* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Basal and Stimulated Sympathetic Responses After Epinephrine No
Survey
Document related concepts
Transcript
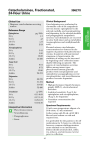
Basal and Stimulated Sympathetic Responses After Epinephrine No Evidence of Augmented Responses C. Michael Stein, Huai B. He, Alastair J.J. Wood Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Abstract—Delayed facilitation of norepinephrine release through the action of epinephrine (NE) at presynaptic b-adrenoceptors has been postulated to account for the delayed hemodynamic effects of epinephrine and to be a mechanism causally related to the development of hypertension. To determine whether a short-term increase in epinephrine concentrations resulted in subsequent facilitation of sympathetic responses, 9 healthy subjects (age, 2160.9 years) were studied at rest and during physiological stress on 2 occasions when they received an infusion of either saline or epinephrine (20 ng/kg per minute) in random order. Heart rate, blood pressure, forearm blood flow, epinephrine concentrations, and NE spillover were measured at rest, during mental stress (Stroop test), and during a cold pressor test. Measurements were performed before, during the 1-hour infusion of epinephrine or placebo, and 1 hour after the infusion. A radioisotope dilution method was used to measure NE spillover. Hemodynamic measurements and NE spillover were increased during the infusion of epinephrine, but 1 hour after discontinuation of epinephrine there was no significant augmentation of hemodynamic or sympathetic responses. NE spillover 1 hour after saline or epinephrine infusion was similar (0.8560.2 versus 0.8760.2 mg/min; P50.92). In addition, there was no delayed facilitation of stress-induced hemodynamic or NE responses after epinephrine. These findings do not support the hypothesis that epinephrine results in delayed facilitation of NE release. (Hypertension. 1998;32:1016-1021.) Key Words: epinephrine n norepinephrine n sympathetic nervous system n stress I t has been suggested that epinephrine plays a role in the pathogenesis of hypertension.1– 4 According to the “epinephrine hypothesis” of hypertension, epinephrine, released from the adrenal medulla during physiological stress, is taken up into sympathetic nerve terminals and later rereleased with norepinephrine (NE) as a cotransmitter. The epinephrine that has been rereleased stimulates further NE release through its action on presynaptic b-adrenergic receptors and in this way amplifies and prolongs sympathetic responses.1,4,5 Therefore, a brief increase in epinephrine concentrations, such as occurs in response to stress, could, through the mechanisms of uptake, rerelease, and stimulation of NE release, amplify and prolong sympathetic responses and facilitate the development of hypertension.1,3,4 Experimental evidence supports the existence of functional presynaptic b-adrenergic receptors as well as the process of uptake and rerelease of epinephrine in the nerve terminal5–10: mechanisms that would allow epinephrine to produce a delayed and sustained facilitatory effect on NE release. Support for the physiological relevance of these mechanisms comes from studies that have demonstrated that short-term, systemic infusion of epinephrine resulted in prolonged tachycardic and/or pressor responses11–14 and that low doses of epinephrine infused directly into the brachial artery augmented vasoconstrictor responses to stimuli that cause release of endogenous NE.15,16 However, while in vitro data support the existence of the individual mechanisms that underlie the epinephrine hypothesis, and while the hemodynamic studies suggest that responses after short-term exposure to epinephrine may be prolonged, there is little evidence to support the proposed underlying mechanism, namely, that a short-term increase in epinephrine concentrations is associated with a prolonged increase in NE release. Recently, using a technique that allowed the intrabrachial artery infusion of epinephrine in doses without detectable systemic effects,17 we did not observe a delayed facilitatory effect of epinephrine on local forearm NE spillover. However, an intriguing and unexplained observation in that study was that systemic NE spillover was higher after the epinephrine infusion. Those data, together with the