* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download urticaria
Survey
Document related concepts
Transcript
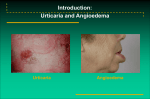
Urticaria Dr.Amirhossein Siadat Associated Professor Isfahan University of Medical Sciences DEFINITION Urticaria is defined as a skin lesion consisting of a wheal-and-flare reaction in which Iocalized intracutaneous edema (wheal) is surrounded by an area of redness (erythema) that is typically pruritic. Individual hives can last from as briefly as 30 minutes to as long as 36 hours. They can be as small as a millimeter or 6 to 8 inches in diameter (giant urticaria). They blanch with pressure as the dilated blood vessels are compressed, which also accounts for the central pallor of the wheal. PHOTO IMAGES OF HIVES Angioedemas : deeper dermal ,subcutaneus and sub mucosal tissues. They are usually painfull rather than itchy ,poorly defined and pale or normal in color ANGIOEDEMA Swelling of lips, face, hands, feet, penis or scrotum Facial swelling most prominent in periorbital area May be accompanied by swelling of the tongue or pharynx Urticaria is classified to acute and chronic with a time devision between 6w and 3m. When urticaria is present daily or almost daily for less than 6w it is acute. PREVALANCE: POINT PREVALANCE=0.1% Cumulative life time prevalance:0.05-23.6% in general population but a range of 1-5% is more realistic 72% ordinary urticaria,20%physical and choloinergic,3.4%allergic(exept stings and injected drug),2.1% u.vasculitis,0.5% hereditary angioedema CLINICAL FEATURES OF ACUTE OR CHRONIC URTICARIA: Ithcing erythematous macules develop into weals consisting of pale to pink edematous raised areas of skin often with a surrounding flare It occurs any where (scalp and palms),in any number and size, any shape even bulla. Wheals are often very itchy especially at night and resolve in a few hour without any residue. Patient always rub not scratch so excoriation is absent. Sometimes they bruise like in thigh. Wheals are more prominent at evening and premens In 50% of of urticaria: there may be angioedema. Angioedema color is like skin ,most frequently on the face but any other area such as ear ,genitalia,hand and feet It may last for several days, It is not always itchy and and may be painful Urticaria may be proceeded with vomiting. It may be associated with: malaise loss of concentration feeling hot or cold headache vomiting abdominal pain diarrhoea arthralgia dizziness scyncope And even anaphylaxies EM LIKE ERYTHEMA MULTIFORME 1) Central dusky purpuric area 2) Elevated edematous pale ring 3) Surrounding macular erythema DERMATITIS HERPETIFORMIS BULLOUS PEMPHIGOID INSECT BITE INSECT BITE PATHOPHYSIOLOGY Histamine: the most important mediator of urticaria. Histamine is produced and stored in mast cells. There are several mechanisms for histamine release via mast cell surface receptors. PHATHOPHYSIOLOGY: Urticaria is due to a local increase in permeability of capillaries of venules. It is due to activation of cutaneus mast cells that contain many mediators predominantly histamin. Pathophysiology of Urticaria Non-immunologic factors Immunologic factors Chemical histamine liberators eg. Opiates, polymyxin antibiotics, thiamine Types II and III complement activation Alternative complement pathway action Anaphylatoxins (C3a, C5a) Physical agents, e.g. cold, heat, sunlight Type I IgE mediated genetic factors modulating factors Cholinergic released mediators (particularly histamine) endogenous hormone vasodilating factors Small blood vessel vasodilation URTICARIA INFANTILE URTICARIA Food origin is important in the etiology of infantile urticaria. Food allergyfor 62% of patients drug etiology (22%) physical urticaria (8%) contact urticaria (8%). LAB TEST FOR ACUTE URTICARIA Antibiotics especially penicilin and cephalosporin are common causes. Risk factors: previous exposure reaction to a drug or chemically related drug intermittant and multiple drug therapy , familial predisposition CHRONIC URTICARIA HISTORY OF CHRONIC URTICARIA PHYSICAL EXAMINATION OF CHRONIC URTICARIA LAB FOR CHRONIC URTICARIA LAB FOR CHRONIC URTICARIA TREATMENT OF CHRONIC URTICARIA Antihistamines are the preferred initial treatment for urticaria and angioedema Cetirizine, loratadine, or fexofenadine are first-line agents and are given once daily Higher doses than suggested by the manufacturers may be required Patients with daytime and nighttime symptoms can be treated with combination therapy These patients can be treated with: a low-sedating antihistamine