* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Prior Authorization Criteria - AmeriHealth Caritas Pennsylvania
Survey
Document related concepts
Transcript
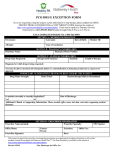
Pharmacy Prior Authorization Criteria
www.amerihealthcaritaspa.com
www.amerihealthcaritasnortheast.com
All images are used under license for illustrative purposes only.
Any individual depicted is a model.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Revision/Review
Date 04/2016
Field Description
Ampyra
Ampyra (dalfampridine) tablets
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PP I), or disease state specific standard of care guidelines.
History of seizures. Moderate or severe renal impairment (creatinine
clearance ≤ 50mL/minute)
See “other criteria”
Patient must be 18 years of age or older
Prescriber must be a neurologist
If the criteria are met, the request will be approved with a 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessit y review.
Initial Authorization:
• Baseline creatinine clearance (within 60 days of request)
• Patient has diagnosis of multiple sclerosis (MS), patient is
ambulatory (baseline 25 foot walk was submitted with request),
AND patient has walking impairment
• Documentation was submitted (consistent with pharmacy claims
data, OR for new members to the health plan, consistent with
chart notes) that patient is currentl y being treated for MS (e.g.
immunomodulator, interferon, immunosuppressive), or
documentation of a medical reason (intolerance, hypersensitivit y)
as to why patient is unable to use one of these agents to treat
their medical condition
• Drug is being requested at an FDA approved dose
Re-authorization:
• Documentation of improvement in 25 foot walk was submitted
with request
• Documentation was submitted patient is on MS treatment (e.g.
immunomodulator, interferon, immunosuppressive), or
documentation of a medical reason (intolerance, hypersensitivit y)
as to why patient is unable to use one of these agents to treat
their medical condition
• Drug is being requested at an FDA approved dose
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
2
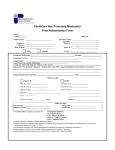
PerformRx Prior Authorization Criteria
ACTHAR (corticotropin) Vials: 80u/ml available in 5 ml vials
PA CRITERI A FOR APPROVAL FOR IN FANTILE SPASMS (WEST SYNDROME):
• Patient is < 2 years of age
• The medication is being prescribed b y a neurologist.
• Documentation of the patient’s current weight (in kg) and height/length (in cm) or bod y
surface area (BSA)
If all of the above conditions are met, the request will be approved for up to a1 month
duration; if all of the above criteria are not met then, the request is referred to a Medical
Director/Clinical reviewer for medical necessit y review.
PA CRITERIA FOR A PPROVAL FOR MUL TIPLE SCLEROSIS:
•
•
Documentation was submitted that patient is having acute attack, with neurologic
symptoms and increased disability or impairments in vision, strength or cerebellar
function, and has failed therap y with IV meth ylprednisolone, or a medical reason has
been submitted why patient is unable to use IV methylprednisolone.
The medication is being prescribed b y a neurologist
If all of the above conditions are met, the request will be approved for up to a1 month duration;
if all of the criteria are not met, the request will be sent to the Medical Director/Clinical
reviewer for medical necessity review.
PA CRITERI A FOR ALL OTHER FD A APPROVED CONDITIONS AND
INDICATIONS :
• Documented trial and failure of IV meth ylprednisolone AND oral prednisone, or
documented medical reason for wh y the patient cannot use these therapies for treatment
AND
• Documentation was provided that ALL other standard therapies have been used to treat
the member’s condition as described in the medical compendium (Micromedex, AHFS,
Drug Points, and package insert) as defined in the Social Security Act and/or per
recognized standard of care guidelines OR there is a documented medical reason (i.e.
medical intolerance, treatment failure, etc.) for why all other standard therapies could
not be used to treat the member’s condition.
AND
• Prescriber is a specialist in the condition they are treating.
If all of the above conditions are met, the request will be approved for up to a1 month
duration, according to standard dosing based on indication. If all of the above criteria
are not met then, the request will be sent to a Medical Director/Clinical reviewer for
medical necessit y review.
Revision/Review Date: 6/2016
NOTE: Clinical reviewer must override criteria w hen, in his/her professional
judgment, the requested item is medically necessary.
3
PERFORMRx PRIOR AUT HORIZAT ION PROTOCOL FOR INJ ECTABLE 5HYDROXYTRYPTAMINE -3 (5HT3) SEROTONIN RECEPT OR ANTAGONISTS
Formulary Status: Generic Ondansetron or Granisetron Preferred
Aloxi (palonosetron)
Anzemet (dolasetron)
Kytril (granisetron)
Zofran (ondansetron)
Any other newly marketed agent
Criteria for Approval:
The request for the medication is for an Food and Drug Administration (FDA) approved indication,
and/or is used for a medical condition that is supported by the medical compendium (Micromedex, American
Hospital Formulary Service (AHFS), Drug Points , Drug Package Insert) as defined in the Social Security
Act 1927 and/or per the National Comprehensive Cancer Network (NCCN), the American Society of Clinical
Oncology (ASCO), National Cancer Institute {NCI} (a Division of the U.S. National Institutes of Health)
and the Multinational Association of Supportive Care in Cancer (MASCC) standard of care guidelines for
antiemetic therapy.
•
Patients receiving an antineoplastic agent =as HIGH or MODERATE emetic risk per the ASCO Practice
guidelines can receive Aloxi® (palonosetron hydrochloride) as a first line antiemetic agent. (See tables that
follow)
•
For all other patients, if the medication request is for any other 5-hydroxytryptamine-3 (5HT3) serotonin
receptor antagonist other than generic Ondansetron or generic Granisetron, the patient has a documented
(consistent with pharmacy claims data, OR for new members to the health plan consistent with medical chart
history) treatment failure after receiving an adequate trial of generic Ondansetron or generic Granisetron
and/or has another documented medical reason ( intolerance, hypersensitivity, contraindication, etc.) for not
utilizing these medications to treat their medical condition.
•
Prescribed dosing of the 5HT3 serotonin receptor antagonist is within FDA approved indications and/or is
supported by the medical compendium as defined by the Social Security Act and/or per the NCCN, ASCO,
NCI or MASCC standard of care guidelines.
•
4
The medication is recommended and prescribed by a specialist in the field to treat the patient’s respective
medical condition.
•
If all of the above conditions are met, the request will be approved for up to 6 months or as recommended per
FDA approved indications and/or as defined by the medical compendium as defined above and/or per the
NCCN, ASCO, NCI or MASCC standard of care guidelines; if all of the above criteria are not met, the
request is referred to a Medical Director/Clinical reviewer for medical necessity review.
5
Level
High
Frequency of Emesis%
>90%
IV Chemotherapy agent
Carmustine, Cisplatin,
Cyclophosphamide ≥1500 mg/ m2
Dacarbazine, Dactinomycin,
Mechlorethamine, Streptozocin
Moderate
30-90%
Ale mtuzu mab, Azacytidine
Belinostat, Bendamustine,
Cabazitaxel, Carboplatin,
Clofarabine,
Cyclophosphamide <1500 mg/ m2
Cytarabine >1000 mg/m2
Daunorubicin *, Doxorubicin*
Epirubicin *, Idarubicin *
Ifos famide, Irinotecan, Oxaliplatin
P ralatrexate, Temozolomide
Low
10-30%
Blinatumo mab, Bortezomib,
Carfilzo mib,
Cytarabine ≤1000 mg/m2
Dabrafenib, Docetaxel, Eribulin
Etoposide, Fluorouracil,
Gemcitabine, Ibrutinib,
Idelalisib, Ipilimumab, Ixabepilone,
Methotrexate**, Mitomycin
Mitoxantrone, P aclitaxel, P anitumu mab,
P egylated liposomal doxorubicin,
P emetrexed
P ertuzumab, Romidepsin, Temsirolimus,
66
6
Topotecan
Trastuzu mab, Ado-trastuzumab
7
emtansine, V emurafenib
8
*These anthracyclines, when combined with cyclophosphamide, are now designated as having high emetic risk. **At doses >1 gram,
methotrexate has at least moderate emetogenic potential.
Reproduced with updated data from: Basch E, Prestrud A, and Hesketh P, et al. Antiemetics: American Society of Clinical Oncology
Clinical Practice Guideline Update. J Clin Oncol 2011; 29:4189.
Graphic 58756 Version 27.0
Degree of emetogenicity
(incidence)
High (>90%)
Oral Antineoplastic Agent*
P rocarbazine
Altretamine (hexameth yl mela min e)
Moderate (30 to 90%)
Bosutinib, Busulfan (≥4 mg/day),
Cabozantinib, Ceritinib, Crizotinib, Cyclophosphamide, Imatinib, Lomustine,
Olaparib, Temozolomide,
Tretinoin, Vandetanib
Afatinib, Axitinib, Bexarotene, Capecitabine, Dasatinib, Estramustine, Etoposide,
Lo w (10 to 30%)
Everolimus, Fludarabine, Ibrutinib, Idelalisib, Lapatinib, Lenalidomide
Lenvatinib, Nilotinib, Palbociclib
P azopanib, Sunitinib, Tegafur uracil
Thalidomide, Topotecan, V emurafenib, Vorinostat
6-Thioguanine, Chlorambucil,
Minimal (<10%)
Erlotinib, Gefitinib, Hydroxyurea,
Melphalan (L-phenylalanine must ard),
Methotrexate, Regorafenib, Sorafenib
9
** Considerable uncertainty prevails for the emetogenic risk of oral agents.
Reproduced with updated data from: Basch E, Prestrud A, and Hesketh P, et al. Antiemetics: American Society of Clinical Oncology
Clinical Practice Guideline Update. J Clin Oncol 2011; 29:4189.
Graphic 58756 Version 27.0
Review Date: 7/2016
10
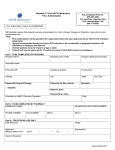
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
NON-FORMULARY MEDICATION FOR USE IN ADHD
TREATMENT FOR MEMBERS OVER 21
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
Members > 21 years old
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
o Appropriate diagnosis/indication for requested non-formular y
medicationo For use in adults for Attention Deficit Hyperactivit y Disorder,
the DSM-V criteria must be met: (see attachment 1).
AND
o Appropriate dose of medication based on age (i.e. pediatric and
elderl y populations) and indication
AND
o Documented trial and failure or intolerance with up to three
formular y medications used to treat the documented diagnosis.
For medications where there is onl y one formular y agent, onl y
that agent must have been ineffective or not tolerated
OR
o No other formular y medication has a medicall y accepted use
for the patient’s specific diagnosis as referenced in the medical
compendia.
OR
All other formular y medications are contraindicated based on the
patient’s diagnosis, other medical conditions, or other medication
therap y
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
11
Attachment 1: DSM-V: Attent ion-Deficit/Hyperactivity Disorder (ADHD)
12
Source: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Copyright 2000 2013 American Psychiatric
Association
People with ADHD show a persistent pattern of inattention and/or h yperactivit y-impulsivit ythat interferes with
functioning or development:
1)
•
•
•
•
•
•
•
•
•
2)
•
•
•
•
•
•
•
•
•
Inattention: Six or more symptoms of inattention for children up to age 16, or five or more for adolescents 17 and older
and adults; sym ptoms of inattention have been present for at least 6 months, and they are inappropriate for
developmental level:
Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
Often has trouble holding attention on tasks or play activities.
Often does not seem to listen when spoken to directly.
Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g.,
loses focus, side-tracked).
Often has trouble organizing tasks and activities.
Often avoids, dislikes, or is reluctant to do tasks that require mental effort over a long period of tim e (such as
schoolwork or homework).
Often loses things necessary for tasks and activities (e.g. school materials, pencils, books, tools, wallets, keys,
paperwork, eyeglasses, m obile telephones).
Is often easily distracted
Is often forgetful in daily activities.
Hyperactivity and Impulsivity: Six or more symptoms of hyperactivity-impulsivity for children up to age 16, or five or
more for adolescents 17 and older and adults; sym ptoms of hyperactivity-im pulsivity have been present for at least 6
months to an extent that is disruptive and inappropriate for the person’s developmental level:
Often fidgets with or taps hands or feet, or squirms in seat.
Often leaves seat in situations when rem aining seated is expected.
Often runs about or climbs in situations where it is not appropriate (adolescents or adults may be limited to feeling
restless).
Often unable to play or take part in leisure activities quietly.
Is often "on the go" acting as if "driven by a m otor".
Often talks excessively.
Often blurts out an answer before a question has been com pleted.
Often has trouble waiting his/her turn.
Often interrupts or intrudes on others (e.g., butts into conversations or games)
In addition, the following conditions must be met:
•
•
•
•
Several inattentive or hyperactive-impulsive symptoms were present before age 12 years.
Several symptoms are present in two or m ore setting, (e.g., at home, school or work; with friends or relatives; in other
activities).
There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning.
The symptoms do not happen only during the course of schizophrenia or another psychotic disorder. The symptoms
are not better explained by another mental disorder (e.g. Mood Disorder, Anxiety Disorder, Dissociative Disorder, or a
Personality Disorder).
13
Based on the t ypes of s ymptoms, three kinds (presentations) of ADHD can occur:
Combined Presentation: if enough symptoms of both criteria inattention and hyperactivity-impulsivity were present for the past 6
months
Predom inantly Inattentive Presentation: if enough sym ptoms of inattention, but not hyperactivity-impulsivity, were present for the
past six m onths
Predom inantly Hyperactive-Impulsive Presentation: if enough sym ptoms of hyperactivity-im pulsivity but not inattention were
present for the past six m onths.
Because symptoms can change over tim e, the presentation may change over tim e as well.
Source: Centers for Disease Control and Prevention. (2013). Attention-Deficit/ Hyperactivity Disorder (ADHD). Retrieved
from http://www.cdc.gov/ncbddd/adhd/diagnosis.html (2014)
14
Field Name
Prior Authorization
Desc
Drug(s)
Group
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Field Description
ALPHA-1 PROTEINASE INHIBITORS (HUMAN)
Alpha-1 Proteinase Inhibitor (human) (Aralast NP, Glassia, Prolastin ®-C,
Zemaira®)
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formular y Service (AHFS), United States Pharmacopeia Drug Information for
the Healthcare Professional (USP DI), and the Drug Package Insert.
