* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pralidoxime Iodide Injection
Prescription costs wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug interaction wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
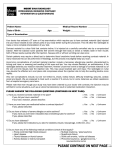
Jet injector wikipedia , lookup
Pralidoxime Iodide Injection (PAM) MIMS Abbreviated Prescribing Information Pralidoxime iodide Pharmalab Section: 20(a) Detoxifying agents, antidotes - Poisoning, Toxicity and Drug Dependence Permitted in sport Use: Anticholinergic organophosphorus pesticide and chemical poisoning; anticholinesterase drug overdose (in myasthenia gravis treatment) Precautions: Iodine content; rapid inj; organophosphate poisoning in myasthenia gravis; nonanticholinesterase substance, carbaryl poisoning; barbiturates, morphine, theophylline, aminophylline, succinylcholine, reserpine, phenothiazine tranquillizers; renal impairment Adverse Reactions: Dizziness; visual disturbances; drowsiness; nausea; tachycardia; hyperventilation; muscle weakness; headache Pralidoxime Iodide Injection (PAM) (Injection) Pralidoxime iodide; amp Pack 25 mg/mL 20 mL [5] : $129.36 Dose Organophosphate poisoning, adults: 1-2 g IVI + atropine; children: 20-50 mg/kg in intermittent doses. Anticholinesterase overdose: 1-2 g IVI, then 250 mg every 5 mins Pralidoxime Iodide Injection MIMS Full Prescribing Information Composition Pralidoxime iodide. Description Chemical name: 2-pyridine aldoxime methiodide. Molecular formula: C7H9IN2O. Yellow crystals formed in a solution of alcohol. Melting point: 225 to 226 deg. C. Very soluble in water, fairly soluble in hot alcohol, poorly soluble in cold alcohol. Insoluble in ether, acetone. Actions Pharmacology. The principal action of Pralidoxime Iodide Injection is to reactivate cholinesterase (mainly outside of the central nervous system) which has been inactivated by phosphorylation due to an organophosphate pesticide or related compound. The reactivation of cholinesterase allows the normal metabolism of acetylcholine to occur, thus allowing the neuromuscular junction and other sites of action to function normally. This includes muscarinic signs to a certain extent. Pralidoxime Iodide Injection also slows the process of aging of phosphorylated cholinesterase to a nonreactivatable form, and detoxifies certain organophosphates by direct chemical reaction. The drug has its most critical effect in relieving paralysis of the muscles of respiration. Pralidoxime Iodide Injection relieves muscarinic symptoms, i.e. salivation and bronchospasm; but this action is relatively unimportant, since atropine is adequate for this purpose. Pralidoxime Iodide Injection antagonises the effects on the neuromuscular junction of the carbamate anticholinesterases, neostigmine, pyridostigmine and ambenonium, used in the treatment of myasthenia gravis. However, it is not nearly as effective as an antidote to these drugs as it is to the organophosphates. Pralidoxime Iodide Injection is distributed throughout the extracellular water; it is not bound to plasma protein. The drug is rapidly excreted in the urine partly unchanged, and partly as a metabolite produced by the liver. The elimination half-life is approximately 1 to 2 hours. Consequently, Pralidoxime Iodide Injection is relatively short acting. In some cases repeated doses or a continuous infusion may be needed, especially where there is any evidence of continuing absorption of the poison. Pharmacokinetics. LD50 in mice (mg/kg): 140 to 178 intravenously; 136 to 260 intraperitoneally; 290 to 340 subcutaneously; 1,500 to 4,000 orally. Indications Antidote in the treatment of poisoning due to those pesticides and chemicals of the organophosphate class which have anticholinesterase activity; and in the control of overdosage by anticholinesterase drugs used in the treatment of myasthenia gravis. Contraindications Hypersensitivity to the drug. Warnings Pralidoxime Iodide Injection is not effective in the treatment of poisoning due to phosphorus, inorganic phosphates or organophosphates not having anticholinesterase activity. As the use of Pralidoxime Iodide Injection for the treatment of poisoning of the carbamate class is relatively ineffective, and the fact that its use with carbamyl poisoning may lead to increased toxicity, Pralidoxime Iodide Injection is not recommended for use in these classes of poisons. Precautions This product contains iodine; use of this product in patients who are allergic to iodine must remain the decision of the treating doctor based on clinical factors. No data are currently available. Intravenous administration of Pralidoxime Iodide Injection should be carried out slowly and, preferably, by infusion, since certain side effects, such as tachycardia, laryngospasm, and muscle rigidity, have been attributed in a few cases to a too rapid rate of injection (see Dosage and Administration). Pralidoxime Iodide Injection should be used with great caution in treating organophosphate overdosage in cases of myasthenia gravis, since it may precipitate a myasthenic crisis. The following precautions should be noted in the treatment of anticholinesterase poisoning, although