* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download C. perfringens
Transmission (medicine) wikipedia , lookup
Triclocarban wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Urinary tract infection wikipedia , lookup
Infection control wikipedia , lookup
Globalization and disease wikipedia , lookup
Germ theory of disease wikipedia , lookup
Neonatal infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
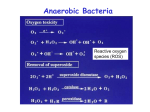
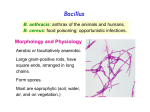
Anaerobic Bacteria Reactive oxygen species (ROS) Anaerobiosis Anaerobic bacteria do not grow in the presence of oxygen. Possible mechanisms: 1) Lack of cytochrome systems for the metabolism of O2. 2) Short of superoxide dismutase. 3) Short of catalase. 4) other unknown mechanisms. Ability of anaerobes to tolerate oxygen or grow in its presence varies from species to species. Most anaerobic clinical isolates are moderately obligate anaerobes, and have small amount of both catalase and superoxide dismutase. Methods for excluding oxygen 1. Fluid media containing fresh animal tissue or 0.1% agar containing a reducing agent, thioglycollate. 2. Anaerobic jar 3. Anaerobic glove chamber Anaerobic bacterial pathogens Non-sporeforming anaerobes Bacteroides spp., Fusobacterium spp., Porphyromonas spp., Prevotella spp., Veillonella spp., Actinomyces spp., Propionibacterium spp., Peptostreptococcus spp. Sporeforming anaerobes Clostridium spp. Non-sporeforming anaerobes 1. Non-sporeforming anaerobes constitute the predominant part of normal indigenous flora in human body. 2. Diseases caused by them are usually not transmissible and are almost autoinfection. The result is usually tissue necrosis and abscess formation. 3. Types of infections are related to the normal endogenous location of the bacteria (Table 41-1). 4. Most infections caused by them are mixed, containing 5-6 species or more, including both anaerobes and facultative anaerobes (synergism). 5. In most cases, treatment requires drainage of the purulent material and appropriate chemotherapy (e.g., metronidazole, carbapenems, clindamycin, etc.) Bacteroides fragilis Pleomorphic in size and shape; capsulated. Aerotolerant; growth is stimulated in 20% bile. Constitutes less than 10% of Bacteroides species in the normal colon, however, is the most common isolate of anaerobes from infections (intra-abdominal, gynecologic, and skin and soft tissue infections; bacteremia.) Major virulence factor Capsular polysaccharides, which may cause abscess formation when injected into the rat abdomen. Its LPS lacks endotoxin activity. The clinical signs of sepsis (fever & shock) could be due to other components. Resistant to penicillin. Bacteroides fragilis Some B. fragilis strains may cause a self-limited watery diarrhea in young children by producing an enterotoxin. This enterotoxin is a heat-labile metalloprotease (B. fragilis toxin, BFT), which causes morphological changes of the intestinal epithelium that leads to stimulation of chloride secretion and fluid loss. Clostridium C. perfringens: gas gangrene; food poisoning C. tetani: tetanus C. botulinum: botulism C. difficile: pseudomembranous colitis Physiology and Structure Anaerobic. Large gram-positive rods. The spores are usually wider than the rods, and are located terminally or subterminally. Most clostridia are motile by peritrichous flagella. C. perfringens Physiology and Structure Large gram-positive bacilli. Spores are rarely observed. Non-motile; capsulated. Hemolytic and metabolically active. Subdivided into 5 types based on the four major lethal toxins they produce. Type A causes most of the human infections. C. perfringens Pathogenicity and Immunity Strains of C. perfringens (particularly type A) are widely distributed in nature, and inhabit the intestine of humans and animals. They (type A strains are most commonly isolated from human infections) cause a spectrum of diseases primarily by producing toxins and enzymes: a-toxin: lecithinase (phospholipase C) that lyses a variety of cells. Lethal, necrotizing and hemolytic. Increases vascular permeability, resulting in massive hemolysis and bleeding, tissue destruction, hepatic toxicity, and myocardial dysfunction. Other necrotizing and hemolytic toxins DNase, hyaluronidase Enterotoxin: produced primarily by type A strains. C. perfringens Clinical Diseases Soft tissue infections Portal of entry: trauma or intestinal tract. Usually caused by mixed infection including toxigenic clostridia, proteolytic clostridia and various cocci and gramnegative organisms. Three types of infections with increasing severity: Cellulitis: gas formation in the soft tissue. Fasciitis or suppurative myositis: accumulation of gas in the muscle planes. Myonecrosis or gas gangrene: a life-threatening disease. C. perfringens Clinical Diseases Gas gangrene Spores germinate vegetative cells multiply, ferment carbohydrates and produce gas in the tissue. This results in distension of tissue and interference