* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Upper and Lower Respiratory Tract Infections
Survey
Document related concepts
Transcript
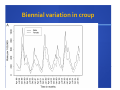
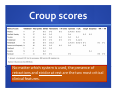
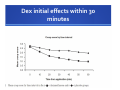
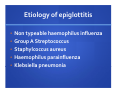
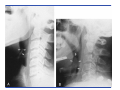
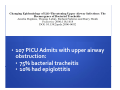
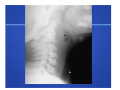
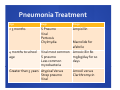
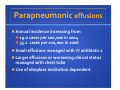
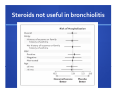
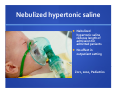
Upper and Lower Respiratory Tract Infections Dr. Shannon MacPhee IWK Emergency Department April 4, 2014 Declaration of Disclosure • I have no actual or potential conflict of interest in relation to this program. • I also assume responsibility for ensuring the scientific validity, objectivity, and completeness of the content of my presentation. Objectives Stridor Community acquired pneumonia Pathogenesis Clinical presentation and medical workup Treatment Complications: Pleural effusion Bronchiolitis Croup • 15% of all pediatric emergency visits in North America • Abrupt onset • Night • 8% admission rate Croup Laryngotracheobronchitis 6 months to 6 years Parainfluenza (75%) Hoarse voice, Inspiratory stridor, Barky cough Croup radiograph Biennial variation in croup Croup scores No matter which system is used, the presence of retractions and stridor at rest are the two most critical clinical features. Croup treatment Humidified air (not mist!) Dexamethasone Dose and population Budesonide not recommended $$$ Inhaled epinephrine Discharge after 1.5‐3 hours of observation in ER if completely stable Mild croup RCT O.6 mg/kg Follow up on Days 1,2,3,7,21 Detailed analysis of costs for the “payer” (ED visit, Physician billing, med cost) Cost for family (parking, lost work, ambulance service, lost productivity) Average societal cost of $92 versus $72 (Dex versus placeb0) Return visits reduced by more than 50% with dexamethasone arm Dex initial effects within 30 minutes Croup Disposition 1.5‐3 hours post epinephrine Disposition should take into account: • Diagnostic certainty • Severity of illness • Response to epinephrine • Presence of fever • Oral intake • Past medical conditions • Social factors Case 2 • 3 yo girl • Sore throat, difficulty swallowing, fever x 24 hours • Respiratory distress, stridor, drooling x 12 hours • T 40.2, HR 160, RR 52, Sats 91% Differential Diagnosis? 3 D’s of Epiglottitis • Drooling • Dysphagia • Distress Tibballs, 2011 Etiology of epiglottitis • Non typeable haemophilus influenza • Group A Streptococcus • Staphylcoccus aureus • Haemophilus parainfluenza • Klebsiella pneumonia Intensive Care Anesthesia ENT Treatment of epiglottitis • Airway control necessarily precedes diagnostic evaluation • IV Antibiotics (Cefuroxime and Vancomycin) • Diagnostic tests which may provoke anxiety, should be postponed until the airway is secure • 107 PICU Admits with upper airway obstruction: • 75% bacterial tracheitis • 10% had epiglottitis Bacterial tracheitis • Incidence: 0.1/100,000 children per year • Age group: < 6 years common • Pathophysiology: • Subglottic and tracheal inflammation, edema and purulent secretions with extension into bronchi commonly • S Aureus 50% Hopkins, 2006 Bacterial tracheitis: Clinical presentation Abrupt presentation URTI symptoms for 24 hours followed by an acute deterioriation with stridor and respiratory distress Cough common – and not painful Fever common but not universal ‐ more often low grade (<39) ?Tracheal tenderness True or False AP neck radiograph is helpful in distinguishing between croup and bacterial tracheitis. A.True B. False AP neck radiograph is helpful in distinguishing between croup and bacterial tracheitis. A. True B. False Treatment of Bacterial Tracheitis • Failed trial of inhaled epinephrine often a clue to diagnosis of bacterial tracheitis • Treatment: Ceftriaxone and Cloxacillin/Vancomycin • Steroids of no benefit • Airway management: 91% intubation rate Retropharyngeal abscess • Clinical presentation: • Fever, sore throat, difficulty swallowing • Etiology: Staph, strep, anaerobes, often polymicrobial • Only rarely presents as upper airway obstruction Please list three reasons for false positive interpretation of widening of the retropharyngeal space on plain film. 3 reasons for false positive interpretation of RPA on Lateral Neck Radiograph: 1.Neck held in flexed position 2.Film taken in expiration 3. Neck held in neutral position. Complications: Retropharyngeal abscess • Mediastinitis • Osteomyelitis • Sepsis • Airway obstruction • Internal jugular vein thrombosis • Carotid artery aneurysm Surgical adage: ”Never let the sun go down on un‐drained pus……” • Surgical drainage traditionally mainstay of therapy • Mild cases (as determined by extent of involvement on CT) successfully managed with IV therapy. • IV Cefotaxime and Clindamycin Pneumonia • Etiology • Clinical features • Indication for CXR • Disposition • Complications of pneumonia Community acquired pneumonia 1 in 20 children under 5 will develop pneumonia each year in developed countries • 30-40% of bacterial pneumonia is caused by S pneumo • More common in boys • Risk factors for severe disease: • Prematurity 24-28 weeks • < 5 years • Immunocompromised hosts Viral Etiology RSV (most common in those <2 years of age) Bocavirus