* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Care Transitions Case for Discussion - 36.5 KB
Heart failure wikipedia , lookup
Baker Heart and Diabetes Institute wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
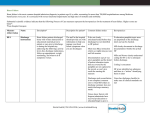
Case The following is a case meant to be used for discussion of transitional care issues in complex medical patients. June Bell is an 86 year old white woman with a complex past medical history (detailed below), who got her primary care in the Piedmont Healthcare system, and one night developed shortness of breath severe enough for her to call 911. Because she lived close to Emory University Hospital, the ambulance took her there out of concern for the time required to transport her to Piedmont Hospital. The information required to answer the questions below is available in the two discharge summaries. Questions for discussion: 1. Please comment on both discharge summaries regarding their completeness, utilizing the guide you have been provided. Direct your focus on data points which would have been most helpful for the primary care physician to take over her care. 2. What elements of management in the first discharge summary were predictive of a failed care transition, with readmission to the hospital? What could have been done differently? 3. Regarding discharge settings, what was problematic about discharging the patient back to her home in the first discharge summary? What are the potential advantages and disadvantages to discharging to a skilled nursing facility in the second scenario? Discharge Summary 1 ADMITTING DIAGNOSES: 1. Acute-on-chronic congestive heart failure with systolic dysfunction. 2. Urinary tract infection. DISCHARGE DIAGNOSES: 1. Acute-on-chronic congestive heart failure with systolic dysfunction. 2. Urinary tract infection. 3. Type 2 diabetes. 4. Hypertension. 5. Bladder cancer. 7. Gout. PROCEDURE: X-ray. Pulmonary edema. HISTORY OF PRESENT ILLNESS: An 86-year-old woman admitted to Emory University Hospital with three days of shortness of breath, cough, and orthopnea. She is usually seen in clinic at Piedmont Healthcare but the ambulance brought her here from her home because it was the closest hospital. In the ER was found to have O2 sats in the 80s on room air and was put on nasal cannula oxygen. The chest X-ray found pulmonary edema, and the patient was given Lasix 40 mg IV, which helped her with her symptoms considerably. She was then admitted to the medical floor for ongoing management of her congestive heart failure. PAST MEDICAL HISTORY: 1. Congestive heart failure with an ejection fraction of approximately 15 percent. 2. Moderate to severe tricuspid regurgitation. 3. Hypertension. 4. Type 2 diabetes. 5. Bladder cancer 6. Gout. 7. Mild dementia ADMISSION MEDICATIONS: 1. Lasix 40 mg once a day 2. Aspirin 325 mg po daily 3. Allopurinol 100 mg po daily 4. Donepezil 10 mg po daily 5. Calcium with Vitamin D, one tab daily 6. Lexapro 10 mg po daily 7. Metformin 500 mg po bid 8. Lisinopril 10 mg po qday ALLERGIES: No known drug allergies. PHYSICAL EXAMINATION: VITAL SIGNS: Blood pressure 142/69, pulse 79, respiratory rate of 18. Pulse ox 94 percent on 2 liters O2. HEENT/Neck: Positive JVD CORONARY: S1 and S2, regular rate and rhythm. LUNGS: Clear to auscultation bilaterally. ABDOMEN: Good bowel sounds, soft, nontender, nondistended. SKIN: Stage I decubitus in the sacral area. NEUROLOGIC: Grossly nonfocal. The patient was alert, and oriented x1. ADMITTING LABORATORY: Sodium 141, potassium 4.4, chloride 110, bicarb 22, BUN 27, creatinine 1.1, glucose of 65. WBC 4.2, hemoglobin 11, hematocrit 34, platelets 289. CK of 72, troponin 0.13, BNP of 1885, alk phos 193, ALT 25, AST 26. HOSPITAL COURSE: 1. Acute-on-chronic congestive heart failure with systolic dysfunction. The patient initially was started on Lasix 40 mg IV q.12 h. This was subsequently increased to 80 mg IV q.12 h. The patient diuresed well. 2. Urinary tract infection. She was given Levaquin for an E.coli UTI. 3. Delirium: Initially after admission, Ms. Bell became quite confused with fluctuating mental status, but this improved after diuresis, and by the time before discharge, her daughter did say that she was getting close to her baseline mental status. 