* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Diarrhoea
Transmission (medicine) wikipedia , lookup
Germ theory of disease wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Globalization and disease wikipedia , lookup
Infection control wikipedia , lookup
Rotaviral gastroenteritis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
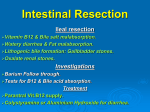
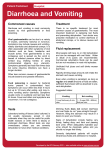
IMS : Diarrhoea By Semester 6 and Smester 7 Agenda of the day • Overview of diarrhoea -Ambiga and Hui Yan • Acute Diarrhoea (Acute Gastroenteritis) -Wen Jiun and Vanessa Epidemiology of Diarrhoea • Leading cause of illness and death among children in developing countries. • estimated 1.3 thousand million episodes and 4 million deaths occur each year in under-fives. • Main cause of death from acute diarrhoea is dehydration. Other important causes of death are dysentery and undernutrition. Definitions Acute Diarrhoea – sudden onset and lasts less than two weeks – 90% are infectious in etiology – 10% are caused by medications, toxin ingestions, and ischemia Chronic Diarrhoea – Diarrhoea which lasts for more than 4 weeks – Most of the causes are non-infectious Persistent Diarrhoea -Diarrhoea lasting between 2 to 4 weeks Clinical Features • Stools – – – – • • • • • • Loose Blood stained Offensive smell Steatorrhea (floating, oily, difficult to flush) Sudden onset of bowel frequency Crampy abdominal pain Urgency Fever Loss of appetite Loss of weight Classifications of Diarrhoea • Duration( Acute, Chronic) • Causes( infectious, post-infectious, drugs, endocrine, factitious) • Chronic DirrhoeaPathophysiologic mechanism (osmotic, secretory, inflammatory, abnormal motility) • Acute Diarrhoea Viral,Bacterial, Protozoa (90%) Medications Laxatives or diuretic abuse Ingestion of environmental preformed toxin such as seafood Ischemic Colitis Graft versus Host • Chronic Diarrhoea Irritable Bowel Syndrome Diverticular disease Colorectal Cancer Bowel Resection Malabsorption Inflammatory Bowel Disease Celiac Disease Carcinoid tumour Mechanism of Diarrhoea • • • • Osmotic Diarrhoea Secretory Diarrhoea Inflammatory Diarrhoea Abnormal Motility Diarrhoea Osmotic Diarrhoea • Mechanism : -retention of water in the bowel as a result of an accumulation of non‐absorbable water‐soluble compounds -cease with fasting, discontinue oral agents • Causes : -Purgatives like magnesium sulfate or magnesium containing antacids -especially associated with excessive intake of sorbitol and mannitol. -Disaccharide intolerance -Generalized malabsorption Secretory Diarrhoea • Mechanism : – Active intestinal secretion of fluid and electrolytes as well as decreased absorption. – Large volume, painless, persist with fasting • Causes : – Cholera enterotoxin, heat labile E.coli enterotoxin – Vasoactive Intestinal Peptide hormone in VernerMorrison syndrome – Bile salts in colon following ileal resection – Laxatives like docusate sodium – Carcinoid tumours Inflammatory Diarrhoea • Mechanism : -damage to the intestinal mucosal cell leading to a loss of fluid and blood -pain, fever, bleeding, inflammatory manifestations • Causes : -- Immunodeficiency patient – Infective conditions like Shigella dysentary – Inflammatory conditions • Ulcerative colitis and Crohns disease Abnormal Motility Diarrhoea • Mechanism : -Increased frequency of defecation due to underlying diseases -large volume, signs of malabsorption (steatorrhoea) • Causes : – – – – Diabetes mellitus- autonomic neuropathy Post vagotomy Hyperthyroid diarrhoea Irritable Bowel Syndrome ACUTE GASTROENTERITIS Acute Gastroenteritis • Gastroenteritis is the inflammation of the lining of stomach, small and large intestine. • >90% of cases are infectious, although acute gastroenteritis may follow ingestion of drugs and chemical toxins (10%). • Acute gastroenteritis is common among children, elderly, and those who are immunocompromised. Infectious Agents • Acquired by – fecal-oral route via direct personal contact – ingestion of food or water contaminated with pathogens from human or animal feces • Acute infection occurs when the ingested agent overwhelms the host’s mucosal immune and non-immune (gastric acid, digestive enzymes, mucus secretion, peristalsis, and suppressive resident flora) defenses. Aetiology: Causative Pathogens • Bacteria • Viral • Protozoa Bacterial • • • • • • • • • Campylobacter jejuni Salmonella sp. Shigella Escherichia coli Staphylococcal enterocolitis Bacillus cereus Clostridium perfringens Clostridium botulinum Gastrointestinal tuberculosis Viral • Rotavirus • Norovirus • Adenovirus Protozoa • Entamoeba histolytica • Cryptosporidium • Giardia intestinalis • Schistosomiasis High Risk Groups 1. 