increased plasma NE concentrations observed by others after systemic epinephrine infusion,1 therefore suggested that epinephrine might enhance NE spillover in vascular beds other than the forearm. The present study set out to examine that hypothesis and determine whether systemic administration of epinephrine, in a dose chosen to reproduce epinephrine concentrations similar to those achieved during physiological stress, was associated with a prolonged increase in systemic NE spillover, both at rest Received August 6, 1998; first decision August 18, 1998; revision accepted August 20, 1998. From the Division of Clinical Pharmacology, Vanderbilt University School of Medicine, Nashville, Tenn. Correspondence to Dr C. Michael Stein, Division of Clinical Pharmacology, Vanderbilt University School of Medicine, Medical Research Building 1, Room 560, Nashville, TN 37232-6602. E-mail [email protected] © 1998 American Heart Association, Inc. Hypertension is available at http://www.hypertensionaha.org 1016 Stein et al and during adrenergic stimulation resulting from mental stress (Stroop test) and nociception (cold pressor test). Methods Subjects Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Nine healthy, normotensive, nonsmoking, white male volunteers (age, 2160.9 years) were studied. All subjects provided written informed consent, and the study protocol was approved by the Vanderbilt Committee for the Protection of Human Subjects. No subject had clinically significant abnormalities on history, physical examination, or routine laboratory tests, including complete blood count, renal and liver function tests, and ECG. Subjects did not take any medications for $2 weeks before the study and were maintained on a diet, provided by the metabolic kitchen of the Vanderbilt Clinical Research Center, that was free of caffeine and alcohol and provided 150 mmol Na1 and 70 mmol K1 per day for 4 days before the study. An additional 2 subjects only completed 1 study day, and their data have not been included. One subject was withdrawn because frequent ventricular ectopic beats were noted during the placebo study day, and in 1 subject an unrelated illness occurred between the first and second study days. None of the subjects participated in our previous study of forearm NE responses to epinephrine.17 Subjects within a narrow age range were studied to minimize the potential confounding effects of age on NE spillover.18 Experimental Protocol Subjects were studied twice and received an infusion of either epinephrine or placebo (saline) in a single-blind fashion on the 2 study days, with the order of administration randomized. Identical procedures were followed on each study day, and the 2 study days were separated by 2 to 4 weeks. Subjects were admitted overnight to the Vanderbilt University Clinical Research Center on the evening of the fourth day of the controlled diet to minimize the effects of environmental factors on autonomic responses. All experiments were performed in the morning in the same temperature-controlled room with subjects resting supine in bed. Subjects fasted from midnight and remained fasting throughout the study. An intravenous cannula was placed in the antecubital fossa of each arm between 5 and 6 AM of the study day. Subjects rested quietly for 60 minutes after the placement of the intravenous catheters. Then [3H]NE (norepinephrine levo-[ring-2,5,6-3H], 56.9 Ci/mmol; New England Nuclear) was infused intravenously into the left arm for determination of NE kinetics (as described below). Forty minutes after the [3H]NE infusion was started, baseline resting heart rate, blood pressure, and forearm blood flow were measured, and blood was drawn for determination of renin and epinephrine concentrations and NE kinetics. Subjects then performed the Stroop test19 as described below. After a 10-minute rest period to allow a return to baseline, a cold pressor test was performed. These 3 data time points are referred to as before epinephrine or placebo resting, Stroop, and cold pressor, respectively. After an additional 10-minute rest period, an intravenous infusion of epinephrine (20 ng/kg per minute) or placebo (saline) was started. To avoid sudden systemic effects that might have been noticed by the subjects, the epinephrine infusion was administered at an initial dose of 67 ng/min and approximately doubled every 2 