in the morning e.g., loratadine 10 mg, or fexofenadine 180 mg, or cetirizine 10 to 20 mg and a sedating antihistamine e.g., hydroxyzine 25 mg in the evening. Cetirizine can be mildly sedating Doxepin is an alternative bedtime medication especially effective for anxious or depressed patients. The initial dose is 10 to25 mg. Gradually increase the dose up to 75 mg for optimal control Some patients with chronic urticaria respond when an H2-receptor antagonist such as cimetidine is added to conventional antihistamines Side Effects Antihistamines are structurally similar to atropine; therefore they produce atropine-like peripheral and central anticholinergic effects : dry mouth, blurred vision, constipation, and dizziness. First-generation antihistamines (H1-receptor antagonists) such as chlorpheniramine, hydroxyzine, and diphenhydramine cross the blood-brain barrier and produce sedation. Antihistamines may produce stimulation in children, especially in those ages 6 through 12 H1 and H2 Antihistamines Cimetidine, ranitidine, and famotidine are H2 antagonists that are used primarily for the treatment of gastric hyperacidity. Approximately 85% of histamine receptors in the skin are the H1 subtype, and 15% are H2 receptors. It would seem that the combination of H1 and H2 antihistamines would provide optimal effects. The results of studies are conflicting but generally show that the combination is only slightly more effective than an H1-blocking agent used alone. First-Generation (Sedating) H1 Antihistamines .The first-generation H1 antihistamines are divided into five classes lipophilic, cross the blood-brain barrier, and cause sedation, weight gain, and atropine-like complications including dry mouth, blurred vision, constipation, and dysuria. Metabolism occurs via the hepatic cytochrome P-450 (CYP) system. In patients with liver disease, or in patients who are taking CYP 3A4 inhibitors such as erythromycin or ketoconazole, the plasma half-life may be prolonged. Antihistamines given during or after the onset of a hive are less effective. Second-Generation (Low-Sedating) H1 Antihistamines The second-generation antihistamines are not lipophilic and do not readily cross the blood-brain barrier They cause little sedation and little or no atropine-like activity Fexofenadine (Allegra) Fexofenadine in a single dose of 180 mg daily or 60 mg twice daily is the recommended dosage for treating urticaria Dosage adjustment is not necessary in the elderly or in patients with mild renal or hepatic impairment Fexofenadine may offer the best combination of effectiveness and safety of all of the low-sedating antihistamines Cetirizine (Zyrtec) Cetirizine is a metabolite of the first-generation H1antihistamine hydroxyzine The adult dose is 10 mg daily. A reduced dosage (5 mg daily) is recommended in patients with chronic renal or hepatic impairment. No drug interactions are reported, and there is no cardiotoxicity A dose higher than recommended may be required. Loratadine (Claritin) Loratadine is a long-acting second-generation H1-histamine antagonist A 10-mg dose suppresses whealing for up to 12 hours; suppression lasts longer after a larger dosage A reduced dosage may be required in patients with chronic liver or renal disease. There are no significant adverse drug interactions A special form of the medication, RediTabs (10 mg)rapidly disintegrates in the mouth A dose higher than recommended may be required. Desloratadine (Clarinex) Desloratadine is an active metabolite of loratadine A 5-mg dose each day is effective There is no evidence that it offers any advantage over loratadine Tricyclic Antihistamines (Doxepin) Tricyclic antidepressants are potent blockers of histamine H1 and H2 receptors. When taken in dosages between 10 and 25 mg three times a day doxepin is effective for the treatment of chronic idiopathic urticaria. Doxepin is a good alternative for patients with chronic urticaria not controlled with conventional antihistamines and for patients who suffer anxiety and depression associated with chronic urticaria Side effects: Lethargy Dry mouth and constipation Doxepin can interact with other drugs that are metabolized by the cytochrome P450 system (e.g., ketoconazole, itraconazole, erythromycin, clarithromycin) Epinephrine Severe urticaria angioedema requires epinephrine Epinephrine solutions have a rapid onset of effect but a short duration of action The dosage for adults is a 1:1000 solution (0.2 to 1.0 ml) given either subcutaneously or intramuscularly the initial dose is usually 0.3 ml