2. 3. 4. 5. Travelers Consumers of certain foods Immunodeficient person Daycare participants Institutionalized person 1. Travelers • Tourists to Latin America, Africa, and Asia develop “traveler's diarrhea” commonly due to enterotoxigenic Escherichia coli, Campylobacter, Shigella, and Salmonella. • Visitors to Russia may have increase risk of Giardia-associated diarrhea. • Visitors to Nepal may acquire Cyclospora. • Campers, backpackers, and swimmers in wilderness areas may become infected with Giardia. 2. Consumers of Certain Food • Diarrhea closely following food consumption may suggest infection with – Salmonella or Campylobacter from chicken; – Enterohemorrhagic Escherichia coli (O157:H7) from undercooked hamburger – Bacillus aureus from fried rice – S. aureus from mayonnaise or creams – Salmonella from eggs – Vibro species, acute hepatitis A or B from (raw) seafood 3. Immunodeficiency Persons • Primary immunodeficiency – IgA deficiency, common variable hypogammaglobulinemia, chronic granulomatous disease • Secondary immunodeficiency – AIDS, senescence, pharmacologic suppression 4. Daycare Participants • Infections with Shigella, Giardia, Cryptosporidium, rotavirus, and other agents are very common and should be considered. 5. Institutionalized Persons • Most frequent cause of nosocomial infections in many hospitals and long-term care facilities • The causes are a variety of microorganisms but most commonly Clostridium difficile. Pathophysiology • Infectious agents cause diarrhoea in 3 different ways as follows: – Mucosal adherence – Mucosa Invasion – Toxin Production Mucosal adherence - Bacteria adhere to specific receptors on the mucosa, e.g. adhesions at the tip of the pili or fimbriae - Mode of action: effacement of intestinal mucosa causing lesions, produce secretory diarrhoea as a result of adherence - Causing moderate watery diarrhoea - e.g. enteropathogenic E.coli Mucosa Invasion - The bacteria penetrate into the intestinal mucosa, destroying the epithelial cells and causing dysentery - e.g. Shigella spp. Enteroinvasive E.coli Campylobacter spp Toxin Production i) - ii) - Enterotoxins toxin produced by bacteria adhere to the intestinal epithelium, induce excessive fluid secretion into the bowel lumen, results in watery diarrhoea without physically damaging the mucosa. Some enterotoxin preformed in the food can cause vomiting e.g Staph.aureus (enterotoxin B) Bacillus cereus Vibrio cholerae Cytotoxins damage the intestinal mucosa and sometimes vascular endothelium, leads to bloody diarrhoea with inflammatory cells, decreased absorptive ability. e.g. Salmonella spp. Campylobacter spp. Enterohaemorrhagic E.coli 0157 Bacterial causes of watery diarrhoea and dysentery Watery diarrhoea Dysentery - Vibrio cholerae - Shigella spp - Enterotoxigenic E.coli (ETEC) - Yersinia enterocolitica - Enteropathogenic E.coli (EPEC) - Campylobacter spp - Salmonella spp. - Salmonella spp. - Clostridium difficile - Clostridium difficile - Clostridium perfringens - Enteroinvasive E.coli - Campylobacter jejuni - Enterohaemorrhagic - Bacillus cereus E.coli (EHEC) - Staphylococus aureus + profuse vomiting Clinical Features • Diarrhoea – Watery – Bloody • • • • • • Cramping abdominal pain Nausea, +/- Vomiting Fever Loss of appetite Lethargy Shock Investigations • • • • FBC U&E, BUN Stool culture Stool examination, microscopy for ova, cysts, parasites and fecal WBC • ELISA test ** For unresolved diarrhoea: sigmoidoscopy, rectal biopsy and radiological studies to rule out other organic causes Management Aims/Goals of management: • Prevent, identify and treat dehydration • Eradicate causative pathogens – Tetracycline, Ciprofloxacin • Prevent spread by early recognition and institution of infection-control measures – immunization, chemoprophylaxis, good hygiene, improve sanitation Prevent, Identify & Treat Dehydration • Moderate to severe dehydration need referral to hospital • Oral Rehydration Solution (ORS) – Glucose, Na, Cl, K, bicarbonate or citrate – encourage fluid intake e.g. salt + glucose drink to assist in co-transport of sodium into the epithelial cells via the SGLT1 protein, which enhances water and sodium reabsorption in small intestines. • IV fluids (lactate Ringer’s solution) are preferred in those with severe dehydration. Chronic Diarrhea Causes • • • Chronic Fatty Diarrhea (Diarrhea due to Malabsorption) Chronic Inflammatory Diarrhea Chronic Watery Diarrhea – – – • • • Secretory Diarrhea Osmotic Diarrhea Drug-Induced Diarrhea Infectious Diarrhea Malignancy Functional Diarrhea (diagnosis of exclusion) – Irritable Bowel Syndrome History 1. Age 2. Diarrhea pattern 3. Differentiating small bowel from large bowel 4. Stool characteristics 5. Diurnal variation 6. Weight Loss 7. Medication and dietary intakes 8. Recent travel to undeveloped areas Age • Young patients – Inflammatory Bowel Disease – Tuberculosis – Functional bowel disorder (Irritable bowel) • Older patients – Colon Cancer – Diverticulitis Diarrhea pattern • Diarrhea alternates with Constipation – – – – • Intermittent Diarrhea – – – • Colon Cancer Laxative abuse Diverticulitis Functional bowel disorder (Irritable bowel) Diverticulitis Functional bowel disorder (Irritable bowel) Malabsorption Persistent Diarrhea – – Inflammatory Bowel Disease Laxative abuse Differentiating small bowel from large bowel • Small intestine or proximal colon involved – Large stool Diarrhea – Abdominal cramping persists after Defecation • Distal colon involved – Small stool Diarrhea – Abdominal cramping relieved by Defecation Stool characteristics • • • Water: Chronic Watery Diarrhea Blood, pus or mucus: Chronic Inflammatory Diarrhea Foul, bulky, greasy stools: Chronic Fatty Diarrhea Diurnal variation • • No relationship to time of day: Infectious Diarrhea Morning Diarrhea and after meals – Gastric cause – Functional bowel disorder (e.g. irritable bowel) – Inflammatory Bowel Disease • Nocturnal Diarrhea (always organic) – Diabetic Neuropathy – Inflammatory Bowel Disease Weight Loss • Despite normal appetite – – • Associated with fever – • Hyperthyroidism Malabsorption Inflammatory Bowel Disease Weight loss prior to Diarrhea onset – – – – – Pancreatic Cancer Tuberculosis Diabetes Mellitus Hyperthyroidism Malabsorption Medication and dietary intakes • • • • • • Drug-Induced Diarrhea Food borne Illness Waterborne Illness High fructose corn syrup Excessive Sorbitol or mannitol Excessive coffee or other caffeine Recent travel to undeveloped areas • • Traveler's Diarrhea Infectious Diarrhea Colorectal Carcinoma • Colorectal carcinoma – Colorectal cancer is second commonest cancer causing death in the UK – 20,000 new cases per year in UK - 40% rectal and 60% colonic – 3% patients present with more than one tumour (=synchronous tumours) – A previous colonic neoplasm increases the risk of a second tumour (=metachronous tumour) – Some cases are hereditary – Most related to environmental factors - dietary red fat and animal fat • Adenoma - carcinoma sequence – – – – Of all adenomas - 70% tubular, 10% villous and 20% tubulovillous Most cancers believed to arise within pre-existing adenomas Risk of cancer greatest in villous adenoma Series of mutations results in epithelial changes from normality, through dysplasia to invasion – Important genes - APC, DCC, k-ras, p53. Colorectal Carcinoma • Clinical presentation – Right-sided lesions present with • Iron deficiency anaemia due occult GI Blood loss • Weight loss • Right iliac fossa mass – Left-sided lesions present with • Abdominal pain • Alteration in bowel habit • Rectal bleeding – 40% of cancers present as a surgical emergency with either obstruction or perforation Colorectal Carcinoma • Developed by Cuthbert Duke in 1932 for rectal cancers • Dukes staging of colorectal cancer – Stage A - Tumour confined to the mucosa – Stage B - Tumour infiltrating