* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Control of Microorganisms
Traveler's diarrhea wikipedia , lookup
Trimeric autotransporter adhesin wikipedia , lookup
Human microbiota wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Portable water purification wikipedia , lookup
Antimicrobial surface wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Magnetotactic bacteria wikipedia , lookup
Microorganism wikipedia , lookup
Triclocarban wikipedia , lookup
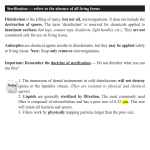
1 Unit -4 Control of Microorganisms Microorganisms present everywhere and since they cause contamination, infection and decay, it becomes necessary to remove or destroy them from the materials or places of work. This is the main objective of sterilization. The process of sterilization is important in microbiology to prevent contamination from extraneous organisms. Sterilization is essential in hospitals for maintaining asepsis, in food and drug manufacture to prevent microbial growth and also in laboratories for ensuring safety from contaminating organisms. The method of sterilization employed depends on the material which has to be sterilized and the purpose on which sterilization is carried out. Sterilization ids defined as a process by which an article, surface or medicine is made free of all microorganisms either in the vegetative or the sporing forms. The sterile object is totally free of viable microorganisms, spores and other infectious agents. Definitions of commonly used Terms: Disinfection: It is killing, inhibiting or removal of microorganisms that may cause disease. Disinfectants: These are agents, usually chemical, used to carry out disinfection. Sanitation: It is the reduction in the microbial population to the level that is considered to be safe by public health standards. Antisepsis: It is the prevention of infection or sepsis by killing or inhibiting the pathogen growth. Antiseptics: These are chemical agents applied to tissue. These are not as toxic as disinfectants. Germicide: A chemical agent which kills germs; most of pathogens but not endospores. Bactericide, Fungicide, Viricide and Algicide: Chemicals which kills bacteria, fungi, viruses and algae respectively. Bacteriostatic and Fungistatic: Chemicals which do not kill but prevent the growth of bacteria and fungi respectively. Methods of control of Microbial Growth. The various methods of sterilization that are employed to kill microorganisms can be broadly put into two categories: 1. Physical methods and 2. Chemical methods. The different physical agents are: 1. Sunlight 2. Drying 3. Heat 4. Filtration 5. Radiation 6. Vibration 7. Refrigeration , Freezing and Freeze –Drying. 8. Osmotic pressure 1. Sunlight: Sunlight possesses considerable bactericidal property and is useful in natural conditions. The killing effect is due to radiation like UV light and heat rays. Under natural conditions, the sterilizing capacity of sunlight varies according to circumstances. Direct sunlight when not filtered, by any impurities in atmosphere has an active bactericidal effect. 2. Drying: Moisture is essential for the growth of bacteria. Drying in air, is therefore has an inhibiting effect on bacteria as drying removes water that is required for growth of bacteria. Susceptibility to drying varies with different bacteria and also on conditions to which they are exposed to drying. 2 3. Heat: The most reliable method of sterilization and the factors influencing sterilization by heat include: a) Nature of heat b) Temperature and time c) Number of microorganism present d) Characteristics of microorganisms e) Type of material from which the organisms are to be eradicated. Dry heat is usually brings about death of organisms by oxidation of cell contents whereas the lethal effect of moist heat is due to denaturation and coagulation of proteins. i )Dry Heat : a) Flaming: Different materials used in microbiological laboratories such as forceps, scalpels are passed over the Bunsen burner for bringing about sterilization before use. b) Red heat: Inoculation loop or wires are usually made hot before it can be used for inoculation. c) Incineration: It is an effective method for rapidly destroying materials such as surgical dressings, animal carcasses and any other material used in hospital. It is usually done in a special device called incinerator. d) Hot- Air Sterilization: This is used where it is either undesirable or unlikely that steam under pressure will make direct contact with materials to be sterilized. Only dry articles such as glass wares, bandages, instruments, mineral oils, talcum powder may be sterilizes by this method. The apparatus used for this type of sterilization may be a special electric or gas oven. Objects are sterilized by dry heat ( hot air oven) when subjected to 171°C for 1 hour ,160°C for 2 hours or 121°C for 16 hours or longer depending on the volume. Picture No:1-Hot -Air Oven Picture No:2- Hot-Air oven Air Circulation Sterility Check Best suited for monitoring your dry heat & sterilization of fluid processes the Browne’s tube is a chemical indicator with a heat sensitive solution within a glass tube, which changes from red to green when the tube is subjected to a high temperature for the required length of time. It is a more reliable indicator of sterility than simple physical indicators such as tapes, as it shows both temperature and time. ii) Moist Heat: a) Pasteurization: This is mainly used for milk and other dairy products and temperature applied is either 63°C for 30 minutes (holder’s method) or 72°C for 15 seconds (flash Method). By this process all non sporing pathogenic organisms present in milk are destroyed. 