* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download - Free Documents
Urinary tract infection wikipedia , lookup
Cysticercosis wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Chagas disease wikipedia , lookup
Hepatitis C wikipedia , lookup
Neonatal infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Infection control wikipedia , lookup
Transmission (medicine) wikipedia , lookup
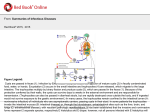
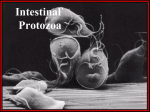
Protozoa Dr Mohiedd n M Abdul Fattah Luminal protozoa . Intestinal amoebae Entamoeba histolytica and E.dispar. . Intestinal flagellates Giardia intestinalis. . Urogenital flagellates Trichomonas vaginalis . Intestinal apicomplexans coccidia Cryptosporidium parvum and C hominis . Intestinal ciliates Balantidium coli Patterns of protozoan life cycle Blood and Tissue protozoa .Blood flagellates Trypanosoma and Leishmania. .Blood apicomplexans coccida Plasmodium malaria parasites and Toxoplasma gametocytes GAMETOGONY zygote SPOROGONY merozoites MEROGONY sporozoites Amoebae E. histolytica and dispar A. Biology Final host Human. Habitat Colon Exit stage trophozoites, precysts, binucleate and Quadrinucleate cysts in feces. Basic morphology trophozoite m amoeboid, and round cyst m. Amoebae Basic Morpology and Life Cycle Entamoeba histolytica large intestine but can invade extraintestinal sites Amoebae Life cycle . Trophozoites colonize large intestine feed on bacteria and debris replicate by binary fission . Trophozoite rounds up to form cyst secretion of cyst wall aggregation of ribosomes chromatoid bodies rounds of nuclear division occur p nuclei survive weeks to months Amebae E. histolytica and dispar B. Epidemiology Distribution both are worldwide of E. histolytica cases are symptomatic, severe infections occurs in pregnant women, young children, the malnourished and people on steroids. Transmission . Intermediate host none . Reservoir host none . Infective stage nuclei cyst. It remains viable in damp cool conditions up to months . Mode of infection ingestion of food and drinks contaminated by the infective stage C.Host r sit r l tionshi The nonpathogenic E. dispar is non invasive. Only E histolytica is invasive and symptomatic, but under certain condition it is non invasive and non symptomatic. Noninvasive condition . Amebae colonize on mucosal surface without inducing symptoms Asymptomatic cyst passer or it induces . Nondysenteric diarrhea . Invasive amebiasis Invasive ondition a Amebae invade mucosa ulcer Dysentery. b Via blood invasion or by direct extension Metastasis extraintestinal amebiasis. . Primarily liver amebic abscess . Other sites skin, lung and brain. Amebafree stools are common in such situations. Colitis is the ost ommon form of disease associated with amoebae Amoeba invade mucosa and erode through laminia propria causing characterisitic flask shaped ulcers contained by muscularis Invasive intestinal phase continued ulcer enlar ement p severe dysentery perforation of intestinal wall p peritonitis local abscesses o bacterial infections occasional ameboma amebic ranuloma cessation of cyst production ameboma inflammatory thickening of intestinal wall around the abscess can be confused with tumor Ulceration can lead to secondary infection and extraintestinal lesions Extraintestinal Amebiasis metastasis via blood stream primarily liver portal vein other sites less frequent amebafree stools common hi h antibody titers Amebic Liver Abscess chocolatecolored pus necrotic material usually bacteria free lesions expand and coalesce further metastasis, direct extension or fistula Cutaneous Amebiasis intestinal or hepatic fistula mucosa bathed in fluids containing trophozoites perianal ulcers urogenital eg, labia, vagina, penis D. Diagnosis D.Intestinal stool examination To detect cysts and/or trophozoites by microscopy Or to detect antigen in stool specific E. histolytica lectin by ELISA. This differentiates histolytica from dispar Lower endoscopy to see lesions, take