with blood supply the bacteria produce necrotizing toxin and hyaluronidase, which favor the spread of infection tissue necrosis extends, resulting in increased bacterial growth, hemolytic anemia, then severe toxemia and death. Incubation: 1-7 days after infection. Symptoms: Crepitation in the subcutaneous tissue and muscle, foul smelling discharge, rapidly progressing necrosis, fever, hemolysis, toxemia, shock, renal failure, and death. Can be also caused by other Clostridium species. C. perfringens Clinical Diseases Food poisoning The enterotoxin causes marked hypersecretion in jejunum and ileum. Enterotoxin: a heat-labile protein produced by some strains of C. perfringens type A. It is released when >108 cells in contaminated meat are ingested and sporulate under the alkaline conditions in the small intestine. It disrupts ion transport in the enterocytes. It is a superantigen and induces antibodies (non-protective) in adults. Symptoms: diarrhea, usually without vomiting or fever. Necrotizing enteritis (pig-bel): a fatal disease (acute necrosis in jejunum attributed to b-toxin) in children in New Guinea caused by type C C. perfringens. Clotridium bacteremia usually occurs in patients with tumors. C. perfringens Laboratory Diagnosis Specimens: pus, necrotic tissue, feces, food, etc. Smears: large gram-positive rods with or without spores, usually in the absence of leukocytes. Culture: anaerobic culture on blood plate. Identification: “Storming fermentation”-- clot torn by gas in 24 hrs. Lecithinase test-- precipitate formed around colonies on egg yolk media. Biochemical tests. C. perfringens Treatment Treatment for suppurative myositis or myonecrosis: Prompt and extensive débridement. Antibiotics (penicillin) administration. Hyperbaric oxygen may "detoxify" patients rapidly. C. perfringens food poisoning requires only symptomatic care. Prevention, and Control Preventive measures: surgical débridement and prophylactic antibiotics. C. tetani Physiology and Structure Small, motile; Spore-forming (drumstick appearance); Extremely sensitive to oxygen toxicity. Pathogenesis and Immunity Tetanospasmin is responsible for clinical manifestations of tetanus. An A-B toxin, released when the bacteria lyse. Subunit A is a zinc-endopeptidase that acts on CNS: Inhibits release of an inhibitory mediator (e.g., GABA or glycine) which acts on postsynaptic spinal neurons (causing spastic paralysis). C. tetani Pathogenesis and Immunity Contamination of devitalized tissue (wound, burn, injury, umbilical stump, surgical suture) with the spores germination of the spores release of tetanospasmin the toxin reaches CNS by retrograde axonal transport or via the bloodstream the toxin is fixed to gangliosides in spinal cord or brainstem and exerts its actions. Germination of the spore and production of toxin are aided by conditions that lead to low oxidation-reduction potential: Necrotic tissue; calcium salts; associated pyogenic infections. C. tetani Clinical Diseases Generalized tetanus Incubation period: 4-5 days. Symptoms: convulsive tonic contraction of voluntary muscles. Spasms involve first the area of injury, then the muscles of the jaw (trismus or lockjaw; risus sardonicus). Other voluntary muscles become involved gradually, resulting in generalized tonic spasms (opisthotonos). Death usually results from interference with respiration. The mortality rate of generalized tetanus: ~50%. In more severe cases, the autonomic nervous systems are also involved. Localized tetanus (confined to the musculature of primary site of infection) Cephalic tetanus (site of infection: head) Neonatal tetanus (infection of the umbilical wound): mortality > 90%, and developmental defects are present in survivors. C. tetani Laboratory Diagnosis Diagnosis depends on the clinical picture and a history of injury. Proof of isolation of C. tetani from contaminated wounds depends on production of toxin and its neutralization by specific antitoxin. Treatment, Prevention, and Control Prevention is much more important than treatment: 1. Active immunization with toxoid. ‘Booster shot’ for previously immunized individuals. This may be accompanied by antitoxin injected into a different area of the body. 2. Proper care of wounds. Surgical débridement to remove the necrotic tissue. 3. Prophylactic use of antitoxin. 