minutes so that the target dose of 20 ng/kg per minute was reached over 10 minutes. This dose of epinephrine was then continued for the next 50 minutes. Identical procedures were followed on the placebo day, with the infusion rate of saline doubled every 2 minutes, as was done for epinephrine, until the target rate was reached. Resting hemodynamic and catecholamine measurements were obtained 40 minutes after commencement of the epinephrine or saline infusion. Then, while the epinephrine or saline infusion continued, the Stroop test was repeated, and after a 10-minute rest period the cold pressor test was repeated. These 3 data time points are referred to as during epinephrine or placebo resting, Stroop, and cold pressor, respectively. The epinephrine or saline infusion was then discontinued, and 60 minutes were allowed to elapse before we obtained after epinephrine or placebo resting, December 1998 1017 Stroop, and cold pressor blood samples and hemodynamic measurements. Measurement of Heart Rate and Blood Pressure Heart rate was recorded from a continuous ECG monitor and calculated as the average of the heart rate obtained over 1 minute during the first minute of the Stroop test and during the second minute of the cold pressor test. Blood pressure was recorded with a semiautomated device (Dinamap, Critikon). Stressor blood pressures were measured 40 seconds after the Stroop test was started and after 1 minute of the cold pressor test. Resting blood pressure and heart rate were obtained from the average of 2 readings obtained within 1 minute of each other. Changes in systolic and diastolic blood pressure were similar, and blood pressure data are presented as mean arterial pressure. Measurement of Forearm Blood Flow Forearm blood flow was measured in the left arm with mercury-inSilastic strain gauge plethysmography,20 as we have previously described.9 The average of the flow determinations obtained during the first minute of the Stroop test and the second minute of the cold pressor test was determined and used for calculations. Stroop and Cold Pressor Tests The Stroop test consists of word stimuli that are presented on a computer monitor placed in front of the subject at 2-second intervals. The words (eg, red, yellow) are presented in varying colors. If the word is presented in black type, the word is read; however, if the word is in type of another color, the color must be stated rather than the word read. In addition, monaural headphones are placed over the subject’s ears and used to carry prerecorded, randomly ordered repetitions of the word stimuli to create competing task interference. Subjects provide responses aloud during 2-minute task intervals. Blood was drawn for catecholamine determinations over the second minute of the test. The cold pressor test was performed by immersing the subjects’ left foot for 2 minutes to the level of the lateral malleolus in a slurry composed of equal parts water and crushed ice. Subjects were instructed to breathe normally and to avoid straining or performing a Valsalva maneuver. Blood pressure was measured after 1 minute of the cold pressor test. Forearm blood flow measurement, determination of heart rate, and drawing of blood for catecholamines were performed during the second minute of the cold pressor test. Determination of Norepinephrine Kinetics [3H]NE (norepinephrine levo-[ring-2,5,6-3H], 56.9 Ci/mmol; New England Nuclear) was prepared for human administration by the Vanderbilt Hospital Radiopharmacy, and appropriate sterility and pyrogen testing was performed. Immediately before use, [3H]NE was diluted to a concentration of 1.5 mCi/mL in normal saline, with ascorbic acid 1 mg/mL added to the infusion solution. An initial loading dose of [3H]NE 19 mCi was administered over 2 minutes, followed by a constant infusion of 0.75 mCi/min. Baseline samples were obtained after 30 and 40 minutes, by which time [3H] NE concentrations achieve steady state,9 and at the time points described in the experimental protocol. Samples were drawn into cooled tubes with EGTA and reduced glutathione (Amersham Corporation), placed on ice, and centrifuged at 4°C. Endogenous and [3H]NE concentrations were measured to allow determination of NE kinetics, as we9 and others18,21 have previously described. We measured NE and epinephrine concentrations by high-performance liquid chromatography