* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Aspirin Resistance in Cardiovascular Disease
Pharmacokinetics wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Paracetamol wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
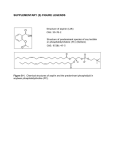
Analgesic??????? An agent that subdues pain by acting in the CNSor on peripheral pain mechanism Classification of Analgesics a) Opioid Analgesics b) Non – opioid Analgesics NON-STEROIDAL ANTI-INFLAMMATORY DRUGS What are NSAIDs? Non- opioid; non-narcotic analgesics Analgesic, antipyretic, anti- inflammatory actions Weaker analgesics than morphine Do not depress CNS No dependence Acts primarily on peripheral pain mechanisms Weakly acidic compounds Highly protein bound Orally absorbed The major pharmacological actions of these drugs are due to their ability to inhibit the synthesis of prostaglandins Beneficial actions due to PG synthesis inhibition: Analgesia Antipyretic Anti-inflammatory Antiplatelet Closure of ductus arteriosus Toxicity due to PG synthesis inhibition: Gastric mucosal damage Bleeding Na+ and H2O retention Prolongation of labour Asthma History The medicinal properties of willow bark (salix alba) was known since centuries In the 5th century, people used the bitter powder extracted from willow bark to relieve pain Salicilin salicylic acid In 1897 aspirin was discovered by Felix Hofmann 1949: phenylbutazone 1950: paracetamol 1963: indomethacin I) Non-selective COX inhibitors: 1. Salicylates: Aspirin, Diflunisal 2. Paraaminophenol derivatives: Paracetamol 3. Pyrazolone derivatives: Phenylbutazone 4. Indole acetic acid derivatives: Indomethacin, Sulindac 5. Aryl acetic acid derivatives: Diclofenac, Tolmetin 6. Propionic acid derivatives: Ibuprofen, Naproxen, Ketoprofen 7. Antranilic acids: Mefenamic acid, Flufenamic acid 8. Oxicams : Piroxicam, Tenoxicam 9. Alkanones : Nabumetone 10. Pyrrolo-pyrole derivative: Ketorolac II) Selective COX-2 inhibitors Nimesulide, Celecoxib, Rofecoxib ASPIRIN One of the oldest drugs Acetylsalicylic acid Rapidly converted in the body to salicylic acid Aspirin: Mechanism of Action Membrane Phospholipids Arachidonic Acid Cyclooxygenase Lipooxygenase PGH2 Prostaglandins PGG2 Thromboxanes Leukotrienes Aspirin: Mechanism of Action Membrane Phospholipids Aspirin Arachidonic Acid Cyclooxygenase Lipooxygenase PGH2 Prostaglandins PGG2 Thromboxanes Leukotrienes COX-1 Continuously stimulated by the body Its concentration in the body remains stable Creates PGs used for basic housekeeping through out the body PGs stimulate normal body functions such as stomach mucous production, regulation of gastric acid secretion, Na+ & water excretion… COX-2 Induced Stimulated only as apart of immune response Used for signaling pain & inflammation Produces PGs for inflammatory response Pharmacological actions 1.ANALGESIA ( 0.3- 1.5/day) Good analgesic, but weaker than morphine Relieves non-visceral pain such as inflammatory, tissue injury related etc… Relieve pain from integumental structures No Euphoria & No Tolerance Analgesic effect is due to: 1. Inhibition of PG synthesis 2. ↑ the threshold to pain perception at central subcortical level 2. Antipyretic action: ↓ body temperature of patients having pyrexia Inhibits PG synthesis in hypothalamus Promotes heat loss by peripheral vasodilatation & sweating 3. Anti-inflammatory action Occurs at high doses ( 3-6 g/day) Potent anti-inflammatory agent Signs of inflammation are suppressed Inhibition of PG synthesis Antagonizes the action of bradykinin 4. Respiration Respiration is stimulated Anti-inflammatory dose ↓ ↑ O2 consumption by skeletal muscles ↓ ↑ CO2 production ↓ Respiratory stimulation ↓ Removal of plasma CO2 ↓ Respiratory Alkalosis High dose : Respiratory centre depression 5. Acid- Base & Electrolyte balance Anti-inflammatory doses ↓ Alkaline pH ↓ ↑ Excretion of HCO3 ,Na+,H2O ↓ Normal pH ↓ Compensated Respiratory Alkalosis 5. Acid- Base & Electrolyte balance Toxic Doses Depress VMC