through muscle – Stage C - Lymph node metastases present – Five year survival - 90%, 70% and 30% for Stages A, B and C respectively Chronic Inflammatory Diarrhea • Inflammatory Bowel Disease – Ulcerative Colitis • is a form of colitis, a disease of the intestine, specifically the large intestine or colon • usually present with diarrhea mixed with blood and mucus, of gradual onset • also may have signs of weight loss, and blood on rectal examination – Crohn's Disease • is an inflammatory disease which may affect any part of the gastrointestinal tract from mouth to anus, causing a wide variety of symptoms. • It primarily causes abdominal pain, diarrhea (which may be bloody), vomiting, or weight loss, but may also cause complications outside of the gastrointestinal tract such as skin rashes, arthritis and inflammation of the eye – Diverticulitis Drug-induced diarrhea • Diarrhea - common side effect of many classes of medications. • Accounts for 7% of all adverse drug effects. • Over 700 drugs have been implicated. Medications commonly involved • • • • • • • Antibiotics Laxatives Antihypertensives Lactulose Antineoplastics Antiretroviral drugs Magnesium containing compounds • • • • • • Anti arrhythmics NSAIDs Colchicine Antacids Acid reducing agents Prostaglandin analogs Medication Laxatives Mechanism Osmotic diarrhea (osmotically active solutes) Stimulant laxatives Secretory diarrhea (excess of fluids & electrolytes) Erythromycin, cisapride Motility diarrhea (shortened transit time) Antimicrobials Pseudomembranous colitis (bacterial proliferation) Medication Antineoplastics NSAIDS Alpha-glucosidase inhibitor Lipase inhibitors (Orlistat) Mechanism Exudative diarrhea (protein losing enteropathy) Lymphocytic or collagenous colitis Malabsorption of carbohydrates (osmotic diarrhea) Malabsorption of fat (steatorrhea) Antibiotic-induced diarrhea • unexplained onset of diarrhea that occurs with the administration of any antibiotic • due to disruption of normal intestinal flora, which leads to • either proliferation of pathogenic microorganisms or impairment of the metabolic functions of the microflora Types • Simple antibiotic associated diarrhea • Erythromycin induced diarrhea • Clostridium difficile associated diarrhea Simple antibiotic associated diarrhea 1. disturbance in the normal colonic flora, leading to impaired fermentation of carbohydrates and osmotic diarrhea 2. reduced production of short-chain fatty acids which by reducing colonic absorption of fluid causes secretory diarrhea 3. reduced digestion of bile salts by normal colonic flora and the resultant increased colonic concentration can stimulate secretion of fluid by the colon and cause a secretory diarrhea • Occurs in dose-related fashion • more common in drugs given orally rather than parenterally, except with drugs excreted in the bile • generally resolves within days of discontinuing the offending antibiotic • typically have a larger impact on anaerobic bacteria in the normal fecal flora Common antibiotics involved • • • • • • • • • • Clindamycin Ampicillin Amoxicillin-clavulanate Cefixime Cephalosporins Fluoroquinolones Azithromycin Clarithromycin, Erythromycin Tetracyclines Erythromycin induced diarrhea • Caused by erythromycin • Increased motility through stimulation of motilin receptors Clostridium difficile associated diarrhea (CDAD) • not dose related • symptoms can last weeks to months after the offending antibiotic has been discontinued, • often until treatment for the infection is administered antibiotic therapy disturbance in the normal flora of the colon colonization of the individual by the organism (faecal-oral route) majority asymptomatic Symptomatic (1st day of antibiotic to 6 weeks after stopping the drug) Common antibiotics involved • • • • • Clindamycin Ampicillin Amoxicillin Quinolones Cephalosporins Clostridium difficile • gram-positive bacillus • spore-former, allowing it to survive under harsh conditions and during antibiotic therapy • development of infection caused by Clostridium difficile involves several steps • Clostridium difficile demonstrate production of 2 toxins • Toxin A – bind to specific receptors in the brush border of the