using electrochemical detection with 3,4-dihydroxybenzylamine as the internal standard, as we have described previously.22 We performed calculations for the determination of NE kinetics using the isotope dilution method,18,21 as we have previously described.9 Data Analysis Data, expressed as mean6SEM, were analyzed by repeatedmeasures ANOVA, comparing responses obtained before infusion, 1018 Epinephrine and Sympathetic Response TABLE 1. Measurements Before Epinephrine or Placebo Infusion Intervention Measurement Statistical Significance Resting Stroop Test Cold Pressor Drug Intervention Drug3Intervention Before placebo 58.863.1 68.463.2 78.964.5 0.5 ,0.001 0.6 Before epinephrine 58.062.3 69.861.9 81.264.6 Before placebo 79.164.1 86.065.8 103.9610.2 0.3 ,0.001 0.4 Before epinephrine 79.564.2 87.066.4 107.7613.8 Before placebo 44.165.2 34.464.7 36.866.4 0.3 0.001 1.0 Before epinephrine 52.966.2 41.167.7 43.7611.9 Before placebo 151.2619.1 148.5624.6 242.4645.1 0.7 0.02 0.5 Before epinephrine 166.6630.5 149.9622.0 214.5627.6 Before placebo 17.862.8 19.763.6 52.8617.7 0.9 0.03 0.95 Before epinephrine 17.462.5 18.961.8 56.3614.9 Before placebo 0.7160.09 0.9060.1 0.7 0.003 0.4 Before epinephrine 0.7960.30 Heart rate, bpm Mean arterial presure, mm Hg Forearm vascular resistance, mm Hg z mL21 z 100 mL21 z min Norepinephrine, pg/mL Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Epinephrine, pg/mL Norepinephrine spillover, mg/min 1.060.25 2.060.31 1.5560.27 Data are expresssed as mean6SEM. Statistical significance comparing responses regarding Drug (epinephrine or placebo), Intervention (resting, Stroop test, and cold pressor test), and the Drug3Intervention interaction is shown. Conversion factor: To convert norepinephrine concentrations from picograms per milliliter to nanomoles per liter, divide by 169.2. during infusion, and after infusion on the placebo and epinephrine study days. The effects of drug (epinephrine or placebo), intervention (resting, Stroop test, cold pressor test), and the drug3intervention interaction were determined. Post hoc analysis, if indicated, was performed with a 2-tailed Student’s t test for paired data if the data were normally distributed or, for data that were not normally distributed, with the Wilcoxon matched pairs signed rank test, as appropriate (SPSS for Windows, Release 6). A 2-tailed P value of ,0.05 was the minimum level accepted for statistical significance. Results Hemodynamic and catecholamine values before the administration of either epinephrine or placebo were similar on the 2 study days, both at rest and after adrenergic stimulation (Table 1) (Figure). The application of stressors (Stroop test and cold pressor test) resulted in significant stimulation of heart rate, mean arterial blood pressure, forearm vascular resistance, NE, epinephrine, and NE spillover (Table 1). The cold pressor test increased heart rate by '20 bpm, increased systolic and diastolic blood pressure by '30 mm Hg and 20 mm Hg, respectively, and doubled NE spillover. The responses to the Stroop test were more modest. The drug3intervention interaction was not significant for any variable, indicating a similarity of resting and stimulated responses before the infusion of epinephrine or placebo on the 2 study days (Table 1). Epinephrine infusion increased plasma epinephrine concentrations 10-fold from 19.363.1 to 217.8618.1 pg/mL (P,0.001), and this resulted in significant increases in resting heart rate (57.863.3 compared with 68.462.6 bpm; P50.004), resting forearm blood flow (1.960.2 compared with 2.760.4 mL/100 mL per minute; P50.05), and resting NE spillover (0.6960.07 compared with 1.460.30 mg/min; P50.02, Wilcoxon signed rank test). As was observed before infusion of epinephrine or placebo, the interventions used for adrenergic stimulation (Stroop test and cold pressor test) had statistically significant effects on all the parameters measured (data not shown). The absolute values of several measurements obtained during stress (eg, systolic blood pressure during the Stroop test) were significantly greater during epinephrine (127.262.8 mm Hg) than during placebo (116.961.3 mm Hg) (P50.009) infusion. However, other than plasma NE concentration (P50.04), the drug3 intervention interaction was not significant for any measurement, indicating that differences in resting values due to the