None
None
18 years of age or older
Prescriber must be pulmonologist
Coverage Duration
The request will be approved for up to a 6 month duration; if all of the above
criteria are not met, the request is referred to a Medical Director for medical
necessit y review.
Other Criteria
IN IT IA L AUTHOR IZATION:
• The member is an adult (≥ 18 y/o) and has a documented diagnosis of a
congenital deficienc y of alpha-1 antitr ypsin (ATT) [serum level < 11uM
or 80mg/dl].
• Documentation was submitted indicating the member has undergone
genetic testing for ATT deficiency and is classified as phenot ype PiZZ,
PiZ(null) or Pi(null)(null) [NOTE: phenotypes PiMZ or PiMS are not
candidates for treatment with Alpha1-Proteinase Inhibitors].
• Documentation was submitted indicating the member does not have
selective IgA deficienc y (IgA level < 15 mg/dL) with known antibodies
against IgA.
• Documentation was submitted (member’s PFT results)_indicating airflow
obstruction by spirometry (e.g., FEV1 <80 percent of predicted)
• Documentation was submitted indicating member is non-smoker or exsmoker (e.g. Smoking cessation treatment)
• Documentation of the member’s current weight
• The Alpha1-Proteinase Inhibitor (human) is being prescribed at an FDA
approved dosage.
If the medication request is for an Alpha1-Proteinase Inhibitor (human)
product other than Prolastin®-C, the patient has a documented medical reason
(intolerance, h ypersensitivit y, contraindication, treatment failure, etc.) for not
using Prolastin®-C to treat their medical condition.
PA CR ITER IA FOR REAUTHOR IZAT ION:
• Documentation of the member’s current weight
• Documentation was submitted indicating the member has clinicall y
benefited from therap y (i.e. improved lung function tests {pulmonary
function tests}), alpha-1 antitrypsin serum level maintained above 80
mg/dL, improved qualit y of life).
• The Alpha1-Proteinase Inhibitor (human) is being prescribed at an FDA
approved dosage.
15
Review Date: 2/2016
NOTE: Clinical reviewer/Medical Director must override criteria when, in
his/her professional judgment, the requested item is medically necessar y.
16
Field Name
Field Description
Prior Authorization Group
ANDROGENIC AGENTS
Drug(s)
ANDROGEL (testosterone) ANDRODERM (testosterone)
TESTIM (testosterone)
AXIRON (testosterone)
ANDROID (testosterone)
ANDROXY (testosterone)
AXIRON (testosterone)
DEPO-TESTOSTERONE (Testosterone Cypionate)
FORTESTA (testosterone)
METHIT EST
STRIANT BUCCAL
TESTOPEL IMPLANT (testosterone)
TESTRED (testosterone)
TESTOSTERONE ENANTHATE
TESTOSTERONE CYPIONATE
VOGELXO
Or any newly marketed testosterone agent
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI) , and the Drug Package Insert).
Patients that are female
Prescriber must document medical reason for low testosterone, such as
Hypogonadism, copy of laboratory result required, demonstrating low testosterone.
None
None
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
If all of the conditions are met, the request will be approved with 3 month duration; if
the above conditions are not met, the request will be referred to a Medical Director
for medical necessity review.
F or Initial Authorization:
• Male patient
• Diagnosis of primary hypogonadism (congenital or acquired) or
hypogonadotropic hypogonadism (congenital or acquired)
• Documented low testosterone level (s) (copy of laboratory result required)
F or Re-Authorization:
• Diagnosis of primary hypogonadism (congenital or acquired) or
hypogonadotropic hypogonadism (congenital or acquired).
Review Date 4/2015
NOTE: Clinical reviewer mu st override criteria when, in his/her professional judg ment,
the requested item is medically necessary.
17
Field Name
Prior Authorization Group
Description
Drugs
Field Description
ANGIOTENSIN II RECEPTOR BLOCKER AND
RENIN INHIBITOR MEDICATIONS
FORMULARY STATUS: Formulary, Pays at Point-of-Sale
(First Line)
• Cozaar (losartan) Tablets
• Hyzaar (losartan/hydrochlorothiazide) Tablets
FORMULARY STATUS: Formulary, Requires Step
Therapy (Second Line)
• Avapro (irbesartan) Tablets
• Avalide (irbesartan/hydrochlorothiazide) Tablets
• Diovan (valsartan) Tablets
• Diovan-HCT (valsartan/hydrochlorothiazide) Tablets
NOTE: Patient must meet criteria #1 for approval of
initial PA request.
FORMULARY STATUS: Non-Formulary, Requires Prior
Authorization (Third Line)
• Atacand (candesartan cilexetil) Tablets
• Atacand HCT(candesartan cilexetil/
hydrochlorothiazide) Tablets
• Azor (amlodipine besylate/olmesartan medoxomil)
Tablets
• Benicar (olmesartan medoxomil) Tablets
• Benicar HCT (olmesartan medoxomil/
hydrochlorothiazide) Tablets
• Edarbi (azilsartan) Tablets
• Edarbyclor (azilsartan/hydrochlorothiazide) Tablets
• Exforge (amlodipine besylate/valsartan) Tablets
• Exforge HCT
(amlodipine/valsartan/hydrochlorothiazide) Tablets
• Micardis (telmisartan) Tablets
• Micardis-HCT (telmisartan/hydrochlorothiazide)
Tablets
• Teveten (eprosartan mesylate) Tablets
• Tribenzor (olmesartan
medoxomil/amlodipine/hydrochlorothiazide) Tablets:
• Twynsta (telmisartan/amlodipine) Tablets
• Tekturna (aliskiren hemifumarate) Tablets
• Tekturna HCT (aliskiren/hydrochlorothiazide)
18
Tablets
NOTE: Patient must meet criteria #1 & #2 for approval
of initial PA request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA),
Micromedex, American Hospital Formulary Service (AHFS),
United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI), the Drug Package Insert
(PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with a 12
month duration; if the criteria are not met, the request will be
referred to a clinical reviewer for medical necessity review.
PA CRITERIA FOR APPROVAL:
1. Documented adequate trial and failure or intolerance
with a first line agent of at least 15 days of therapy
within the previous 90 days.
2. Documented adequate trial and failure or intolerance
with a second line agent of at least 15 days of therapy
within the previous 90 days. .
Revision/Review Date
10/2016
Medical Director/clinical reviewer must override criteria
when, in his/her professional judgement, the requested
item is medically necessary.
19
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Topical Antiviral Treatment Prior Authorization Criteria
FORMULARY STATUS: Formulary, pays at the point of sale
Abreva® (docosanol)
FORMULARY STATUS: Non-Formulary, Prior Authorization
Required
Denavir® (penciclovir)
Xerese® (acyclovir/hydrocortisone)
Zovirax® (acyclovir) cream/ointment
or any newly marketed topical antiviral agent
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred to
a clinical reviewer for medical necessity review.
Initial Authorization
For the treatment of herpes labialis (cold sores):
Documented trial and failure or intolerance to a preferred oral
antiviral, such as acyclovir.
OR
Documented trial and failure or intolerance to a preferred topical
agent, such as Abreva.
For the treatment of venereal herpes:
Documented trial and failure or intolerance to a preferred oral
antiviral, such as acyclovir.
Revision/Review
Date 10/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
20
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Agents for Atopic Dermatitis
Eucrisa® (crisaborole), Protopic® (tacrolimus), Elidel®
(pimecrolimus)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
Provider must be a pediatrician or dermatologist
If the criteria are met, the request will be approved with up to a 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization
For Elidel®:
o Diagnosis of mild to moderate atopic dermatitis in non
immunocompromised patient in whom the use of alternative,
conventional therapy is deemed inadvisable because of potential
risks, or who are not adequately responsive to or intolerant of
alternative conventional therapies.
Revision/Review
Date 02/2017
For Protopic®:
o Diagnosis of moderate to severe atopic dermatitis in whom the use
of alternative, conventional therapies is deemed inadvisable because
of potential risks, or in the treatment of patients who are not
adequately responsive to or are intolerant of alternative,
conventional therapies
For Eucrisa®:
o Diagnosis of mild to moderate atopic dermatitis
AND
o Trial and failure of a formulary corticosteroid
AND
o Trial and failure of Protopic® or Elidel®
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
21
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Oral Antipsychotic Agents
For antipsychotic medications that require PA for members less than
18 years of age
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
Prescription is written by a specialist or appropriate consultation with
a specialist has occurred. Specialists may include Pediatric
Neurologist, Child and Adolescent Psychiatrist, Child development
Pediatrician, or General Psychiatrist for recipients 14 or older.
If the criteria are met, the request will be approved with up to a 12
week duration for initial authorization and up to 12 month duration for
reauthorization; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
1. Documentation of severe behavioral problems related to
psychotic or neuro-developmental disorders (such as but not
limited to autism, intellectual disability, conduct disorder,
bipolar disorder, tic disorder (including Tourette’s syndrome),
transient encephalopathy or schizophrenia )
2. Documentation prescription is written by a specialist or
appropriate consultation with a specialist has occurred.
(specialists may include Pediatric Neurologist, Child and
Adolescent Psychiatrist, Child development Pediatrician, or
General Psychiatrist for recipients 14 or older).
3. Documentation of a comprehensive patient evaluation
including baseline monitoring of all of the following:
a. Weight/BMI
b. Blood pressure
c. Glucose
d. Lipids
e. Extrapyramidal symptoms (EPS) using the abnormal
involuntary movement scale (AIMS)
4. Documentation of a trial of non-pharmacologic therapies (such
as but not limited to behavior, cognitive or family based
therapies)
Re-Authorization:
1. Documentation of improvement of target symptoms
2. Documentation prescription is written by a specialist or
appropriate consultation with a specialist has occurred.
(specialists may include Pediatric Neurologist, Child and
Adolescent Psychiatrist, Child development Pediatrician, or
General Psychiatrist for recipients 14 or older
22
3. Documentation of follow up monitoring of all of the following:
a. Weight/BMI (at least quarterly)
b. Blood pressure (after 3 months of therapy and annually
thereafter)
c. Glucose (after 3 months of therapy and annually
thereafter)
d. Lipids (after 3 months of therapy and annually
thereafter)
e. Extrapyramidal symptoms (EPS) using the abnormal
involuntary movement scale (AIMS) (after 3 months of
therapy and annually thereafter)
4. Clinical rationale for continued use or plan for discontinuation
of therapy
Duplicate Antipsychotic Criteria
Duplicate antipsychotic use will be approved when one of the
following criteria is met:
1. Documentation member is being titrated to or tapered from a
drug in the same class
2. Documentation of peer reviewed literature or national
treatment guidelines that support the use of the regimen
requested
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
23
PERFORMRX N ATIONAL PA CRITERIA
®
AVINZ A (morphine sulfate extended release) Capsule: 30mg, 45mg, 60mg, 75mg, 90mg, 120mg
FORMULARY ST ATUS : Non-Formulary
PA CRITERI A FOR APPROV AL :
•
Diagnosis of moderate to severe pain requiring opioid analgesic for extended period of time.
AND
•
Documented trial and failure or intolerance to generic morphine sulfate extended release tablets.
AND
®
•
Documented trial and failure or intolerance to Kadian .
If the above conditions are met, the request will be approved with a 6-month duration; if the above conditions
are not met, the request will be referred to a Medical Director for medical necessity review.
FDA INDIC ATIONS :
Intended for once daily administration indicated for the relief of moderate to severe pain requiring
continuous, around the clock opioid therapy for an e xtended period of time. Efficacy and safety has not been
evaluated for postoperative use. Not intended for prn use.
DOSAGE AND ADMINISTRATION:
All doses are intended to be administered once daily. Ma xim um daily dose which must be adhered to is
1600mg/day. Patients should swallo w capsules intact or to sprinkle the contents on applesauce and
immediately swallo w without chewing.
Conversion from Other Oral Morphine Formulations to Avinza:
Patients receiving other oral morphine formulations may be converted to AVINZA by administering the
patient’s total daily oral morphine dose as AVINZA once-daily. AVINZA should not be given more
frequently than every 24 hours. As with conversion from any oral morphine formulation to another,
supplemental pain medication may be required until the response to the patient’s daily AVINZA dosage has
stabilized (up to 4 days).
Conversion from Parenteral Morphine to Avinza:
Anywhere from 3 to 6 mg of oral morphine may be required to provide pain relief equivalent to 1 mg of
parenteral morphine. Based on this rationale, a reasonable starting dose of AVINZA would be approximately
three times the previous daily parenteral morphine requirement.
Conversion from Other Parenteral or Oral Non- Morphine Opioids to Avinza:
Physicians and other healthcare professionals are advised to refer to published relative potency information,
keeping in mind that conversion rates are only approximate. In general, it is safest to administer half of the
estimated daily morphine requirement as the initial AVINZA dose once per day and then manage insufficient
pain relief by supplementation with immediate-release morphine or other short-acting analgesics.
WARNING:
The beads may not be chewed, crushed or dissolved due to the risk of rapid release and absorption of a
potentially fatal dose of morphine. Patients must not consume alcoholic beverages while on AVINZA
therapy. Additionally, patients must not use prescription or non-prescription medicine containing alcohol
while on AVINZA therapy. Consumption of alcohol while taking AVINZA may result in the rapid release and
absorption of a potentially fatal dose of morphine. The daily dose must be limited to a maxi mum of
1600mg/day. Doses above 1600mg/day contain a quantity of fumaric acid that has not been demonstrated
to be safe, and which may result in serious renal toxicity. The 45, 60, 75, 90, and 120mg capsules are for
use only in opioid-tolerant patients.
REFERENCES:
1. Ballantyne JC, Mao J. Opioid therapy for chronic pain. NEJM 2003;349(20):1943-1953
2. Tassain V, Attal N, Fletcher D, Brasseur L, et al. Long term effects of oral sustained release
morphine on neuropsychological performance in patients with chronic non-cancer pain. Pain
2003;104(2):389-400
3. Portenoy RK; Sciberras A; Eliot L; Loewen G; Butler J; Devane J. Steady-state pharmacokinetic
comparison of a new, e xtende d-release, once-daily morphine formulation, Avinza, and a twice-daily
controlled-release morphine formulation in patients with chronic moderate-to-severe pain. J Pain
Symptom Manage 2002 Apr;23(4):292-300
24
4.