3 b) Temperature at 100°C: Boiling: The vegetative forms are killed at 90-100°C but spore forming bacteria require considerable periods of boiling. Sterilization may be promoted by the addition of 2% sodium carbonate to the water. In cases where boiling is considered to be adequate , the material should be immersed in water and boiled for a period of 10-30 minutes. c) Steam at atmospheric Pressure ( 100°C ) : An atmosphere of free steam is used to sterilize culture media which may decomposed if subjected to high temperatures. Special devices such as Koch’s steam sterilizer or Arnold steam sterilizer can be used for sterilization. One exposure of 9 minutes usually ensures complete sterilization but for media containing sugars and gelatin, an exposure of 100°C for 20 minutes on three successive days is used. This is known as Fraction Sterilization or Tyndallization. The principle is that the first exposure kills all vegetative bacteria and spores present will germinate and be killed on subsequent exposures. d) Temperature above 100°C: This is commonly obtained by holding the steam under pressure in an instrument called Autoclave. Steam under pressure provides temperatures above those obtainable by boiling as shown in the table No:1 Picture No: 3 -Autoclave Picture No: 4- Cross view of Autoclave Table No:1 Temperatures of steam under Pressure Steam Pressure, Lb/in2 0 5 10 15 20 Temperature in °C 100 109 115 121.5 126.5 There are different types of autoclaves. It is essentially a double –jacketed steam chamber equipped with devices 4 which permit the chamber to be filled with saturated steam and maintained at a designated temperature and pressure for any period of time. In the proper use of autoclave, dry air from inside the autoclave is completely driven out by saturated steam. If air is present, it will reduce the temperature obtained within the chamber. In routine use of autoclave, the temperature of 121.5°C at 15 lb / in2 for 15 minutes is employed. This period is referred to as holding Period during which effective sterilization takes place. Many media, solutions, discarded cultures, and contaminated materials are regularly sterilizes with autoclave. In order to maintain optimum performance of autoclave in sterilizing the materials, sterility checks are done frequently. Sterility checks are done by using certain indicators. There are two types of indicators to check sterility. 1) Chemical indicator-this includes Bowie _Dick tape or Browne’s tubes and 2) Biological indicators- this contains spores strip of Bacillus stearothermophilus. The spore strip and an ampoule of medium are enclosed in a plastic vial. The vial is placed in the centre of the material to be sterilized and is autoclaved. Then the inner ampoule is broken, releasing the medium and the whole container is incubated. If no growth appears in the autoclaved culture, sterilization is considered effective. 4.Filtration: This is a method adopted to remove organisms from eat labile liquids. This is used for antibiotic solutions, serum preparations and carbohydrate solutions used in culture media. By this technique, one can obtain bacteria free filtrates. This method is also useful where separation of microorganisms is required which less in specimens. The different types of filters used have their own applications. Different types of filters are available with different porosity. Hence different types are used depending upon the puropose. Types of Filters a) Earthenware candle filter. Ex: Berkefeld and Chamberland filter Candle Type Filters: Berkefeld are made up of diatomatious earth or Kieselgarh. These filters are available in different pore sizes. The filters are in the form of hollow candle open at one end. Chamberland filters are porcelain filters available in various pore sizes. These are also hollow candles open at one end. Picture No: 5 –Candle filter. 