Second-Line Agents Oral Corticosteroids Because of toxicity, corticosteroids are reserved for antihistamine failures or the most severe cases They are reliable and effective The patient receives 5 days each of 60 mg, 40 mg, and 20 mg Leukotriene Modifiers Leukotriene modifiers may provide improvement in some cases of antihistamine-resistant chronic urticaria Excellent safety, absence of required monitoring in the cases of montelukast and zafirlukast, and wide availability make leukotriene modifiers the preferred alternative agent Montelukast was demonstrated to be effective for patients with NSAIDexacerbated chronic urticaria. Patients with positive autologous serum skin test (ASST) results may predict better response to leukotriene modifiers Experience in physical urticarias has also been promising. Other second line Drugs: Dapsone, Cyclosporine, Mycophenolate Mofetil Third Line Treatments: IVIg, MTX (10 to 15 mg weekly) Topical Measure: Calamine Menthol Avoid factors that enhance pruritus Taking aspirin, drinking alcohol, or wearing tight elasticized apparel or coarse woolen fabrics PHYSICAL URTICARIAS 20% of all urticarias Dermatographism Cholinergic/Adrenergic Cold/Heat Solar Pressure Exercise induced Aquagenic Vibratory Angioedema Physical urticaria PHYSICAL URTICARIAS May occur so intermittently as to appear acute but typically are chronic entities – most idiopathic SYMPTOMATIC Symptomatic Dermatographism DERMATOGRAPHISM Simply scratching the skin promotes linear hives within minutes Delayed form described Typically is short-lived in duration (1/2 to 3 hours) and responds readily to antihistamines Cholinergic Urticaria CHOLINERGIC URTICARIA Cholinergic urticaria Goal of raising body temperature (oral) by 0.7oC Hot bath to 420C or having patient exercise Small pruritic papules result surrounded by erythema (but without hypotension) result Passive heat challenge may separate exerciseinduced anaphylaxis from cholinergic urticaria COLD-INDUCED URTICARIA Cold-induced urticaria Familial (autosomal dominant) vs acquired (usually infection associated) Acquired form positive ice-cube challenge Usually responds to cyproheptadine DIAGNOSIS OF COLD-INDUCED URTICARIA Cold Stimulation Time Test (CSTT) Positive in acquired cold-induced urticaria Ice cubes and water in a plastic bag applied to patient’s forearm up to 10 minutes Urticaria results after warming of area Timing of cold stimulus indirectly proportional to severity (less time needed, worse symptoms upon exposure to cold) Many patients with good history for coldinduced urticaria may have negative CSTT DELAYED PRESSURE URTICARIA DELAYED PRESSURE ANGIOEDEMA ~ 37% incidence of delayed pressure urticaria in chronic urticaria 15 pound weight suspended by thick strap over the shoulder and worn for 15 minutes Typically, erythema with induration and tenderness occurs at least 2 hours after the test VIBRATORY ANGIOEDEMA Vortex to induce angioedema in a patient with swelling of hands while driving car Lawlor F et al Br J Dermatol 1989; 120: 93-99 THE END ANGIOEDEMA HEREDITARY ANGIOEDEMA 2nd to 4th decade, + Family history, AD May occur q2 weeks, lasting 2 to 5 days Eyelid and lip involvement NOT SEEN. Face, hands, arms, legs, genitals buttocks, stomach, intestines, bladder affected. N/V, Colic, may mimic Appendicitis Triggers: minor trauma, surgery, sudden changes in temperature or sudden emotional stress Presence of urticaria rules out HA HEREDITARY ANGIOEDEMA aka Quincke’s Edema NO PRURITIS OR URTICARIA, + PAIN Low C4, C1, C1q, C2 levels Low or dysfunctional plasma C1 esterase inhibitor protein. 25% of deaths from laryngeal edema Tx of choice: fresh frozen plasma, stanazol, tranexamic acid TYPE I AND TYPE II HA Type I – LOW serum levels of NORMAL C1 esterase inhibitor protein Type II – NORMAL levels of DYSFUNCTIONAL C1 esterase inhibitor protein. C4 best screening test, it will be low in both of the above cases. HA - TREATMENT 25% of deaths due to HA are the result of laryngeal edema TOC for acute HA is fresh frozen plasma Stanazol useful for short-term prophylaxis in patients undergoing dental surgery, endoscopic surgery or intubation. Tranexamic acid in low doses has few side effects and useful for acute or chronic HA. ACQUIRED ANGIOEDEMA Symptoms same as HA, but NO family hx. Aka Caldwell’s Syndrome Occurs at night, pt wakes up with it. Acute evanescent circumscribed edema Affects most distensible tissues: eyelids, lips, earlobes, genitalia, mouth, tongue, larynx. Swelling is subcutaneous, not dermal. Overlying skin is not affected. THE END