Caldwell JR, Rapoport RJ, Davis JC, et al. Efficacy and safety of a once-daily morphine formulation
in chronic, moderate-to-severe osteoarthritis pain: results from a randomized, placebo-controlled,
double-blind trial and an open-label extension trial. J Pain Symptom Manage (United States), Apr
2002, 23(4) p278-91
5. American Cancer Society (ACS). National Comprehensive Cancer Network (NCCN). Cancer Pain.
Treatment Guidelines for Patients. Version I. January 2001
6. W orld Health Organization. Geneva. 1996. Cancer Pain Relief. Second Edition. W ith a guide to
Opioid Availability.
7. Morphine oral--Elan Corporation. Avinza. Drugs R D (New Zealand), 2002, 3(3) p208-9
8. National Institutes of Heath. National Heart, Lung and Blood Institute. Division of Blood Diseases
and Resources. The Management of Sickle Cell Disease. NIH Publication No. 02-02117. June
1997, Revised June 2002
9. Facts and Comparisons, St. Louis, eFacts 2012 CliniSphere Version ISBN 1-57439-036-8
10. Kadian Product Information. Actavis Elizabeth LLC. July 2012.
11. Avinza Product Information. King Pharmaceuticals, Inc. July 2012.
12. Avinza W arning Letter. Food and Drug Administration. March 2008
Revision/Revie w Date: 11/2015
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the
requested item is medicall y necessar y.
25
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Bactroban®
®
Bactroban (mupirocin calcium ointment) Nasal Ointment
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with a 5 day
duration; if the conditions are not met, the request will be referred
to a Medical Director for medical necessity review.
Revision/Review Date
02/2017
Use is consistent with pre-operative prophylaxis of S. aureus
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
26
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Banzel®
®
Banzel (rufinamide) tablet and oral suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
Patient is 1 year of age or older
N/A
If the conditions are met, the request will be approved with a 12
month duration; if the conditions are not met, the request will be
referred to a Medical Director for medical necessity review.
Diagnosis of Lennox-Gastaut syndrome
AND
Revision/Review Date
02/2017
Patient is currently receiving another anticonvulsant
medication at a therapeutic dosage.
AND
Patient does not have Familial Short QT syndrome
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
27
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Botulinum Toxins A&B
Field Description
OnabotulinumtoxinA (Botox®), IncobotulinumtoxinA (Xeomin®),
AbobotulinumtoxinA (Dysport™), RimabotulinumtoxinB
(Myobloc®)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service(AHFS), United States
Pharmacopeia Drug Information for the HealthcareProfessional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
N/A
N/A
None
If all of the conditions are met, the request will be approved for a 3
month duration. If the conditions are not met, the request will be sent
to a Medical Director/clinical reviewer for medical necessity review.
**The use of these medications for cosmetic purposes is NOT a
covered benefit under the Medical Assistance program.**
Botox® is the preferred botulinum toxin for pediatric patients,
chronic migraine, overactive bladder and hyperhidrosis.
Xeomin is the preferred botulinum toxin for spasmodic torticollis
(cervical dystonia), blepharospasm, upper limb spasticity, and any
other off labeled indication that is supported or recommended by
the medical compendia and standard of care guidelines.
For Approval:
The request is for a FDA approved indication, and/or is used
for a medical condition that is supported by the medical
compendia and/or per Standard of Care Guidelines in each
respective disease state.
Documentation was submitted, that the patient had an
(consistent with pharmacy claims data) adequate trial
(including dates of treatment at maximum recommended doses
of therapy) of standard conventional first line therapy for their
respective disease state (where applicable) as recommended by
the medical compendia and standard of care guidelines and/or
has a documented medical reason (intolerance,
1
28
Revision/Review Date
11/2016
hypersensitivity, contraindication, etc) for not taking standard
conventional first line therapy to treat their medical condition.
If the medication request is for Botulinum toxin type A
(Botox) for treating Chronic Migraines (≥15 days per month
with headache lasting 4 hours a day or longer), the patient has
a documented (consistent with pharmacy claims data)
treatment failure after receiving an adequate trial of beta
blockers (e.g. metoprolol, atenolol, nadolol, propranolol,
timolol), tricyclic antidepressants (e.g. amitriptyline),
Depakote, and topiramate, or a medical reason was submitted
(intolerance, hypersensitivity, contraindication, etc) why
patient is not able to utilize these therapies .
If the medication request is for Botulinum toxin type A
(Botox) for treating Overactive Bladder, the patient has a
documented treatment failure after receiving an adequate trial
(consistent with pharmacy claims data) of at least 2 formulary
medications (e.g. oxybutynin)
If the medication is being requested for an off labeled use that
is recommended by the medical compendia, the patient has a
documented trial/failure (including dates) of Xeomin and/or
has a medical reason (intolerance, hypersensitivity,
contraindication, etc.) for not utilizing Xeomin to manage their
medical condition
Prescribed dosing of medication is within FDA approved
guidelines and/or is supported by the medical compendia as
defined by the Social Security Act and/or per Standard of Care
Guidelines in each respective disease state.
Physican/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
2
29
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Butrans
®
Butrans® (buprenorphine) patches
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a Pharmacist for medical necessity review.
• Must have moderate to severe chronic pain.
AND
• Recent trial of or failure to two preferred long-acting
opioids including: morphine sulfate, methadone or
fentan yl patches
Medical Director/clinical reviewer must override criteria when, in
Revision/Review Date
his/her professional judgement, the requested item is medically
02/2016
necessary.
30
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Celebrex®
Celebrex®(celecoxib) capsules
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PP I), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6 month
duration (refer to individual section below for exact duration of
approval); if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessit y review.
Initial Authorization:
Anticoagulant Therap y:
• Diagnosis of osteoarthritis, rheumatoid arthritis, juvenile
rheumatoid arthritis, or ankylosing spond ylitis
and
• Current therap y with anticoagulant therap y such as warfarin
If the above conditions are met, the request will be approved with a 3month duration; if the above conditions are not met, the request will be
referred to a clinical reviewer for medical necessity review.
Re-evaluation of continued warfarin therap y will be assessed at 3-month
intervals for renewal.
Documented Gastrointestinal Disease (GERD, Erosive Esophagitis, Barret
Esophagus, Zollinger Ellison Disease):
• Diagnosis of osteoarthritis, rheumatoid arthritis, juvenile
rheumatoid arthritis, or ankylosing spond ylitis
and
• Documented gastrointestinal disease of the following conditions:
gastroesophageal reflux disease, erosive esophagitis, Barretts
esophagus, or Zollinger Ellison disease), currently taking either a
proton pump inhibitor or an H2 receptor antagonist.
If the above conditions are met, the request will be approved with a 6
month duration; if the above conditions are not met, the request will be
referred to a clinical reviewer for medical necessity review.
NSA ID Therap y Failure:
• Diagnosis of osteoarthritis, rheumatoid arthritis, juvenile
rheumatoid arthritis, or ankylosing spond ylitis
31
and
• Documented trial and failure with therapeutic prescription doses
or intolerance to at least two formular y nonsteroidal antiinflammatory drugs (NS AIDs).
If the above conditions are met, the request will be approved with a 6month duration; if the above conditions are not met, the request will be
referred to a clinical reviewer for medical necessity review.
Familial Adenomatous Pol yposis (FAP):
• Diagnosis of familial adenomatous polyposis (FAP)
If the above conditions are met, the request will be approved with a 6month duration; if the above conditions are not met, the request will be
referred to a clinical reviewer for medical necessity review.
Primar y D ysmenorrhea:
• Premenopausal female patient
and
• Diagnosis of primar y d ys menorrhea
and
• Documented trial and failure with therapeutic prescription doses
or intolerance to at least two formular y nonsteroidal antiinflammatory drugs (NS AIDs).
If the above conditions are met, the request will be approved with a 5 day
duration; if the above conditions are not met, the request will be referred
to a clinical reviewer for medical necessit y review.
Acute Pain:
• Diagnosis of acute pain
and
• Documented trial and failure with therapeutic prescription doses or
intolerance to at least two formular y nonsteroidal anti-inflammator y
drugs (NSA IDs).
If the above conditions are met, the request will be approved with a 5 da y
duration; if the above conditions are not met, the request will be referred
to a clinical reviewer for medical necessit y review.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
32
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Cholbam™
Cholbam™ (cholic acid)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
MD is a gastroenterologist OR hepatologist
If all of the conditions are met, the request will be approved for a 3 month duration
for the first year of therapy, and then for a 6 month duration after one year of
treatment. If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
33
Other Criteria
Initial authorization:
• Patient has a confirmed diagnosis of:
Bile acid synthesis disorder due to single enzyme defect (SEDs)
OR
peroxisomal disorders (PDs) including Zellweger spectrum
disorders in patients that exhibit manifestations of liver disease,
steatorrhea or complications from decreased fat soluble vitamin
absorption
• Current labs (within 30 days of request) have been submitted for the
following:
ALT/AST
GGT (serum gamma glutamyltransferase)
ALP (Alkaline phosphatase)
Bilirubin
INR
Re-authorization:
• Documentation has been submitted indicating clinical benefit/ liver
function has improved since beginning treatment*
* TREATMENT SHOULD BE DISCONTINUED IF LIVER FUNCTION DOES NOT
IMPROVE WITHIN 3 MONTHS OF STARTING TREATMENT, IF COMPLETE BILIARY
OBSTRUCTION DEVELOPS OR CHOLESTASIS
•
Current labs (within 30 days of request) have been submitted for the
following:
ALT/AST
GGT (serum gamma glutamyltransferase)
ALP (Alkaline phosphatase)
Bilirubin
INR
34
Revision/Review Date
11/2016
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
35
PRIOR AUTHORIZATION CRITERIA
®
CIPRODEX (0.3% ciprofloxacin, 0.1% dexamethasone) Otic Suspension: 7.5mL
FORMULARY STATUS Non-Formulary
PA CRITERIA FOR APPROVAL
Acute otitis externa:
®
• Documented trial and failure, contraindication, or intolerance to ofloxacin otic AND Cortisporin
otic drops.
OR
• Prescribing provider is an ear, eye, nose and throat (EENT) physician
Acute otitis media in patients with tympanostomy tubes:
• Documented trial and failure, contraindication, or intolerance to ofloxacin otic drops
AND
• Approvable for a diagnosis of acute otitis media with tympanostomy tubes
OR
• Prescribing provider is an ear, eye, nose and throat (EENT) physician
If the above conditions are met, the request will be approved with a 3 month duration; if the above
conditions are not met, the request will be referred to a Medical Director for medical necessity
review.
FDA INDICATIONS
Ciprodex is indicated for acute otitis externa and acute otitis media in patients with tympanostomy
tubes.
• Acute Otitis Media in pediatric patient (age 6 months and older) with tympanostomy tubes due
to Staphylococcus aureus, Streptococcus pneumonia, Haemophilus influenza, Moraxella
catarrhalis, and Pseudomonas aeruginosa.
• Acute Otitis Externa in pediatric (age 6 months and older), adult and elderly patients due to
Staphylococcus aureus and Pseudomonas aeruginosa.
DOSAGE AND ADMINISTRATION
• Shake well immediately before use
• Acute Otitis Externa: Pediatric patients (age 6 months and older)- Instill four drops into affected
ear twice daily (about 12 hours apart i.e. 8 AM and 8 PM) for 7 days.
• Acute Otitis Media: Patients 6 months and older- Instill four drops into affected ear twice daily
(about 12 hours apart i.e. 8 AM and 8 PM) for 7 days.
• Patient should lie with affected ear upward and remain in this position for 60 seconds following
application. Drops should be instilled directly into tympanostomy tube (if present) and tragus
should be pumped 5 times to facilitate penetration into the middle ear
REFERENCES
1. Facts and Comparisons, St. Louis, 2011 eFacts CliniSphere Version ISBN 1-57439-036-8.
2. Ciprodex Product Information. Alcon Laboratories, Inc. November 2012.
3. Floxin Product Information. Daiichi-Sankyo. November 2006.
4. Cortisporin Otic Product Information. Monarch Pharmaceutical, Inc. Ma y 2010
5. Rosenfeld RM et al. American Academy of Otolaryngology—Head and Neck Surgery
Foundation Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg 2006
Apr; 134(4 Suppl): S4-23.
6. Sander R. et al. Otitis Externa: A Practical Guide to Treatment and Prevention. American
Family Physician. 2001; 63927-36,941-2.
7. Subcommittee on management of acute Otitis Media. Diagnosis and management of Acute
Otitis Media. Pediatrics. May 2004;113(1451-65).
36
Revision/Review Date: 10/2016
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Physician reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary
37
Field Name
Field Description
Prior Authorization Group COLCRYS®
Desc
Drug(s)
Colcrys® (Colchicine)
Covered Uses
*Medically accepted indications are defined using the following sources: the
Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare
Exclusion Criteria
None
Professional (USP DI) , and the Drug Package Insert).
Required Medical
None
Information
Age
Restrictions
None
Prescriber Restrictions
None
Coverage Duration
Other Criteria
See Specific Indications
CRITERIA FOR APPROVAL:
Acute gout attack:
Is 17 years of age or older
Has a documented history of therapeutic failure, intolerance, or
contraindication to the following at appropriate doses and
frequencies for the treatment of gout:
NSAIDs or COX-2 Inhibitors
AND
Intra-articular or systemic corticosteroids
If the above conditions are met, the request will be approved with up to three
0.6 mg tablets (total 1.8mg) for up to 2 week duration; if the above conditions
are not met, the request will be referred to a Pharmacist for medical necessity
review.
Chronic gout:
•
Is 17 years of age or older
•
Is being prescribed Colcrys in combination with a uric acid
lowering medication (such as allopurinol, probenecid, Uloric, or ColProbenecid) recently
started for the prophylaxis of gout attacks.
If the above conditions are met, the request will be approved for a 6 month
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Familial Mediterranean Fever (FMF):
•
is 4 years of age or older
If the above condition is met, the request will be approved with 6 month
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Review/Revision Date:
10/2016
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
38
1.
2.
3.
4.
Treatment of Acute Gout. UpToDate ONLINE. Updated June 17, 2010. Accessed December 3, 2010.