5 b) Asbestos disc filter. Ex: Seitz filter: Thse are made of asbestos and chemically composed of magnesium silicate. These filters are usually in the forms of discs and are available in different pore sizes. c) Sinter glass filter: These are made of finely ground glass which are then made to fuse. They are also available in different pore sizes. d) Collodion or Membrane filter: These are usually made of nitrocellulose and have precise pore sizes from 25μm 0.025 μm. Advantages of these filters are, they relatively inexpensive ,do not clog easily and can filter large volumes of fluid rapidly. They can be autoclaved. Disadvantages are that they allow viruses and mycoplasmas to pass through and absorb relatively large amounts of the filtrate and may introduce metallic ions into the filtrate. Membrane filters are used to sterilize materials likely to be damaged by heat sterilization. Materials like special nutrients that are added to culture media, sera, drugs, and vitamins are regularly filtered through membrane filters. Cellulose acetate filters with extremely small pore size are used in removing viruses from liquids. Membrane filters are used to trap bacteria from air and water sample can be transferred directly to agar plates and the quantity of bacteria can be determined. Picture No: 6- Membrane Filter. e) Isopore Filters: The Isopore membrane is a polycarbonate, track-etched screen filter recommended for all analyses in which the sample is viewed on the surface of the membrane. Isopore membrane offers distinct 6 advantages for the analysis of airborne contaminants and other particles using optical or electron microscopy. The Isopore membrane is composed of polycarbonate film, which has a smooth, glasslike surface for clearer sample observation. The unique manufacturing process of the membrane ensures a precise pore diameter and a consistent pore size for accurate separation of samples by size. Isopore membranes do not stain resulting in low background interference. Clearing is not necessary for most transmitted light microscopy. Matched-weight filters are not usually required because of low, constant tar and ash weights. Isopore membranes are non-hygroscopic, which permits rapid drying and reduced sample analysis time. The Isopore™ membrane is a polycarbonate, track-etched screen filter recommended for all analyses in which the sample is viewed on the surface of the membrane. Isopore™ membrane offers distinct advantages for the analysis of airborne contaminants and other particles using optical or electron microscopy. The Isopore™ membrane is composed of polycarbonate film, which has a smooth, glass-like surface for clearer sample observation. The unique manufacturing process of the membrane ensures a precise pore diameter and a consistent pore size for accurate separation of samples by size. Matched-weight filters are not usually required because of low, constant tar and ash weights. Features & Benefits Membrane structure retains particles on the surface, simplifying counting and analysis Isopore™ membranes do not stain, resulting in low background interference Non-hygroscopic, allowing for rapid drying and reduced sample analysis time Translucent material does not require clearing for transmitted light microscopy; also available in brown variety Applications Air Monitoring, Epifluorescent Microscopy, Chemotaxis Assays f) High-efficiency particulate air filters ( HEPA ): These are used in the ventilation systems of areas where microbial control is especially important ,such as operating rooms, burn units, and laminar flow transfer units in laboratories. These filters remove all organisms larger than 0.3 μm in diameter. Picture No:-7- HEPA Filter. 7 5. Radiation: Four types of radiation-ultraviolet light, ionizing radiation, microwave radiation and in some case strong visible light can be used to control microorganisms. i) Ultraviolet ( UV ) light: UV light consists of wavelength between 40 and 390nm,but wave length in the 200 nm range are most effective in killing microorganisms by damaging DNA and proteins. UV light is absorbed by nitrogen bases of DNA causing permanent damage to the DNA molecules thus resulting killing effect of bacteria. UV light also inactivates viruses. However, bacteria have DNA repair mechanisms which minimize the damage to bacterial cells by UV light. UV light does not penetrate glass, cloth, paper or most other materials and it does not reach corners and crevices of laboratory surfaces and materials thus limiting its use. ii) Ionizing Radiation: X rays which have wave length of 0.1 to 40nm and gamma rays which have even shorter wavelengths are forms of ionizing radiation. These cause ionization of molecules when they hit them resulting in death of microorganisms and viruses. Ionizing radiation damages DNA and produce peroxides which act as powerful oxidizing agents in cells causing death. Ionizing radiations are used to sterilize plastic laboratory and medical equipment and pharmaceutical products. iii) Microwave Radiation: This radiation fall at the longer wavelength end of electromagnetic spectrum with the wave length of approximately 1mm to 1 m. Microwave oven frequencies are turned to match energy level in water molecules. In the liquid state, water molecules quickly absorb the microwave energy and then release it to surrounding materials as heat. Specialized microwave oven is available now that can be used to sterilize the medium in just 10 minutes. iv) Strong visible light: It has bactericidal property because of UV rays in sunlight. Strong visible light which has wave length from 400 to 700 nm can oxidize light sensitive molecules such as riboflavin and porphyrins.The fluorescent dyes eosin and methylene blue can be denature proteins on the presence strong light. Therefore the combination of a dye and strong light can be used to rid materials of both bacteria and viruses. 