* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cell wall deficient bacteria
Survey
Document related concepts
Transcript
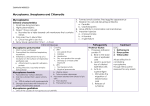
Mycoplasmas and Cell Wall Defective Bacteria Mycoplasmas smallest known free-living organisms Due to their smallest size, originally thought to be viruses, but differ in i) Contain both RNA and DNA ii) Can synthesize proteins by their own enzymes iii) Can multiply on their own Classification For many years thought to be viruses Nowdays classified as atypical bacteria because they lack the cell wall At least 15 spp are thouhgt to be of human origin, only 4 spp are of medical importance Spp. Disease M.pneumoniae . atypical pnuemoina M.hominis . postpartum fever . pelvic inflamatory diseases Ureaplasma urealyticum . non gonococcal urethritis . lung diseases in premature infants of low birth weight (LBW) M.genitalium . Urethral infections General characterisitcs Smallest organisms that can be free living 125250 nm in size Highly pleumorphic because of lack of rigid cell wall Completely resistant to penicillin cephalosporins because of lack of cell wall and Can reproduce in cell free media, on agar produce colonies of fried egg appearance Have affinity for mammalian cell membrane Morphology Stain poorly with bacteria stain (gram stain), but stain well with Giemsa stain They lack cell wall so: Highly pleomprphic Not stained with gram stain Can’t be killed by penicillin On Giemsa stain they appear as tiny pleomorphic cocci, short rods, short spirals, and sometimes as hollow ring forms. Their diameter ranges from 0.15 µ to 0.30 µ Growth and Cultural Characteristics Cannot be studied by usual bacteriologic methods because of the small size of their colonies and delicacy due to lack of rigid cell wall Facultative anaerobes except for M.pneumoniae that are strict aerobe Grows better on H2 and N2 with 10% CO2 Most grow at 370C. Generation time slow, 1-6 hrs Use glucose as energy source Many strains grow in heart infusion peptone broth with 2% agar, pH 7.8 and animal serum or 30% ascitic fluid added Mycoplsama contain sterols in their cell membrane, so their growth requires the addition of serum or cholestrol to the medium to produce sterols, Ureaplasma reqiure urea After 2-6 days of incubation, produce small colonies that have freid- egg appearance Pathogenesis Pathogenic Mycoplasma have polar tips structures-mediate adherence to host cells Direct cytotoxicity through generation of hydrogen peroxide and superoxide radicals Cell lysis-by antigen antibody reactions/ chemotaxis and action of mononuclear cellls Medical importance Part of normal flora of mouth, genitourinary tract especially females i) Asymptomatic Many infections asymptomatic. due to Mycoplsmas are Medical importance ii) Mycopasma pneumoniae and pneumonia (walking pneumonia) atypical M.pneumoniae is a prominant cause of a typical pneumonia especially in persons 5-20 years of age transmitted by infected respiratory secretions Incubation period 1-3 wks Generally mild disease, but can range from asypmtomatic infection-serious pneumonitis Complications-neorologic, hemolytic anaemia, skin lesions Medical importance iii) Mycoplsma hominis uterine tube infections (salpingitis and tubo-ovarian abscesses) 10% post abortal or post partum fever(10%) Occasionally arthritis Medical importance IV) Ureaplasma urealyticum Common in female genital tract Attributed to some cases gonococcal urethritis in men Associated with lung disease in premature LBW infants Weak evidence correlates U.urealyticum to infertility of non Medical importance V) Mycoplasma genitalium Attributed to some cases of non acute and chronic non-gonococcal urethritis in men In females, M.genitalium has been associated with cervicitis, endometritis salpingitis and infertility Diagnosis Specimen include, blood,sputum,nasopharyngial or urethral exudates Direct staining is of limited use. For direct detection in clinical specimen : . IF . PCR Culture is difficult and time consuming Diagnosis Serology (most widely used) Detection of IgM or rising titer of IgG by ELISA or CFT (acute and convalescent phase sera are necessary to demonstrate a fourfold rise in the CF antibodies) Cold agglutinins at a titer of 1/128 or higher = acute infection (Heamoaglutination) Cold agglutinins? Positive in? Specific? o Certain antigens on human red blood cells are identical to Mycplasma pneumonia antigens. So, antibodies to mycoplasma cross react with human red blood cells causing them to agglutinate at 4 degree but not at 37 degree o Positive in 50 % of cases o Not specific. Positive in other diseases like viral infections & malaria Treatment Lack of cell wall make organisms resitant to antimicrobials acting on cell wall e.g penicillines, cephalosporins and vancomycin Sensitive to antimicrobials that inhibit protein synthesis e.g. tetracyline, erythromicin , azithromycin and chloramphenical Other Cell wall- defective bacteria (L-forms bacteria) First isolated in 1935 by Emmy Klienburger who named them Lforms (Lister Institute in London where she was working) Don’t occur naturaly and not genetically related to mycoplasma Usually result from Spontaneous mutation Effects of chemicals Enzymes (lysozymes) Antibiotic treatment Other Cell wall- defective bacteria (L-forms bacteria) Two types: Protoplast (stable L-forms) usually derived from gram positive bacteria in which the cell wall is completely destroyed.They can’t be reverted to their original morphology. Spheroplast (unstable L-forms) usually derived from gram negative bacteria in which cell wall is not completely destroyed; they retain some outer membrane material and can revert to their original morphology. Their role in disease is uncertain; may be responsible for the recurance of the infection after antimicrobial treatment. L Forms vs Mycoplasma contain a rigid cell wall, at least at one stage of their life cycle no sterols in their cytoplasmic membrane