Prevention of Recurrent Gout. UpToDate ONLINE. Updated October 7, 2010. Accessed December 16,
2010.
Facts and Comparisons, St. Louis, 2014 eFacts CliniSphere Version ISBN 1-57439-036-8.
®
Colcrys . Prescribing information. Takeda Pharmaceuticals. June 2012.
Revision/Revie w Date: 12/2014
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the requested item
is medicall ynecessar y
39
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Crinone®
Crinone® (micronized progesterone)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criterion is met, the request will be approved for 2 boxes (15 single use
applicators per box) per 30 days until the end of pregnancy if the diagnosis is short
cervix, or for up to six doses if the diagnosis is secondary amenorrhea;. If the
criterion is not met, the request will be referred to a Clinician for medical necessity
review.
Initial Authorization:
•
Documented ultrasound of transvaginal cervical length
(TVCL) ≤ 25mm between weeks 17 and 24 of gestation.
AND
Revision/Review Date
07/2016
OR
•
Crinone 8% is not being used for infertility.
•
Patient has dx of secondary am enorrhea
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
40
P rior Authorization Group Description
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical I nfor matio n
Age Restrictions
Prescriber Restrictions
Coverage Dur atio n
Other Criteria
Cystic Fibrosis Agents
Aztreona m l ysine (Cayston®), dornase alfa
(Pul mozyme®), tobra mycin ( T obi®, T obi Podhaler®),
ivacaftor (Kalydeco®, Kalyde co Granules®),
Lu macaftor/Ivacaftor (Orka mbi®)
Medically accepted indicatio ns are defined using the
follo wing sources: the Food and Drug
Ad ministration (FD A), Micro medex, American
Hospital For mular y Service (AHFS), United States
Phar macopeia Drug Infor mati on for the Healthcare
Professional (USP DI), the Drug Package Insert
(PPI), and/or per standard of care guidelines.
See “Other Criteria”
See “Other Criteria”
See “Other Criteria”
MD is pul monologist
If all o f the conditions are met, for Kalydeco® and
Orka mbi® the initial request will be 3 mo nths, all
other med s will be approved with a 6 -mo nth
duration. Reauthorization for Kal ydeco® and
Orka mbi® will be 6 months. If all of the criteria are
not met, the request is referred to a Medical
director/clinical revie wer for medical necessit y
revie w.
CR ITER IA FOR THE USE OF KALYDECO® (IVAC AFTOR) IN
THE TRE ATMENT O F CYSTIC FIB ROSIS :
•
•
•
•
•
•
•
•
41
T he medication is for the treatment of a CF
patient who has an FD A approved
indication for treat ment o f the patient ’s
genot ype (there is a FD A clear ed CF
mutation test that can be used to deter mine
genot ype if unkno wn).
Copy o f the FDA-cleared CF mutation test
has been provided with request
T he patient is 2 years or older.
For patients age 2 -6, docu mentation o f the
patient ’s weight
T he patient is not a ho mozygo us for the
F508del mutation in the c ystic fibrosis
trans me mbrane conductance r egulator
(CFT R) gene.
Baseline FEV1 has been sub mitted with
request (within 90 da ys of req uest)
Docu mentation o f current ALT /AST levels (
within -90 days of request). (Ivacaftor is
contraindicated for ALT and AST levels 5
ti mes over upper li mit o f nor mal. If ALT
and AST levels are 5 times o ver the upper
li mit o f nor mal or higher, ivac aftor sho uld
not be started until the levels are below this
range.)
T he medication is being prescribed at a
dose that is within FD A approved
guidelines.
Continuation o f therap y for KALYDECO®
( IVAC AFTOR):
•
•
•
•
•
Docu mentation has been sub mitted that
patient has obtained clinical benefit fro m
med ication (i.e. i mprove me nt in FEV1,
B MI, decrease in number or frequency o f
pul mo nar y exacerbations, or imp rove ment
in quality of life)
Repeat FEV1 ( within 90 days of request)
Repeat ALT /AST (within 90 da ys of
request) , and results are not 5 ti mes the
upper li mit o f nor mal or higher
T he medicatio n is being used for an FD A
approved indication at an FDA approved
dose
T he prescriber is a pul monologist
CR ITER IA FOR THE USE OF TOB I® ( TOBR AMYC IN)
PRODUCTS IN THE TREATMENT OF CYSTIC F IBROS IS:
•
•
T he medication is being prescribed for the
treat ment of a c ystic fibrosis p atient
colonized with Pseudo mo nas aeruginosa.
T he medication is being prescribed at a
dose that is within FD A approved
guidelines.
CR ITER IA FOR THE USE OF PU LMOZYME® (DORNASE
ALFA) IN THE TRE ATMENT O F CYSTIC FIBROS IS :
•
•
•
T he medication is not being used as
mo notherap y.
T he patient is 5 years or older.
T he medication is being prescribed at a
dose that is within FD A approved
guidelines.
CR ITER IA FOR THE USE OF C AYSTON® ( AZTREONAM
LYS INE) IN THE TRE ATMENT O F CYSTIC F IBROS IS:
•
•
T he medication is being prescribed for the
treat ment of a c ystic fibrosis p atient
colonized with Pseudo mo nas aeruginosa.
T he medication is being prescribed at a
dose that is within FD A approved
guidelines.
CR ITER IA FOR THE USE OF ORKAMB I ®
( LUM ACAFTOR/ IV AC AFTOR) IN THE TRE ATMENT O F
CYSTIC FIBROS IS :
•
•
•
•
42
T he patient is 12 years o f age or older
T he patient IS ho mozygous for the F508del
mutation in the the cystic fibro sis
trans me mbrane conductance r egulator
(CFT R) gene.
Copy o f the FDA-cleared CF mutation test
has been provided with request
Baseline FEV1 has been sub mitted with
•
request (within 90 da ys of
request)Documentation of curr ent
ALT /AST and bilirubin levels ( within -90
days of request)
T he medication is being prescribed at a
dose that is within FD A approved
guidelines.
Continuation o f therap y for OR KAMB I ®
( LUM ACAFTOR/ IV AC AFTOR):
•
•
•
•
•
Review/Revision Date 2/2016
43
Docu mentation has been sub mitted that
patient has obtained clinical benefit fro m
med ication (i.e. i mprove me nt in FEV1,
B MI, decrease in number or frequency o f
pul mo nar y exacerbations, or imp rove ment
in quality of life)
Repeat FEV1 ( within 90 days of request)
Repeat ALT /AST (within 90 da ys of
request) , and results are not 5 ti mes the
upper li mit o f nor mal or higher
T he medicatio n is being used for an FD A
approved indication at an FDA approved
dose
T he prescriber is a pul monologist
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
02/2017
Field Description
®
Danocrine (danazol)
®
Danocrine (danazol) capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
Pregnancy- see “other criteria”
See “other criteria”
N/A
See “other criteria”
If the criteria are met, the request will be approved with a 6 month
duration for generic medication; if the criteria are not met, the
request will be referred to a Medical Director for medical
necessity review.
ENDOMETRIOSIS
Diagnosis of endometriosis
AND
Documented trial and failure, intolerance or documented
medical reason for not using first line therapy of oral
contraceptive therapy.
AND
Prescribing physician is a gynecologist.
AND
Negative pregnancy test
FIBROCYSTIC BREAST PAIN DISEASE
Diagnosis of fibrocystic breast disease.
AND
Documented trial and failure, intolerance or documented
medical reason for not using first line therapy of analgesics
including acetaminophen and NSAIDs.
AND
Prescribing physician is a gynecologist.
AND
Negative pregnancy test
HEREDITARY ANGIOEDEMA:
Diagnosis of hereditary angioedema.
AND
Negative pregnancy test
44
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
45
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
®
DDAVP
DDAVP® (desmopressin) Tablets & Nasal Spra y/Nasal Solution
(Rhinal Tube)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PP I), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 12 month
duration. If the conditions are not met, the request will be sent to a
Medical Director/clinical reviewer for medical necessity review.
Tablets
• Diagnosis of primar y nocturnal enuresis in children 6 years of
age and older.
OR
• Diagnosis of central cranial (neurogenic) diabetes insipidus.
NOTE: Tablet formulation w ill process at the point-of-sale for
members ≥6 years old.
Nasal Spray and Rhinal Tube (nasal solution):
• Diagnosis of central cranial (neurogenic) diabetes insipidus.
Revision/Review
Date 02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
46
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Diamox Sequel
®
Diamox Sequel® (acetazolamide sustained release) capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 6 month
duration; if the above conditions are not met, the request will be
referred to a Medical Director/clinical reviewer for medical necessity
review.
Initial authorization:
• Diagnosis of chronic simple open angle glaucoma, or
secondar y glaucoma.
AND
• Documented trial and failure with therapeutic doses or
intolerance to acetazolamide immediate release tablets.
Medical Director/clinical reviewer must override criteria when, in
Revision/Review Date his/her professional judgement, the requested item is medically
02/2016
necessary.
47
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
02/2016
Field Description
Diclegis®
Diclegis® (doxylamine/pyridoxine HCL)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
Member is a male
See “other criteria”
N/A
Prescriber must be an obstetrician/gynecologist
If the above conditions are met, the request will be approved for 6 (six)
months. If the conditions are not met, the request will be sent to a
Medical Director/clinical reviewer for medical necessity review.
Initial authorization:
• The indicated diagnosis of nausea and vomiting due to pregnancy.
AND
• The member has had an adequate trial and failure with one (1) of
the agents
o Ondansetron, pyridoxine, vitamin B6, metoclopramide
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
48
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Dostinex®
Dostinex® (cabergoline) tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 12
month duration; if the above conditions are not met, the request will be
referred to a Medical Director/clinical reviewer for medical necessity
review.
Initial authorization:
Diagnosis of hyperprolactinemia.
AND
Revision/Review Date
2/2017
Documented trial and failure with therapeutic doses or intolerance
to bromocriptine therapy.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
49
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Elmiron
Field Description
®
Elmiron® (pentosan polysulfate sodium)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization
Diagnosis of interstitial cystitis
***Please Note: Patients should be evaluated at 3 months and may be
continued an additional 3 months if there has been no improvement and
if there are no therapy-limiting side effects. The risks and benefits of
continued use beyond 6 months in patients who have not responded
is not yet known.
Revision/Review
Date 10/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
50
Entresto
Angiotensin II Receptor Blocker - Neprilysin Inhibitor Combination (ARNi)
Covered Uses
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
Patient is 18 and older
Prescriber
Restrictions
Prescribed by (or in consultation with) a cardiologist or specialist in cardiac care
Coverage
Duration
If these criteria are met, then an initial 12 months duration will be authorized.
Upon reauthorization, if criterion is met, 12 months duration will be authorized.
51
AUTHORIZATION:
Other Criteria
Patient is diagnosed with NYHA Class II – IV Heart Failure with reduced ejection fraction
(HFrEF) < 40%
Patient has tolerated anACEI or ARB (without evidence of angioedema) and Entresto
will replace the ACEI or ARB
• Female patients have a negative pregnancy test result within previous 30 days of request
• Patient does not have severe hepatic impairment (Child Pugh Class C)
• Used in conjunction with other heart failure therapies such as a beta blocker, aldosterone
antagonist, or combination therapy of hydralazine plus isosorbide dinitrate).
• If patient is diabetic, must not be currently taking an aliskiren-containing medication (ie
Tekturna or Tekturna HCT)
RE - AUTHORIZATION:
• Documentation Requirements (e.g. Labs, Medical Record, Special Studies):
- Positive response to therapy
- Negative pregnancy test result (females) within previous 30 days of request
- No evidence of severe hepatic impairment (Child Pugh Class C)
• Used in conjunction with other heart failure therapies such as a beta blocker, aldosterone
antagonist or combination therapy of hydralazine plus isosorbide dinitrate)
Review Date:
September 2016
• If patient is diabetic, must not be currently taking an aliskiren-containing medication (ie
Tekturna or Tekturna HCT)
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
52
Field Na me
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Infor mation
Age Restrictio ns
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Entocort EC
®
®
Entocort EC (budesonide)
Medically accepted indications are defined using the follo wing sources: the
Food and Drug Ad ministration (FDA), Micro medex, Ameri can Hospital
For mular y Service (AHFS), United States Phar macopeia Drug Infor mation
for the Healthcare Professiona l (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved for up to a 16 week
duration; if the criteria are not met, the request will be referred to a clinical
reviewer for medical necessity review.
Initial Aut horization:
• Diagnosis of mild to moderate active or remissive
Crohn’s disease involving the ileum and/or the
ascending colon.
AND
•
Prescription written by a gastroenterologist.
AND
Revision/Review Date
07/2016
• Documented trial and failure with 16 weeks of
therap y at therapeutic doses of at least two first-line
therapies of sulfasalazine, mesalamine and
prednisone.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
53
P rior Authorization Group: Erythropoiesis-Sti mulat ing Agents
Drug(s): Darbepoetin Alfa-Polysorbate 80 (Aranesp), Epoetin Al fa (P rocrit)
***AR ANESP is preferred agent for Chronic Kid ney Diseas e and for patients receiving che mother apy that are 18
years o f age or older. *****
Covered Uses: Medically ac cepted indications are defined using the follo wing sources: t he Food and Drug
Ad ministration (FD A), Micr o medex, American Hospital For mular y Service ( AHFS), Unite d States
Phar macopeia Dr ug I nfor mati on for the Healthcare Professional (USP DI), the Drug Package Insert (P P I).
Criteria:
All la b results must be sub mitted w ithi n 30 days of the request
• He matocrit, Serum ferritin le vel (nor mal is greater tha n 100n g/ ml), T ransferrin satur atio n ( T SAT )
(nor mal is greater than 20%), Serum iron, Total Iron Binding Capacity (TIB C),Vitamin B 1 2 level,
Folate level, Glo merular Filtration Rate (GFR) ( for chronic kidney disease ane mia), and
Erythopoietin level ( for HIV related ane mia)
****Procrit requires documentation (consistent with pharmacy claims data, OR f or new
members to the health plan consistent with medical chart history) of adequate trials and/or has
a documented medical reason (e.g. intolerance or hypersensitivity) for not utilizing ARANESP
w hen appropriate****
1. Initial approval for ane mia of P r e-di al ysi s chronic kid ne y disease or ane mia due to che mo t her ap y:
• He moglobin less than 10 g/dl OR if the me mber is ne w to the health plan and was receiving therap y at
the previous health plan the me mber has a docu mented (sub mitted lab result dated withi n 30 days o f
request) he mo globin <12 g/d L.