6. Vibrations: Sonic or sound waves in the audible range can destroy bacteria if waves are of sufficient intensity. Ultrasonic waves or waves with frequencies above 15,000 cycles per second can cause bacteria to cavitate ( formation of partial vacuum in a liquid). Bacteria so treated disintegrate and their proteins are denatured. The disruption of cells by sound waves is called sonication. Neither sonic nor ultrasonic waves are a practical means of sterilization. 7. Refrigeration, Freezing and Freeze –Drying: Cold temperatures retard the growth of microorganisms by slowing the rate of enzyme –controlled reactions but do not kill microbes. Refrigeration of foods at 5°C prevents spoilage from microorganisms. However, the storage should be limited to a few days as some bacteria and fungi continue to grow at this temperature. Freezing at -20°C is used to preserve foods in homes and in food industry. Although freezing does not sterilize foods, it does significantly slow down the rate of chemical reactions so that microorganisms do not cause food to spoil. Freezing at much lower temperature can also be used to preserve microorganisms. Microorganisms are suspended in glycerol or protein to prevent the formation of ice crystals, cooled with solid carbon dioxide to a temperature of -70°C and then held there or they can be placed in liquid nitrogen and cooled at -180°C. Freeze drying or lyophilization is the drying of a material from frozen state. This process is used in the manufacture of some brands of instant coffee which retains more natural flavor than other kinds. Microbiologists use lyophilization for long term preservation of cultures of microorganisms. Organisms in vials are rapidly frozen in alcohol and dry ice or in liquid nitrogen, are then subjected to a high vacuum to remove all water while in the frozen state and finally sealed 8 under vacuum. Organisms thus treated can be kept alive for years, stored under vacuum in the freeze-dried state. 8. Osmotic pressure: High concentration of salt, sugar or other substances creates a hyper osmotic medium which draws water from microorganism by osmosis. Plasmolysis or loss of water severely interfere with cell function and eventually leads to cell death. The use of sugar in jellies , jams and syrups or salt solution in curing meat and making pickles plasmolyzes most organisms present and prevents growth of new organisms. A few halophilic organisms grow even in such conditions and spoil the food stuff. 9 Summary of Properties of Physical Antimicrobial Agents-Table -2 Agent Action Use Dry heat Denatures proteins Oven heat is used to sterilize glassware and metal objects; open flame used to incinerate microorganisms. Moist heat Denatures proteins Autoclaving sterilizes media, bandages and many kinds of hospital laboratory equipment not damaged by heat & moisture; pressure cooking sterilizes canned foods. Pasteurization Denatures proteins Kills pathogens in milk, dairy products and beer. Refrigeration Slows the rate of enzymecontrolled reactions Greatly slows the rate of enzyme- controlled reactions Inhibits enzymes Used to keep fresh foods for a few days; does not kill most microorganisms. Freezing Used to keep fresh foods for several months; does not kill microorganisms; used with glycerol to preserve microorganisms. Drying Used to preserve some fruits and vegetables; sometimes used with smoke to preserve sausage for years. Freeze-drying Dehydration Inhibits Used to preserve microorganisms for years; used to enzymes manufacture some instant coffees. Ultraviolet Denatures proteins Used to reduce the number of microorganisms in light & nucleic acids air in operating room, animal rooms and where cultures are transferred. Ionizing Denatures proteins Used to sterilize plastics and pharmaceutical radiation & nucleic acids products and to preserve foods Microwave Absorbs water Can not be used reliably to destroy microbes except radiation molecules, then in special media sterilizing equipment. releases microwave energy to surroundings as heat Strong visible Oxidation of light- Can be used with dyes to destroy bacteria and light sensitive materials viruses; may help sanitize clothing. Sonic and Cause cavitation Not a practical means of killing microorganisms but ultra sonic useful in fractionating and studying cell waves components. Filtration Mechanically removes Used to sterilize media, pharmaceutical products membranes microbes and vitamins, in manufacturing vaccines and in sampling microbes in air and water. Osmotic Removes water from Used to prevent spoilage of foods such as pickles pressure microbes and jellies. 