* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Atrial FIbrillation - familypracticeresidency.org
Survey
Document related concepts
Saturated fat and cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Transcript
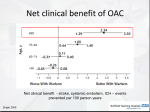
David W Kabel MD, FACC September 4, 2013 2.7 million Americans have atrial fibrillation Numbers are expected to rise in the future Aging population More chronic cardiac conditions Better detection through long term monitoring Event monitors, pacemakers, implantable monitors Costs continue to rise Annual cost is $7-10 billion per year and rising Admissions for AF are up 66% in past 20 years Overall prevalence-1% <65 3-5% <80 10%+ 1.5 times higher in men 2 times higher in caucasians Cardiac risk factors Non-cardiac risk factors Hypertension ASHD and PVD CHF Cardiac surgery (25-30% postop) Family history of AF Diabetes and metabolic syndrome Obstructive sleep apnea Obesity Psychological stress COPD Hyperthyroidism Tall stature Inflammatory conditions (elevated CRP) Modifiable risk factors Smoking ETOH >3 drinks per day AF in absence of underlying risk factors 12-20% of all AF patients 45% of AF in younger patients Presence and nature of symptoms Clinical type Onset of first attack or date of discovery Frequency, duration, precipitating factors, and mode of termination Response to any medications previously given Presence of underlying heart disease or other reversible conditions (hyperthyroidism, etc) Confirm presence of AF LVH P wave morphology Pre-excitation Previous MI Left or Right BBB Other atrial arrhythmias Measure PR, QRS, and QT intervals in conjunction with anti-arrhythmic therapy Valvular disease LA and RA atrial size LV size and function LVH Right sided pressures (pulmonary hypertension) LA thrombus(low sensitivity) Pericardial disease Chest X-ray Cardiomegaly Pulmonary disease Blood work Thyroid functions BMP Hepatic profile CRP? CBC May be indicated in some circumstances Stress testing Holter monitor, event monitor Looking for LAA thrombus To guide cardioversion EP studies If diagnosis is in question To assess rate control TEE If AF is exercise induced To assess rate control Wide complex tachycardia Pulmonary vein isolation AV node ablation and pacemaker Sleep study-especially if episodes are mostly nocturnal Rate control Restoration of sinus rhythm (rhythm control) Most important initial strategy Prevention of CHF (tachycardia induced cardiomyopathy) May be initial strategy in some patients Prevention of thromboembolism(TE) Class I Symptoms or signs of ischemia, hypotension, angina or heart failure Pre-excitation syndrome with extreme tachycardia and hypotension Symptoms are unacceptable to the patient Class IIa Part of long term management strategy Patient preference in cases of infrequent episodes of AF Class III Relatively short intervals between episodes of AF Presence of digitalis toxicity or hypokalemia Class I Duration >48 hrs or unknown-Oral anticoagulation (OAC) for 3 weeks before and 4 weeks after DCC Duration >48 hrs and hemodynamically unstable-IV heparin followed by OAC for 4 weeks. Role of LMWH is uncertain Duration <48 hrs-DCC without prior OAC, followed byOAC post-procedure depending upon TE risk Class IIa Duration <48 hrs-OAC prior dependent upon risk TEE guided-Proceed if no LAA thrombus-OAC for 4 weeks post DCC. Limited date on LMWH AV node ablation with pacemaker Indicated in persistent or permanent AF when ventricular rate cannot be controlled medically or patient is intolerant to rate control medications Cryoablation of AV node Patient becomes pacemaker dependent Pulmonary vein isolation-cryoablation Right sided approach across atrial septum to LA. 4 pulmonary veins are identified and cryoablation occurs in circular pattern around pulmonary vein orifices Rare complication of PV stenosis leading to PHT Initial success rate of 80-90% Repeat PVI common Surgical Maze Procedure Series of incisions inside the left atrium to redirect and organize electrical impulses -done on cardiopulmonary bypass Usually done in conjunction with mitral valve surgery or other cardiac surgeries May be done as stand alone procedure in intractable cases who are highly symptomatic Risk Stratification is key to decision making Must weigh risk of bleeding into the calculation Newer anticoagulants appear “non-inferior” to warfarin for prevention of TE “Non-valvular” AF means absence of rheumatic mitral valve disease of mechanical prosthesis Estimates are that only 50-60% of AF patients at risk for TE are on OAC Reasons cited include risk of bleeding and risk of falls. Patients at highest risk of bleeding and falls are also at highest risk of TE 182,000 patients through national registry Compared risk of ischemic stroke without OAC vs risk of intracranial hemorrhage while taking OAC Used CHADS-VASC and HAS-BLED scoring systems Anticoagulation and Risk Factors in AF Cohort Kaiser Permanente of Northern California database 13,559 adults with AF followed a mean of 6 years Followed patients taking and not taking OAC Benefits of OAC far outweigh risks in high risk populations, even when intracranial hemorrhage is weighted a higher risk More weight can be assigned to age Vascular disease and ischemic heart disease do not appear to increase TE risk in AF Renal disease and proteinuria are risk factors for TE ATRIA score may be better at predicting both low risk patients and those at highest risk of severe stroke than CHADS2 and CHADS-VASC The incidence of AF is rising exponentially due to an aging population and improved prognosis in patients with cardiovascular disease AF is multifactoral Prevention of AF depends upon aggressive management of risk factors such as hypertension Strategies of rate vs rhythm control depend upon individual patient characteristics There are several anti-arrhythmic drugs available, all of which have issues of effectiveness and side effects which limit their usefulness Non-pharmacologic therapies are gaining in popularity and becoming more effective AF is associated with high medical costs in both inpatient and outpatient settings A large number of AF patients are at low risk for TE and should be treated with ASA or nothing OAC is under-utilized in the group of patients at highest risk for ischemic stroke, namely the elderly Risk for falls is not a contraindication to OAC