4. Type 2 diabetes. She came in on metformin but due to her age was switched to Lantus insulin, which she tolerated well during her hospital stay. 5. Functional status: The patient did start seeing physical and occupational therapy during her stay. By the time of discharge was able to walk about 50 feet with no help, though she did get somewhat short of breath with longer distances. CONDITION ON DISCHARGE: She was discharged hemodynamically stable. DIET: A 2-g sodium diet ACTIVITY: She is to progress as tolerated. DISCHARGE PLAN: The patient lives alone, so she will leave with home health services including physical/occupational therapy and a homemaker. Her daughter plans to check in on her once daily MEDICATIONS ON DISCHARGE: 1. Lasix 40 mg twice a day 2. Aspirin 81 mg po daily 3. Allopurinol 100 mg po daily 4. Donepezil 10 mg po daily 5. Calcium with Vitamin D, one tab daily 6. Lexapro 10 mg po daily 7. Lantus insulin 10 units SC QHS 8. Captopril 12.5 mg pot id 9. Norvasc 10 mg po q day 10. Isosorbide dinitrate 10 mg po bid Discharge Summary 2 ADMISSION DIAGNOSES: 1. Acute on chronic and systolic congestive heart failure exacerbation. BRIEF HISTORY: Ms. Bell is an 86-year-old white woman with past medical history of CHF, hypertension, type 2 diabetes, history of bladder, gout, who has been admitted to Emory University Hospital ten days ago with shortness of breath, having been found to be in CHF from CXR. Was diuresed successfully and patient improved. Then she was discharged to home a week later. One day prior to this admission, she again developed shortness of breath and anxiety. She came back to the Emory ER, where she was found to have pulmonary edema on chest X-ray and was given 40 mg IV lasix with improvement in her symptoms. Was admitted for further management of her congestive heart failure. PAST MEDICAL HISTORY: 1. Congestive heart failure with an ejection fraction of approximately 15 percent. 2. Moderate to severe tricuspid regurg. 3. Mild Dementia 4. Type 2 diabetes. 5. Bladder cancer 6. Gout. 7. Hypertension ALLERGIES: The patient does have no known drug allergies. MEDICATIONS ON ADMISSION: 1. Lasix 40 mg twice a day 2. Aspirin 81 mg po daily 3. Allopurinol 100 mg po daily 4. Donepezil 10 mg po daily 5. Calcium with Vitamin D, one tab daily 6. Lexapro 10 mg po daily 7. Lantus insulin 10 units SC QHS 8. Captopril 12.5 mg pot id 9. Norvasc 10 mg po q day 10. Isosorbide dinitrate 10 mg po bid PHYSICAL EXAMINATION: VITAL SIGNS: Blood pressure on admission was 130/89, pulse of 89, respirations 18, temperature 36.1. GENERAL: The patient was alert. HEENT: Normocephalic, atraumatic. CARDIOVASCULAR: S1, S2. Regular rate and rhythm. RESPIRATORY: Bibasilar crackles to auscultation GI: Positive bowel sounds. Soft, nontender, nondistended. MUSCULOSKELETAL: With 1+ pitting edema. NEUROLOGICAL: Grossly nonfocal. GU: The patient did have Foley. ADMITTING LABORATORY STUDIES: Sodium 143, potassium 4.8, chloride 110, bicarb 22, BUN 35, creatinine 1.2, glucose of 80. WBC 4.2, hemoglobin 11, hematocrit 34, platelets 289. CK of 72, troponin 0.03, BNP of 2190, alk phos 193, ALT 25, AST 26. HOSPITAL COURSE: The patient was admitted with CHF exacerbation. She was started on Lasix 40 b.i.d. IV. In terms of her diabetes, Accu-Chek was ordered. She was continued on Lantus and she was also continued on norvasc but changed from captopril to lisinopril for high blood pressure. The patient did have cardiac enzymes negative. A 2D echo was checked which revealed that the patient has 15 percent EF with severe systolic dysfunction. She was continued also on aspirin. The patient's hospital stay was noncomplicated. BNP was repeated and went down from 2190 to 1174. No event on tele. The patient was discharged to Budd Terrace Subacute Rehab for rehabilitation five days after admission. DISCHARGE MEDICATIONS: Include: 1. Furosemide 40 mg twice a day 2. Allopurinol 100 mg po daily 3. Aspirin 81 mg po daily 4. Isosorbide dinitrate 10 mg po bid 5. Calcium with Vitamin D, one tab daily 6. Norvasc 10 mg po q day 7. Lantus insulin 10 units SC QHS 8. Captopril 12.5 mg pot id 9. Lexapro 10 mg po daily 10. Donepezil 10 mg po daily Discharge plan: The plan was discussed with the patient and her daughter and it was thought that due to the patient’s functional deficits, she would be transferred to the Budd Terrace nursing facility’s subacute rehab unit with the goal of eventual transfer to home.