* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical management of secondary antibody deficiency (SAD)
Survey
Document related concepts
Transcript
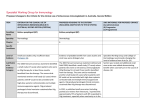
Clinical management of secondary antibody deficiency (SAD) Sinisa Savic Consultant clinical immunologist Conflict of interest • Research grants from BPL, Biotest, Baxter • Advisory board: Biotest • Travel grant: CSL Behring Overview of the talk • Causes • Selection criteria • Immunoglobulin replacement strategy • Practical matters • How to improve recognition and Rx of SAD • Concluding remarks Causes of SAD • Malignancy: Haematological >>>others • Chronic infections • Drugs • Protein-losing states, eg nephrotic syndrome • Systemic inflammatory diseases • Trauma -IgG levelsHow low can we go? Factors to consider • Isolated low IgG, panhypogamma or generalised immunosuppression • Underlying disease: severity and activity • Comorbidities bronchiectasis, CVD • Duration-temporary eg secondary to treatment EURO Lupus cohort • 36% presented with infection F/U • 30% of deaths related to infection Emery et al, Association between disease activity and risk of serious infection in subjects with RA treated with etanercept or DMARDS’s 2014, accepted for publication CLL • Infection cause of death between 25-50% • Hypogammaglobulinaemia present in up to 85% of patients • Common pathogens: – S. pneumoniae, – Haemophilus influenzae Hamblin AD, Hamblin TJ. The immunodeficiency of chronic lymphocytic leukaemia. Br Med Bull. 2008;87:49–62. Hypogamma 2nd to drugs Low IgG pre Rituximab-outcomes 10 IgG levles g/l 8 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 6 4 2 RA 6 CTD 0 Vas 0 no infections 2 2 3 Infections 5 6 5 Dead 0 Pre R N 29 Post R1 Post R2 Post R3 Post R IgM has a protective role against sinopulmonary infections-evidence form PID CVID patients who lacked IgM memory B-cells and failed to produce anti-PnPS IgM had greater incidence of respiratory infections and bronchiectasis Study of 473 patients -low baseline IgA, IgM, and IgG levels all correlate independently with chronic lung disease. Multicenter prospective study- 201 patients with CVID over a 5-year period. Mean IgA and IgM levels were significantly lower in patients who had more than 1 episode of pneumonia compared with patients with only 1 episode or no pneumonias. Anti-PS23 IgM and/or IgA antibodies were detectable in a minority of CVID patients. Antibody responses were correlated to B cell subpopulations and serum immunoglobulin concentrations. The non responders had a higher incidence of pneumonia and bronchiectasis and responders had the lowest incidence of respiratory complications Frequency and type of infections? Sinopulmonary infections and encapsulated bacteria Typical pathogens in PAD: • S. pneumoniae, • Streptococcus pyogenes • Haemophilus influenzae • Staphylococcus areus Poor record of infective episodes (many ‘minor’ chest infections treated in community) Challenge vaccination Areas of controversy • Adequate vaccine response and protective titers – Total vs serotype specific measurement – >0.35μg/ml, or >1.3 (>70% of serotypes tested) • Different methodologies for measuring Sp Ab • • 1.3 cutoff-27%(D28) and 40% (1yr) >0.35 cutoff- 4% Flow cytometry and Luminex • Prevaccination (5/10) • Postvaccination (3/10) • 86% agreement on SPAD SPAD • 43.7% ELISA (23v) • 32.8% Multiplex (>0.35) • 76.5% Multiplex >1.3 Other considerations • HiB titers do not correlate to non-typeable H.influenzae • Protective effects from pneumovax minimal at the best(1) • Role for other vaccine challenges- S. typhi (2) 2 1 M.A. J. Westerink et al Pneumococcal vaccines in adults and children Volume 3, Number 1; 51-67, February 2012 Review Immune Responses to pneumococcal vaccines in children and adults: Rationale for age-specific vaccination M.A. Julie Westerink1, Harry W. Schroeder, Jr.2, and Moon H. Nahm3* 1 University of Toledo, Department of Medicine, Division of Infectious Diseases, Department of Medical Microbiology and Immunology and Department of Pathology,Toledo OH 43614, USA University of Alabama at