Depress Respiratory centre Impairs Renal Function ↑↑ CO2 Accumulation of strong acids ↓ pH Respiratory Acidosis Uncompensated Metabolic Acidosis 6. Metabolic Effects Anti-inflammatory doses ↓ Uncoupling of oxidative phosphorylation ↓ ↑ Cellular Metabolism ↓ ↑ Heat production ↓ ↑ Utilization of glucose ↓ ↓ Blood sugar level Large Dose: a) Negative nitrogen balance b) Hyperglycemia 7. G.I.T Gastric irritant: epigastric distress; Nausea; Vomiting High Doses : Gastritis; Gastric ulceration; GI bleeding Salicylic Acid Adhere to gastric mucosa Inhibit PGE synthesis Irritation Gastritis; Peptic Ulcer How to avoid GI irritation & Ulcer ? Aspirin should be administered 1. With plenty of water 2. With an alkali 3. With misoprostol, a PGE analogue 8. CVS High dose : depress VMC ↓ BP 9. Uric Acid Excretion Therapeutic doses: ↓ urate excretion High doses : ↑ urate excretion 10. Blood Prostaglandins Thromboxane synthetase TXA2 Inhibit Adenyl cyclase ↓ Platelet cAMP ↑ Platelet aggregation 10. Blood ___ ASPIRIN Prostaglandins Thromboxane synthetase TXA2 is not synthesized No Inhibition Adenyl cyclase ↑ Platelet cAMP ↓ Platelet aggregation Pharmacokinetics Absorbed from stomach & upper intestine Rapid deacetylation→ salicylic acid 80% plasma protein bound Crosses BBB & placenta Metabolism : glycine conjugation Excretion : kidney Half life: 3-5 hours Adverse Effects Nausea, vomiting, epigastric distress, occult blood loss Rashes, urticaria, rhinorrhea,angioedema, asthma SALICYLISM dizziness, tinnitus, vertigo reversible impairment of hearing & vision excitement, mental confusion Liver damage: Reye’s syndrome Nephrotoxicity Acute salicylate intoxication (15- 30g) Manifestations dehydration, GI irritation, vomiting acid- base imbalance hyperpyrexia restlessness, delirium, hallucination tremor, convulsions haematemesis respiratory failure Treatment of Acute salicylate Intoxication Gastric lavage IV fluids External cooling Vit K & blood transfusion Alkaline diuresis CONTRAINDICATIONS Peptic ulcer Children suffering from influenza Chronic liver disease Diabetics Pregnancy prolongation of labour greater postpartum blood loss premature closure of ductus arteriosus Stopped 1 week before surgery Drug Interactions Displaces Warfarin, Sulfonylureas, Phenytoin, Methotrexate from their protein binding sites. Antagonizes the action of probenecid Blunts the action of diuretics Therapeutic Uses Head ache, back ache, myalgia, joint pain pulled muscle, neuralgia, dysmenorrhoea Fever Acute Rheumatic fever first choice 4-6g/day Rheumatoid arthritis relieves pain, swelling, morning stiffness 3-5 g/day Osteoarthritis Patent ductus arteriosus Therapeutic Uses Myocardial infarction Low dose aspirin started immediately after MI prevents reinfarction and reduce mortality. Use with or with out Heparin Clopidogrel/Ticlopidine are alternatives Therapeutic Uses Unstable Angina Aspirin (100- 150 mg/day) given along with Heparin followed by Warfarin decreases risk of MI & sudden death in patients with unstable angina. Clopidogrel/Ticlopidine are alternatives/adjuvant to aspirin. Therapeutic Uses Cerebrovascular disease Aspirin has been used to prevent transient ischemic attacks of stroke in patients with cerebrovascular disease, although aspirin do not alter the cause of stroke Aspirin considered a wonder drug for >50 years (1899-1950), inhibit Cyclooxygenase, . . . but found to cause gastrointestinal ulcers and bleeding, to cause CNS “salicylism,” altered acid-base balance (respiratory alkalosis), Reye’s syndrome in children with viral infections. . . MORPHINE 1. Basic drug 2. Potent analgesic 3. Relieves visceral pain 4. Removes the associated reactions to intense pain ASPIRIN 1. Acidic drug 2. Potent analgesic 3.Relieves inflammatory, tissue injury related pain 4. Does not remove the associated reactions to intense pain 5. No anti-inflammatory/ antipyretic action 5. Potent anti-inflammatory/ antipyretic action 6.Produces sedation 6. No sedation MORPHINE 7. Produces euphoria 