• If the me mber has ane mia due to Pre-dialysis chronic kidney disease then documentatio n must be
sub mitted that the me mber has a glo mer ular filtration rate (GFR) less than 60 ml/ min/1.73 m2 for > 3
mo nths OR meets the criteria for chronic kidney disease as defined b y the National Kid ne y Foundatio
n.
• If the me mber has lo w B 12 levels and/or Folate levels the n docu mentation sub mitted that indicates
the me mber is or will be prescribed appropriate supple mentation.
• If the me mber is iron deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• T he medicatio n is being reco mmended and/or prescribed at an FD A appropriate dose for indication.
• If the request is for P rocrit, the provider sub mitted a documented medical reason (i.e. intolerance) wh y
it is medically necessar y to utilize P rocrit (instead o f Aranesp) for the treat ment o f CKD ane mia and
for patients with chemotherapy-induced ane mia that are 18 years o f age or older.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 mont h ma y be
authorized if the me mb er is functionally iro n deficient ( ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate deficient; if all of the abo ve criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
Reauthorizatio n:
• If the me mber has been receiving therap y and their hemo globin is less than 12 g/d L and one of
the follo wing apply (if applica ble):
a) T he order ed dose is reduced by 25 % o f previous dose if the rate of Hgb increase was great er
than 1g/dL o ver a t wo week period OR the Hgb is increasing and approaching 12 g/d L.
b) T he ordered dose is increased fro m the previous dose if the patients Hgb impro ved less than
1g/dL over a 4 to 6 week perio d and iron stores were adequate.
c) An increase in dose does not occur more tha n once per month (b y 25%)
• If the me mber is iron deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• If the me mber was deficient in either B 12 or folate and is NOT receiving supple mentatio n, r epeat
B 12 and Folate labs are required (within 30 da ys of request).
54
•
T he medicatio n is being reco mmended and/or prescribed at an FD A appropriate dose for
indication.
• If the request is for P rocrit, the provider sub mitted a documented medical reason (i.e. intolerance)
wh y it is medically necessar y t o utilize P rocrit (instead o f Aranesp) for the treat ment o f CKD
ane mia and for patients with che motherapy-induced ane mia that are 18 years o f age or older.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 mont h ma y be
authorized if the me mb er is functionally iron deficient (ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate deficient; if all of the abo ve criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
2. Initial appr o val for ane mia due to Zido vudin e-tr eated HI V infected patients:
• He moglobin less than 11 g/dl OR if the me mber is ne w to the health plan and was receiving therap y at
the previous health plan the me mber has a docu mented (sub mitted lab result dated withi n 30 days o f
request) he mo globin <12 g/d L.
• Patient has been receiving a highly reactive antiretro viral therap y (H AART ) regi men for the past 35
days.
• Docu mentatio n, within 30 days of the request, that the patie nt has an erythropoietin level < 500
units/ mL.
• If the me mber has lo w B 12 levels and/or Folate levels the n docu mentation sub mitted that indicates
the me mber is or will be prescribed appropriate supple mentation.
• If the me mber is iron deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• T he medicatio n is being reco mmended and/or prescribed at an FD A appropriate dose for indication.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 mont h ma y be
authorized if the me mb er is functionally iro n deficient ( ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate deficient; if all of the abo ve criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
Reauthorizatio n:
• If the me mber has been receiving therap y and their hemo globin is less than 12 g/d L and one of
the follo wing apply (if applica ble):
a) T he order ed dose is reduced by 25 % o f previous dose if the rate of Hgb increase was great er
than 1g/dL o ver a t wo week period OR the Hgb is increasing and approaching 12 g/d L.
b) T he ordered dose is increased fro m the previous dose if the patients Hgb impro ved less than
1g/dL over a 4 to 6 week perio d and iron stores were adequate.
c) An increase in dose does not occur more tha n once per month
• If the me mber is iron deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• If the me mber was deficient in either B 12 or folate and is NOT receiving supple mentation, r ep eat
B 12 and Folate labs are required (within 30 da ys of request).
• T he medicatio n is being reco mmended and/or prescribed at an FD A appropriate dose for
indication.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 mont h ma y be
authorized if the me mb er is functionally iro n deficient ( ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient and/or folate deficient; if all of the abo ve criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
55
3. Initial appr o val for ane mia due to Ribavirin Ind uced Ane mia:
He moglobin less than 11 g/dl OR if the me mber is ne w to the health plan and was receiving therap y at
the previous health plan the me mber has a docu mented (sub mitted lab result dated withi n 30 days o f
request) he mo globin <12 g/d L.
• Patient is currently receiving ribavirin ther ap y and initiated therap y ≤
20 weeks ago.
• If the me mber has lo w B 12 levels and/or Folate levels the n do cu mentatio n sub mitted that indicates
the me mber is or will be prescribed appropriate supple mentation.
• If the member is iro n deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• T he medication is being reco mmended and/or prescribed at an FD A appropriate dose for indication.
•
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 month may be
authorized i f the me mber is functionally iron d eficient (ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate defici ent; i f all o f the above criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
Reauthorizatio n:
• If the me mber has been receiving therap y and their hemo globin is less than 12 g/d L and one of
the follo wing apply (if applica ble):
a) T he ordered dose is reduced by 25 % o f previous dose if the rate of Hgb increase wa s greater
than 1g/dL over a t wo we ek period OR the Hgb is increasing and approaching 12 g/d L.
b) T he ordered dose is increased fro m the previous dose if the patients Hgb i mproved less than
1g/dL over a 4 to 6 week perio d and iron stores were adequate.
c) An increase in dose does not occur more than once per month.
• If the member is iron deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• If the me mber was deficient i n either B 12 or folate and is NOT receiving supplementation, r epeat
B 12 and Folate labs are required (within 30 da ys o f request).
20 weeks ago, or if
• T he me mber is currently receiving ribavirin therap y that was initiated ≤
be yo nd week 20 of ribavirin therap y, docu mentation sub mitted indicates a dosage reduction of
ribavirin to 600 mg/day a fter week 20 but the me mber still became ane mic.
• T he medication is being reco mmended and/or prescribed at an FD A appropriate dose for
indication.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 month may be
authorized i f the me mber is functionally iron d eficient (ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate defici ent; i f all o f the above criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
4. Initial app roval for Allo ge nic B lood T ransfusio n S ur ger y P atients:
•
•
•
•
He moglobin less than 13g/dl a nd greater than 10g/dl.
T he patient has nor mal iro n st ores and is, or will be, receiving adequate iron supple mentation.
T he patient is scheduled for an elective, non-cardiac, nonvascular surger y.
T he medication is being reco mmended and/or prescribed at an FD A appropriate dose for indication.
If all o f the above conditions are met, the request will be approved with a 1-month duration; if all o f the above
criteria are not met, the reques t is referred to a Medical Director for medical necessity revie w.
5. Initial approval for ane mia due to Other Medicall y Accep t ab le Indications:
He moglobin less than 11g/dl OR if the me mber is ne w to the health plan and was receiving therap y at
the previous health p lan the me mber has a docu mented (sub mitted lab result dated withi n 30 days o f
request) he mo globin <12 g/d L.
• If the me mber has lo w B 12 levels and/or Folate levels the n docu mentatio n sub mitted that indicates
the me mber is or will be prescribed appropriate supple mentation.
•
56
•
•
If the member is iro n deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
T he medication is being reco mmended and/or prescribed at an FD A appropriate dose for indication.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 month may be
authorized i f the me mber is functionally iron d eficient (ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate defici ent; i f all o f the above criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
Reauthorizatio n:
• If the me mber has been receiving therap y and their hemo globin is less than 12 g/dL and one of
the follo wing apply (if applica ble):
a) T he ordered dose is reduced by 25 % o f previous dose if the rate of Hgb increase wa s greater
than 1g/dL over a t wo we ek period OR the Hgb is increasing and approaching 12 g/d L.
b) T he ordered dose is increased fro m the previous dose if the patients Hgb impro ved less than
1g/dL over a 4 to 6 week perio d and iron stores were adequate.
c) An increase in dose does not occur more than once per month.
• If the member is iron deficient , the me mber is in the process of receiving either oral or IV iron
supple mentation or the treat ment plan is to start iron therap y.
• If the me mber was deficient i n either B 12 or folate and is NOT receiving supplementation, r epeat
B 12 and Folate labs are required (within 30 da ys o f request).
• T he medication is being reco mmended and/or prescribed at an FD A appropriate dose for
indication.
If all o f the above conditions are met, the request will be approved for up to a 3-month duration if the me mber is
not functionally iron deficient (ferritin concentration is > 100-800 ng/ mL and the transferrin saturation are > 2055%) and not vita min B -12 deficient and not folate deficient, OR a te mporar y supply o f up to 1 month may be
authorized i f the me mber is functionally iron d eficient (ferritin concentration < 100 ng/ mL and/or percentage
transferrin saturation < 20%) and/or vita min B -12 deficient a nd/or folate defici ent; i f all o f the above criteria are
not met, the request is referred to a Medical Director for medical necessity revie w.
REVIEW D AT E: 11/2014
Associated Policy: Prior Authorization of Medications 236.200
57
Field Name
Prior Authorization
Group
Description
Drugs
Covered Uses
Exclusion Criteria
Field Description
Daraprim®
Daraprim® (pyrimethamine)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
Patients with documented megaloblastic anemia due to folate deficiency.
Required Medical
Information
Age Restrictions
Prescriber Restrictions
If diagnosis is toxoplasmosis, and request is for PRIMARY
PROPHYLAXIS, a medical reason was provided as to why patient is
not able to use trimethoprim-sulfamethoxazole
If diagnosis is toxoplasmosis, request is for TREATMENT and will be
used in combination with a sulfonamide. If patients are allergic to
sulfa, densitization should be attempted or another preferred
regimen can be used
If request is for CHRONIC MAINTENANCE treatment of
toxoplasmosis, and patient was NOT TREATED with a
pyrimethamine regimen, a medical reason was provided why
patient is not able to continue with alternative regimen for
maintenance
If diagnosis is isosporiasis in an HIV patient, a medical reason was
provided why patient is not able to use trimethoprimsulfamethoxazole to manage their condition
If diagnosis is pneumocystis pneumonia in an HIV patient,
documentation was submitted with a medical reason for not
utilizing trimethoprim-sulfamethoxazole or dapsone to manage
their condition If diagnosis is prophylaxis of malariadocumentation was submitted with a medical reason as to why patient
is not able to use all other first line malaria agents, as resistance to
pyrimethamine is prevalent worldwide, and it is not suitable as a
prophylactic agent for travelers to most areas.
N/A
Prescriber must be an appropriate specialist or documentation has been provided
that prescriber has consulted with an appropriate specialist (i.e. infectious disease,
OB/GYN)
58
Coverage Duration
Other Criteria
Revision/Review Date
11/2016
If all of the conditions are met, PRIMARY PROPHYLAXIS requests will be approved for 3
months, TREATMENT requests will be approved for 6 weeks, and CHRONIC
MAINTANENCE requests will be approved for 3 months at a time.. If the conditions
are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
N/A
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
59
PERFORMRX PRIOR AUTHORIZATION CRITERIA
EPOGEN (epoetin alfa): 2,000 units/ml, 3,000 units/ml, 4,000 units/ml, 10,000 units/ml, 20,000 units/ml, 40,000
units/ml
®
P A Criteria f or Approval Administration of Epogen in ESRD P atients Treated at Dialysis Centers.
• Patient is being treated at a dialysis center.
AND
• T he necessary lab work (listed below) is documented on the PA form or submitted with request;
-Hemoglobin – last 3 months results (to determine rolling Hgb)
-Hematocrit – last 3 months results (to determine rolling Hct)
-Serum ferritin – within past 2 months
-T ransferrin saturation – within past 2 months
-Serum iron – within past 2 months.
-Total Iron Binding Capacity (TIBC) – within past 2 months
-Vitamin B12 and Folate levels – within past 2 months
-History of Epogen usage
If all of the above criteria are not met then the request is referred to a Medical Director/clinical reviwer for medical necessity
review. If all of the above conditions are met, place the patient into one of the following categories based on diagnosis:
Place the patient into one of the following categories
-Epogen treatment naïve with normal iron status (Section A)
-Epogen treatment naïve with iron deficiency (Section B)
-Receiving Epogen treatment with normal iron status (Section C)
-Receiving Epogen treatment with iron deficiency (Section D)
Section A: Epogen treatment naïve w ith normal iron status (TSAT > 20% and Ferritin > 100ng/ml)
• T he patient has a hemoglobin <10g/dL and/or hematocrit <33%.
• Epogen dosing is being initiated at 100 units/kg 3 times a week (TIW) or less.
If all of the above conditions are met, the request will be approved with a 3-month duration, if all of the above criteria are
not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
Section B: Epogen treatment naïve w ith iron deficiency (TSAT < 20% and Ferritin < 100ng/ml)
• T he patient has a hemoglobin <10g/dL and/or hematocrit <33%.
• T he patient is in the process of receiving iron supplementation (i.e. 25-125 mg IV once weekly or >200 mg elemental
iron orally daily).
• T he patient’s Epogen dose is less than or equal to 100 units/kg- 3 times a week (T IW).
If all of the above conditions are met, the request will be approved with a 2-month duration to allow follow up on outcome
of iron supplementation; if all of the above criteria are not met, 50,000 units of Epogen per month will be authorized and
the request is referred to a Medical Director/clinical reviewer for medical necessity review.
Section C: Existing therapy w ith Epogen with normal iron status (TSAT > 20% and Ferritin > 100ng/ml)
• T he patient has a hemoglobin <12g/dL and/or hematocrit <36%
• T he patient’s hematocrit increased greater than 8 percentage points in the past month, or Hgb increased by more than
1g/dl in a two week period, after starting current dose and the Epogen dose has been reduced by at least 25% compared
to the last course of therapy and therapy withheld for 1-2 weeks.