Birmingham, Department of Medicine, Division of Immunology and Rheumatology, Birmingham, AL 35294, USA 3 University of Alabama at Birmingham, Department of Pathology, Division of Laboratory Medicine, Birmingham, AL 35294, USA 2 [Received April 12, 2011; Revised July 19, 2011; Accepted July 19, 2011] ABSTRACT: Streptococcus pneumoniae is a significant human pathogen and currently available Consideration of dosage, interval and route of administration of immunoglobulin Dosage • 0.4-0.6 g/kg/month aiming to keep IgG >6 g/l • Higher doses might be necessary in patients with bronchiectasis • Ideal body weight as a guide to dose Evidence Khan S, Grimbacher B, Boecking C, et al. Serum trough IgG level and annual intravenous immunoglobulin dose are not related to body size in patients on regular replacement therapy. Drug Metabolism Letters. 2011;5(2):132-6. Route • IV or SC • Duration of treatment • Volume • Patient related factors – Comorbidities – Preferences • Hospital resources IVIG ScIG Vox Sanguinis (2013) 105, 54–64 ORIGINAL ARTICLE © 2013 International Society of Blood Transfusion DOI: 10.1111/vox.12025 Thromboembolic events associated with immunoglobulin treatment M. B. Funk,1 N. Gross,2 S. Gross,2 A. Hunfeld,3 A. Lohmann,1 S. Guenay,1 K. M. Hanschmann 4 & B. Keller- Stanislawski 1 1 Department Department Department 4 Department 2 3 of of of of Safety of Medicinal Products and Medical Devices, Paul-Ehrlich-Institut, Langen, Germany Immunology, Paul-Ehrlich-Institut, Langen, Germany Haematology/Transfusion Medicine, Paul-Ehrlich-Institut, Langen, Germany Biostatistics, Paul-Ehrlich-Institut, Langen, Germany. Objective Due to an increasing number of reported thromboembolic events (TEE) after the administration of one intravenous immunoglobulin (IVIG) and one subcutaneous immunoglobulin (SCIG), pharmacovigilance and laboratory data were collected to analyse the root cause and assess the reporting frequency of TEEs for various IG products. Methods Paul-Ehrlich-Institut retrospectively analysed 228 reports of TEEs associated with six different IG products and estimated annual TEE-reporting rates based on worldwide sale fi gures over a period of 6 years (2006–2011). In addition, non-activated partial thromboplastin time (NAPTT) testing was performed to capture pro-coagulant potential of six IG products (four IVIG and two SCIG). Received: 10 July 2012, revised 10 December 2012, accepted 13 December 2012, published online 9 February 2013 Results For three IVIGs, the drug-related TEE-reporting rates remained stable from 2006 to 2011 (0–0 83 cases per 1000 kg IVIG distributed). In contrast, the TEE rate of one IVIG increased signifi cantly from 0 33 cases in 2006 to nearly nine cases in 2010 (P < 0 001). The NAPTT testing of IG products with a low TEE rate revealed a NAPTT time >200 s and a NAPTT ratio >0 8, whereas TEE-associated batches of IG products with an increased TEE rate had a NAPTT ratio <0 8. After modifi cations of manufacturing processes, a normalization of NAPTT results and a decrease in TEE rates could be demonstrated. Key words: frequency, immunoglobulin – severity, IVIG – corrective actions, NAPTT, pharmacovigilance, Thromboembolic events. Introduction There is clinical evidence of an association between intravenous administration of immunoglobulin (IVIG) and thromboembolic events (TEEs) such as myocardial infarction, stroke, pulmonary embolism and deep vein thrombosis, which is assumed to be related to the relative increase in blood viscosity through the high infl ux of IG in at-risk patients [1]. An increased risk was found in patients with pre-existing risk factors for thrombotic events such as Correspondence: Markus B. Funk, Paul-Ehrlich-Institut, Division: Safety of Medicinal Products and Medical Devices, Paul-Ehrlich-StraÔe 51-59, 63225 Langen, Germany E-mail: [email protected] 54 advanced age, hypertension, diabetes mellitus, obesity and a history of vascular diseases and thrombotic episodes. The summary of product characteristics (core SPC) also emphasized that thromboembolic reactions are very rare undesirable effects [1]. In 