Parainfluenza virus Influenza virus Metapneumoviruses Adenovirus (Onate 2008) Bacterial etiology Streptococcus pneumoniae mycoplasma pneumoniae chylamydia pneumoniae Staph aureus (MRSA) Bortdella pertussis (neonate) Clinical presentation • Fever • Cough • Difficulty breathing • Poor feeding or vomiting • Chest or abdominal pain • Abrupt onset of rigors favors S Pneumo • Significant, persistent cough M pneumoniae Clinical Presentation Tachypnea stressed by WHO as a marker of pneumonia when seen with fever or cough Age (years) Respiratory Rate <2 2‐12 >12 >60 >50 >40 • Radiological confirmation is encouraged whenever possible to support the clinical diagnosis and may be useful if the child subsequently deteriorates (Can Pediatric Society) When can you omit the Xray? Pediatric Emergency Care, 2012 Prospective study, 278 patients undergoing xray to r/o pneumonia Negative predictive value fever 95% Wheezing was negatively predictive of pneumonia on xray OR 0.56 (0.32-.98) • Rates of pneumonia: • All wheezers 4.9% • Afebrile wheezers 2% • Febrile wheezer 6.9% • Febrile, hypoxic wheezer 20.6% • Safely omit xray in afebrile wheezer. Occult pneumonia: Acad Emerg Med 2007 • 9% of children under age 5 with fever in the absence of tachypnea, hypoxemia, respiratory distress, or signs of LRTI will have pneumonia on xray • Clinical features that increase the likelihood of occult pneumonia are: • cough • fever for 5 days • fever >39C • WBC >20 000 Interpretation of CXR • Multiple studies that indicate radiographic appearance does not correlate with confirmed viral or bacterial etiology • Bettenay, Ped Radiology 1988 • Korppi Acta Peadiatric 2008 Pneumonia Treatment Age Bugs Drugs < 3 months S Pneumo Viral Pertussis Chylmydia Ampicillin Macrolide for afebrile 4 months to school Viral most common Amoxicillin 80 age S pneumo mg/kg/day for 10 Less common days mycobacteria Amoxil versus Greater than 5 years Atypical Versus Clarithromycin Strep pneumo Viral Putting a plug in for Amoxil 40% of circulating s pneumo strains in US are resistant to clarithromycin Amoxil is better tolerated and has better absorption than penicillin Only 70% of s pneumo isolates are susceptible to second and third generation cephaloporins! Giving amoxil 90mg/kg/day TID leads to 95% cure rate compared to 65% cure rate at same dose with BID dosing AMOXIL TID is the number one choice to treat CAP in kids Decision to Admit Moderate to severe respiratory distress: RR > 60 breaths/min for infants less than 2 months RR > 50 breaths/min for 2-12 months RR > 40 breaths/min for 1-5 years RR > 30 breaths/min for greater than 5 years Moderate/severe suprasternal, intercostal or subcostal retractions Grunting Nasal flaring Apnea Significant shortness of breath Cyanosis Altered mental status Hypoxemia (< 90% on room air) Not feeding in infants or signs of dehydration in older children Tachycardia Capillary refill > 2 seconds Treatment failure Repeat CXR to rule out effusion Add Macrolide Consider Clindamycin /Cloxacillin to cover for Staph Bishop N B et al. Pediatrics 2003;111:e188‐e190 ©2003 by American Academy of Pediatrics Pleural effusion Parapneumonic effusions Annual incidence increasing from 19.0 cases per 100,000 in 2004 35.2 cases per 100,000 in 2006 Small effusions managed with IV antibiotic s Larger effusions or worsening clinical status managed with chest tube Use of alteplase institution dependent BMC Infectious Disease. Empyema associated with community‐acquired pneumonia: A Pediatric Investigator's Collaborative Network on Infections in Canada (PICNIC) Langley et al. 2008. 8 Canadian pediatric centres, N=251 77% needed Oxygen supplementation 75% had chest tube placement 33% were admitted to an intensive care unit. use of chest tubes, thoracentesis and thorascopic lysis varied from center to center Final topic: Bronchiolitis Bronchiolitis most common acute infection of the lower respiratory tract in infants rhinorrhea, cough, wheezing, respiratory distress, and hypoxemia most often caused by respiratory syncytial virus Hospital admissions for bronchiolitis have doubled over the past 10 to 15 years US Annual hospital costs for RSV‐ associated bronchiolitis estimated up to $691 million in 1998 Hot topics in management Medications: Salbutamol Steroids, and if so dosing controversies Inhaled epinephrine Hypertonic saline nebulizations Chest radiograph Salbutamol/epi nebs : no effect in bronchiolitis Steroids not useful in bronchiolitis Steroids : no effect in bronchiolitis One exception: combination of inhaled epinephrine and Dexamethasone 1 mg/kg for five days lower rate of admission by 7 days CanBetter Authors not using this regime currently Nebulized hypertonic saline Nebulized hypertonic saline reduces length of admission for admitted patients No effect in outpatient setting Zorc, 2010, Pediatrics Risk factors for severe disease Prematurity Immunodeficiency Low birth weight Passive smoke Age less than three exposure Household crowing Native heritage months Chronic pulmonary diseae (CF, PCD) Congenital heart disease What are you going to do with your next baby with bronchiolitis? Summing it up… Careful discharge planning for the patient with croup…bacterial tracheitis low incidence but significant morbidity. Amoxil 80/kg/day TID First Line for typical pneumonia Parapneumonic effusions on the rise Supportive care only for bronchiolitics‐therapy only for those going to ICU