* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Takayasu Arteritis Associated with Hyperlipidemia presented with
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
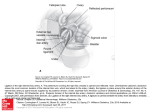
Takayasu arteritis associated with hypercholesterolemia presented with abdominal mass in a 9 Year-old boy: case report Alyaa Kotby1, Ola A Elmasry1, Omneya I Youssef1, Mervat G Mansour2, Abdul Rahman Shahein3 Address: 1 Division of Cardiology; 2 Pediatrics intensive care unit; Department of Pediatrics, Children’s Hospital of Ain Shams University, 38 Abbassia, Cairo, Egypt. 3 Department of Pediatrics, 555 University Avenue, Toronto, M5G 1X8, Canada. Corresponding author email address: [email protected] ABSTRACT Introduction: Takayasu arteritis (TA) is a large vessel granulomatous vasculitis that commonl y affects the thoracic and abdominal aorta with unknown etiology. The majorit y of TA occurs between 10 -40 years of age and present with hypertension and absent right radial pulse. Case presentation: We report a unique case of 9 year-old boy with angiogram proven Takayasu arteritis associated with hypercholesterolemia . The initial clinical manifestations included high erythrocyte sedimentation rate, right iliac fossa swelling and pulseless right lower limb. He responded to oral steroids and surgical resection of the aneurysm. Conclusion: The contribution of hypercholesterolemia in patients with TA is not known and sho uld be investigated. KEY WORDS: large vessel granulomatous disease, abdominal aorta, angiogram, hypercholesterolemia, aneurysm, iliac fossa, pulseless disease MANUSCRIPT TEXT Introduction: Takayasu arteritis was first diagnosed by a Japanese ophthalmologis t on the year 1908. It is now considered a world wide disease. Takayasu arteritis is a large vessel granulomatous vasculitis that commonl y affects the thoracic and abdominal Aorta with unknown etiology. The mechanism of arteritis has not been full y elucid ated to date but a non specific cell mediated inflammatory process that progresses to fibrotic stenosis of the aorta is widel y accepted [1]. The disease passes into earl y inflammatory pre -pulseless and late arterial occlusive pulseless phase. The inflamma tory stage usuall y presents with nonspecific low grade fever, tachycardia and easy fatigabilit y with hypertension and diminished upper extremities pulses. The most commonl y involved vessels include the left subclavian artery (50%), left common carotid arte ry (20%), brachiocephalic trunk, renal arteries, celiac trunk, superior mesenteric artery, and pulmonary arteries. Axillary, vertebral, coronary and iliac arteries are infrequentl y involved [2]. There have been many clinical reports of the disease and it s various associations. The association between Takayasu's arteritis and hyperlipidemia has not been described in the literature. In this case report, the first case of childhood Takayasu's arteritis in combination with h ypercholesterolemia is presented. Case Presentation : A 9 year-old white Caucasian Egyptian male child, the 4 t h born to consanguineous parents presented with gradual onset of non-radiating dull-aching pain in the right iliac fossa of one month duration. The pain increased with active movem ent of the limb and decreased with resting. There was neither history of trauma or back strain nor history of pervious operations or hernia s. The patient had no fever, tachycardia, chest pain, arthralgia, rashes or blurring of vision. Famil y history was fr ee of cardiac or renal troubles and antenatal period passe d smoothl y with normal records. Physical examination revealed diminished right femoral, popliteal and dorsalis pedis pulses with capillary perfusion from 2 -3 seconds. A deep oval swelling in right iliac fossa measuring 5 centimeters in diameter was palpated. The swelling was intra-abdominal, non-pulsating, firm in consistency and tender with no fixation to the skin or muscle. Blood pressure measured 111/72 (85 t h percentile) in the right upper limb. A comprehensive radiological and laboratory assessment were done in order to establish the diagnosis (Table 1). A color coded duplex examination of the right lower limb arterial system showed a partiall y thrombosed aneurysm of the right common iliac arter y with thrombus matter occupying 50% of the arterial lumen and turbulent flow in the rest of the lumen. The rest of the arterial system was all patent , showing biphasic flow pattern with average flow velocities and no