8. Depress respiratory centre 9. Depress cough centre 10. High dose ↓BP 11.Do not cause acid- base imbalance 12.No GI irritation; bleeding 13. Produce constipation 14. Produces miosis 15. Causes tolerance & dependence 16. Precipitate asthma 17. No Salicylism 18. No antiplatelet action 19. Pre- anaesthetic medication ASPIRIN 7. No euphoric effects 8. Stimulates respiratory centre 9. No effect 10. High dose ↓BP 11. Produce acid- base imbalance 12.Cause GI irritation; bleeding 13.No constipation 14.No miosis 15. No tolerance & dependence 16. Precipitate asthma 17. Causes Salicylism 18. Antiplatelet action 19. Not a pre- anaesthetic medication PARACETAMOL Acetaminophen De-ethylated active metabolite of PHENACETIN Commonly used drug Over The Counter (OTC) drug Potent antipyretic & equianalgesic with Aspirin Weak/no anti-inflammatory action More active on COX in brain Poor inhibitor of PG synthesis in peripheral tissues No GI irritation, acid-base imbalance No affect on blood No respiratory stimulation Not uricosuric Pharmacokinetics Well absorbed orally Metabolism : liver i) glucuronide conjugation ii) sulfate conjugation Excretion: kidney Half life: 2-3 hours Adverse Effects Safe & well tolerated Nausea, rashes, anemia Nephropathy Acute Toxicity(>150mg/kg) Early manifestations nausea, vomiting, liver tenderness After 12-18 hours centrilobular hepatic necrosis renal tubular necrosis hypoglycemia coma After 2 days jaundice, hepatic failure, death Mechanism of toxicity Paracetamol (150mg/day) Saturation in glucuronidation capacity ↑ NABQI (minor metabolite) Binds to proteins in liver NECROSIS Treatment Gastric lavage Activated charcoal Specific antidote: N-acetylcysteine Replenishes glutathione stores of liver 150mg/kg IV for 15 min; followed by same dose IV over the next 20 hours Therapeutic uses Headache, musculoskeletal pain Dysmenorrhoea OSTEOARTHRITIS Fever 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. ASPIRIN Potent analgesic Good antipyretic Potent anti-inflammatory agent Inhibits COX even in presence of peroxides Stimulate respiratory centre Alter acid- base balance Increase cellular metabolism Produces GI irritation Inhibit platelet function Metabolism: glycine conjugation SALICYLISM Reye’s syndrome Nephropathy No specific antidote for acute poisoning 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. PARACETAMOL Potent analgesic Good antipyretic No anti-inflammatory action Do not inhibit COX in presence of peroxides Do not stimulate respiratory centre Do not alter acid- base balance Do not increase cellular metabolism Do not produce GI irritation Do not inhibit platelet function Metabolism: glucuronide conjugation No SALICYLISM No Reye’s syndrome Nephropathy Specific antidote for acute poisoning : N- acetylcysteine Ibuprofen Introduced in 1969 Analgesic, Antipyretic & Anti-inflammatory activity similar to aspirin Better tolerated orally Inhibition of synthesis of PG 92-99% bound to plasma albumin Adverse Effects Nausea, Vomiting Gastric discomfort Headache, Dizziness, Blurred vision Tinnitus Edema Therapeutic uses As an analgesic Fever Dysmenorrhoea Rheumatoid arthritis Tooth extraction, Fractures, Soft tissue injuries Indomethacin Potent anti-inflammatory agent Promptly acting antipyretic Good analgesic action Inhibit PG synthesis Suppress neutrophil activity Well absorbed orally Metabolism: liver glucuronide conjugation Half life: 2-5 hours Adverse Effects Gastric irritation, gastric bleeding, diarrhea Nausea, anorexia Head ache, Giddiness, Mental confusion Blurring of vision Therapeutic uses Ankylosing spondylitis Acute Gout Closure of patent ductus arteriosus Diclofenac Analgesic, antipyretic, anti-inflammatory agent Inhibit PG synthesis, neutrophil chemotaxis, super-oxide production Well absorbed orally Accumulates in synovial fluid GI distress, epigastric pain, nausea, dizziness Therapeutic uses Rheumatoid arthritis Ankylosing spondylitis Dysmenorrhoea Post-operative inflammatory conditions Wound edema