aspirate, or biopsy ii.Extraintestinal hepatic Serology to detect amobic lectin antigen or its antibodies Imaging CT, MRI, Sonar Abscess aspiration non suppurative reddish brown liquid full of trophozoites. Only applied on clinical cases to differentiate between amoebic and bacterial abscesses . Trophozoite imaging CT, MRI, Sonar They do not differentiate between bacterial and amoebic abscess . Precyst . Binucleate cyst. . Quadrinucleate cyst E.Treatment . Asymptomatic cyst pasers dilxanide furoate mg tds for days, iodoquinol or paromomycin mg tds for days endemic areas Mass treatment. . symptomatic metronidazole mg tds for days or tinidazole followed by lumenal agents dilxanide furoate mg tds for days . drain liver abscess only with high probability of rupture Amoebae E. histolytica F.Control Personal hygiene, Food sanitation proper disposal of human sewage. Pathogenic Free Living Amoebae Mohiedden M AbdulFattah Classification Schizopyrenida Amoeboflagellates Naegleria fowleri Acanthpodina Acanthamoeba culbertsoni. Ecology of Naegleria fowleri It grows fastest at oC, in water piped above ground, swimming and medicinal pools, acquarium, and in sewage. stages in the life cycle . Trophozoite is an amoeboid feeding stage Biology in the human host Naegleria is pathogenic to human host when gets access to him. Habitat in man brain tissues and meninges. Exit stage None, but trophozoites can be recovered from brain tissue biopsy and CSF. Flagellated form from CSF only. Three stages exist in its life cycle amoeboid trophozoite, flagellate and cyst. Cysts exist only in the environment . All stages are characterized by a single nucleus with a large karyosome and no visualised peripheral chromatin. . The ameboid transforms into a pearshaped flagellate with two flagella at the end if placed in distilled water or CSF . In desiccation or low nutrients, amoeboid encysts. . The cyst reverts back to trophozoite in favorable cases. . Cysts exist only outside human. Epidemiology Distribution freshwater habitats and rarely moist soil throughout the world. Human infections are quite rare and are acquired directly from the environment. Transmission No humantohuman transmission or vector transmission. . Intermediate host no . Reservoir host no . Infective stage Trophozoites. . Mode of infection During swimming in warm or heated waters, the trophozoites enter through the olfactory neuroepithelium in the nasal cavity migrate along the olfactory nerves into the brain. Hostparasite relationship Naegleria produces a fulminate, almost always fatal, acute meningoencephalitis primary amoebic meningoencephalitis PAM in healthy children and young adults. There is a rapid progression from headache and fever to coma, seizures and death. Diagnosis Unless diagnosed, treated early, infection is fatal. Cloudy CSF shows neutrophils, glucose, and proteins. Wet microscopy of CSF motile amoebae without bacteria. Biopsy from brain tissues stained by Wright or by monoclonal PAP stains may help, but it is almost always too late. Treatment only documented survivors Amphotericin B .mg/kg IV daily for d and mg/kg/d for d or intrathecally by lumbar catheter . mg for d then mg every other day for d. Health education to avoid bathing in .stagnant fresh water lake, .pools contaminated with sewage, .underchlorinated swimming pools. Chloramination, ammonia and chlorine to the water, is more effective in practice. control Acanthamoeba Acanthamoeba is group of amoebae unrelated to Naegleria, but also freeliving. It is infectious, causing two diseases .Granulomatous amoebic encephalitis GAE It occurs in immunesuppressed patients, usually secondary to infection elsewhere in the body e.g. skin ulceration. .Amoebic Keratitis AK is a severe corneal infection, among the immune competent hosts Biology It is free living, but can infects man Habitat in human nostrils and throats skin, lung tissues, and brain. Exit diagnostic stage No... But trophozoites and cyst can be found in histological sections No