epinephrine infusion accounted for the apparent increased hemodynamic responses to stress during the epinephrine infusion. One hour after the saline or epinephrine infusion was discontinued, the plasma concentrations of epinephrine were similar (26.463.4 compared with 30.266.5 pg/mL; P50.58) (Table 2). The preceding epinephrine infusion had effects that were of borderline statistical significance on heart rate (drug effect P50.10, ANOVA). Thus, resting heart rate was significantly higher 1 hour after epinephrine infusion (66.163.0 compared with 60.462.2 bpm; P50.01), but heart rate responses during Stroop or cold pressor testing were not different (Table 2). There was no evidence of a delayed stimulatory effect of epinephrine on NE spillover either at rest (0.8560.2 compared with 0.8760.2 mg/min; P50.92) or after stimulation by stress (Table 2) (Figure). Stein et al Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Norepinephrine spillover at rest and after adrenergic stimulation by Stroop test and cold pressor test before, during, and after saline or epinephrine infusion. Discussion We found no evidence to support the hypothesis that the systemic administration of epinephrine resulted in a delayed, facilitatory effect on NE release, either at rest or after the application of physiological stressors. Several previous studies have found that a short-term infusion of epinephrine was followed by sustained increase in heart rate and/or increase in blood pressure.11–13 These observations could not be accounted for by circulating levels of December 1998 1019 epinephrine since epinephrine has a half-life of ,1 minute23 and plasma concentrations of epinephrine return to baseline within minutes after the discontinuation of a systemic infusion.13 In addition, several studies have shown that a delayed, amplified blood pressure response to sympathetic stimulation occurred hours after the discontinuation of a systemic infusion of epinephrine.13,24 However, few studies have directly examined whether epinephrine does in fact cause a sustained increase in sympathetic activity and NE release, the proposed mechanism for the prolonged physiological responses. Several earlier studies have found that plasma NE concentrations remained elevated after an epinephrine infusion.1,12 However, plasma NE concentrations are determined not only by the amount released into plasma but also by the amount of NE cleared from plasma. Thus, systemic interventions that alter physiological responses may alter not only NE release but also NE clearance. The radioisotope dilution technique, which takes account of the clearance of NE and thus allows the determination of NE spillover, a measure of neuronal NE release, is sensitive to pharmacological and physiological changes and has been used extensively9,10,18,21,25 as a model to examine changes in neuronal NE release in vivo. Using NE spillover methodology, Persson and colleagues26 found that both muscle sympathetic nerve activity and NE spillover were increased 30 minutes after systemic infusion of epinephrine (100 ng/kg per minute), while Esler and colleagues27 found no increase after infusion of epinephrine (40 ng/kg per minute). The present study has several advantages. First, the dose of epinephrine infused, 20 ng/kg per minute, has previously been reported to result in a delayed increase in hemodynamic and plasma NE measurements12 and, while resulting in epinephrine concentrations similar to those achieved during physiological stress, avoids the confounding effect that large hemodynamic changes would have on subsequent measurements. Second, hemodynamic and NE responses were measured 1 hour rather than 30 minutes after the epinephrine infusion. We have previously noted that the increase in forearm blood flow after the administration of intra-arterial isoproterenol, a b-adrenergic agonist, is prolonged for up to 30 minutes after discontinuation of the infusion.28 Thus, a longer washout period of 60 minutes allowed time for any confounding effects resulting from reflex cardiovascular responses to return to baseline. Third, the placebo control allowed any potential confounding temporal effects to be factored out. Our findings, and those of Persson and colleagues,26 are compatible with a temporary reflex overshoot in sympathetic response present 30 minutes, but not 60 minutes, after the