10 Chemical Antimicrobial Agents There are a wide variety of chemical agents available to control growth of microorganisms. Several qualities should be considered in deciding which disinfectant to use. An ideal disinfectant should have the following characteristics: 1. Be fast acting even in the presence of organic substances, such as those in body fluids. 2. Be effective against all types of infectious agents. 3. Easily penetrate material to be disinfected without damaging or discoloring material. 4. Be easy to prepare and stable even when exposed to light, heat or other environmental factors. 5. Be inexpensive and easy to obtain and use. 6. Not have unpleasant odor. Since not a single disinfectant meets all conditions, the one that meets the greatest number of criteria is often chosen for disinfection. Conditions That Affect the Efficiency of Antimicrobial agents Destruction and inhibition of microorganisms depend on the factors: 1. Population Size: A larger population needs a longer time to be killed than a smaller one. 2. Population Composition: The nature of organisms subjected to sterilization determines the effectiveness of the agent used for sterilization. Endospores of bacterial are hard to kill and are more resistant to disinfection, heat and radiation. Bacteria like Mycobacterium tuberculosis are more resistant to antimicrobial agents. 3. Concentration and intensity of an antimicrobial agent: Many a times, a high concentration of chemical agent or an intensive physical process kills organisms rapidly. Some times an agent is more effective at lower concentrations. For example, 70% ethanol is more effective than 95% . 4. Duration of exposure: More organisms are killed when they are exposed to a longer duration. 5. Temperature: An increase in temperature at which a chemical acts often enhances its activity. 6. Local environment: Local conditions in which microorganisms present affect their killing property. Organisms in a low acidic (Low pH) conditions are killed easily than those in present high pH conditions. Organic matter protects organisms against heating or disinfectants. Therefore, objects are to be cleaned before they are subjected for sterilization. Mechanisms of Action of Chemical Chemical antimicrobial agents kill microorganisms by participating in one or more chemical reactions that damage cell components. The different reactions are grouped whether they affect proteins, membranes or other cell components. 1. Reactions that affect Proteins: Most antimicrobial agents when used in a strong enough concentrations over a period of sufficient time denature proteins permanently killing microorganisms. Reactions that denature proteins include hydrolysis, oxidation and the attachment of atoms or chemical groups. 2. Reactions that affect Membranes: Membranes contains proteins and so can be damaged by the reactions as mentioned earlier. Membranes also contain lipids and can be disrupted by the substances that dissolve lipids. Surfactants are soluble compounds that reduce surface tension. Ex: soaps and detergents. Phenols dissolve lipids and denature proteins. 3. Reactions that affect other cell components: Other cell components affected by chemical agents include nucleic acids and energy producing sysyems. Alkylating agents can replace hydrogen on 11 amino or alcohol group in nucleic acids certain dyes, such as crystal violet, interfere in cell wall formation. Lactic acid and Propionic acid inhibit fermentation and prevent energy production in certain bacteria. 4. Reactions that Affect Viruses: Inactivation of viruses is effected by destroying either the viruses’ nucleic acid or their proteins. Alkylating agents, such as ethylene oxide, nitrous acid and hydroxylamine damage DNA or RNA. Detergents and alcohols and other agents that denature proteins act on bacteria and viruses in the same way. Dyes like acridine orange and methylene blue make viruses susceptible to inactivation when exposed to visible light. Major Groups of Chemical Antimicrobial Agents 1. Phenol and phenolic compounds 2. Alcohols 3. Halogens 4. Heavy metals and their compounds 5. Dyes 6. Detergents 7. Quarternary ammonium compounds 8. Aldehydes 9. Gaseous agents 1. Phenol and phenolic compounds: Phenol and phenolic compounds are very effective disinfectants. A 5% aqueous solution of phenol rapidly kills the vegetative cells of microorganisms; spores are much resistant. Antimicrobial activity is enhanced by the addition of chemical substitution in the phenol ring structure. Hexylresorcinol, a derivative of phenol is a solution of glycerin and water and it is a strong surface –tension reductant which has high bactericidal