flagellated form. Morphology and life cycle Trophozoite um with spine like pseudopodia. Cyst double walled, polygonal or spherical um Epidemiology Distribution Throughout the world. .In soil fresh, brackish, and sea water sewage swimming pools .Contact lens equipment and in medicinal pools .Dental treatment units .Dialysis machines .Heating, ventilating, and air conditioning systems Transmission Transmission No humantohuman or vector transmission. Intermediate host no. Reservoir host no. Infective stage Trophozoites and cysts. Mode of infection The trophozoites and cysts can enter human through .eye, .nasal passages to the lower respiratory tract, or .through ulcerated skin .to CNS via blood. Host parasite relationship, continued Disseminated infections of various other tissues including lung pneumonitis and skin ulceration. In healthy individuals, The prominent disease is Acanthamoeba keratitis AK, A potentially sightthreatening eye infection, especially in patient with contact lens. In immune copromised Chronic granulomatous encephalitis GAE Autopsy of GAE The autopsy revealed extensive necrotizing granulomatous encephalitis with subependymal necroinflammatory process. Tissue section c of the brain were made and stained with HampE. Lesions in acanthamoebic infection Acanthamoebic skin ulceration Acanthamoebic keratitis Acanthamoebic granuloma in brain tissues Diagnosis . It is difficult . Amebas not yet detected in spinal fluid . Cysts and trophozoites are detected in brain biopsy GAE or in corneal scrapings keratitis. Treatment . Some success in treating amebic keratitis has been obtained with propamidine isethionate Brolene. . Surgery is often needed to correct the loss of vision. Control . Health education . Care of skin lesions, . use of sterilized saline for contact lens. Luminal flagellates Basic morphology and life cycle Urogenital flagellate Trichomonas vaginalis Intestinal flagellates small inrtestine Giardia lamblia Giardia lamblia A. Biology Final host man Habitat small intestine. Exit diagnostic stage Trophozoite and cyst. Basic morphology and life cycle B. Epidemiology of Giardiasis Distribution Worldwide, more prevalent in warm climates, and in children. Transmission. Intermediate host no. Reservoir host no. Infective stage cyst. Mode of infection By the ingestion of cysts in contaminated water, food, or by the fecaloral route hands or fomites, autoinfection . C. Giardiasis Hostparasite relationship Giardia never invade intestinal mucosa Asymptomatic infection to severe diarrhea and malabsorption. Acute infection develops after days and usually lasts to weeks Diarrhea, abdominal pain, bloating, nausea, and vomiting occur. Chronic infection Symptoms recur with malabsorption and debilitation. D. Diagnosis of Giardiasis Identification of cysts or trophozoites in the feces or in duodenal aspirate Enterotest. Detection of antigens in stool by ELISA, or parasites by immunofluorescence. E. Treatment of Giardiasis Metronidazole flagyl ,tinidazole Fasygin or Nitazoxanide cryptonaz. F. Control Environmental sanitation and personal hygiene Trichomonas vaginalis A. Biology Final host man Habitat In the female, lower genital tract and the male urethra and prostate. Exit diagnostic stage Trophozoite no cyst stage. Basic morphology and Life cycle B. Epidemiology of Trichomoniasis Distribution Worldwide. Higher prevalence among persons with multiple sexual partners. Transmission Intermediate host no. Reservoir host no. Infective stage trophozoite. Mode of infection By direct contact during sexual intercourse. C. Hostparasite relationship . In female Vaginitis with a purulent discharge is the prominent symptom. It can be accompanied by vulvar and cervical lesions, abdominal pain, dysuria and dyspareunia. . In men, the infection is frequently asymptomatic occasionally, urethritis, epididymitis, and prostatitis can occur. D. Diagnosis Detecting actively motile organisms in wet smears from vaginal, urethral or prostatic secretions. Direct immunofluorescent