* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Physics/Engineering Aspects of Medical Accelerators
Survey
Document related concepts
Transcript
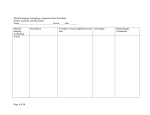
Physics/Engineering Aspects of Medical Accelerators January 9-11, 2013 Timothy J. Waldron, M.S. University of Iowa Hospital & Clinics Iowa City, Iowa, USA Med Accels Jan2013 Waldron D2 1 Physics/Engineering Aspects of Medical Accelerators, January 9-11, 2013 Day 2 1130 – Image Guided Radiation Therapy (IGRT) • • • • What is Image Guidance? Types of IG in RT Image formation and characteristics Example Systems Med Accels Jan2013 Waldron D2 2 Image Guided Radiation Therapy (IGRT) Short History Earliest External Beam Radiotherapy (i.e., Co-60, 250 kV) 2D (film) Imagery diagnoses. Clinical setup to bony landmarks and external anatomy Treatment of large volumes Non-isocentric treatment machines, “SSD techniques” Crude Beam Shaping “Portal Verification” Film portal verification not very useful if Co-60. • Large source size –geometric penumbra • Energy limited bone contrast • Solution to add kV imager to Cobalt machine Development of Medical Linear Accelerators (1960’s) Isocentric techniques Improvements in film imagery –intensifier cassettes for MV. Beam shaping with custom molded blocks Conventional simulators Med Accels Jan2013 Waldron D2 3 IGRT Short History (3) Development of “Conventional Simulator” (1970’s?) CT-based diagnostic imagery becoming available Med Accels Jan2013 Waldron D2 4 IGRT Short History (2) Development of “Conventional Simulator” (1960’s-1970’s?) CT-based diagnostic imagery becoming available Fluoroscopic/Film planning of beam arrangements using “Conventional simulators”- fluoroscopic and film based treatment planning. Computerized treatment planning at some institutions Positron Emission Tomography (PET) Development of other Technologies (1980’s) Magnetic Resonance Imaging (MRI) Computerized treatment planning widely available (PCs) Digital image processing for handling and manipulation of digitized films and CT images. Image segmentation Digital imaging in fluoroscopic and interventional use Med Accels Jan2013 Waldron D2 5 IGRT Short History (3) Use of “CT Simulator” (1990’s) CT-simulation 3D Computerized Treatment planning systems Growth of image registration algorithms Electronic Portal Imaging Devices (EPIDs) Multileaf Collimation Intensity Modulated Radiation Therapy (IMRT) Multi-modality Imaging (2000’s) PET/CT On Board Imaging (OBI) Cone Beam CT (CBCT) Magnetic Resonance Imaging (MRI) 4D Imaging and Gated Treatment Delivery Adaptive Radiation Therapy At what time was radiotherapy not “image guided”? Med Accels Jan2013 Waldron D2 6 Imaging Use in Radiation Therapy 3 Major Image Applications Simulation & Planning (CT, 4DCT, MRI, PET, MRSI, fMRI, US) Localization/Verification (CBCT, CT, MRI, CT, US, IR, Surface, etc.) Treatment/Response Monitoring (PET, MRI, MRSI, fMRI, CT) Med Accels Jan2013 Waldron D2 7 Imaging Use in Radiation Therapy Simulation and planning: Imaging data is collected with the patient in the treatment state with respect to immobilization and planned treatment devices. Images are transferred to the Treatment Planning System, where they may be combined with other modality images for organ delineation and beam planning. Ultimately a set of deliverable beam parameters and images for use in treatments are generated that will treat the target as designated by prescription. Simulation and planning may be performed once or more than once for a given course of treatment. These activites are usually not done in the treatment room. Imaging modes for simulation and planning are generally CT and often others such as PET and MRI. Med Accels Jan2013 Waldron D2 8 Imaging for Simulation and Planning Xray Computed Tomography (CT) CT imaging is the mainstay of patient data for simulation/treatment planning. Advantages: • • • • Fast acquisition (seconds) Geometrically accurate High resolution Good anatomic visualization • Data are useful for dose computation ( signal level correlates to electron density) • 3 dimensional data set • Compatible markers, immobilization aid in setup Med Accels Jan2013 Waldron D2 9 Imaging for Simulation and Planning Xray Computed Tomography (CT) Disadvantages: • • • • Patient Radiation Dose –Limit dose = limit signal Little or no biological function information High-Z artifacts; these also impede use for dose calculation. Limited soft tissue contrast Med Accels