2010, the Paul-Ehrlich-Institut (PEI) as the national competent authority suspended the marketing authorization of an intravenous immunoglobulin (IVIG) Octagam, which subsequently was also suspended by the European Commission due to an unexpected high number of reported TEEs and evidence of presence of pro-coagulant activity [2] in certain batches. In 2011, cases of thromboembolic events, including strokes and pulmonary embolism were notifi ed to the PEI following treatment with a subcutaneous immunoglobulin, (SCIG) Vivaglobin. Monitoring General considerations • IgG trough levels • Infection frequency • 6-12 months assessment • If trial of therapy- period of treatment At diagnosis of SAD J Clin Immunol DOI 10.1007/s10875-014-9995-5 ASTUTE CLINICIAN REPORT Antibody Deficiency Secondary to Chronic Lymphocytic L eukemia: Should Patients be Treated with Prophylactic Replacement I mmunoglobulin? Fatima Dhalla &M ar y L ucas &Anna Schuh & M alini Bhole &Rashmi Jain &Smita Y. Patel & Sir aj M isbah &Helen Chapel What is evidence for use of IVIG in secondary antibody deficiencies? Total :5119 SAD: 77 (1.5%) No data on SAD Total :6735 SAD: 430 (6.3%) No specific information on the type or cause of SAD 2013-July SAD:539 Leuk Lymphoma. 2009 May;50(5):764-72 Immunoglobulin prophylaxis in chronic lymphocytic leukemia and multiple myeloma: systematic review and meta-analysis. Raanani P, Gafter-Gvili A, Paul M, Ben-Bassat I, Leibovici L, Shpilberg O. Conclusion made on: • 1st randomized trial • Prior to introduction of com Rx • Different selection criteria • Different costs Commissioning Figure 2.1.1 Change to the approval process Red Priority – High Blue Priority – Medium Grey Priority – Low Black Clinician completes immunoglobulin request form Immunoglobulin Assessment Panel (IAP) review signed off by Trust immunoglobulin designated person Automatic IAP approval retrospective sign off by Trust immunoglobulin designated person approved by IAP approved by IAP not approved by IAP Individual funding request process All applications for immunoglobulin to be registered on the immunoglobulin database (accepted or declined) approved Immunoglobulin given and release of funding 2.1.1 Change to the approval process in 2013 The resulting change to the approval process (Figure not approved Immunoglobulin not given/funding not approved 2.2 Commissioner’s Database Information Service Figure 2.4.1 The Immunoglobulin Key Performance Indicators Dashboar d Prepared by Methods Insight Analytics for NHS England Immunoglobulin Specialised Service Quality Dashboard Winter 2013/14 S pine Charts LEEDS TEACHING HOSPITALS NHS TRUST Dom Thm Quarterly Indicators (Q3 1314) 2 CO IVG06 Proportion of patients who are receiving immunoglobulin for a grey/black indication who have outcomes entered on the national database 5 CO IVG09 Rate of adverse events documented on the national database 4 CP IVG10 3 CO IVG11 2 CP IVG12 Rate of patients receiving immunoglobulin for designated short term conditions who are re-registered on the national database Rate of patients receiving immunoglobulin for designated short term red/blue indication who have outcomes reported on the national database Patients receiving immunoglobulin for designated grey and grey unlisted indications who have been reviewed and approved by a multidisciplanary panel before commencing on immunoglobulin therapy Rolling Year Indicators (RY Q3 1314) Proportion of patients who are on long term immunoglobulin therapy for PID who have 6 monthly trough immunoglobulin levels measured IVG01 2 CP 5 CP IVG03 5 CP IVG04 5 CP IVG05 2 CP IVG07 2 CP IVG13 2 CP IVG15 Lower Limit 3SD 2SD Acute Trust Value Upper Limit 2SD 3SD National Mean Num Denom Value National Mean <5 <5 100.0% 38.5% <5 <5 0.1% 0.5% <5 <5 0.0% 4.3% 18 23 78.3% 45.5% <5 <5 100.0% 100.0% Num Denom Value National Mean 54 111 48.6% 73.4% 105 105 100.0% 83.3% 52 52 100.0% 81.3% 111 111 100.0% 102.9% 84 235 35.7% 29.7% Rate of patients on long term immunoglobulin therapy for a neurological condition who have oBjective measures of improvement documented <5 <5 16.1% 35.3% Rate of patients