antibody staining more sensitive and Culture of the parasite most sensitive. for both parteners Metronidazole mg t.d.s. days, tinidazole gm single dose. Condom limits transmission. E. Treatment F. Control Hemoflagellates Leishmania Trypanosoma cruzi amastigote and promastigote Amastigote, trypomastigote Trypanosoma brucei and epimastigote epimastigote and trypomastigote Leishmania life cycle A. Biology of Leishmania organisms . . . . Organisms Old world cutaneous L.tropica, L. major New world cutaneous L mexicana New world mucocutaneousL. braziliense. Visceral L. donovani, and L. infantum Final host Man only in L.donovani and L. tropica. Man and animals in the others Habitat Reticuloendothelial cells of skin or viscera. Exit diagnostic stage Amastigotes within macrophages. Life cycle B. Epidemiology of Leishmania infection . Intermediate host vector phlebotomus old world and Lurzomyia new world. . Reservoir host arboreal mammal monkeys New.World. Rodents in African donovani and L. major. Dogs in L.infantum Transmission cycles Zoonotic in all except Indian L. donovani, and L. tropica. . Infective stage Metacyclic promastigotes regurgitated from pharynx . Mode of infection During vector feeding metacyclic promastigotes are regurgitated into the bite wound not in the salivary gland C. Hostparasite relationship . Ulcerative cutaneous lesions self healing, painless, nonpruritic ulcer dry tropica wet major. . Scaly non ulcerated lesions i. Anergic diffuse cutaneous L.mexicana and ethiopica with abundant amstigotes . ii. Hypersensitive leishmaniasis recidivans L. tropica with rare amstigotes. . Mucocutaneous lesion in of cutaneous leishmaniasis braziliense. . Visceral leishmaniasis Kalaazar fever, anaemia, hepatosplenomegaly in L. donovani. . Post kalaazar dermal leishmaniasis lesion that resembles leprosy. It occurs months or years after successful treatment D. Diagnosis of leishmaniasis Cutaneous types Detecting amastigotes in the raised border of the lesion and positive leishmanin skin test. Visceral type Detecting amastigotes in bone marrow, lymph nodes or spleen aspirates and serotesting to detect o specific IgG anti K antigen antiIgG , Intradermal leishmanin test is usually negative E. Treatment Pentostam mg/kg/d IM or IV for ds, Pentamidine mg/kg on alternate days for doses. Amphotericin B parenteral and orally aminosidine paromomycin. Protective clothing, insect repellents, insecticides and control of reservoirs. F. Control African trypanosomes Basic morphology and life cycle Trypanosoma brucei A. Biology Two organisms Trypanosoma gambiense in West and T. rhodesiense in East Africa Final host . Man and domestic animals for T. gambiense. . Game animals and sometimes man for T. rhodesiense. Habitat Blood lymphatics CNS vessels. Exit diagnostic stage Blood stream short stumby trypomastigotes Basic morphology and Life cycle Trypanosoma brucei life cycle B.Epidemiology Distribution T. gambiense in rainforest, riverine and lakes in West Africa. T. rhodesiense in dry bush and woodland in East africa Transmission Intermediate host vector o Glossina palpalis in West and G morsitans in East. Infective stage metacyclic trypomastigotes in saliva Mode of infection o Glossina injects saliva with metacyclic trypomastigotes into skin. o Congenital transmission and o Accidental lab inoculation are recorded. C. HostParasite relationship . . . The parasite in skin Chancre swelling in the bite site The parasite in blood fever and headache lymphadenopathy posterior cervical L.N. Winterbottom sign The parasite in CNS anorexia amp apathy severe sleep disturbance. neurological signs delayed pain sensation Kerandle sign. Coma and death. D. Diagnosis Detecting trypanosomes in blood, lymph nodes or spinal fluid CSF. o IgM in serum, CSF. E. Treatment Pre CNS o Pentamidine gambiense, or o suramin for rhodesiense amp gambiense CNS o Melarsoprol. o Difluoromethyornithine DFMO. F. Control Treat cases and reduce the vector American trypanosome Basic morphology and