Jan2013 Waldron D2 10 Imaging for Simulation and Planning CT Disadvantages: Med Accels Jan2013 Waldron D2 11 Imaging for Simulation and Planning Magnetic Resonance Imaging (MRI) CT • • MRI Advantages: • • • T1 T2 No Ionizing Radiation Dose to Patient Good Soft Tissue Contrast High resolution (depends on magnet strength) Good anatomic visualization 3 dimensional data set Imaging for Simulation and Planning MRI Disadvantages: • Inductive heating, of both the patient and any metallic items in the patient. • Force on implanted metals, i.e. surgical clips. (Not all patients can be imaged). • Neurostimulation in very high fields. • Compatibility with markers, immobilization, etc. • Slow acquisition time, compared to CT • Geometric distortion inherent in image formation. • No functional biological information in standard images. • Image data not especially useful for dose calculations. Med Accels Jan2013 Waldron D2 13 Imaging for Simulation and Planning Position Emission Tomography (PET) and PET/CT PET Advantages: • Image set contains information about biological function, i.e.,F18DG provides sugar metabolism information. • If attenuation correction CT is used (PET/CT image set is and accurate 3 D model of uptake. Med Accels Jan2013 Waldron D2 14 Imaging for Simulation and Planning Position Emission Tomography (PET) and PET/CT PET/CT Disadvantages: • Resolution: Limited by range of positrons in tissue (~0.4 cm). • Sensitivity: Limited by injected activity/dose to patient. • Patient must be injected with radioactive tracer –dose. • Very long acquisition times. • Liquid radioisotope management/radiation safety issues may be problematic. Med Accels Jan2013 Waldron D2 15 Imaging for Simulation and Planning Combining Image Data Sets – “Image Fusion” Multiple types of imaging may be combined to aid in structure delineation in the treatment planning process. This is sometimes referred to as “image fusion”. When two image sets are “fused”, or co-registered, the secondary image data set is manipulated so that it is maximally match to the primary data set. The two data sets may then be viewed together or independently. Changes to the secondary set are normally “non-deformable”, meaning that they are limited to translation, rotation and magnification of the entire data set. No local changes are made. Typically for treatment planning, the CT image set is selected as primary data, both for geometric stability and dose calculation. MRI and/or PET/CT typically are selected as the secondary sets, but additional CT acquisitions might also be used. Med Accels Jan2013 Waldron D2 16 Imaging for Simulation and Planning Combining Image Data Sets – “Image Fusion” Note PET/CT data are inherently “fused”, but this is due to machine geometry. Imaging for Simulation and Planning Combining Image Data Sets – “Image Fusion” CT MRI PET/CT 3 DATASETS Slide from John Bayouth Imaging for Simulation and Planning The “output” data from Simulation and Planning1: Treatment Data Calculated Dose Distribution “Image” Machine treatment parameters: The set of data needed for the machine to deliver the calculated dose to the patient. • Couch, gantry collimator setting • MLC settings • Energy and MU settings • Et cetera Med Accels Jan2013 Waldron D2 20 Margins for target definition - Add to GTV to get clinical target volume (CTV) - For internal motion due to respiration, bladder filling, etc. - Accounts for spatial uncertainties in the radiation delivery process - Presence of organs at risk can decrease margin size (spinal cord, optic nerve, etc.) Figure from ICRU Report 62 (1999) Imaging for Simulation and Planning The “output” data from Simulation and Planning 2: Localization Localization Data are the mages and parameters necessary to accurately place the patient such that the pose and location of the target with respect to the treatment machine is consistent with the dosimetric treatment plan. Parameters • Couch and fiducial coordinates. • Patient marking notes and diagrams • Shifting instructions • Data for use with in-room localization tools, such as lasers and non-radiographic imaging systems. Med Accels Jan2013 Waldron D2 22 Images • 2D Digitally Reconstructed Radiographs (DRR). • Surface renderings from TPS • 3D Simulation/planning CT with delineated contours, fiducials indicated. DRR/Portal imaging example DRR Double-exposure EPID image Slide from Junyi Xia, Ph.D. Imaging Use in Radiation Therapy 3 Major Image Applications Simulation & Planning (CT, 4DCT, MRI, PET, MRSI, fMRI, US) Localization/Verification (CBCT, CT, MRI, CT, US, IR, Surface, etc.) Treatment/Response Monitoring (PET, MRI, MRSI, fMRI, CT) Med Accels Jan2013 Waldron D2 24 Imaging for Localization and Verification Now in the treatment room… Localization: The process (in the treatment room) of accurately placing the patient such that the pose and location of the target with respect to the treatment machine is consistent with the dosimetric treatment plan. (Each fraction). Verification: Radiographic confirmation of correct localization. Images collected in the treatment pose are compared with reference image data from treatment planning. This may be daily or less frequent, depending upon modality used. While localization may be performed using either radiographic or nonradiographic tools, verification is an inherently radiographic process. Med Accels Jan2013 Waldron D2 25 Imaging for Localization and Verification NonRadiographic Tools Treatment Room, Daily Coordinate transform from TPS to Tx room (isocenter). Verify tumor location unchanged from plan Beam data (MLCs, MU’s, Machine parameters) Med Accels Jan2013 Waldron D2 26 This seems to be where the “guidance” part comes in. • • • • • • • Lasers Light Field Gating Devices IR Tracking Surface Monitors RF Transponders Ultrasound Radiographic Tools • • • • • • • • Portal Films EPID CT on Rails CT Built In (Tomo) kV X-ray (2D) Stereoscopic kV X-ray kV CBCT MV CBCT Which of these are “image” tools? Non-Radiographic Image Guidance Tools (Systems acquire data in 2D or 3D, can be considered image guidance, even though images may or may not be presented to the user.) Advantage and Limitations • Can be used for maintenance of localization, generally after initial radiographic verification. + • No additional radiation dose to patient. + • Generally not significant machine modifications, potential for cost containment. + • Accuracy is ok when applied correctly. + • Variable level of “clearance” issues with couch, machine, room clutter, etc. ~ • No information about internal anatomy, so efficacy of any technology is site-dependent. • Non-radiographic tools cannot be used for initial verification of setup. Radiologic images are still necessary. Med Accels Jan2013 Waldron D2 27 Non-Radiographic Image Guidance Infrared (IR) light based systems Machine vision systems capable of measuring the location of emitters or markers whose pose and location are known with respect to the treatment room coordinate system (“Isocenter”). • Markers are placed on the patient at the time of CT and incorporated into the planning data set. • The coordinate transform from the CT coordinate system to the room coordinate system is computed and sent to the sensor computer in the treatment room. • The treatment room sensor is calibrated to isocenter, and when the patient is set up for treatment, the in-room sensor is used to localize the patient with relative accuracy (0.5-1 mm). Med Accels Jan2013 Waldron D2 28 InfraRed/Fiducial Stereo Position Sensor Example: NDI Polaris Moore et al, “Opto-electronic sensing of boyd surface topology changes during radiotherapy for rectal cancer, IJROBP 56:1 p248, 2003. IR/Fiducial Position Sensor NDI Polaris •This sensor is not an RT specific device but is present in RT products and other medical “navigation” systems. •Active or passive markers, singly or arranged in “tools” for 6DOF output. •Up to 60 frames per second, depending upon markers being tracked. •Volume of view: Domed cylinder approximately 1 m dia x 1 m long. •Accuracy: Manufacturer specifies 0.35 mm within the effective VOV, <0.2 mm in literature. 1m Patern Projection Stereo Correspondence (Image Feature Correspondence) •Another method to enhance image search space is via projection of patterned or structured light onto the scene. •A known pattern provides unique features for search and correlation. •Depending upon the geometry, apparent distortion of the projected pattern might also be used to compute distances. Images from: Siebert et al, “Human body 3D imaging by speckle texture projection photogrammetry,” Sensor Review 20:3, p 218, 2000. Patterned Light Projection Stereo Example VisionRT Ltd., ALIGNRT Stereo camera pair •RT Vision sensor system arranged in pods, each is capable of stereo “vision”. •A pod contains 1 stereo pair of cameras and a speckle pattern projector. flash •A texture camera and white flash are also present. •Phantom static accuracy <0.54 mm dev and 