who are on immunoglobulin for a long term condition who receive an annual review and a letter is sent to the GP 76 76 100.0% 96.9% Proportion of patients receiving immunoglobulin for PID who are treated via homecare Proportion of patients receiving immunoglobulin for PID who are receiving treatment at home who have received training from an accredited home therapy centre Proportion of patients receiving immunoglobulin who are entered on the national database Number of patients who are receiving immunoglobulin for a long term condition who have documented evidence of dose reduction and/or increased dosing interval Trust Comments IVG01 Figure from IVIG database. Higher percentage have had done and on results server but this data not easily accessible. S PC Sparklines Lower 3SD Acute Trust Value National Mean Upper 3SD Chart Trend Chart Trend Are we likely to see more cases of secondary antibody deficiency in the future? Reduction in IgG serum levels post rituximab-RA 35 **** **** **** IgG levles g/l ** * ** 16 Normal range 6 5 N 517 379 261 167 103 59 17 Po st R 7 R 7 Pr e Po st R 6 R 6 Pr e Po st R 5 R 5 Pr e Po st R 4 R4 Pr e Po st R 3 R 3 Pr e Po st R 2 R 2 Pr e R 1 st Po Pr e R 1 0 Reduction in IgM serum levels post rituximab-RA 7 **** **** IgM levles g/l **** **** *** * 2.5 Normal range 0.6 N 517 379 261 167 103 59 17 7 R Po st R 7 Pr e 6 R Po st R 6 Pr e 5 R Po st R 5 Pr e 4 R Po st R4 Pr e 3 R Po st R 3 Pr e 2 R Po st R 2 Pr e 1 R Po st Pr e R1 0 % of patients with reduced Ig’s following rituximab 80 70 60 RA 50 40 30 20 10 0 Pre Rx C1 C2 C3 C4 C5 C6 C7 80 IgG 70 60 CTD IgA 50 40 30 IgM 20 10 0 Pre Rx C1 C2 C3 C4 C5 C6 100 80 Vasculitis 60 40 20 0 Pre-Rx C1 C2 C3 C4 C5 Rate of infection post rituximab 60 50 40 30 20 10 0 Sinopulomonary UTI Other Table 2 PI3K inhibitors in clinical trials Drug Target(s) Tumors Toxicities Idelalisib (CAL-101) p110-δ Buparlisib (BKM-120) p110-α,-β, -δ,-γ CLL/SLL, iNHL, MCL breast, GBM, NSCLC GDC-0941 p110-α,-β, -δ,-γ pyrexia, nausea, decrease appetite, fatigue rash, hyperglycemia diarrhea, anorexia nausea, diarrhea, rash vomiting, anorexia PX-866 p110-α,-β, -δ,-γ breast, NSCLC, melanoma endometrial, pancreatic ovarian, prostate, GBM NSCLC breast, NSCLC Clinical trials III References [76,77,80,83,86,88-90] IB/II [103-109] IB/II [117-123] fatigue, diarrhea II [126-129] thromboembolism GDC-0032 p110-α, -δ,-γ diarrhea, hyperglycemia I [132] fatigue, nausea, decreased appetite BAY 80-6946 p110-α,-β NHL, esophageal, alopecia, dysgeusia anemia, I [135-137] sarcoma pancreatic mucositis IPI-145 p110-δ,-γ CLL/SLL, iNHL, cytopenias liver enzyme I [138,139] MCL elevations BEZ-235 p110-α,-β, -δ,-γ/mTOR breast, GBM mucositis IB/II [149-152] BYL-719 p110-α breast, cervical, nausea, diarrhea IB/II [153-155] endometrial ovarian, hyperglycemia,vomiting H&N BGT-226 p110-α,-β, -δ,-γ/mTOR solid tumors, breast nausea, vomiting diarrhea I/II [156] PF-04691502 p110-α,-β, -δ,-γ/mTOR endometrial fatigue, nausea, vomiting II [162] decreased appetite, rash GDC-0980 p110-α,-β, -δ,-γ/mTOR prostate hyperglycemia, rash IB/II [167,168] mucositis GSK-2126458 p110-α,-β, -δ,-γ/mTOR RCC, bladder nausea, vomiting diarrhea I [169,170] PF-05212384 p110-α,-γ/mTOR solid tumor, CRC rash, mucositis II [172] transaminitis, hyperglycemia XL-765 p110-α,-β, -δ,-γ/mTOR NSCLC, gliomas nausea, diarrhea elevated IB/II [176-178] liver enzymes XL-147 p110-α,-β, -δ,-γ solid tumor, GBM nausea, vomiting diarrhea I/II [180-183] Abbreviations: CLL/SLL chronic lymphocytic leukemia/small lymphocytic leukemia; CRC colorectal cancer; GBM glioblastoma multiforme; H&N head and neck cancer; iNHL indolent non-Hodgkin’s lymphoma; MCL mantle cell lymphoma; NHL non-Hodgkin’s lymphoma; NSCLC non-small cell lung cancer; RCC renal cell cancer. Idelalisib (CAL-101, GS-1101) Idelalisib (formerly CAL-101, GS-1101) is an oral, first-in-class, highly selective inhibitor of How to improve management of SAD • Improved recognition – Patient infection/vaccination passport – Improved testing of immune function • Prospective studies of IgG replacement • Better documentation of outcomes