Life Lycle American trypanosomes Trypanosoma cruzi A. Biology Final host Man and armadillo. Habitat Free trypomastigotes in blood low parasitaemia and Intracellular amastigotes in spleen, liver, lymph nodes and muscles. Exit diagnostic stage o Blood stream short stumpy trypomastigotes Basic morphology and Life cycle o o Trypanosoma cruzi life cycle B. Epidemiology Distribution South and central America Transmission Intermediate host vector Kissing bugs Triatoma via infected feces Reservoir hosts various mammals Transmission cycles sylvatic and human cycles. Infective stage metacyclic trypomastogotes. Mode of infection . During vector feeding metacyclic trypomastigotes are released into feces. They enter via the bite wound near the mouth or the eyes. . Blood transfusion, . congenital, and . accidentally by ingestion of contaminated food C.HostParasite relationship Pathogenesis is parasite mediated damage, or by autoimmunity. Acute stage . Chagoma Rmana sign in the bite site periorbital edema and conjunctivitis few days postinfection and persists for months. . Fever, malaise, lymphadenopathy and/or acute myocarditis for months. Chronic stage o After decades of latency, it is manifested as cardiomyopathy and autonomic neural dysfunction megaesophagus and megacolon. D. Diagnosis Detecting trypanosomes . In blood smear, . In buffy coat layer during the acute stage. . In Culture NNN media. . By xenodiagnosis. . By PCR. Detection of specific serum IgG by Elisa in chronic stage. E. Treatment o o o Acute stage Nifurtimox mg/kg/h Po for ds or Benznidazole . mg/kg/h for ds. Chronic stage No specific drug in the chronic stage is useful. Treat symptoms. F. Control improve housing conditions. Insecticides. screening blood donors. Life cycle of Plasmodium Plasmodium species . . . . Benign malaria Plasmodium vivax tertian malaria Plasmodium ovale. Oval tertian malaria Plasmodium malariae quartan malaria malignant malaria Plasmodium falciparum malignant sutertian malaria .Final host Female Anopheles mosquitoes .Habitat in FH stomach lumen then stomach wall. .Exit stage from FH Sporozoites. .Exit stage from IH man diagnostic ring, schizont and gametocytes in all species except falciparum ring and gametocytes only. A. Biology B. Epidemiology Distribution Tropical and subtropical areas. Formerly throughout temperate areas. Transmission Intermediate host human. Commonly in liver cells and RBCs. Reservoir host None except P. malariae monkeys.. Infective stage sporozoites in mosquitos saliva or merozoites in RBCs. Mode of infection . mosquito injects sporozoites into blood vessels percutaneously. . Transmission of merozoite in RBCs via blood transfusion or transplacentally. C. Hostparasite relationship Clinical features Fever cold, shivers hot up to oC sweating hypopyrexia sleep. Anemia due to hemolysis and cytokine suppression on erythropoiesis severe in falciparum, Splenomegaly and hypersplenism anemia. Jaundice due to massive and repeated hemolysis severe in falciparum. Abortion, stillbirth in pregnant womenesp primigravidae infected with P falciparum. complications Falciparum malaria .cerebral malaria and death .Persistent anaemia exists because recrudescence of blood forms that survive the immune attacks .Algid malaria is characterized by rapid development of shock due to sudden hypotension and fall of temperature. .Blackwater fever It results from massive intravascular hemolysis and consequent hemglobinuria. Plasmodium vivax and ovale relapse up to years due to latent liver hynozoites. P. malariae glomerulonephritis and nephrotic syndrome. P. vivax Splenic rupture is rare complication but with high mortality . Hyperreactive malarial splenomegaly may develop with recurrent infections. D. Malaria diagnosis .Light microscopy of thin and thick blood films to detect ring, schizont and gametocytes in all species and only ring and gametocytes in falciparum species sensitive in field and specific .Rapid diagnostic strip or cassette format tests based on pLDH