• If the patient’s Hgb/Hct is below target range after receiving therapy for at least 4 weeks and the dose is the same as
last month or was increased by no more than 25% of the previous dose.
• If the patient’s current Epogen dose was started less than 8 week ago and their hematocrit has increased by less than 4
percentage points over the past 2 weeks or less than 8 percentage points over the last 4 weeks and the ordered dose o
Epogen is the same as last month or less.
• If the patient’s hemoglobin is in target range (10-12g/dL) and the ordered dose is either reduced or the same dose as
the previous month.
• T he ordered dose is not an increase in dosage that is with5i560
n535 4 weeks of last dosage change or start of therapy with a
•
•
medical reason being provided for an early increase.
If the patient’s hemoglobin exceeds 12 g/dl despite dose reduction, the Epogen dose was withheld until hemoglobin
dropped to 12g/dL or less and the ordered Epogen dose was reduced by 25%.
If the dose is greater than 300 units/kg T IW, then documentation (within the past 2 months) of iron maximum
supplementation, documentation of patients TSAT >20% and ferritin >100ng/ml and documentation (within the past 2
months) was submitted from a hematologist recommending the current dose if all reversible causes for Epogen
resistance have been ruled out.
If all of the above conditions are met, the request will be approved with a 3-month duration, if all of the above criteria are
not met then the request is referred to a Medical Director/clinical reviewer for medical necessity review.
Section D: Existing therapy on Epogen w ith iron deficiency (TSAT < 20% and Ferritin < 100ng/ml)
• T he patient has a hemoglobin <12g/dL and/or hematocrit <36%
• T he patient is currently in the process of receiving iron supplementation (i.e. 25-125 mg IV once weekly or >200 mg
elemental iron orally daily).
• T he ordered dose is an increase in dosage that is within one-month time of last dosage change or start of therapy, and
a medical reason was provided for an early increase.
• T he Epogen dose is less than or equal to 100 units/kg TIW.
If all of the above conditions are met, the request will be approved with a 2-month duration to allow follow up on outcome
of iron supplementation; if all of the above criteria are not met then the request is referred to a Medical Director/clinical
reviewer for medical necessity review.
DOSAGE AND ADMINISTRATION:
CKD patients:
General Therapeutic Guidelines in CKD Patients for Epoetin Alfa
Starting dose
(initiate Epogen treatment when the hemoglobin level is
less than 10g/dL)
Adults: 50 to 100 Units/kg TIW
Pediatric: 50 Units/kg TIW
Maximum dose – (with normal Iron stores)
Intravenous administration
300 units/kg T IW†
**Doses greater than maximum doses require hematologist
consultation and recommendation.
†max dose for the treatment of anemia cause by zidovudine
in HIV -infected patients. There are no well-established
maxi mum doses for the other approved indications.
Reduce dose by 25% when
2) Hgb increases by more than 1 g/dl in 2-week period
Dose should be temporarily withheld when
Hgb exceeds 12 g/dl and until Hgb falls to 11g/dl. Therapy
should be reinitiated at a dose approximately 25% below
the previous dose.
1) Hgb remains < 10 g/dl
AND
2) Hgb increases by less than 1 g/dl after 4 weeks of
therapy
Individualize to achieve and maintain the lowest Hgb level
sufficient to avoid the need for RBC transfusion and not to
exceed 12 g/dl.
10 to 12 gm/dl
Increase dose up to 25% of previous dose if:
Maintenance dose
Suggested target hemoglobin
•
Dose adjustment should not be made more frequently than once a month, unless clinically indicated.
Revision/Review Date: 4/2016
NOTE: P hysician/clinical review er must override criteria when, in his/her prof essional judgement, the requested item is
4
5n
6 ecessary.
medically61
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Agents to Treat Gaucher’s Disease
Cerdelga ® (Eliglustat Tartrate), Cerez yme ® ( Imiglucerase), Vpriv®
(velaglucerase alfa), Elelyso ® (taliglucerase alfa), Zavesca® (miglustat)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), and the Drug
Package Insert (PP I).
None
See “Other Criteria”
See “Other Criteria”
MD is a specialist in treatment of Gaucher’s Disease (hematologist or
geneticist), or is in consultation with a specialist including
endocrinologists, hematologists, and geneticists.
If all of the conditions are met, the request will be approved with 6month duration. If all of the criteria are not met, the request is referred to
a clinical reviewer for medical necessity review.
Initial Authorization:
Cerez yme ®, Vpriv®, or Elel yso ® initial authorization:
• Patient has a confirmed diagnosis of Gaucher’s disease, t ype
1 (GD1)
• Request is for an FDA approved dose
Zavesca® initial authorization:
• Patient has a confirmed diagnosis of Gaucher’s disease, t ype
1 (GD1)
• Documentation has been provided with medical reason wh y
patient is unable to use Cerez yme®, Vpriv®, or Elelyso® to
manage their medical condition
• Request is for an FDA approved dose
Cerdelga ® initial authorization:
• Patient is 18 years of age or older.
• Patient has a confirmed diagnosis of Gaucher’s disease, t ype
1 (GD1) and is a CYP2D6 extensive metabolizer (EM),
intermediate metabolizer (IM) or poor metabolizer (PM), as
detected b y an FDA-approved test.
• Patient is not concomitantly taking a moderate or strong
CYP3A inhibitor (e.g. ketoconazole, fluconazole) or a Class
IA or Class III antiarrh ythmic.
• Patient has no pre-existing cardiac disease or long QT
syndrome.
• The patient has a documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with
medical chart history) adequate trial (including dates and doses)
62
of Cerez yme®, Vpriv ®, or Zavesca ®, or has a documented
medical reason for not utilizing these therapies to manage their
condition.
Re-Authorization criteria for all agents:
• Documentation has been provided that patient has obtained
clinical benefit from medication (e.g. increased platelet count,
improvement in anemia, PFT’s, improvement in radiographic
scans, improved qualit y of life,)
• Request is for an FDA approved dose
Revision/Review
Date 4/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
63
Field Name
Prior Authorization Group
Description
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
GONADOTROPIN RELEASING HORMONE AGONISTS (GNRH)
Degarelix Acetate (Firmagon), Goserelin Acetate (Zoladex), Histrelin Acetate
(Supprelin LA, Vantas), Leuprolide Acetate (Lupron, Eligard), Lupron Depot,
Lupron Depot-Ped, Nafarelin (Synarel), Triptorelin Pamoate (Trelstar Depot,
Trelstar LA, Trelstar Mixject), and newly marketed GnRH agonists.
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), and/or per the National
Comprehensive Cancer Network (NCCN), the American Society of Clinical
Oncology (ASCO), the American College of Obstetricians and Gynecologists
(ACOG), or the American Academy of Pediatrics (AAP) standard of care guidelines.
None
None
None
None
If all of the conditions are met, the request will be approved for up to 6 months for
treatment of prostate/breast cancer, endometriosis or central precocious puberty and
up to 3 months or as recommended per FDA approved indications and/or as defined
by the medical compendium as defined above and/or per the NCCN, ASCO, ACOG,
or AAP standard of care guidelines. If the conditions are not met, the request will be
sent to a Medical Director/Clinical Reviewer for medical necessity review.
INIT IAL AUT HORIZAT ION
• If the medication request is for the treatment of central precocious puberty
(CPP ) patient may be authorized either Lupron-Depot Ped® OR Supprelin
LA® for the treatment of the condition as long as there is a clinical diagnosis
of CP P with onset of secondary sexual characteristics less than age 8 in
females and age 9 in males and ALL of the following apply to the patient:
1. Diagnosis is confirmed by a pubertal response to a GnRH stimulation test
and/or measurement of gonadotropins (FSH/LH), and bone age advanced 1
year beyond chronological age.
If basal levels of LH are markedly elevated [e.g. more than 5mlU/ml (where
IU- International units)] in a child with precocious puberty, then a diagnosis of
Gonadotropin Dependent Precocious Puberty (GDPP) can be made without
proceeding to a GnRH stimulation test.
Patients with low or intermediate basal levels of LH should have a GnRH
stimulation test to clarify the diagnosis.
2. There are documented baseline evaluations (including ultrasound, CT , MRI,
and laboratory levels) to rule out a tumor.
•
For all other indications, if the medication request is for any other GnRH
agonist other than Lupron®, the patient has a documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent
with medical chart history) treatment failure after receiving an adequate trial
(including dates of 3 months or more of therapy) of Lupron® and/or has
another documented medical reason (intolerance, hypersensitivity,
64
contraindication, etc.) for not utilizing Lupron® to treat their medical
condition.
If the diagnosis is HER2 positive breast cancer, and the request is for
Zoladex (goserelin), no prior trial of a GNRH is required for that patient.
•
• If the medication request is for the treatment of advanced prostate cancer
(Stage III or Stage IV) then the patient must be an adult male (≥18 y/o).
•
If the medication request is for the treatment of a confirmed diagnosis of
endometriosis, the patient is an adult female (≥18 y/o) who does not have
documented Osteoporosis, and documentation has been provided that the
patient has had an adequate trial and failure with conservative treatment (i.e.
analgesics, oral contraceptives).
•
If the medication request is for the treatment of fibroids, the patient is an
adult female (≥18 y/o) and ONE of the following apply to the patient:
1. The patient is anemic (Hgb < 10.2 g/dl or Hct of < 30%) attributed to
fibroids and the patient has had a one to three month trial of iron therapy
alone which is (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) to try
and correct the anemia or there is a medical reason (intolerance,
hypersensitivity, contraindication, etc.) for not using iron alone to manage
the anemia.
2. T he patient requires the medication to decrease uterine volume as a result
of uterine fibroids to manage sympto ms (i.e. pelvic pressure, pelvic
fullness, urinary frequency, nocturia, constipation and/or anemia) and for
shrinkage of size to allow surgical intervention.
•
If the medication request is for the treatment of endometrial thinning,
documentation was submitted indicating the patient is scheduled for
endometrial ablation for dysfunctional uterine bleeding.
•
Prescribed dosing of GnRH agonist is within FDA approved indications
and/or is supported by the medical Compendium as defined by the Social
Security Act and/or per the NCCN, ASCO, ACOG or AAP standard of care
guidelines.
•
T he medication is recomme nded and prescribed by a specialist in the field to
treat the patient’s respective medical condition.
REAUT HORIZAT ION :
•
•
T he prescribing physician has provided documentation as to the clinical
benefits of the medication supporting continued treatment, OR the
medication is being continued in accordance with the recommended time as
defined by FDA drug package insert, and/or per recommendations of the
medical compendium as described above, and/or per the NCCN, ASCO,
ACOG or AAP standard of care guidelines.
If the medication reauthorization is for endometriosis ALL of the following
65
apply to the patient:
1. If the request is for a continuation of treatment exceeding 6 months, the
patient is receiving or will be prescribed “add back” hormonal therapy
(norethindrone acetate 5 mg daily or conjugated estrogen therapy)
{consistent with pharmacy claims data, OR for new members to the health
plan consistent with medical chart history}, OR if the patient has a
documented medical reason for not being able to take “add back” therapy,
the patient is receiving or is intended to receive anti-osteoporosis therapy
(e.g. alendronate or risedronate) {consistent with pharmacy claims data, OR
for new me mbers to the health plan consistent with medical chart history}.
2. If the patient received > 6 to 11 months cumulative doses of the GnRH
agonist a Dexa scan was performed and the results were submitted with the
medication request, indicating that the patient does not have documented
Osteoporosis AN D the patient is receiving calcium supplementation (1200
mg /day) and vita min D (400-800 units/day), which is (consistent with
pharmacy claims data, OR for new me mbers to the health plan consistent
with medical chart history).
3. The patient has not received cumulative doses of the GnRH agonist up to or
greater than 12 months of therapy.
Review Date 2/2016
•
If the medication reauthorization is for fibroids, the patient has not received
cumulative doses of the GnRH agonist up to or greater than 6 months of
therapy, and documentation that the drug is being used prior to surgery.
•
If the medication reauthorization is for central precocious puberty, the
child is male and < 12 years or female and < 11 years of age OR the child is
male and is > 12 years of age or a female that is > 11 years of age, and has
an acceptable documented medical reason to continue treatment, and
documentation of current height and bone age (every 6-12 months).
•
T he medication is recomme nded and prescribed by a specialist in the field to
treat the member’s respective medical condition
•
Prescribed dosing of medication is within FDA approved indications and/or
supported by the medical compendium as de fined by the Social Security Act
and/or per the NCCN, ASCO, ACOG or AAP standard of care guidelines.
NOTE: Clinical review er must override criteria w hen, in his/her professional judg ment,
the requested item is medica lly necessary.
66
Field Name
Prior Authorization Group
Drug(s)
Covered Uses
Field Description
Growth Hor mo ne
So matropin ( Genotro pin, Ge notropin M iniQuick, Hu mat rope, , Norditropin
FlexPen, , Nutro pin AQ, Nutropin AQ NuSpin, O mnitrop e, Saizen, , Tev-Tropin),
and new ly marketed growth hor mo ne agents.
Medically accepted indicatio ns are defined using the follo wing sources: the Food
and Drug Ad ministration (FD A), Micro medex, American Ho spital For mular y Service
(AHFS), United States P har ma copeia Drug I nfor mation for the Healthcare P ro fessional
(USP DI), the Drug P ackage Insert (P PI), or disease state specific standard of care
guidelines.
Exclusion Criteria
Required Medical Infor mation
Age Restrictions
Prescriber Restrictions
Treatment o f idiopathic short stature (ISS)-not a covered benefit and will not be approved
See other criteria
None
MD is an endo crinologist
Coverage Duration
If all o f the conditions are met, the initial request will be approved with a 6- mo nt h
duration, and requests for reauthorization will be approved for a 12 month duration. I f all
of the above criteria are not met, the request is re ferred to a Clinical Re vie wer/ Medical
Director for medical necessity revie w.