0.2° in computed 6DOF shifts. Static/dynamic accuracy in humans 1.02 ±0.51 mm upper thorax. (Schöffel et al 2007). Speckle projector Speckle Pattern Schöffel et al, “Accuracy of a commercial optical 3D surface imaging system for realignment of patients for radiotherapy of the thorax,” Phys. Med. Biol. 52 (2007) 3949-3963. Texture camera Patterned Light Projection Stereo Example VisionRT Ltd., ALIGNRT •Typically 2 pods are used in clinical installation, mounted lateral to couch to ensure full view of patient (~240°). •The psuedorandom speckle pattern is projected onto the patient during image acquisition. This pattern provides a set of defined “objects” in the image to facilitate the stereo search/correspondence process. •The illuminated surface positions are computed at approximately 5 mm spacing, and the combined model from the two pods is stored. Bert et al, “A phantom evaluation of a stereo-vision surface imaging system for radiotherapy patient setup,” Medical Physics 32:8, p.2753 (2005). Laser Line Projection Methods (Laser Triangulation Method) Laser spot in image at I(x,y) Laser line projected at P( x, ) CCD Camera Galvanometer – laser fan line scanning projector •Here, the invariant geometry is the camera-laser projector geometry and the projections of the laser as a function of time. •Under reference conditions, each pixel I(x,y) in the image can be associated with a laser projection P( ). x, •Apparent change in pixel location can then be related to surface distance from reference. Laser Line Projection Methods Laser spot in image at I(x’,y’) CCD Camera s D i (deflected ΔI) Laser spot projected at P x,( ) I z Galvanometer –laser fan line scanning projector •For surface displaced •Spota deflection, ΔI is related normally fromchange the reference by to the height z and the xspot ,canP(be z, the reflected laser overall geometry, and )computed now projects to a as different so long the pixel I(x’y’) in the image. incident angles and camerainterferometer geometry are well known. FS cos2 i I D S sin i cosi Moore et al, “Opto-electronic sensing of body surface topology changes during radiotherapy for rectal cancer, IJROBP 56:1 p248, 2003. Line Projection/Triangulation Example C-RAD Sentinel •The Sentinel device consists of a line scanning laser and CCD camera, pictured at right. •The projected laser fan beam incident angle is stepped via a galvanometer with approximately 1 cm pitch at the patient surface. •Each line step is captured and analyzed by searching the image for the laser line. •Since the incident angle for each line is known, the displacement from the reference is readily computed via triangulation. •Resolution/accuracy: Vertical resolution < 0.1 mm, transverse < 0.5 mm (Brahme (2008). Line Projection/Triangulation Example C-RAD Sentinel •Normal detection VOV 40x40x20 cm3. •Frame rate at full FOV ~1 fps. Higher rates available with reduced FOV. •Resolution/accuracy: Vertical resolution < 0.1 mm, transverse < 0.5 mm (Brahme (2008). Brahme et al, “4D laser camera for accurate patient positioning, collision avoidance, image fusion and adative aproaches during diagnostic and therapeutic procedures,” Medical Physics 35 (5) p. 1670 (2008). RF Transponder Marker-Tracking Systems Calypso System EM-excitable transponders Transponders can be located many times per second with better than 1 mm accuracy. Slide from Junyi Xia, Ph.D. Radiographic Image Guidance (In tx room) Radiographic Tools in IGRT Advantage and Limitations • Can be used for initial localization, verification and maintenance of localization. + • May provide information about internal anatomy. + • Useful for monitoring anatomic changes relative to tx plan + • Generally significant machine modifications, costly add-on • Radiographic tools deliver radiation dose to patient • Accuracy may also depend upon selected technology and anatomic site. ~ 2D Images: • Emulsion Films • kV and MV Electronic Imaging Med Accels Jan2013 Waldron D2 40 3D Image Data: • CT On Rails/In Room • kV and MV Cone Beam CT Portal imaging with film - Permanent record of beam's eye view - Film system used at UIHC (Kodak EC-L screen) - Megavoltage films inferior to kilovoltage films - As beam energy increases, contrast decreases Image from www.kodak.com Slide from Junyi Xia, Ph.D. Flat panel detector systems EPID image from: Hell E, et al, Nucl. Instrum. Meth. Phys. Res. A (2000) Slide from Junyi Xia, Ph.D. Indirect detection flat panel systems - Detectors sensitive to