evidence of arterial occlusion. Left renal artery duplex showed mild stenosis with acceleration of 2.4 M/sec (N: > 3M/sec) and normal resistive index of 0.37 (N :< 0.7). Electrocardiogram ( ECG) and chest X-ray were normal. Both right and left lower limbs deep venous systems were thrombosed. Contrasted computerized tomography and angiogram of the abdomen and pelvis showed right common iliac artery aneurysm displacing the right psoas muscle (Figure 1A and 1B). A decision was made to surgicall y resect and bypass the thrombosed aneurysm with saphenous graft. The limp perfusion and pain markedl y improvement after the surgery. MRSA grown upon culturing the revealed thrombus and was eradicated with intr avenous Vancom ycin 15mg/kg/dose q8hrs over 14 days . The patient was then maintained on oral antico agulant therapy (warfarin sodium 3mg/day) and cancelled his follow-up visits. One year later, he presented with a picture of heart failure due to hypertensive cardiomyopathy. Blood pressure measured 149/109 mmHg (> 95 t h percentile), 138/99 mmHg, 128/98 mmHg and 162/115 mmHg in right upper limb, left upper limb, right lower limb and left lower limb respectivel y. Echo cardiogram revealed left ventricular hypertrophy, stenosed abdominal aorta with normal flow and anatom y of the coronaries. The electrocardio gram (ECG) showed left heart axis deviation. Taking in consideration the patient’s past history a thorough examination with a (64) sixt y four multi -slice CT angiography for the aorta and both lower limb arteries showed multiple stenotic segments of the aor ta and brachiocephalic trunk with segments of relative dilatation. The left renal artery couldn’t be delineated with complete occlusion of the right common iliac artery (Figure 2). Lipid profile was done and repeatedl y showed mild hyperlipidemia although n ormal dietetic habits. Both erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were again elevated. Patient was then diagnosed to have Takayasu arteritis with an unusual presentation based on the previousl y described angiograms , hypertensio n and the markedl y elevated erythrocyte sedimentation rate . Discussion: Our patient first present ed with right iliac mass and pulseless right lower limb which was preliminary thought to be a thrombosed congenital right common iliac artery aneurysm. Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) at this time were explained by the on top infection. He improved after surgical resection and intravenous antibiotics . During the interim period between his first and second presentati on, the disease seems to continue evolving with blood pressure climbing up until precipitated heart fail ure (diastolic failure) . He was finally diagnosed with takayasu arteritis ( TA) in his second presentation and fulfilled the revised EULAR/PReS criteria for TA, given (1) aortic and renal narrowing on radiographic imaging, (2) undetectable right tibial pulses, and (3) hypertension [3]. The majorit y of TA cases occur between 10 -40 years of age [4]. The youngest age of presentation was reported by Weiss et al. about an eighteen month -old infant with TA proven by arterial autopsy and presented with cerebral aneurysm [5]. TA is more common in females with ratio varied from (6.6: 1) in Korea and (2.9: 1) in China as reported by Park et al [6] and Zheng et al [7] respectively. As a part of his work-up, fasting serum cholesterol level was done repeatedl y and showed a moderate elevation 293 mg/dL (N: < 200). Hypercholesterolemia couldn’t explain the above findings solel y. We suggested this increase to contribute with the ongoing inflammation affecting the major blood vessels with TA. But this explanation was not studied before. Parissis et al concluded in his study on a cohort of hypertensive patients who proved to have elevated inflammatory markers in their blo od that hypertension could induce an inflammatory process in blood vessels . He also added that the coexistence of hypercholesterolemia may enhance this inflammatory process . [8]. TA is usuall y treated by Corticosteroids to achieve remission. Although more than 50% of these patients flare with tapering [9]. There are case reports of treatment with methotrexate, azathioprine, infliximab adalimumab [12]. [10, 11] and The use of C yclophosphamide is reserved for severe s ystemic involvement and frequent relapses [13]. Once diagnosis of TA took place, the pati ent started on oral prednisolone (2mg/kg/day divided doses ) in order to control