Other Criteria
1. For patients with gro wth hor mone deficiency states (adult and pediatric) either the
appro priate infor mation, diagnosis &/or labor ator y infor mation has been pro vided with
the request. T his includes Gr o wth Hor mone (GH) level i n response to the preferred
sti mul ator y test (i.e. Insulin Tolerance T est or Glucagon or Ar ginine) &/or Insulin
Gro wth Factor 1 level indicative of GH deficiency. I n additi on, for pediatric patients,
docu mentation o f his or her gro wth velocity (b elo w 4.5 c m/year), their height
percentile for age and gender, ho w far belo w the standard deviation (SD) their height is
for their age (at least 2 SD belo w nor mal), ho w far belo w the SD their height is fro m
their mid -parent height perce ntile (at least 2 SD belo w), and bone age (at least 2 SD
belo w) the mean for age.
AN D
2. If the patient is 17 years o f age or older and was diagnosed with childhood o nset
gro wth hor mone deficiency, d ocu mentation was provided that indicates GH
therap y is still medically neces sar y despite a 1 -3 mo nth trial o ff the medicatio n
(GH ther ap y discontinued for 1 -3 mo nths and resulting GH/I GF-1levels are lo w).
AN D
3. If the patient is 17 years o f age or older and still requires GH ther ap y and is
receiving childhood dosing ver sus lo wer adult dosing, appropriate docu mentatio n
wa s provided (i.e. patient has not reached maxi mu m predicted height or is still
having clinical response) docu menting the medical necessity of childhood GH
dosing.
AN D
4. If the request is not for Humatrope brand gro wth hor mo ne, the provider sub mitted a
docu mented medical reason (i. e. intolerance) why it is medi cally necessar y to
utilize so me other brand for mulation o f gro wth hor mo ne.
If all o f the conditions are met, the initial request will be approved with a 6- mo nth duration,
and requests for reauthorizatio n will be approved for a 12 month d uratio n. I f all o f the above
criteria are not met, the reques t is referred to a Clinical Reviewer/Medical Director for
medical necessit y revie w.
Revision Date 2/2016
If all o f the above criteria are not met, the request is referred to a Clinical
eviewer/M edical Director for medical necessity revie w.
67
PRIOR AUTHORIZATION PROTOCOL FOR HEPATITIS C TREATMENT for Pennsylvania
ZEPATIER™ (50mg elbasvir/ 100mg Grazoprevir): tablet (PREFERRED AGENT)
EPCLUSA® (400mg sofosbuvir/100mg velpatasvir): tablet
HARVONI™ (90mg ledipasvir/400mg sofosbuvir): tablet
SOVALDI ™ (sofosbuvir ): 400mg tablets
OLYSIO™ (simeprivir)
PEG-INTRON™ (peginterferon alfa‐2b)
RIBAVIRIN tablets or capsules
PEGASYS ™ (peginterferon alfa‐2a)
VIEKIRA PAK™ (Ombitasvir 12.5mg , paritaprevir 75mg, ritonavir 50mg tablets and dasabuvir 250mg)
TECHNIVIE™ (Ombitasvir 12.5mg , paritaprevir 75mg, ritonavir 50mg tablets)
DAKLINZA™ (Daclatasvir)
ANY OTHER NEWLY MARKETED AGENT for treatment of Hepatitis C
NOTE: WHERE APPLICABLE AND APPROPRIATE FOR GENOTYPE, if the request is for a treatment
regimen that includes any other direct acting antiviral (DAA) other than ZEPATIER the patient has a
documented medical reason (intolerance, hypersensitivity, contraindication, etc.) for not using
ZEPATIER. (Please see TREATMENT SUMMARY BELOW)
The presence of ANY of the following excludes approval:
1. Severe or uncontrolled co-morbidities
2. Severe renal impairment or End Stage Renal Disease (ESRD), (with the exception of Viekira Pak without Ribavirin and
Zepatier)
3. Contraindication to any component of the treatment regimen
All Initial requests MUST meet the following requirements:
1.
Patient Age 18 or older, AND
2.
Patient does not have a limited life expectancy of less than 12 months due to non-liver related comorbid
conditions, (complete medical history, co-morbidities and complications of liver disease have been provided),
AND
3.
Patient has one of the following:
History of liver transplant
OR
Is HIV co-infected or HBV co-infected, OR
Serious extrahepatic manifestations of Hepatitis C such as leukocytoclastic vasculitis,
membranoproliferative glomerulonephritis, or symptomatic cryoglobulinemia, OR
A Metavir fibrosis score of F2-F4 documented by a liver biopsy, OR
A Metavir fibrosis score of F2-F4 documented by Fibroscan, OR
A Metavir fibrosis score of F2-F4 documented by a blood test, OR
Physical findings consistent with substantial or advanced fibrosis or cirrhosis
Hospitalization within the past 12 months for a condition attributed to hepatic cirrhosis, OR
History of hepatic encephalopathy requiring medication management and/or hospitalization
Within the past 12 months,
OR
68
4.
History of portal hypertension as demonstrated by variceal bleeding or
radiographic evidence or Transjugular Intrahepatic Portsystemic Shunt (TIPS)
procedure, AND
Lab testing required before starting treatment (copy of results required):
Genotype
For Zepatier Genotype 1a requests: testing for the presence of virus with NS5A resistance-associated variant
polymorphisms (RAV’s) to determine appropriate therapy
within three (3) months of starting treatment (copy of results required):
ALT/AST
Detectable HCV RNA viral load
CBC (for treatment regimens with interferon or ribavirin, and for ribavirin requests hemoglobin is at least
10g/dL)
GFR
HIV
TSH (for interferon regimens)
INR
5.
Lab testing within one (1) month of starting treatment (copy of results required):
Pregnancy test in women of childbearing age (for treatment regimens with ribavirin), with patient agreeing to
use two or more forms of contraception, and will have monthly pregnancy tests during therapy, AND
6.
If the patient is actively abusing alcohol or IV drugs, or has a history of abuse documentation has been provided of
prescriber counseling regarding the risks of alcohol or IV drug abuse, and offer of referral for substance abuse
disorder treatment, AND
7.
If the patient has a history of failed treatment due to non-adherence, documentation has been provided that the
causes of non-adherence have been corrected or addressed, AND
8.
The dose that has been prescribed for the patient is consistent with the dosing recommendations listed
below, and is prescribed by a specialist in hepatology / gastroenterology / infectious disease/ or transplant,
AND
9.
Presence of previous treatment, treatment regimen and response, AND
10. If the patient is cirrhotic, there is documentation of compensated or decompensated disease, AND
11. Provider has addressed all potential drug interactions with Hepatitis C regimen (including discontinuation of the
interacting drug, dose reduction, or counseling of the patient of the risks associated with the use of both medications),
AND
12. The beneficiary will be referred to participate in Hepatitis C educational and counseling program provided
by the health plan. AND
13. Physician has provided a standing lab order with the request to authorize and obtain SVR12 as required.
Treatment for patients with Hepatitis C Genotypes 1, 2, 3, or 4 infections with Hepatocellular
Carcinoma: All initial requests must meet the following additional requirement
Documentation of testing confirming the diagnosis of Hepatocellular Carcinoma through either Imaging Testing
(such as Ultrasound, Computed Tomography, Magnetic Resonance Imaging), Laparoscopy, or Biopsy.
Treatment of recurrent HCV infection post liver transplant: (Does not require patient to have advanced to severe fibrosis)
Documentation of liver transplant including date of transplant, treatment history and current HCV Viral Load
69
APPROVAL CONSIDERATIONS MUST BE REVIEWED BY MEDICAL DIRECTOR FOR MEDICAL NECESSITY
Dose and Duration of Therapy: (SEE TREATMENT SUMMARY THAT FOLLOWS)
Approvals of requests will be consistent with package labeling or current guidelines, at FDA approved dosing.
These regimens are subject to change as newly marketed agents become available.
ALL regimens are for 28 day supply per fill (See REFILL CONSIDERATIONS BELOW).
Hepatitis C Treatment Summary
Treatment Naïve-No Cirrhosis
Genotype
Genotype 1a WITHOUT baseline
NS5A RAVs or Genotype 1b, GT4
Genotype 1a WITH baseline
NS5A RAVs
Genotype 2, 3, 5 or 6
Treatment Option
Zepatier
Duration
12 weeks
Harvoni (VL < 6,000,000)
OR
Epclusa (VL > 6,000,000)
8 weeks
Epclusa
12 weeks
12 weeks
Treatment Naïve-With Cirrhosis
Genotype
Genotype 1a WITHOUT baseline
NS5A RAVs or Genotype 1b, GT4
Genotype 1a WITH baseline
NS5A RAVs
Genotype 2, 3, 5, or 6
Treatment Option
Zepatier
12 weeks
Duration
Epclusa
12 weeks
Epclusa
12 weeks
Previously treated patients NO CIRRHOSIS
Genotype
Genotype 1a
WITHOUT baseline
NS5A RAVs or
Genotype 1b
Genotype 1a WITH
baseline NS5A RAVs
Failed Regimen
Peg/Riba
Treatment Option
Zepatier
Duration
12 weeks
Peg/Riba
Epclusa
12 weeks
Genotype 1
Sovaldi/Ribavirin +/- Peg
Harvoni with weight
based ribavirin
12 weeks
Genotype 1
Incivek, Victrelis, or
Olysio + Peg/Riba (NS3
Protease inhibitors)
Epclusa
12 weeks
70
Genotype 1
Genotype 1
Genotype 2
Sovaldi/Olysio
NS5A inhibitors
Peg/Riba
Defer treatment
Defer treatment
Epclusa
Defer treatment
Defer treatment
12 weeks
Genotype 2
Sovaldi/Riba
Epclusa with weight
based ribavirin
12 weeks
Genotype 3
Peg/Riba
Epclusa
12 weeks
Genotype 3
Sovaldi/Riba
Epclusa with weight
based ribavirin
12 weeks
Genotype 4
Peg/Riba
Epclusa
12 weeks
Genotype 5 and 6
Peg/Riba
Epclusa
12 weeks
Previously treated patients WITH CIRRHOSIS
Genotype
Genotype 1a
WITHOUT baseline
NS5A RAVs or
Genotype 1b
Genotype 1a WITH
baseline NS5A RAVs
Genotype 1
Failed Regimen
Peg/Riba
Treatment Option
Zepatier
Duration
12 weeks
Peg/Riba
Epclusa
12 weeks
Sovaldi/Ribavirin +/- Peg
Harvoni with weight
based ribavirin
24 weeks
Genotype 1
Incivek, Victrelis, or
Olysio + Peg/Riba (NS3
Protease inhibitors)
Zepatier and weight
based ribavirin
Genotype 1
Sovaldi/Olysio
If immediate treatment
is required-testing for
NS5A and NS3A RAVs
must be completed. If
nucleoside-based dual
DAA therapy is
requested (e.g.
sofosbuvir), give with
weight based ribavirin,
and refer to current
guidelines
12-16 weeks*
*16 weeks for GT1a
WITH baseline NS5A
RAVs
24 weeks
Genotype 1
NS5A inhibitors
Defer treatment If
immediate treatment is
required-testing for
NS5A and NS3A RAVs
must be completed. If
71
If immediate treatment
is required, refer to
current guidelines
nucleoside-based dual
DAA therapy is
requested (e.g.
sofosbuvir), give with
weight based ribavirin,
and refer to current
guidelines
Genotype 2
Peg/Riba
Epclusa
12 weeks
Genotype 2
Sovaldi/Riba
Epclusa with weight
based ribavirin
12 weeks
Genotype 3
Peg/Riba
Epclusa with weight
based ribavirin
12 weeks
Genotype 3
Sovaldi/Riba
Epclusa with weight
based ribavirin
12 weeks
Genotype 4
Peg/Riba
Epclusa
12 weeks
Genotype 5 and 6
Peg/Riba
Epclusa
12 weeks
Decompensated Cirrhosis including Hepatocellular Carcinoma
Genotype
Genotype 1 or 4
Genotype 1 or 4
Ribavirin ineligible
Genotype 1 or 4
Genotype 2 or 3
Failed Regimen
Sovaldi or NS5A based
regimen
Treatment Option
Epclusa with weight
based ribavirin
Duration
12 weeks
Epclusa
24 weeks
Epclusa with weight
based ribavirin
24 weeks
Epclusa with weight
based ribavirin
12 weeks
Patients with Renal Impairment, Including Severe Renal Impairment (CrCl , 30mL/min) or ESRD
requiring Hemodialysis
Genotype
Creatinine Clearance
Treatment Option
Duration
All Genotypes
CrCl 30mL/minNo dosage adjustment is No dosage adjustment
80mL/min
required for this level of
is required for this level
renal impairment, see
of renal impairment,
charts above
see charts above
Genotype 1a, 1b or 4 CrCl < 30ML/min for
Zepatier
12 weeks
treatment BEFORE
kidney transplant
72
Genotype 2, 3, 5 or 6
CrCl < 30ML/min for
treatment BEFORE
kidney transplant
Peg + dose adjusted
ribavirin (200mg daily)
Post-Transplant, Including Compensated Cirrhosis
Genotype
Genotype 1 or 4
Naïve or Experienced
All levels of fibrosis
including
compensated
cirrhosis
Genotype 1 or 4
Treatment Naïve and
with compensated
disease and are
ribavirin ineligible
Genotype 2 and 3
Treatment Option
Harvoni with weight
based ribavirin
Duration
12 weeks
Harvoni
24 weeks
Sovaldi and Daklinza with
low initial dose ribavirin
(600mg and increased as
tolerated)
12 weeks
Genotype 2 and 3
ribavirin ineligible
Sovaldi and Daklinza with
low initial dose ribavirin
(600mg and increased as
tolerated)
24 weeks
Post-Transplant, Decompensated Cirrhosis
Genotype
Genotype 1 or 4
Naïve or Experienced
All levels of fibrosis
and decompensated
cirrhosis
Genotype 1 or 4
Treatment Naïve and
with compensated
Treatment Option
Harvoni with low initial
ribavirin (600mg and
increased as tolerated)
Duration
12 weeks
Harvoni
24 weeks
73
disease and are
ribavirin ineligible
Genotype 2
Sovaldi and ribavirin
(initial dose 600mg/day,
increased monthly by
200mg/day as tolerated
to weight based dose)
24 weeks
Continuation of therapy to be completed by Health Plan or Case Management
REFILL CONSIDERATIONS:
1. The health plan will reach out to all members approved for treatment, with the intent to educate
and ensure successful completion of the regimen.
2. The health plan will guide and reinforce compliance through ongoing interaction with the
member.
