* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Bicalutamide Prescribing Guidance V2.0
Survey
Document related concepts
Transcript
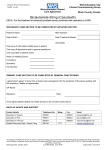
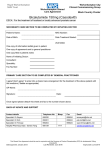
Doncaster & Bassetlaw Area Prescribing Committee February 2017 V2.0 Guidance for the Prescribing of Bicalutamide in the treatment of Prostate Cancer (Amber-G) 1.0 INTRODUCTION This document sets out guidance for the assessment and treatment of patients who are prescribed the antiandrogen Bicalutamide for the treatment of prostate cancer and delineated responsibilities when care for the patient is initiated in Secondary Care and transferred to Primary Care for continuation. It is intended to provide clear guidance to General Practitioners (GPs) and hospital prescribers regarding the procedures to be adopted when clinical (and therefore prescribing and financial) responsibility for a patient’s treatment on bicalutamide is shared between secondary and primary care. The decision to start a patient on treatment of carcinoma of the prostate should be taken by a Consultant Urologist. Green Traffic light system classification AmberA Amber-GAG RedR Drug Class Antiandrogen Bicalutamide Amber G (AG) – Drug must be initiated and titrated to stable dosage by specialist before GPs take over prescribing responsibility. Once medical condition and drug dosage is stable, there is no specific requirement for ongoing monitoring This guidance applies only for the indication for which the drugs are stated to be used for. It should not be used for other indications listed on the Doncaster & Bassetlaw APC traffic light system or for unlicensed indications for the drug. 1 This Document will be reviewed in the light of new or emerging evidence or by February 2022 Doncaster & Bassetlaw Area Prescribing Committee February 2017 V2.0 2.0 Background Information Cancer of the prostate usually responds to hormonal treatment aimed at androgen depletion. Standard treatments include bilateral orchidectomy, use of a gonadorelin analogue or anti-androgen such as bicalutamide. No entirely satisfactory therapy exists for disease progression despite this treatment (hormone-refractory prostate cancer) but occasional patients respond to other hormone manipulation e.g. with an anti-androgen as additional treatment in conjunction with an LHRH agonist. Bicalutamide may be used as monotherapy in advanced disease, or in conjunction with radiotherapy. 2.1 National Institute for Health and Clinical Excellence (NICE) In January 2014, the National Institute for Clinical Excellence (NICE) published a Clinical Guideline on the diagnosis and management of prostate cancer (CG175). NICE recommended that anti-androgens should be considered in men with metastatic disease as an alternative to LHRH agonist therapy in those wishing to preserve sexual function. Whilst not first line therapy, combined androgen blockade with LHRH agonist and bicalutamide may be rarely considered. It may be used as hormone treatment following failure of previous radical treatment for localised disease. 3.0 Prescribing Details Refer to Summary of Product Characteristics for full details at http://www.medicines.org.uk/emc/search 3.1 Dosage 1. Treatment of advanced prostate cancer as monotherapy, or in combination with radiotherapy, 150mg daily. 2. Treatment of advanced prostate cancer as part of combined androgen blockade (with orchidectomy or LHRH agonist), 50mg daily. 3.1 Administration Bicalutamide is taken orally as a single daily dose. There is no requirement to adjust the dose in patients with renal impairment or mild hepatic impairment. Increased accumulation may occur in patients with moderate to severe hepatic impairment, and therefore should be used with caution in these patients. 3.2 Adverse effects 2 This Document will be reviewed in the light of new or emerging evidence or by February 2022 Doncaster & Bassetlaw Area Prescribing Committee February 2017 V2.0 Bicalutamide is generally well tolerated, with a side effect profile of common reactions similar to placebo in large studies. Bicalutamide is metabolised by the liver and should be used in caution in patients with significant hepatic dysfunction. Elevated levels of transaminases and jaundice may occur, usually in the first few months of use. For this reason, baseline and 6 monthly liver function testing is required during treatment in addition to PSA monitoring. Expected anti antrogenic side effects include hot flushes, pruritis, decreased libido, breast tenderness and gynaecomastia. The latter is particularly common and may be ameliorated by the use of breast bud irradiation before starting bicalutamide treatment. 