property. Practical Application: Phenolic substances may be either bactericidal or bacteriostatic depending upon the concentration used. Bacterial spores and viruses are resistant The antimicrobial activity is reduced at an alkaline pH , by organic material, presence of soap and low temperature. Aqueous solutions of 2 to 5% can be used to disinfect materials like sputum, urine, feces, and contaminated instruments or utensils. Derivates of phenol diluted in detergents are use din many antiseptic and disinfectant preparations. o-phenylphenol is a combination of phenol and detergent. Mode of Action: Cause disruption of cells, precipitation of cell protein, and inactivation of enzymes and leakage of aminoacids from the cells. Lethal effect is associated with physical damage to the membrane structures in the cell surface. 2. Alcohols: ethyl alcohol,CH3CH2OH, in concentration between 50 and 90% is effective against vegetative or nonsporing cells. 70% concentration of alcohol is generally used. Ethyl alcohol is ineffective against bacterial spores. Methyl alcohol is less bactericidal and more over it is toxic for personnel. The higher alcohols –propyl, butyl, amyl and others are more germicidal and germicidal power of alcohols increases with increase in their molecular weight but since they are not miscible with water, they are not generally used. Practical Applications: Used to reduce the surface microflora of skin and for disinfection of clinical oral thermometers. Mode of Action: Alcohols denature proteins and damage lipid complexes in the cell membranes. They are also dehydrating agents. 3. Halogens: 12 a) Iodine: Iodine is one the most effective germicidal agents. Traditionally it is used as tincture of iodine several preparations are: 2% iodine plus 2% sodium iodide diluted in alcohol, 7% iodine plus 5%potassium iodide in 83% alcohol and 5% iodine and 10% potassium iodide in aqueous solution. Iodophores are mixtures of iodine with surface active agents which act as carriers and solubilizers for the iodine. They are nonstaining and low irritant. Eg: Polyvinypyrrolidone (PVP-I) complex from which iodine is released slowly . Practical Application: Used mainly as the best skin disinfectant ,used for disinfection of water ,air, (iodine vapors) and sanitization of food utensils. Mode of Action: Oxidize essential metabolic compounds such as proteins with sulfhydryl groups. The action, ay also involve the halogenation of tyrosine units of enzymes and other cellular proteins requiring tyrosine activity. b) Chlorine and Chlorine Compounds: This either in form of gas or in certain chemical combinations is most commonly used disinfectant. The compressed gas in liquid form is used in large scale operations such as water purification plants. The convenient forms of Chlorine for use are hypochlorite- calcium hypochlorite, Ca(Ocl2) and Sodium hypochlorite, NaOCl. Chloramines are used as disinfectants, sanitizing agents or antiseptics. Chemically it has one or more of the hydrogen atoms replaced with chlorine in an amino group of a compound. Eg: Monochloramine and Azochloramide. These are more stable than hypochlorite and releases chlorine for a prolonged period. Practical Application: Chlorine compounds are widely used in water treatment, in food industry, for domestic use and in medicine. Products containing calcium hypochlorite are used for sanitizing dairy equipment and eating utensils in restaurants. Solutions of Sodium hypochlorite of a1% concentration are used for personal hygiene and as a household bleaches and disinfectants. Higher concentrations of 5 to 12% are used as house hold bleaches and disinfectants Chorine compounds are also used to disinfect open wounds, to treat athlete’s foot, to treat other infections and as a general disinfectant. Mode of Action: The antimicrobial action is due to hypochlorous acid formed when free chlorine is added to water: Cl2 + H2O HCl + HClO (hypochlorous acid) Hypochlorite and Chloramines under go hydrolysis with the formation of hypochlorous acid. The hypochlorous acid formed in each case is further decomposed: HClO HCl + O The nascent oxygen released in this reaction is a strong oxidizing agent and through its action on cellular constituents, microorganisms are destroyed. The killing effect is also partially due to the direct combination of Chlorine with proteins of the cell membranes and enzymes. 4. Heavy metals and their compounds: Heavy metals like Mercury, Silver and Copper either in combination or alone in certain compounds bring about detrimental effects upon microorganisms. 