disease activit y. Blood pressure returned to the 75 t h centile on amlodepine, Carvidalol and spironolactone. His lipid profile no rmalized on diet control and atorvastatin (20 mg/day). Assessing response to treatment in takayasu arteritis is challenging. Prior studies have shown that clinical signs and symptoms of disease and elevated acute phase reactants are poorl y correlated with disease activit y. In the presence of hardware or clips from aneurismal repair, non -invasive studies such as magnetic resonance angiogram ( MRA) and computerized tomography angiogram ( CTA) are limited due to artifact. One recent report discussed the utilit y of non-invasive measurement of aortic arterial elastic properties with M -mode echocardiographic images in children with TA [14]. Furthermore, the optimal interval for serial imaging during remission is uncertain. Conclusion: A question should be raised: Could hypercholesterolemia play a role in Takayasu arteritis? ACKNOWLEDGMENTS I would like to express m y thankfulness and profound gratitude to m y famil y and m y father professor “Hussein Shahein” for his support. CONFLICTS OF INTEREST “The author(s) declare that they have no competing interests’'. SUPPORTING INFORMATION There are two echocardiographs showing the stenosed abdominal aorta below the diaphragm with a possibilit y of a plaque formation. REFERENCES 1. Lupi-Herrera E, Sanchez -Torres G: Takayasu's arteritis. Clinical stud y of 107 cases. Am Heart J 1977; 93(1): 94-103. 2. Numano F, Okawara M: Ta kayasu's arteritis. Lancet 2000; 356(9234): 1023 -5. 3. Ozen S, Ruperto N, Dillon MJ, Bagga A, Barron K, Davin JC, Kawasaki T, Lindsley C, Pett y RE, Prieur AM, Rave lli A, Woo P: EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides.” Ann Rheum Diseases 2006; 65(7):936-941. 4. Arend W, Michel B: The American College of Rheumatology 1990 criteria for the classification of Takayasu arte ritis. Arthritis Rheum 1990; 33(8): 1129 -34. 5. Weiss P, Corao D: Takayasu arteritis presenting as cerebral aneurysms in an 18 month old: A case report. Pediatrics Rheumatology Online J 2008 ; 6: 4. 6. Park YB, Hong SK, Choi KJ: Takayasu's arteritis in Korea: Clinic al and angiographic features. Heart Vessel – Suppl 1992; 7:55-59. 7. Zheng D, Fan D, Liu L: Takayasu's arteritis in China: A report of 530 cases. Heart -Vessel - Suppl. 1992; 7:32-36. 8. Parissis JT, Korovesis S: Plasma profiles of peripheral monocyte related inflammatory markers in patients with arterial hypertension correlations with plasma endothelin -1. Int J Cardiol 2002 ; 83(1): 13-21. 9. Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS: Takayasu arteritis. Ann Intern Med 1994 ; 120(11):919-929. 10.Della Rossa A, Tavoni A, Merlini G, Baldini C, Sebastiani M, Lombardi M, Neglia D, Bombardieri S: Two Takayasu arteritis patients successfull y treated with infliximab: a potential disease modifying agent? Rheumatology 2005 ; 44(8):1074-1075. 11.Jolly M, Curran JJ: Infliximab -responsive uveitis and vasculitis in a patient with takayasu arteritis. J Clin Rheumatology 2005 ; 11(4):213-215. 12.Tato F, Rieger J, Hoffmann U. “Refractory Takayasu's arteritis successfull y treated with the human, monoclonal anti -tumor necrosis factor antibody adalimumab.” Int Angiol 2005 ; 24(3):304307. 13.Ozen S, Duzova A, Bakkaloglu A, Bilginer Y, Cil BE, Demircin M, Davin JC, Bakkaloglu M: Takayasu arteritis in children: preliminary experience with cyclophosphamide induction and co rticosteroids followed by methotrexate. J Pediatrics 2007 ; 150(1):72-76. FIGURES AND FIGURE CAPTIONS Figure 1A Contrasted computerized tomography of the abdomen; a roughl y rounded heterogeneous right iliac soft tissue densit y mass lesion anterolateral t o L5 measuring 6x4x4 cm and displacing the right psoas muscle with breaking down and thrombosis of right iliac vein (arrowhead). Figure 1B CT angiogram of the abdomen and pelvis; right common iliac artery aneurysm (arrowhead). Figure 2 Multi-slice CT angi ography for the aorta; marked irregular thickening of the aortic wall affecting whole course of abdominal aorta, till just proximal to the origin of inferior mesenteric artery with multiple stenotic and relatively dilated segments (red arrowheads). Mild stenotic segments are also noted at the brachiocephalic trunk, right subclavian and both common carotid arteries (red arrowhead). Absent flow in righ t iliac artery (blue arrowhead) T AB LE S AN D T ABL E T IT LE Table 1: Results of laboratory evaluation of the pat ient