3.3 Monitoring Requirements Test: LFT’s – Baseline and 6 monthly Test: PSA – Baseline and as directed by Secondary Care Patients will be provided with blood forms by Secondary Care and attend the GP for the blood test 1 week prior to attending Secondary Care Outpatient appointment. Blood test results are interpreted by Secondary Care. 3.4 Drug Interactions Bicalutamide may potentiate the effect of warfarin. Close monitoring of the INR should be undertaken. Co-administration with terfenadine, astemizole or cisapride is contraindicated. (NB Terfenadine and cisapride are no longer available in the UK but may be available outside of the UK). Bicalutamide inhibits enzymes of the cytochrome p450 system, therefore caution is advised when co-administering enzyme inhibitors such as cimetidine and ketoconazole. Caution is also advised when co-administering bicalutamide with drugs metabolised predominantly by CYP 3A4. (ciclosporin, calcium channel blockers – these drugs may need dosage reductions and plasma ciclosporin levels should be monitored) 3 This Document will be reviewed in the light of new or emerging evidence or by February 2022 Doncaster & Bassetlaw Area Prescribing Committee February 2017 V2.0 4.0 ARRANGEMENTS All patients receiving bicalutamide will be under the ongoing care (minimum of 6 month review) of a Consultant Urologist or Clinical Oncologist. 4.1 Aspects of care for which Secondary Care Team is responsible Diagnosis and assessment Inform GP of the intention to start therapy Initiation of drug therapy Patient/guardian/carer education Ensure patient/guardian/carer is fully informed of potential benefits and side effects of treatment Ensure patient’s parents/guardian/carer is fully informed of the treatment (if required) Provide a comprehensive treatment package in addition to medications including appropriate information/monitoring sheet(s) Write to the GP after every clinic visit detailing whether the medication regime should remain the same or be changed. Specify any products / dose or frequency changes. Extra monitoring needed for dose changes will be organised by specialist team and conveyed to patient. Monitor side effects of medication. Monitor patient’s response to treatment Report adverse events via the Yellow Card reporting system in the BNF or at https://yellowcard.mhra.gov.uk/ 4.2 Aspects of care for which Primary Care Team is responsible Ensure that the patient/guardian/carer is clear what is being monitored and by whom Ensure that the patient/guardian/carer knows what significant adverse effects/events to report urgently and to whom they should report (specialist or GP) Confirm that proposed therapy is not contra-indicated because of concurrent therapy for other conditions the patient may be suffering from e.g. check drug-contraindications and drug-interactions. Contact specialist team if possible interactions found. Confirm the specialists have provided the patient/carer with appropriate information sheet(s) for monitoring and/or to alert other clinical staff to the treatment they are receiving. If appropriate information has not been provided by the specialist, the GP must ensure the information is provided Ensure patient’s parents/guardian/carer is fully informed of the treatment (if required) Monitor treatment as stated in the guidance Amend prescription as per requests from secondary care 4 This Document will be reviewed in the light of new or emerging evidence or by February 2022 Doncaster & Bassetlaw Area Prescribing Committee February 2017 V2.0 Confirm with specialist which changes in these or other parameters should trigger urgent referral back to the specialist Seek specialist advice promptly as advised in the guidance or if signs/symptoms of changes occur Report adverse events via the Yellow Card reporting system in the BNF or at https://yellowcard.mhra.gov.uk/ Report adverse events to the consultant sharing the care of the patient Stop treatment on advice of specialist, or immediately if intolerable side effects occur provided that it is safer to do so than to continue this therapy 4.3 Patient (or Carer’s) Responsibilities Discuss potential benefits and side effects of treatment with the specialist and GP. Identify whether they have a clear picture of these from the specialist and to raise any outstanding queries Check that where possible the specialists have provided a patient-held record or information sheet for monitoring and/or to alert other clinical staff to the treatment they are receiving Share any concerns they have in relation to treatment with the medicine Report any adverse effects to their specialist or GP whilst taking the medicine Report to the specialist or GP if they do not have a clear understanding of their treatment Participate in the monitoring of therapy and the assessment of outcomes, to assist health professionals to provide safe, appropriate treatment 5.0 REFERENCES NICE CG175 The diagnosis and management of prostate cancer January 2014 BNF 72 September 2016 Casodex 50mg Summary of Product Characteristics – revised February 2015 Casodex 150mg Summary of Product Characteristics – revised December 2015 Guidance Development Written By: Mr J Leveckis, Consultant Urological Surgeon, Doncaster & Bassetlaw Hospitals NHS Foundation Trust. January 2012 Reviewed By: Doncaster & Bassetlaw Area Prescribing Committee January 2012 Mr J Leveckis, Consultant Urological Surgeon Ms T Soar Urological Specialist Nurse Doncaster & Bassetlaw Hospitals NHS Foundation Trust February 2017 Approved by: Doncaster & Bassetlaw Area Prescribing Committee February 2017 5 This Document will be reviewed in the light of new or emerging evidence or by February 2022