13 Table-3 -Con’d Mercury Silver Copper Organic compounds: Mercurochrome Metaphen Merthiolate Murcresin Colloidal silver compounds: Silver nitrate Silver lactate Silver picrate Less irritating and less toxic that inorganic forms; employed as antiseptics on cutaneous and mucosal surfaces; may be bactericidal or bacteriostatic. Copper sulfate Most effective against algae and molds.2 ppm in water prevents algal growth, used in swimming pools and open water reservoirs; used in the form of Bordeaux mixture against fungal diseases to plants. Used as antiseptics, silver nitrate at concentration of 1:1000 dilution is bactericidal and used in few drops for the eyes of new born babies to prevent ophthalmia neonatrum and gonococcal infection. Mode of Action: These compound combine with cell proteins and inactivate them. Mercuric chloride act upon sulfhydryl group of enzyme. 1 High concentrations of salt of heavy metals coagulate cytoplasmic proteins and precipitate causing death to the cells. 5. Dyes: There are two categories of dyes having antimicrobial property. They are: a) Triphenylmethane and b) Acridine Dye. a) Triphenylmethane: It included dyes like malachite green, brilliant green and crystal violet. Genrally Gram-positive organisms are easily killed by these dyes than Gram-negative ones. Crystal Table-3 Heavy metal Mercury Example of Compound Inorganic compounds: Mercuric Chloride Mercurous chloride Mercuric oxide Ammoniated mercury Application Bactericidal in dilutions 1:1,000;limited use due high toxicity, reduction in effectiveness in presence of organic material; insoluble compounds, used in ointments as antiseptics. Con’d 14 violet is effective at the concentrations of 1:200,000 to 1:300,000.Malachite green is effective against Staphylococcus aureus at the concentration of 1:1000, 000. Practical Application: These dyes in low concentrations are included in certain culture media to inhibit the growth of Gram-positive bacteria. Species of Brucella bacteria can be identified based on their resistance pattern to several dyes. Mode of Action: It may interfere in cellular oxidation process. b) Acridine Dye: There are two derivatives of acridine dye. It include 1) Acriflavine and 2)Tryptoflavine. These have selective inhibition against Staphylococci and Gonococci bacteria. Used in treatment of burns and wounds. 6.Detergents: These are surface –tension depressants, or wetting agents used mainly for cleaning purposes. Soap is a poor detergent in hard water. Synthetic detergents used in laundry, dishwashing powders, shampoos are superior to soaps as they do not precipitate in alkaline or acid water, do not produce deposits with minerals in hard water. Chemically detergents are classified in to: 1) anionic detergents; which ionize into anion with detergent property. Ex: Sodium lauryl Sulfate, 2) Cationic detergents; which ionize into cat ion with detergent property. Ex: Cetylpyridinium chloride ( Ceepryn), 3) Nonionic detergents which do not ionize. Practical Application: General cleaning, laundry, household dish washers. Mode of Action: Soaps and detergents reduce surface tension of water and increase wetting property of water in which they dissolved. Soap water can emulsify and dispense oils and dirt. Microorganisms become enmeshed in the soap lather and are removed by rinse water. 7.Quaternary Ammonium Compounds: Ex: Cetrimide & Diaparene Chloride : These are cationic detergents having superior antimicrobial properties. They have chemically four carbon groups (R1,R2, R3 & R4 ) linked to the nitrogen atom and R group may be any of the alkyl groups. The bactericidal power of quaternaries is extremely high for Gram –positive bacteria while they are fairly effective against Gram-negative and fungi. These have low toxicity and high solubility, stability in solution and noncorrosiveness and therefore make them ideal antimicrobial substances. Practical Application: Used as skin disinfectants, as a preservative in ophthalmic solutions and in cosmetic preparations. Used widely in hospitals to disinfect surfaces, food processing plants and as sanitizers of utensils in restaurants. Mode of Action: These cause denaturation of proteins, interfere in glycolysis and damage to cytoplasmic membrane, alter permeability of cell structures. 8. Aldehydes: These are low molecular weight compounds with general formula RCHO and have most effective antimicrobial; even sporicidal property. Two classes of compounds include a) Formaldehyde and b) Glutaraldehyde. a) Formaldehyde (HCHO): It is a solid substance at room temperature but a stable gas only at elevated temperature and in high concentrations. Paraformaldehyde is a colorless substance which gives formaldehyde upon heating. Formaldehyde is available in a aqueous solution as formalin, which contains 37 to 40 % formaldehyde. Fumes of formaldehyde are noxious and irritating to tissues and eyes. Practical Application: Formaldehyde in solution is useful for sterilization of instruments and in gaseous form for disinfection and sterilization of enclosed areas. Vaporization of formaldehyde into an enclosed area for adequate time at room temperature and humidity of 60 to 80 % is commonly employed for sterilizing enclosed areas. Mode of Action: Formaldehyde combines readily with proteins and nucleic acids damaging them resulting in death of organisms. 