4. Antibiotic treatment. Metronidazole; not penicillin (it inhibits GABA activity) *Patients with symptoms of tetanus should receive muscle relaxants, sedation and assisted ventilation. C. tetani Control Active immunization with tetanus toxoid (toxin detoxified with formalin) Aluminum salt-adsorbed toxoid DPT vaccine Course of immunization: as mentioned in C. diphtheriae. C. botulinum Physiology and Structure This species is a heterogeneous group of fastidious, sporeforming, anaerobic bacilli. Produce seven (A-G) antigenically distinct toxins (botulinum toxins; Botox). Types A, B, E, and F are most commonly associated with human illness. These are composed of a neurotoxic protein with a lethal dose of 1-2 mg. Liberated during the growth and during autolysis of the bacteria. A-B toxins. The subunit A is a zinc-endopeptidase blocking release of acetylcholine at peripheral cholinergic synapses. Destroyed by heating for 20 min. at 100 oC. C. botulinum Pathogenicity and Immunity An intoxication. Ingestion of food (spiced, smoked, vacuum-packed, or canned alkaline foods) in which C. botulinum has grown and produced toxin the toxin acts on both the voluntary and autonomic nervous systems at synapses and neuromuscular junctions flaccid paralysis. C. botulinum Clinical Diseases Foodborne botulism Incubation period: 18-24 hrs. Symptoms: double vision, inability to swallow, speech difficulty, bulbar paralysis, constipation, and abdominal pain. Bilateral descending weakness of peripheral muscle. Death occurs from respiratory paralysis (mostly) or cardiac arrest. No fever. Mortality is reduced through better supportive care. Recovery may need months to years. Patients who recover do not develop antitoxin. 肉毒素中毒症 一名六十多歲原住民婦女吃了家人醃製的山豬肉,兩、三天後, 即出現噁心、嘔吐、眼瞼下垂、說話說不清楚、吞嚥困難及手腳 沒力的症狀,到醫院就醫,後來轉送至北榮神經內科,經會診毒 物科採集病患血液、胃抽取物及糞便送至衛生署疾管局化驗,才 確定病患是肉毒素中毒。另一個病例則是新竹市一對姊妹疑似吃 了自己做裝在罐子內的素食肉燥,結果姊姊出現眼瞼下垂、視力 模糊、吞嚥困難及說話說不清楚等症狀,最後甚至呼吸困難插管 住進加護病房。根據衛生署疾管局統計,食物型肉毒素中毒案例, 九十四年有一例、九十五年兩例、九十六年三例。台北榮總毒物 科主治醫師楊振昌表示,肉毒桿菌為厭氧性的細菌,一般的魚貝 肉類及蔬菜均有污染到肉毒桿菌孢子的危險性。醃製品多為罐裝 密封口,提供肉毒桿菌厭氧的生長環境,另醃製的肉品未洗淨或 是鹽加的不夠,食用前,又未高溫加熱,肉毒素即可能會吃下肚。 Modified from 自由時報 97.4.23新聞 C. botulinum Clinical Diseases Infant botulism Occurs in infants < 1 year. Weakness, signs of paralysis, C. botulinum and its toxin are found in feces. May be caused by ingestion of the bacteria or spores which grow in the gut and produce toxin. Mortality is very low. Feeding of honey has been implicated as a possible cause. Patients recover with supportive therapy alone. Wound botulism Develops from contaminated wounds. Symptoms similar to those of food borne botulism with longer incubation time. Less GI symptoms. C. botulinum Laboratory Diagnosis Culture of C. botulinum in patient feces and implicated food. Detection of toxin in feces or serum from the patient and in leftover food: i.p. injection of mice die rapidly. Toxin may also be detected by other serological tests. Typing of toxin is done by neutralization with specific antitoxin in mice. Treatment Stomach lavage and high enemas, and metronidazole or penicillin therapy. Trivalent (A, B, E) antitoxin administered intravenously promptly. Adequate ventilation by mechanical respirator. C. botulinum Prevention and Control Spores of C. botulinum are widely distributed in soil and often contaminate vegetables, fruits etc. Strict regulation of commercial canning has largely reduced the danger of widespread outbreaks. The chief danger lies in home-canned foods (e.g. canned vegetables), smoked fish or vacuum-packed fresh fish. The cans with toxic food may swell or may show innocuous appearance. The risk from home-canned food can be reduced by boiling the food for 20 min. Children younger than 1 year should not eat honey. Botulinum toxins can be used as biochemical warfare and cause inhalation botulism with high mortality. C. difficile C. difficile is responsible for antibiotic-associated gastrointestinal disease ranging from self-limited diarrhea to severe, life threatening psudomembranous colitis. It is a part of normal intestinal flora in a small number of healthy people and hospitalized patients. The spores can contaminate an environment for many months and can be a major source of nosocomial outbreaks. This organism produces two toxins: Toxin A (an enterotoxin) disrupts tight junction, resulting in increased permeability of intestinal wall and subsequent diarrhea. Toxin B (a cytotoxin) causes tissue damage. C. difficile Pseudomembranous colitis Administration of antibiotics results in proliferation of drug-resistant C. difficile. Antibiotics that are most commonly associated with pseudomembranous colitis are ampicillin, fluoroquinolones, and clindamycin. Disease occurs if the organism proliferates in the colon and produces toxins: watery or bloody diarrhea, abdominal cramps, leukocytosis and fever. Laboratory diagnosis depends on isolation of C. difficile in the feces and detection of toxins with tissue culture cells (cytotoxicity assay). The disease is treated by discontinuing the offending antibiotic, and orally giving either metronidazole or vancomycin in severe cases. C. difficile Antibiotic-associated diarrhea 25% of cases are associated with C. difficile. Mild to moderate diarrhea, less severe than the typical pseudomembranous colitis. The role of the toxins is not well understood. Other Clostridial Species C. septicum is a cause of nontraumatic myonecrosis and frequently exists in patients with occult colon cancer, acute leukemia, and diabetes. It can spread from GI tract into tissue and result in fulminant infection with high mortality within 1 to 2 days. B. fragilis +Ab -Ab Nagler’s reaction