visible light - X-rays are converted to visible light in scintillator - Visible light scatters in scintillator, causing blurring Image from Bushberg et al, “The Essential Physics of Medical Imaging” (2002), p. 304 Slide from Junyi Xia, Ph.D. Direct detection flat panel imagers • No scintillator => no visible light scatter prior to detection • Direct detection system*: similar image quality as indirect, 55% less efficient • Direct detection system more sensitive to x-ray scatter from patient • Scatter sensitivity (direct) and visible light scatter (indirect) offset each other Image from Bushberg et al, “The Essential Physics of Medical Imaging” (2002), p. 304 *Partridge et al, Nucl. Instrum. Meth. Phy. Res. 484, 351-63 (2001): Slide from Junyi Xia, Ph.D. Flat panel detector array 40 cm, 1024 pixels Image from Bushberg et al, “The Essential Physics of Medical Imaging” (2002), p. 301 Slide from Junyi Xia, Ph.D. Flat panel readout - Detectors collect charge produced by radiation when switches open - When switches closed, charge goes out to digitizer through multiplexer Switches closed first Row of detectors read Switches closed second Row of detectors read Switches closed third Row of detectors read Image from Bushberg et al, “The Essential Physics of Medical Imaging” (2002), p. 301 Slide from Junyi Xia, Ph.D. Radiographic Image Guidance (In tx room) “3D” In-Room Imaging: Fan beam CT CT On Rails: Treatment couch modified to pivot patient from treatment location to CT location. CT then moves to scan patient on treatment couch. MVCT: Tomotherapy performs spiral CT acquisition using reduced energy (~4 MV) linac beam. Radiographic Image Guidance (In tx room) “3D” In-Room Imaging: Cone Beam CT Fan Beam CT: A narrow fan beam of radiation is used in conjunction with a row of detectors to acquire a “slice” of data each rotation. The patient is translated to collect a full data set. Cone Beam CT: A large field of radiation is used in conjunction with a 2D detector to acquire a full 3D data set in 1 rotation. Radiographic Image Guidance (In tx room) “3D” In-Room Imaging: Cone Beam CT kV CBCT: A kilovoltage (kV) x-ray source and image receptor are incorporated into the treatment machine, typically mounted orthogonal to the treatment beam. MV CBCT: A megavoltage beam is used (6X) with an electronic portal imaging panel to acquire data. Megavoltage cone beam CT (MVCBCT) • Treatment beam used for 3-D volumetric imaging • Flat panel with a-Si detectors used for acquisition • Streaking artifacts from high-Z materials reduced rel. to kVCT • Additional on-board imaging system not required Slide courtesy of Ryan Flynn, Ph.D. Video from Siemens Oncology Care Systems UNIVERSITY of IOWA Carver College of Medicine Megavoltage cone beam CT (MV CBCT) Helical kV CT • Images acquired using conventional equipment: Flat panel imager + 6 MV Tx beam • Imaging and treatment isocenters are the same MV CBCT • Streaking artifacts from high-Z materials reduced rel. to kVCT • Imaging dose trivial to model in treatment planning system and can be incorporated into Tx plan Slide courtesy of Ryan Flynn, Ph.D. Images from J. Pouliot UNIVERSITY of IOWA Carver College of Medicine Reduced high Z artifacts Kilovoltage fan beam CT Megavoltage cone beam CT Images from Jean Pouliot, UCSF Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Reduced high Z artifacts Image from Jean Pouliot, UCSF Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine MVCBCT Positioning System MVCBCT kVCT • An automatic image registration algorithm is applied following MVCBCT acquistion • kVCT used as a guide each day for MVCBCT patient positioning • User can then fine-tune the registration manually • User has freedom to select contoured structures to aid in process Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Day-to-day position of a single patient UNIVERSITY of IOWA Carver College of Medicine Spinal cord location over 5 fractions Images from Kevin Bylund, M.D. Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Daily MVCBCT workflow kVCT imaging Delineation Treatment planning Yes Correct for shift Correction required? MVCBCT Daily Imaging No, go to next Tx day No Daily Treatment Last Treatment? No, go to next Tx day Slide courtesy of Ryan Flynn, Ph.D. Yes Done with Treatment UNIVERSITY of IOWA Carver College of Medicine MVCBCT Shifts Correct Dose Errors Planned Uncorrected Corrected 70 Gy 75 63 56 45 30 20 Shifts: 0 mm Lateral -6 mm Anterior 4 mm Inferior Data from Ann Morris, M.D. Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine MVCBCT Shifts Correct Dose Errors Planned 70 Gy Uncorrected Corrected 75 63 56 45 30 20 Shifts: 0 mm Lateral -6 mm Anterior Data from Ann Morris, M.D. 4 mm Inferior UNIVERSITY of IOWA Carver College of Medicine Slide courtesy of Ryan Flynn, Ph.D. MVCBCT Shifts Correct Dose Errors Planned Uncorrected Corrected 75 Gy 70 63 45 56 30 Shifts: 0 mm Lateral -6 mm Anterior 4 mm Inferior Data from Ann Morris, M.D. Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Delivered doses to organs at risk match planned dose after shift correction Volume Fraction Spinal Cord CTV Planned: Uncorrected: Lt Parotid Rt Parotid Corrected: Dose (cGy) Data from Ann Morris, M.D. Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Plot from John Bayouth Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Plot from John Bayouth Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Plot from John Bayouth Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine MVCBCT Dose Management • Daily MVCBCT imaging dose calculated for all patients at UIHC – For pelvic cases, could be 5-10% of total dose • Imaging dose incorporated into 3D-CRT planning during prescription assignment • Imaging dose incorporated into optimization process for IMRT Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Treatment beam MVCBCT imaging dose Head and neck case 5.0 cGy 4.5 4.0 3.5 15.0 cGy 13.5 Prostate case 12.0 10.5 9.0 7.5 6.0 Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine Incorporating imaging dose into IMRT treatment plans • Imaging protocol is selected, and imaging dose is calculated • Inverse planning process is run with imaging dose as a baseline dose • Imaging beam functions as a treatment beam Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine MVCBCT treatment planning workflow for IMRT Cone Beam Imaging Dose Generate Optimized Plan 73 Gy Conventional Planning Method MVCBCT Dose Integration Method 10 Dose Actually Delivered >75 Gy 55 Ideal Plan, with zero imaging dose Dose (cGy): MVCBCT Imaging (10 cGy for this case) 60 Similar 70 Gy 9.0 8.0 7.0 +5-7 minutes calc time Slide courtesy of Ryan Flynn, Ph.D. UNIVERSITY of IOWA Carver College of Medicine CT Image Quality CT dose index (cGy) listed 1.5 kV CT (Siemens Somatom Emotion® ) 3.0 1.5 1.0 3.0 1.5 1.0 16.0 8.2 3.0 kV Cone Beam CT (Siemens Artiste® ) MV CT (TomoTherapy Hi-Art II® ) MV Cone Beam CT (Siemens Artiste® , using treatment beam) UNIVERSITY of IOWA Carver College of Medicine Images shown with permission from Simeon Nill, DKFZ MV CBCT and kV CBCT Significant difference between kV-based CBCT and MV-based CBCT • Image Quality MVCB Images tend to have poor high-Z (bony) contrast. This is due to the primary interaction of the photon beam with matter as Compton scatter. On the other hand, MV images tend to have better soft-tissue contrast than kVCB for the same reason. In general MV imaging is a low-efficiency signal process, so images tend to be “noisy”. MVCB beams may be accurately modeled in the TPS and the dose accounted for in treatment planning. • Equipment and QA kVCB imaging systems add a complete subsystem to the treatment machine. The kVCB has a separate, but hopefully coincident, isocenter from the treatment machine. Imaging Use in Radiation Therapy 3 Major Image Applications Simulation & Planning (CT, 4DCT, MRI, PET, MRSI, fMRI, US) Localization/Verification (CBCT, CT, MRI, CT, US, IR, Surface, etc.) Treatment/Response Monitoring (PET, MRI, MRSI, fMRI, CT) Med Accels Jan2013 Waldron D2 71 Imaging for Treatment Response and Monitoring Monitoring for changes to the patient that might influence dosimetric objectives. These may be expected or unexpected: Weight loss Depth to target/SSD Location of target Shape of target Some changes are fully expected responses to treatment, and typical regimens have multiple prescriptions (boost) based on etiology and expected tumor response. Some changes can be observed by treatment personnel, but some can only be observed with frequent radiographic imaging such as in-room CT. Even then, this triggers a return to Imaging for Simulation and Treatment Planning. (Welcome back) Imaging Use in Radiation Therapy 3 Major Image Applications Simulation & Planning (CT, 4DCT, MRI, PET, MRSI, fMRI, US) Localization/Verification (CBCT, CT, MRI, CT, US, IR, Surface, etc.) MOTION MANAGEMENT? Treatment/Response Monitoring (PET, MRI, MRSI, fMRI, CT) Med Accels Jan2013 Waldron D2 73