with ipsilateral headache Visual deficits- blurry vision and describe the phenomenon of "seeing halos around objects.“ In a large percentage of patients, extraocular symptoms and systemic manifestations are the chief complaint. Headache Nausea and/or vomiting abdominal pain Precipitating factors Presentation - Examination Visual acuity, the external eye, visual fields, a fundoscopic examination, pupils, ocular motility, and IOP. Slit-lamp evaluation: corneal edema, synechiae, irregular pupil shape or function, or segmental iris atrophy. Patients complain of blurred vision, and testing reveals the ability only to detect hand movements. They are unable to identify numbers and letters on distance charts or near cards. Cornea and scleral injection and ciliary flush are present. The obviously edematous and cloudy cornea obscures the fundoscopic examination. Increased IOP (normal limit, 10-20 mm Hg) and ischemia result in pain on eye movement, a mid-dilated nonreactive pupil, and a firm globe. Diagnosis Clinical presentation and a physical examination. No definitive laboratory or imaging studies are available. However, tonometry must be performed and must demonstrate increased intraocular pressure (IOP). „‟TIME SENSITIVE DIAGNOSIS!” DDX Acute Orbital Compartment Syndrome Conjunctivitis Corneal Abrasion Corneal Laceration Corneal Ulceration and Ulcerative Keratitis Endophthalmitis Glaucoma, Malignant Glaucoma, Neovascular Herpes Zoster Ophthalmicus Iritis and Uveitis Orbital Infections Periorbital Infections Ultraviolet Keratitis Vitreous Hemorrhage Management: GOAL = reduce IOP Prehospital Care: Emergency !! 1. Suppressing aqueous comfort and reduce IOP. It is alsohumor believed that, while supine, the production lens falls away from the iris decreasing pupillary block. Remain in the supine position as long as possible-may aid in Avoid eye patches, covers, or blindfolds - maintaining the conditions that cause pupillary dilation 2. Reversing Hospital Care: inflammation 3. Eliminating pupillary block Medical management is the first step - decreases the duration of elevated IOP and the potential for visual field loss. Management – Initial Tx Decrease IOP-decrease aqueous humor production and to enhance opening of the angle Carbonic anhydrase inhibitors - Acetazolamide should be given as a stat dose of 500 mg IV followed by 500 mg PO Topical Beta-adrenergic blockers - (ie, carteolol, timolol) Alpha-adrenergic agonists – (ie. apraclonidine, brimonodine) can be added for a further decrease in IOP. Decrease the inflammatory reaction and reduce optic nerve damage. Topical Corticosteroids- (ie. Prednisolone ophthalmic), 1-2 doses Extraocular manifestations analgesics for pain antiemetics for nausea and vomiting-can drastically increase IOP Management – Reassessment Ophthalmic agents, miotic- (Pilocarpine) opening of the angle Approx 1 hour after beginning treatment, administered every 15 minutes for 2 doses. In the initial attack, the elevated pressure in the anterior chamber causes a pressure-induced ischemic paralysis of the iris. At this time, pilocarpine would be ineffective. During the second evaluation, the initial agents have decreased the elevated IOP and hopefully have reduced the ischemic paralysis so pilocarpine becomes beneficial in relieving pupillary block. Pilocarpine must be used with caution! -constricting the ciliary muscle, increase the axial thickness of the lens and to induce anterior lens movement. This could result in reducing the depth of the anterior chamber and worsening the clinical situation in a paradoxical reaction. Management – Reassessment Hyperosmotics – (ie. PO glycerin, isosorbride –in diabetics or IV mannitol) If the IOP is not reduced 30 minutes after the second dose of pilocarpine reduce vitreous volume, which, in turn, decreases IOP. !!osmotic diuresis-not for cardiovascular and renal patients. Repeat doses may be necessary if no effect is seen and if tolerated. Management – Reassessment Corneal indentation (CI) used as a temporizing measure to reduce IOP until definitive treatment is available. Laser peripheral iridotomy (LPI)-DEFINITIVE Tx performed 24-48 hours after IOP is controlled LPI may be offered prophylactically to individuals anatomically predisposed to AACG if identified before the first acute attack. Argon laser peripheral iridoplasty (ALPI) burns made in the peripheral iris resulting in iris contraction and opening of the angle Anterior chamber paracentesis (ACP) Follow up Patients remain on oral acetazolamide, pilocarpine, and beta- blockers or alpha-agonists until definitive treatment. After laser peripheral iridotomy (LPI), 33% of patients require topical medication to maintain lower IOP. Complications Permanent decrease in visual acuity Repeat episode Malignant glaucoma Fellow eye attack Central retinal artery occlusion Central retinal vein occlusion Prognosis With adequate treatment, most patients recover their lost vision. In whites, IOP was controlled with LPI alone in 65-76%. Asians more often have medically refractory initial attacks and require medications after LPI. They also have higher rates of visual field loss and subsequent increases in IOP. Thank you