OptiMal. sensitive. It Differentiates flaciparum from others based on PfHRPII sensitive .Fluorescent microscopy Acridin orange AO stained thick blood film sensitive and specific .Quantitaive buffy coat QBC sensitive and gt specific Differentiation of plasmodium sp E. Treatment . Benign malaria Cloroquine base PO for days. If vivax/Ovale give primaquin for days after chloroquine to treat liver stage and prevent relapse. . Falciparum malaria If can swallow and has no complications, give quinine salt PO for d tetracycline, doxycyclin or clindamycin for days. If seriously ill take to ITU give quinine IV. F. Control . Avoid the major sources of infection mosquito. . Chemical prophylaxis chloroquine base or proguanil, PO. Take drug one week before travel and continue for weeks after return. Outline of Txoplasma life cycle A. Biology of Toxoplasma Final host Cats Habitat Intracellular in enteroepithelial cells of gut. Exit stage from FH Immature oocyst. No exit stage from IH Basic morphology and Life cycle B. Epidemiology of Toxoplasma Distribution Worldwide. . Transmission Intermediate host mammals including human. commonly in skeletal muscle, myocardium, and brain Reservoir host cats, rodents and domestic animals. Infective stage mature oocysts, tissue cysts, tachyzoites. Mode of infection .Ingestion of undercooked infected meat containing Toxoplasma cysts. .Ingestion of the oocyst from fecally contaminated food .Organ transplantation or blood transfusion. .Transplacental transmission. .Accidental inoculation of tachyzoites. C. Hostparasite relationship . Adymptomatic infection. . Fever and lymphadenopathy . . Encephalitis, acquired retinochoroiditis or pneumonitis in the immune compromised. . Congenital toxoplasmosis . abortion, stillbirth, hydrocephalus and/or congenital retinochoroiditis. The latter may manifest early or later up to years after birth. D.Diagnosis of toxoplasmosis Observation of parasites in LN biopsy. Isolation of parasites from blood BCL by intraperitoneal inoculation into mice. Detection of parasite genetic material by PCR, in congenital infections in utero. Serologic testing Acute infection is confirmed by by a fold rise in specific IgG antibody titer over weeks. IFA, ISAGA, IHAT and ELISA are the routine methods of diagnosis to detect specific IgM, IgG, IgE and IgA. Immunofluorescent antibody test IFA Positive test Negative test E.Treatment Often none is used except in . If the eye is involved or in the immunecompromized Pyrimethamine Daraprim for weeks, sulfadiazine. . Women with seroconversion during pregnancy spiramycin g/h daily for days. F.Control Avoid the two major sources of infection raw meat and cont. cat feces. Outline of Cryptosporidium life cycle A. Biology of Cryptosporidium species hominis and parvum Final host man and cattle Habitat intracellular extracytoplasmic within the brush borders of the enterocytes of whole GIT, biliary and respiratory epithelia. Exit diagnostic stage mature Oocyst asporocystic tetrazoic in human and calves feces. Basic morphology and Life cycle B. Epidemiology of Cryptosporidium Distribution About of the adult population in developed counties and in developing C. Transmission . Intermediate host no. . Reservoir host cattle in C parvum. No reservoir host in C. hominis. . Infective stage Oocyst. . Mode of infection Humantohuman fecaloral transmission. Animaltoperson transmission. Waterborne transmission C. Hostparasite relationship Incubation period of days The patient develops watery diarrhea, This may be associated with abdominal cramps and a lowgrade fever Stool microscopy Modified acidfast staining of stool shows redstained round oocysts against a bluegreen background. Antigendetection assays are more sensitive and include IFA assays, ELISA, and IC tests. Polymerase chain reaction PCR assays, more sensitive than others. D. Diagnosis of cryptosporidiosis E. Treatment Nitazoxanide Cryptonaz. For days with food F. Control Using a home microstraining water filter, to remove particles m in size.