discontinuation of the vasodilator. Recently, such a sympathetic overshoot has been shown to occur after a systemic epinephrine infusion of '40 ng/kg per minute and to return to baseline within '20 minutes.27 The significance of minor changes in NE spillover would be uncertain, and it is likely that the effects of epinephrine on NE release would be substantial, if indeed this was a physiologically relevant mechanism. Persson and colleagues26 found that NE spillover was doubled 30 minutes after discontinuation of epinephrine. Our study had 93% power to detect such a doubling of NE spillover after epinephrine, and we can thus confidently exclude the possi- 1020 Epinephrine and Sympathetic Response TABLE 2. Measurements 1 Hour After Epinephrine or Placebo Intervention Measurement Statistical Significance Resting Stroop Test Cold Pressor Drug Intervention Drug3Intervention After placebo 60.462.2 69.762.6 80.064.9 0.09 0.003 0.25 After epinephrine 66.163.0 72.961.9 78.764.0 After placebo 79.265.0 81.066.3 104.7614.1 0.56 0.001 0.41 After epinephrine 80.664.8 84.666.9 103.4611.1 After placebo 50.967.0 39.267.5 41.268.3 0.10 0.03 0.91 After epinephrine 68.9611.9 52.6612.0 55.3612.2 After placebo 164.2627.8 166.8626.5 223.7636.6 0.44 0.01 0.19 After epinephrine 168.5624.7 155.7621.8 206.1630.7 After placebo 26.463.4 24.563.5 59.5613.3 0.54 0.04 0.2 After epinephrine 30.266.5 31.965.1 57.768.9 After placebo 0.8560.2 0.9860.2 1.360.2 0.41 0.004 0.26 After epinephrine 0.8760.2 1.360.3 1.560.3 Heart rate, bpm Mean arterial presure, mm Hg Forearm vascular resistance, mm Hg z mL21 z 100 mL21 z min Norepinephrine, pg/mL Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Epinephrine, pg/mL Norepinephrine spillover, mg/min Data are expresssed as mean6SEM. Statistical significance comparing responses regarding Drug (epinephrine or placebo), Intervention (resting, Stroop test, and cold pressor test), and the Drug3Intervention interaction is shown. Conversion factor: To convert norepinephrine concentrations from picograms per milliliter to nanomoles per liter, divide by 169.2. bility that changes in NE spillover likely to be of physiological significance occur. The epinephrine hypothesis will be validated or refuted by cumulative evidence provided by studies, such as the present one, that bring increasingly sophisticated techniques to bear on the question. The findings in the present study, our negative findings in the forearm,17 and a recent negative study from Esler and colleagues27 collectively provide strong evidence that delayed facilitation of NE release does not explain the delayed hemodynamic responses that have been observed after administration of epinephrine and thus do not support the epinephrine hypothesis of hypertension. Acknowledgments This study was supported by a Grant-in-Aid from the American Heart Association and by US Public Health Service grants HL 56251 and GM 5 M01-RR00095. Dr Stein is the recipient of a Pharmaceutical Manufacturers of America faculty development award in clinical pharmacology. References 1. Floras JS. Epinephrine and the genesis of hypertension. Hypertension. 1992;19:1–18. 2. Brown MJ, Dollery CT. Adrenaline and hypertension. Clin Exp Hypertens Pt A Theory Pract. 1984;6:539 –549. 3. Brown MJ, Macquin I. Is adrenaline the cause of essential hypertension? Lancet. 1981;2:1079 –1082. 4. Rand MJ, Majewski H. Adrenaline mediates a positive feedback loop in noradrenergic transmission: its possible role in development of hypertension. Clin Exp Hypertens Pt A Theory Pract. 1984;6:347–370. 5. Majewski H, Rand MJ, Tung LH. Activation of prejunctional betaadrenoceptors in rat atria by adrenaline applied exogenously or released as a co-transmitter. Br J Pharmacol. 1981;73:669 – 679. 6. Iversen LL. Role of transmitter uptake mechanisms in synaptic neurotransmission. Br J Pharmacol. 1971;41:571–591. 7. Langer SZ. Presynaptic regulation of the release of catecholamines. Pharmacol Rev. 1980;32:337–362. 8. Stjarne L, Brundin J. Beta2-adrenoceptors facilitating noradrenaline secretion from human vasoconstrictor nerves. Acta Physiol Scand. 1976;97:88–93. 9. Stein M, Deegan R, He H, Wood AJJ. Beta-adrenergic receptor-mediated release of norepinephrine in the human forearm. Clin Pharmacol Ther. 1993;54:58 – 64. 10. Chang PC, Grossman E, Kopin IJ, Goldstein DS. On the existence of functional beta-adrenoceptors on vascular sympathetic nerve endings in the human forearm. J Hypertens. 