intestinal epithelium • Toxin B – site of binding has not yet been described Toxin A & B Release of inflammatory mediators & cytokines Chemotaxis of inflammatory cells Increased fluid secretion by the epithelium Patchy necrosis with production of an exudate composed fibrin and neutrophils Pseudomembrane fomation (necrotic cellular debris, fibrin, mucin & leucocytes) Contributing factors to CDAD • • • • Host susceptibility to infection Virulence of the infecting strain Type of antibiotic used Timing of exposure Spectrum of disease • • • • Asymptomatic colonization Simple antibiotic associated diarrhea Pseudomembranous colitis Fulminant colitis Clinical features • • • • • • • Lethargy Abdominal pain Nausea Anorexia Water diarrhea Low-grade fever Peripheral leucocytosis Pseudomembranous colitis – more profuse diarrhea, occult bleeding, high fever. Fulminant colitis • 1-3% of patients with Clostridium difficile infection • Presentation –severe abdominal pain, distension, high fever, marked leucocytosis • Complications – colonic perforation, toxic megacolon Diagnosis of Clostridium difficile infection • Tissue culture assay for toxin B • ELISA for toxin A/B • Latex agglutination assays (detect enzyme glutamate dehydrogenase) Treatment of CDAD • Discontinuation of the offending antibiotic • Supportive fluids and electrolytes replacement • Enteric isolation precautions • Aviod antiperistaltic agents and opiates • Antibiotic is indicated for moderate to severe cases • 1st line : Vancomycin 125mg qds and metronidazole 250mg tds or bacitracin 25,000 units qds • Parenteral metronidazole 500mg qds may be used if oral agents are not tolerated • Used of probiotics in recurrent relapses of Clostridium difficile infection • Saccharomyces boulardii 1g od during concurrent antibiotic treatment Endocrine causes • Diabetic autonomic neuropathy • Thyrotoxicosis • Neuroendocrine tumours ~ Zollinger Ellison syndrome ~ VIPoma ~ Somatostatinoma ~ Carcinoid syndrome ~ Medullary carcinoma of thyroid Diabetic autonomic neuropathy • Reduces small bowel motility & • affects enterocyte secretion Bacterial overgrowth Watery, continuous/interrupted by constipation diarrhoea, worse at night(nocturnal diarrhoea) Other clinical features • • • • • Postural hypotension Gastroparesis ( nausea and vomitting) Difficulty in micturition ( bladder atony) Erectile dysfunction Gustatory sweating Treatment • • • • Broad spectrum antibiotics Antidiarrhoeal- Loperamide Alpha 2 adrenergic agonist- Clonidine Somatostatin analogue- Octreotide Thyrotoxicosis • Increase motility of GIT • Shortened transit time • Reduced time for action of bile on fat digestion • Malabsorption of nutrients Increased bowel movement, diarrhoea, mild steatorrhoea Other clinical features Symptoms • Weight loss • Increase appetitite • Heat intolerance • Palpitations • Tremor • Irritability Signs • Tachycardia • Goitre • Lid retraction • Lid lag Graves’ + ophthalmoplegia (diplopia) + pretibial myxoedema + thyroid acropachy Investigations • Serum T4 & TSH Treatment • Carbimazole • Propranolol Neuroendocrine tumours of pancreas Zollinger Ellison syndrome 1. Severe peptic ulceration 2. Gastric acid hypersecretion 3. Non beta cell islet tumour of pancreas (gastrinoma) Gastrinoma • Increase gastrin levels • Increase acid production by parietal cells of stomach • Small intestine pH low &acidic • Pancreatic lipase inactivated, bile acids precipitated • Diarrhoea & steatorrhoea Treatment: High dose proton pump inhibitors VIPoma • Vasoactive intestinal peptide (VIP) • Stimulate adenyl cyclase in enterocytes (stimulate secretion of water and electrolytes) • Secretory diarrhoea Clinical syndrome: watery diarrhoea, hypokalemia, metabolic acidosis Somatostatinoma • Function of somatostatin: suppress GI hormones, pancreatic hormones, pancreatic enzymes • Increase levels of somatostatin • Diabetes mellitus and diarrhoea/steatorrhoea Investigations • Fasting blood sample for: ~ Chromogranin A ~ Hormones ( gastrin, VIP, somatostatin) • Ultrasound scan, CT, MRI to look for tumours Treatment • Surgically resect solitary tumours • Somatostatin analogue (Octreotide) Carcinoid tumour • Most commonly found in small