they do not bear directly on the use of Pralidoxime Iodide Injection. Barbiturates should be used cautiously in the treatment of convulsions since they are potentiated by anticholinesterases; morphine, theophylline, aminophylline, suxamethonium, reserpine, and phenothiazine-type tranquillizers should be avoided in patients with organophosphate poisoning. Impaired renal function. Because pralidoxime iodide is excreted in the urine, a decrease in renal function will result in increased blood levels of the drug. Thus, the dosage of Pralidoxime Iodide Injection should be reduced in the presence of renal insufficiency. Adverse Reactions Dizziness, blurred vision, diplopia and impaired accommodation, headache, drowsiness, nausea, tachycardia, hyperventilation, and muscular weakness have been reported after the use of Pralidoxime Iodide Injection, but it is very difficult to differentiate the toxic effects produced by atropine or the organophosphate compounds from those of the drug. When atropine and Pralidoxime Iodide Injection are used together, the signs of atropinisation may occur earlier than might be expected when atropine is used alone. This is especially true if the total dose of atropine has been large and the administration of Pralidoxime Iodide Injection has been delayed. Excitement and manic behaviour immediately following recovery of consciousness have been reported in several cases. However, similar behaviour has occurred in cases of organophosphate poisoning that were not treated with Pralidoxime Iodide Injection. Dosage and Administration Pralidoxime Iodide Injection is extremely well tolerated in healthy volunteers. Single oral doses up to 7 g have produced minimal side effects. Intravenous doses are even better tolerated with doses as large as 40.5 g over a seven day period having no reported side effects. Organophosphate poisoning. Adults. Treatment of organophosphate poisoning consists of maintaining respiration; administration of atropine and Pralidoxime Iodide; removal of organophosphates from clothing and skin, and administration of supportive measures. Pralidoxime Iodide Injection administration should be started at the same time as atropine. Pralidoxime Iodide Injection is initially administered intravenously in a dose of 1 to 2 g. Signs of recovery (increasing consciousness, decreasing fasciculations and weakness) should occur rapidly. If the symptoms reappear, then an infusion of 2.5% Pralidoxime Iodide is infused at a rate of 0.5 g/hour. A continuous infusion maintains adequate blood levels of Pralidoxime better than intermittent injections. Intramuscular and oral administration is also effective, but intravenous is preferred because of rapidity of action. Atropine is administered intravenously until signs of mild atropinisation occur and the muscarinic symptoms relieved. Assessing cardiac effects by monitoring heart rate, watching for signs of mydriasis, dry mouth and decreased respiratory symptoms will give a good clinical assessment of atropinisation. Children. 20 to 50 mg/kg as intermittent doses required to alleviate symptoms. An infusion can be used after an initial dose has been given. Pralidoxime Iodide Injection 1 g in 5% dextrose and 0.2% saline injection 250 mL has been recommended. Treatment will be most effective if given within a few hours after poisoning has occurred. Usually, little will be accomplished if the drug is first administered more than 48 hours after exposure, but in severe poisoning, it is, nevertheless, indicated since occasionally patients have responded after such an interval. In severe cases, especially after ingestion of the poison, it may be desirable to monitor the effect of therapy electrocardiographically because of the possibility of heart block due to the anticholinesterase. Where the poison has been ingested, it is particularly important to take into account the likelihood of continuing absorption from the lower bowel, since this constitutes new exposure. In such cases, additional doses of Pralidoxime Iodide Injection may be needed every 3 to 8 hours. In effect, the patient should be titrated with Pralidoxime Iodide Injection as long as signs of poisoning recur. In the absence of severe gastrointestinal symptoms resulting from the anticholinesterase intoxication, Pralidoxime Iodide Injection may be administered orally in doses of 1 to 3 g (2 to 6 ampoules) every five hours. As in all cases of organophosphate poisoning, care should be taken to keep the patient under observation for at least 24 hours. If convulsions interfere with respiration, sodium thiopental 2.5% solution may be given intravenously with care. Anticholinesterase overdosage. As an antagonist to such anticholinesterases as neostigmine, pyridostigmine, and ambenonium, which are used in the treatment of myasthenia gravis, Pralidoxime Iodide Injection may be given in a dosage of 1 to 2 g intravenously followed by increments of 250 mg every five minutes. Overdosage Treatment. Administer artificial respiration and other supportive therapy as needed. Presentation Ampoules, 25 mg/mL 20 mL: 5's. Poison Schedule Unscheduled. Date of TGA approval or last amendment 01/09/1990