1994;12:681– 690. 11. Brown MJ, Brown DC, Murphy MB. Hypokalemia from beta2-receptor stimulation by circulating epinephrine. N Engl J Med. 1983;309: 1414 –1419. 12. Nezu M, Miura Y, Adachi M, Kimura S, Toriyabe S, Ishizuka, Ohashi H, Sugawara T, Takahashi M. The effects of epinephrine on norepinephrine release in essential hypertension. Hypertension. 1985;7:187–195. 13. Blankestijn PJ, Man in’t Veld AJ, Tulen J, van den Meiracker AH., Boomsma F, Moleman P, Ritsema van Eck HJ, Derkx FH, Mulder P, Lamberts SJ. Support for adrenaline-hypertension hypothesis: 18 hour pressor effect after 6 hours adrenaline infusion. Lancet. 1988;2:1386–1389. 14. Fellows IW, Bennett T, MacDonald IA. The effect of adrenaline upon cardiovascular and metabolic functions in man. Clin Sci. 1985;69: 215–222. 15. Floras JS, Aylward PE, Mark AL, Abboud FM. Adrenaline facilitates neurogenic vasoconstriction in borderline hypertensive subjects. J Hypertens. 1990;8:443– 448. 16. Floras JS, Aylward PE, Victor RG, Mark AL, Abboud FM. Epinephrine facilitates neurogenic vasoconstriction in humans. J Clin Invest. 1988;81: 1265–1274. 17. Stein CM, Nelson R, He HB, Wood M, Wood AJJ. Norepinephrine release in the human forearm: effects of epinephrine. Hypertension. 1997;30:1078 –1084. 18. Esler M, Jennings G, Korner P, Willett I, Dudley F, Hasking G, Anderson W, Lambert G. Assessment of human sympathetic nervous system activity from measurements of norepinephrine turnover. Hypertension. 1988;11:3–20. Stein et al 19. Fauvel JP, Bernard N, Laville M, Daoud S, Pozet N, Zech P. Reproducibility of the cardiovascular reactivity to a computerized version of the Stroop stress test in normotensive and hypertensive subjects. Clin Auton Res. 1996;6:219 –224. 20. Benjamin N, Calver A, Collier J, Robinson B, Vallance P, Webb D. Measuring forearm blood flow and interpreting the responses to drugs and mediators. Hypertension. 1995;25:918 –923. 21. Esler M, Jennings G, Korner P, Blombery P, Sacharias N, Leonard P. Measurement of total and organ-specific norepinephrine kinetics in humans. Am J Physiol. 1984;247:E21–E28. 22. He HB, Deegan RJ, Wood M, Wood AJJ. Optimization of high-performance liquid chromatographic assay for catecholamines: determination of optimal mobile phase composition and elimination of species-dependent differences in extraction recovery of 3,4-dihydroxybenzylamine. J Chromatogr. 1992;574:213–218. 23. Ferreira SH, Vane JR. Half-lives of peptides and amines in the circulation. Nature. 1967;215:1237–1240. December 1998 1021 24. Vincent HH, Boomsma F, Man in’t Veld AJ, Schalekamp MA. Stress levels of adrenaline amplify the blood pressure response to sympathetic stimulation. J Hypertens. 1986;4:255–260. 25. Lang CC, Stein CM, Brown RM, Deegan R, Nelson R, He HB, Wood M, Wood AJJ. Attenuation of isoproterenol-mediated vasodilatation in blacks. N Engl J Med. 1995;333:155–160. 26. Persson B, Andersson OK, Hjemdahl P, Wysocki M, Agerwall S, Wallin G. Adrenaline infusion in man increases muscle sympathetic nerve activity and noradrenaline overflow to plasma. J Hypertens. 1989;7: 747–756. 27. Thompson JM, Wallin BG, Lambert G, Jennings GL, Esler MD. Human muscle sympathetic activity and cardiac catecholamine spillover: no support for augmented sympathetic noradrenaline release by adrenaline co-transmission. Clin Sci. 1998;94:383–393. 28. Stein CM, Lang CC, Brown RM, Wood AJJ. Vasodilation in AfricanAmericans: attenuated nitric oxide mediated responses. Clin Pharmacol Ther. 1997;62:436 – 443. Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Basal and Stimulated Sympathetic Responses After Epinephrine: No Evidence of Augmented Responses C. Michael Stein, Huai B. He and Alastair J. J. Wood Downloaded from http://hyper.ahajournals.org/ by guest on May 4, 2017 Hypertension. 1998;32:1016-1021 doi: 10.1161/01.HYP.32.6.1016 Hypertension is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1998 American Heart Association, Inc. All rights reserved. Print ISSN: 0194-911X. Online ISSN: 1524-4563 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://hyper.ahajournals.org/content/32/6/1016 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Hypertension can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Hypertension is online at: http://hyper.ahajournals.org//subscriptions/