* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download NORTH OF ENGLAND CARDIOVASCULAR NETWORK ATRIAL
Cardiac contractility modulation wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
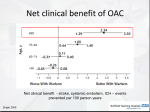
NORTH OF ENGLAND CARDIOVASCULAR NETWORK ATRIAL FIBRILLATION PATHWAY Opportunistic case finding1 Symptomatic presentation Emergency admission2 Acutely unwell, rapid ventricular rate, early cardioversion indicated 12 lead ECG confirmation Examination and baseline investigations3 Diagnosis 1 Patients aged 65 and older should have a manual pulse palpation at least annually and any irregularity should be followed up with a 12 lead ECG Consider ECHO5 Stroke risk assessment / initiation of stroke prevention4 For details please refer to the North of England Cardiovascular network guidelines: www.necvn.nhs.uk 2 Consider emergency hospital admission for patients with haemodynamic instability, heart failure, chest pain, breathlessness at rest, lightheadedness or syncope, stroke / TIA, rates in excess of 150bpm and wide QRS complexes. Patients considered for immediate cardioversion (clear history of AF onset within 48hrs) If not confident refer to AF/arrhythmia clinic 3 Physical examination including manual BP evaluation, 12‐ lead ECG if not already carried out, FBC, U & Es, TFTs and LFTs, CXR if appropriate Stroke prevention 4 See back for details Refer: ‐ Symptomatic persistent AF - Paroxysmal AF, particularly young patients and lone AF ‐ Mixed arrhythmias ‐ AF with structural abnormality6 Asymptomatic or acceptable symptoms Treat as permanent AF Rate vs Manage rate control7 in Primary Care Refer to AF/arrhythmia clinic8 8 Provision of primary AF services vary across the network and may be provided by specialist nurses, GPwSI or within cardiology departments Not achieved Annual follow up9 by CHD nurse / lead GP: ECG, manual BP, drug review Rate control Follow up 6 Structural heart disease such as valve disease, heart failure, cardiomyopathy 7 Target heart rate at rest < 90bpm (<110 during exertion in sedentary individuals and 200 – age in active individuals). First line treatment: beta‐blockers or rate limiting calcium channel blockers Rhythm Achieved 5 Consider echocardiogram for patients with suspected structural heart disease (murmur, abnormal ECG etc.) and occasionally for refinement of stroke risk assessment Sinus rhythm / rate control achieved Therapy tolerated and stable No – refer to electrophysiologist10 9 Needs to include review of stroke prevention and the appropriateness of the rate/rhythm strategy 10 For consideration of pulmonary vein isolation, pacemaker / AV node ablation or surgery Stroke prevention is arguably the most important aspect of atrial fibrillation management Warfarin is highly effective in reducing stroke risk but is greatly underused AF as a Cause of Stroke Does my patient need warfarin?* Assessing stroke risk in AF patients National Data The annual risk of stroke is 5‐6 times greater in AF patients than in people with normal heart rhythm 18% of patients presenting with stroke are in AF at presentation. This equates to 16,000 strokes in England, of which 12,500 are thought to be directly attributable to AF Warfarin is highly effective in preventing stroke in AF, reducing risk of stroke by 64% compared to placebo Particularly in the elderly the risk of major haemorrhage is similar for Warfarin and Aspirin (1.9% vs 2.0% pa) Aspirin only reduces stroke risk by 22% Around 25 patients at high risk of stroke require warfarin treatment for one year to prevent one stroke The 2006 NICE guidance on AF costing report concluded that 46% of patients who should have been receiving warfarin were not CHF Hypertension Age ≥75 Diabetes Stroke /TIA Risk category 0 Stroke Risk % pa 1.9 1 2.8 2 4.0 3 5.9 CHADS2 Score CHADS2 Score 1 1 1 1 2 CHADS2 score 4 8.5 5 12.5 6 18.2 HAS‐BLED bleeding risk score Hypertension >160mmHg 1 Abnormal renal and liver Creatinine >200, 1 or 2 function ALT >3 x ULN Stroke / TIA 1 Bleeding diathesis 1 Labile INR 1 Elderly (>65) 1 Drugs / alcohol 1 or 2 Exercise caution and review regularly if score ≥ 3 FALLS ARE NOT A MAJOR RISK FACTOR FOR BLEEDING IN ANTICOAGULATED PATIENTS Recommended stroke prevention High ≥2 Oral anticoagulation (OAC) Moderate particularly if age > 65 & evidence of vascular disease 1 Either OAC or Aspirin 75–325 mg daily Preferred: OAC rather than Aspirin No risk factors and age < 65 0 Either Aspirin or no antithrombotic therapy Preferred: no antithrombotic therapy Absolute contraindications to Warfarin# • • • • • • • • Hypersensitivity to warfarin Within 2 days of surgery Bacterial endocarditis Intracranial haemorrhage #this is not an Bleeding diathesis exhaustive list Existing or recent peptic ulcer Uncontrolled hypertension >180mmHg Pregnancy * target INR 2‐3 with time in therapeutic range >65% GRASP‐AF Query and risk stratification tool is FREE and available for use with all GP clinical systems in England Find further information at: Important information for your patients: www.atrialfibrillation.org.uk Do you know why you are taking warfarin, your target INR and the importance of attending for INR checks? It is important to tell your doctor and dentist that you are taking warfarin Before buying any medicines including alternative remedies tell the pharmacist that you are taking warfarin The concomitant use of aspirin, clopidogrel & warfarin or aspirin & warfarin may be appropriate in patients with coronary heart disease Any major changes in your diet may affect how your body responds to warfarin. If this exceeds a few days you should have an INR test Cranberry & grapefruit juice can affect your INR and should be avoided It is dangerous to ‘binge drink’ whilst taking anticoagulants GRASP‐AF provides a set of MIQUEST queries to identify, for your practice, patients with a diagnosis of AF who are not on warfarin http://www.npsa.nhs.uk/nrls/alertsand-directives/alerts/anticoagulant It calculates their risk of stroke using the validated CHADS2 scoring system and highlights patients with a CHADS2 score of 2 or more who are not on warfarin and would benefit from a review to assess the issue of anticoagulation. www.stroke.org.uk To find out more about this new tool and to sign up to run the search simply go to www.improvement.nhs.uk/graspaf Thanks to Stroke Network * For references please go to NECVN website Surrey Heart and