bowel • Local mass effect (obstruction, appendicitis) or • Hormone excess ~ ectopic ACTH or 5-HT (serotonin) Carcinoid syndrome- when vasoactive hormones reach systemic circulation Carcinoid syndrome • • • • • Flushing Wheezing ( bronchoconstriction) Diarrhoea Facial telangiectasia Cardiac involvement Investigations • 24 hour urine collection of 5HIAA (5 hydroxyindoleacetic acid) Medullary carcinoma of thyroid • Parafollicular C cells • Produce calcitonin & also 5HT • diarrhoea Post Gut Resection Diarrhoea Pathophysiology Mesenteric vascular occlusion Crohn’s disease Necrotising enterocolitis Volvulus Gut resection Injury/ trauma to the gut Tumours of the small intestine Short Bowel Syndrome (SBS) Impaired absorption of fluid and nutrients Diarrhoea * Normally, length of small intestine: 6m; in SBS, <2m * Factitious diarrhoea • 1. Purgative abuse • High diarrhoea volume, low serum potassium • Sigmoidoscope shows pigmented mucosa (melanosis coli) • Barium enema shows dilated colon • May be associated with eating disorders 2. Dilutional diarrhoea • dilute stools on purpose • Check stool osmolality and electrolytes Investigation of diarrhoea • Acute-self limiting diarrhoeaNo investigations are necessary • Investigations are indicated when: -Signs of Dehydration (electrolytes imbalances) -Chronic or persistent diarrhoea -Bloody Diarrhoea -Anemia, Weight loss, abdominal mass or suspicion of neoplasia -Patients with IBS with significant change of symptoms Irritable Bowel Syndrome • Functional bowel disorder • Absence of any organic causes Epidemiology • Young • <35 years old • Female Clinical Features • Abdominal pain or discomfort • Abdominal bloating/ distension • Change in bowel habits (constipation alternating with diarrhoea) • Urgency of bowel movements • Tenesmus Diagnosis • no specific laboratory or imaging test • Diagnosis of exclusion • Rome Criteria Rome III Criteria (2006) • Recurrent abdominal pain or discomfort at least 3 days per month during the previous 3 months that is associated with 2 or more of the following: – Relieved by defecation – Onset associated with a change in stool frequency – Onset associated with a change in stool form or apperance. Cont. • Supporting symptoms: – Altered stool frequency – Altered stool form – Altered stool passage (straining and/or urgency) – Mucorrhoea – Abdominal bloating or subjective distention Etiology • Currently unknown. • Thought to result from – an interplay of abnormal gastrointestinal(GI) tract movements – Increased awareness of normal bodily functions – Change in the nervous system communication between the brain and the GI tract, Cont. • Has also developed after episodes of gastroenteritis • Dietary allergies or food sensitivities (not yet proven) • Symptoms worsen during periods of stress or menses Management • • • • • • Exclusion diet Fiber supplements Laxatives Anti-diarrhoea medication Antispasmodic Antidepressants Blood Tests 1. Full Blood Count - Anemia? MCH? (iron deficiency? Anemia of chronic illness?) - MCV (inc in Crohn’s, celiac disease; dec in iron defi anemia) 2. Renal Profile - Electrolyte imbalances (dec K) 3. Arterial Blood Gas - Acid-Base balance (loss of alkali in diarrhoea) 4. HIV serology (opportunistic infection of the gutchronic diarrhoea) 5. ESR (cancer, IBD) 6. CRP (IBD) 7. Thyroid function test (hyperthyroidism) 8. Celiac Serology 9. Tumor Markers (eg: CEA) …… Depends on your differential diagnosis~ Stool • ( must be collected fresh on three occasions) – Microscopy for parasites and red and white cells ( warm specimen for amoebiasis) – Cultures: Pathogens, Campylobacter sp., C.difficile (pseudomembranous colitis, Yersinia, sp Stool – For occult blood – For ova and cyst (eg: Cryptosporidiosis, Blastocystis) – For fat excretion (steatorrhoea) Imaging and Scope: • • • • • Barium Studies: Barium enema, Barium follow-through Ultrasound Abdominal X-Ray (chronic pancreatitis) CT scan MRI Imaging and Scope: • Small Bowel Endoscopy (for malabsorption disorders) and Capsule Endoscopy • Colonoscopy/ Barium enema – To exclude malignancy and in colitis • Rigid / Flexible sigmoidoscopy – Biopsy of normal and abnormal looking mucosa Complications of Diarrhoea • • • • • • • Hypokalaemia Depletional hyponatraemia Hypernatraemia Hypophosphataemia Hypomagnesemia Dehydration Hypovolaemic shock Principles of Management of Acute Diarrhoea Acute Diarrhoea : Management • • • • Access Hydration Status Encourage fluids intake Consider antibiotics if ill or frail Consider referring if very ill, diabetic on insulin or metformin • Symptomatic relief with antimotility drugs • Advice on how to reduce spread by hand washing. • Food-handlers and staff in health care services should be symptom free for 48 hours before return. • Drink glucose containing liquids and soups • Carbohydrates e.g. pasta and bread, assist the co-transport of glucose and sodium, so the amount of diarrhoea lost will be less than if water is used alone Particular care should be taken when dealing with the following patients: • The very young or elderly • Those with co-morbidity e.g.diabetes, immunodeficiency, inflammatory bowel disorder or gastric hypochlorhydria • Patients taking systemic corticosteroids, ACE-inhibitors, diuretics or acid suppressants • Antibiotic therapy is usually only indicated for patients with positive stool cultures, who are systemically unwell and whose condition fails to improve within a few days. Dehydration: Management • Children and Elderly are especially prone to dehydration. • A child should be encouraged by their preferred diet. • Breastfeeding should be continued and alternate with ORS Oral Rehydration Therapy • The use of Oral Rehydration Therapy (ORT) is advisable for all cases with dehydration seen. – Oral Rehydration Salt –standard or reduced osmolarity – Home solutions Oral Rehydration Therapy – Sodium chloride 3.5 g – Trisodium citrate dehydrate 2.9 g (or sodium bicarbonate 2.5g) – Potassium chloride 1.5g – Glucose 20 g – To be dissolved in one litre of clean drinking water – encourage fluid intake e.g. salt + glucose drink to assist in co-transport of sodium into the epithelial cells via the SGLT1 protein, which enhances water and sodium re-absorption in small intestines. • Adults should receive 2 litres of ORT in the first 24 hours, followed by unrestricted normal fluids with 200 ml of ORT for every loose stool or vomit. • Mild dehydration (<5%) can be treated in a primary care, by giving ORS. • Moderate (5-10%) or severe (greater than 10%)dehydration is an indication for admission. Fluid management of Moderate to Severe Dehydration Treat Shock Rehydrate Maintainance Ongoing Losses • Treat Shock: 20 ml /kg 0.9% saline over 10 to 15 mins • Rehydration fluid deficit: % of dehydration X body weight 0.45% saline/2.5 % dextrose over 24 hours-low or normal plasma sodium over 48 hours-high plasma sodium • Maintenance : First 10 kg Second 10 kg Subsequent kg : 100 ml/kg/24 hours : 50 ml/kg/24 hours : 20 ml/kg/24 hours • Close monitoring : clinical condition (vomiting, diarrhoea), plasma creatinine, and electrolytes. Principles of Management of Chronic Diarrhoea 1. Rehydration • Oral rehydration therapy – Oral Rehydration Salt –standard or reduced osmolarity – Home solutions • Intravenous therapy – Ringer’s Lactate solution (Hartmann’s soln) – Normal saline/ Half normal saline with 5-10% glucose – Half strength Darrow’s soln 2. Stop diarrhoea • Anti-motility agents: Codeine, Loperamide, Diphenoxylate, Bismuth subsalicylate • Adsorbents: Zaldaride Maleate • Anti-spasmodic agents: Propantheline, Dicyclomine, Mebeverine • Antibiotics? Cholera, Dysentery, Giardiasis 3. Treat the underlying cause 4. Symptomatic Management • • • • Blood transfusion Analgesics Rehydration and electrolyte replacement Diet modification (malabsorption disorders) Treat accordingly~ References • Harrison’s Principal of Internal Medicine.2005, pg 225-233 • Kumar and Clark, • Rehydration Project • http://rehydrate.org/diarrhoea/tmsdd/1med .htm#intro • Kochar’s Clinical Medicine for Students, Fifth edition.pg41-47 • Murtagh’s Family Practicespg467-483 References • http://www.patient.co.uk/showdoc/4002502 0/ • Emedicinehealth.Dehydration • Medication Induced Constipation and Diarrhea; May 2008 issue; Practical Gastroenterology • Medication Induced Constipation and Diarrhea; May 2008 issue; Practical Gastroenterology