15 b) Glutaraldehyde: It is a saturated dialdehyde. A 2% solution this chemical agent has a wide spectrum of antimicrobial activity. It is effective against bacteria, fungi, bacterial and fungal spores and viruses,. It used for sterilizing urological instruments, lensed instruments, respiratory therapy equipment and other special equipment. 9. Gaseous agents: Sterilization by means of gaseous agents is employed for plastic syringes, blood transfusion apparatus and other laboratory materials which can not be sterilized by heat. There are two types of gaseous agents. a) Ethylene oxide and b)β-Propiolactone. Formaldehyde fumes are also a gaseous agent. a) Ethylene oxide: It is a liquid at temperatures below 10.8°C and vaporizes quickly above this temperature. It is highly inflammable. For use, it is prepared as a nonflammable mixture of ethylene oxide and carbon dioxide or Freon. This still retains antimicrobial property. Ethylene oxide has high penetrating power. It can pass through and sterilize large packets of materials, bundles of cloth and even certain plastics. It is used in specially constructed autoclaves under specified conditions of temperature, humidity and pressure. Bacterial spores are also killed by ethylene oxide. Practical Application: It is used for sterilizing agent for heat and moisture sensitive materials. It is used on spices, biological preparations, soil, plastics certain medical preparations and contaminated laboratory equipment. It also used to decontaminate space craft components. Though ,it is slow in its action , it is effective low temperature and does not damage material exposed it. Mode of Action: The killing effect of ethylene oxide is due to alkylation with organic compounds and enzymes. Alkylation is replacement of hydrogen atom in organic compound with an alkyl group. b) β-Propiolactone: This compound is a colorless liquid at room temperature with a high boiling point. It is considerably more active It is a vesicant and lachrymator and therefore must be handled carefully. It is sporicidal, fungicidal and virucidal. Only 2to 5mg / litre of β-Propiolactone is enough for sterilization purposes. Since it has a low penetration power and may be carcinogenic, it is of restricted use as a sterilizing agent. Evaluation of Antimicrobial Agent Effectiveness The best known disinfectant screening test is the Phenol-coefficient test. In which a potency of a disinfectant is compared with that of phenol. Method: 1) A series of dilutions of phenol and the experimental disinfectant are inoculated with the test bacteria Salmonella typhi and Staphylococcus aureus. 2) Then they are placed in a 20 or 37°C water bath. 3) These inoculated disinfectant tubes are next sub cultured to regular fresh medium at 5 minute intervals. 4) Sub cultures incubated for two or more days. The highest dilution that kill the bacteria after a 10 minute exposure , but not after 5 minutes , are used to calculate the phenol coefficient. 5) The reciprocal of the appropriate test disinfectant dilution is divided by that for phenol to obtain the coefficient. Example: The phenol dilution is 1/90 and maximum effective dilution for disinfectant X is 1/150. Phenol-coefficient of X = 150/90=1.6 - The phenol coefficient of X would be 1.6 The higher the phenol-coefficient value, the more effective the disinfectant under these test conditions. A value grater than 1 means that the disinfectant in more effective than phenol. Table-4 An example of the Type Result in the phenol-coefficient Method with Salmonella typhi 16 Dilution Disinfectant -X Phenol Note: 0 = No growth, += Growth Subculture Tubes. 5 min 10 min 15 min 1:100 1:125 1:150 0 + + 0 0 0 0 0 0 1:175 1:200 + + + + + 0 0 + 0 + + + 1:90 1:100 Table-5 :Phenol-coefficient for Some Disinfectants Disinfectant Phenol-coefficient Salmonella typhi Staphylococcus aureus Phenol Mercurochrome Lysol Ethanol 1 2.7 1.9 0.04 1 5.3 3.5 0.04 17 Table-6: Application of Chemical Agents for Controlling Microorganisms Chemical Agent Phenol& Phenolic Compounds Alcohols: ethyl & isopropyl Iodines Recommended Use General disinfectant Chlorine Water disinfection Silver nitrate Mercurials Quaternaries Formaldehyde Treating burns Skin disinfection Skin disinfection Sterilizing instruments; Fumigation Sterilizing instruments; Fumigation Sterilizing heat sensitive materials, instruments and large equipment Sterilizing heat sensitive materials & instruments Glutaraldehyde Ethylene oxide β-Propiolactone Limitations Microbial effectiveness limited ;irritating and corrosive thermometer antiseptic Skin & antiseptic Disinfect skin Irritating to mucous membrane Inactivated by organic material: pH dependent for effectiveness; objectionable taste and odor unless strictly controlled. Possible irritation Slow acting; toxic Not sporicidal Permeation poor; corrosive Stability limited Flammable; potentially explosive in pure form Lacks penetrating power.