3. Repeat viral load at treatment week 4, week 8, week 12 and 12 weeks following completion of
therapy to establish SVR. If quantitative HCV viral load is detectable at week 4 of treatment,
repeat quantitative HCV RNA viral load testing is recommended after 2 additional weeks of
treatment (treatment week 6). If quantitative HCV viral load has increased by greater than 10-fold
(>1 log10 IU/mL) on repeat testing at week 6 (or thereafter), then discontinuation of HCV
treatment is recommended.
4. For Zepatier requests, repeat ALT/AST should be completed at week 8 if on 12 weeks of therapy,
and also at week 12 (if patient is on 16 weeks of therapy)
Revision/Review Date: 1/2017
74
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Hepsera®
Covered Uses
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PP I), or disease state specific standard of care guidelines.
N/A
See “other criteria”
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Revision/Review
02/2016
Hepsera® (adefovir)
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration; If the conditions are not met, the request will be sent to
a Medical Director/clinical reviewer for medical necessit y review.
Initial authorization:
• Diagnosis of hepatitis B.
AND
• Submitted current laborator y values indicating evidence of active
viral replication.
AND
• Submitted current laborator y values indicating persistent elevations
in ALT or AST or histologicall y active disease.
AND
• Documented
treatment failure with or contraindication to
Baraclude® (entecavir) therap y.
AND
• Patient under the care of a gastroenterologist or an infectious disease
specialist.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
75
PERFORMRX PRIOR AUTHORIZATION PROTOCOL FOR TREATMENT OF HEREDITARY ANGIOEDEMA
Cinryze
Berinert
Kalbitor
Firazyr
Ruconest
Or any newly marketed agent
FORMULARY STATUS: Non-Formulary, Require PA
All requests MUST meet the following requirements:
• Confirmed diagnosis of hereditary angioedema (HAE) with measurement of C1-INH antigenic level,
C1-INH functional level, and C4 level
• MD must be an immunologist, allergist or hematologist
• The patient is not taking ACE inhibitors or estrogen replacement
• Documentation submitted indicates the medication is being prescribed for an FDA approved
indication at FDA approved dose.
For acute treatment:
• If all of the above conditions are met, the request will be approved for the standard FDA approved
dosing per treatment episode, with 5 refills.
For prophylaxis treatment:
•
The patient has a history of at least two severe attacks/month with swelling of the face, throat, or
GI tract, and chart notes have been submitted indicating the date and severity of attack.
• The patient has tried and failed and/or has a documented medical reason (intolerance or
contraindication) for not using danazol, stanozolol, or oxandrolone.
If all of the above conditions are met, the request will be approved for three month duration. If all of the
above criteria are not met, the request is referred to a Medical Director/Clinical reviewer for medical
necessity review.
Renewal Criteria:
• Documentation was submitted that the patient has clinically benefited from medication in an
acute attack, or documentation was submitted that the patient has clinically benefited with
reduced attacks, if using as prophylaxis.
• Documentation submitted indicates the medication is being prescribed for an FDA approved
indication at FDA approved dose.
• Approval duration for acute treatment is the FDA approved dosing per treatment episode, with 5 refills.
• Approval duration for prophylaxis treatment is 3 months.
If all of the above criteria are not met, the request is referred to a Medical Director/Clinical Reviewer for
medical necessity review.
References
1. Craig T, Pürsün E, Bork K, Bowen T, Boysen H et al. WAO Guideline for the Management of
Hereditary Angioedema. World Allergy Organization Journal 2012; 5(12): 182-199. WAO Guideline for
the Management of Hereditary Angioedema, WAO Journal, December2012
http://www.waojournal.org/content/pdf/1939-4551-5-12-182.pdf
76
2. http://www.haea.org/wp/wp-content/uploads/2013/09/guidelines.pdf
3. http://www.haea.org/professionals/diagnosing-hae/
4. Cicardi, Marco. Hereditary angioedema: Treatment of acute attacks. In: UpToDate, Waltham, MA.
(Accessed on October 7, 2016.)
5. Cicardi, Marco. Hereditary angioedema: General care and long-term prophylaxis. In: UpToDate, Waltham,
MA. (Accessed on October 7, 2016.)
Revision/Review Date: 11/2016
77
Field
Description
Field Na me
P rior Authorization Group Desc
Drug(s)
Covered Uses
Exclusio n Criteria
Required Medical Infor matio n
Age Restrictions
P rescriber Restrictions
Coverage Duration
HYALURONIC ACID DERIVATIVES
EUFL EXXA is PREFERRE D agent
Gel-One
Hyalgan
M onovisc
Orthovisc
Supartz
Synvisc
Synvisc One
Any other newly mar keted Hyaluronic Acid derivative
*Medically accepted indications are defined using the follo wing sources: the Food
and Drug Ad ministration (FDA), Micro medex, American Hospital For mular y
Ser vice ( AHFS), United States P har macopeia Drug Infor mation for the Healthcare
Professional (USP DI), or the Drug P ackage Insert (P P I).
None
See other criteria
None
None
If all o f the criteria is met, the request will be appro ved for one co mplete course o f tr eat ment
(based on the FDA labeled dose of the drug requested). If all of the criteria is not met, the
request is referr ed to a Medical Director for medical necessity revie w.
78
Other Criteria
Initial Authorization:
• A diagnosis o f Osteoarthritis (OA)/Degen erati ve j oint disease (DJ D) of the knee.
• There is docu mentatio n (in clai m history or provider state ment) that the patient recently (o ver
the past 4 months) has had adequate trials o n si mp le analgesics (aceta minophen containing
products or topical capsaicin crea m) & NS AIDS (including t wo different prescription strength
NSAIDS) on a continuous basis for 3 months without success or has a medical reason
(intolerance, hypersensitivity, contraindicatio n, etc.) for not being able to utilize si mple
analgesic products and NS AIDS.
• Docu ment atio n has been pro vided that a steroid inj ection has been tried and failed, per
affected knee or patient has a medical reaso n for not being able to utilize steroid inj ections.
• If the request is for any other product other than E uflexxa, the patient has a documented
medical reason (intolerance, h ypersensiti vity, contraindication, etc) for not using Euflexxa to
treat their medical conditio n.
Reauthorization:
• At least 6 months have elapsed since the previous course o f HAD ther ap y for the treated
knee(s).
• Docu ment atio n was sub mitted that the patient had a response to the treated knee (s) that lasted
for > 6 months to previo us HAD therap y, as docu mented b y at least ONE of the follo wing:
Decreased joint pain or stiffness, improved knee range o f mo tion, decrease in midpatellar knee
circu mference in millimeters, or syno vial effusion absent or volu me decreased.
• Docu ment atio n was sub mitted that the patient has a return of symp to ms o f osteoarthritis, and
has been retreated with NS AIDS and simple analgesics
(aceta minophen containing pro ducts or topical capsaicin crea m) without success,
or has a medic al reason (intolerance, h ypersensiti vit y, co ntrai ndication, etc) for not being able to
utilize si mple analgesic products and NSAIDS.
• If the request is for any other product other than E uflexxa, the patient has a documented
medical reason (intolerance, h ypersensiti vity, contraindication, etc) for not using Euflexxa to
treat their medical conditio n.
If all of the criteria is not met, the request is referred to a Medical Director for medical
necessity re vie w.
Revision/Revie w Date: 2/201 6
79
PERFORMRx PRIOR AUTHORIZ ATION CRITERI A for Ibrance
PR EF E R R ED ST AT U S: REQUIRES Prior Authorization
Ibrance® (Palbociclib): 75mg, 100mg, 125mg capsules
INIT I AL C R IT E RI A FOR IB R ANCE:
Patient is 18 years of age or older, AND
Documentation has been submitted that patient has a diagnosis of estrogen receptor
(ER) positive, human epidermal growth factor receptor 2 (HER2) negative advanced or
(metastatic) breast cancer, AND
Patient is one of the following:
• postmenopausal as demonstrated by one of the following: prior bilateral oophorectomy,
age is ≥60 years old, age is < 60 and amenorrheic for 12 months or more in the absence of
chemotherapy, tamoxifen or toremifene, or ovarian suppression (FSH and estradiol in postmenopausal range) and will be using in combination with letrozole
• postmenopausal (as described above) who have progressed on endocrine therapy and will be
using in combination with fulvestrant (Faslodex)
• premenopausal women who have progressed after receiving a luteinizing hormonereleasing hormone (LNRH) agonist, and will be using in combination with fulvestrant
(Faslodex)
AND
Documentation submitted includes complete blood count with differential (within 30 days
of request).
Prescriber is oncologist.
If all of the above conditions are met, the request will be approved for up to a 2-month
duration; if all of the above criteria are not met, the request is referred to a clinical reviewer for
medical necessity review.
C O NT I NU AT IO N OF T H ER APY F OR IB R AN CE:
Repeat complete blood counts with differential were submitted with request (within 30 days
of request).
Documentation submitted indicates that there is no evidence of disease progression on
therapy member has obtained clinical benefit from the medication.
Prescriber is oncologist.
If all of the above conditions are met, the request will be approved for up to a 3-month
duration; if all of the above criteria are not met, the request is referred to a clinical reviewer for
medical necessity review.
NOTE: Medical Director/clinical re view er must override criteria w hen, in his/her professional judgment,
the requested itemis medicall ynecessar y.
Revision/Revie w Date: 4/2016
80
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Idiopathic
Pulmonary Fibrosis (IPF)
PREFERRED STATUS: REQUIRE Prior Authorization
Ofev® (Nintedanib Esylate): 100mg,150mg capsules
Esbriet® (Pirfenidone): 267mg capsule
INITIAL CRITERIA FOR IDIOPATHIC PULMONARY FIBROSIS:
Patient is 18 years of age or older
Documentation submitted includes patient’s complete medical history/co-morbidities
Confirmed diagnosis of Idiopathic Pulmonary Fibrosis as demonstrated by a High Resolution CT
scan with “honeycombing” or “ground glass opacities” or lung biopsy, and other known causes
of interstitial lung disease have been excluded
MD is a pulmonologist or lung transplant specialist
Pulmonary function test indicate patient has Forced Vital Capacity (%FVC) greater than or equal
to 50% within 30 days of request
Baseline ALT, AST, and bilirubin has been submitted within 30 days of request
• Patient does NOT have severe hepatic impairment (Child Pugh C)
If the request is for Ofev, the patient is not currently taking a P-glycoprotein or CYP3A4 inducer
(e.g. rifampin, carbamazepine, phenytoin, St. John’s Wort)
If the request is for Ofev and the patient has history of coronary artery disease, documentation
submitted indicates that the prescriber has consulted with cardiology
If the request is for Esbriet, the patient is not currently taking a strong CYP1A2 inducer (e.g.
carbamazepine, rifampin) or a strong CYP1A inhibitor (e.g. fluvoxamine)
Documentation has been provided that the patient does not smoke
If all of the above conditions are met, the request will be approved for a 3 month duration; if all of the
above criteria are not met, the request is referred to a Medical/clinical reviewer for medical necessity
review.
REAUTHORIZATION CRITERIA FOR IDIOPATHIC PULMONARY FIBROSIS:
MD is a pulmonologist or lung transplant specialist
Repeat ALT, AST and bilirubin within 30 days of request
If the ALT/AST are more than 3-5 times the upper limit of normal, the requested dose is being
reduced based on the manufacturer labeling.
If ALT/AST is more than 5 times the upper limits of normal or increased ALT/AST with
hyperbilirubinemia the medication should be discontinued
Documentation submitted indicates that the member has obtained clinical benefit from the
medication
Documentation
has been provided that the patient does not smoke
If all of the above conditions are met, the request will be approved for a 6 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
NOTE: Medical Director/Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
Revision/Review Date: 7/2016
81
PerformRx Prior Authorization Criteria for Immunoglobulins (IVIG)
ALL REQUESTS MUST HAVE A CONFIRMED DIAGNOSIS BY A SPECIALIST
FOR ALL INDICATIONS: Patient has documented trial and failure of all other standard of care
therapies as defined per recognized guidelines, or have a documented medical reason why patient is
not able to utilize other standard of care therapy.
IVIG will be considered for the following indications provided the required information is present:
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Primary immunodeficiency
Thrombocytopenia purpura, Idiopathic and chronic immune
Kawasaki disease
Chronic B- cell lymphocytic leukemia
Bone marrow transplantation
Pediatric HIV
Multifocal motor neuropathy
Chronic inflammatory demyelinating neuropathy
Guillain-Barre syndrome
Other medically accepted indications
If criteria is met, the request will be approved for the duration listed below, if criteria is not met, the
request is referred to a Medical Director/Clinical reviewer for medical necessity review.
•
Primary immunodeficiency
Congenital agammaglobulinemia
Hypogammaglobulinemia (Common Variable
Immunodeficiency,
CVID)
Severe combined immunodeficiency (SCID)
Wiskott-Aldrich syndrome
X-linked agammaglobulinemia or Bruton’s
Hypergammaglobulinemia
X-linked Hyper IgM syndrome
•
•
Documentation submitted includes patient’s
IgG
level and is below normal level for
indication
Clinically significant deficiency of humoral
immunity as evidenced by ONE of the
following:
Documented inability to produce an
adequate immunologic response
to specific antigens.
Patient has history of recurrent
infections despite prophylactic
antibiotics
Dose does not exceed 400-800mg/kg every 28
days
If criteria is met, approve for 6 months.
82
Thrombocytopenia purpura, Idiopathic and
chronic immune
Acute : (active bleeding, patients requiring an
urgent invasive procedure, to defer splenectomy, or
platelet counts
< 20,000/ul at risk for intra-cerebral hemorrhage or has
life
threatening bleeding)
• Dose does not exceed 1g/kg daily for up to 2
days, or 400mg/kg daily for 5 days
Chronic:
•
•
83
Duration of illness of greater than 6
months
Patient has documented trial and failure of
corticosteroids and splenectomy, or has a
documented medical reason why they are not
able to use corticosteroids or patient is at high
risk for post-splenectomy sepsis.
Kawasaki disease
•
•
IVIG is being given with high dose aspirin
Requested dose does not exceed a single 2g/kg dose
or a dose of 400mg/kg for five consecutive days
If criteria is met, approve for up to 5 days.
Chronic B-cell lymphocytic leukemia
•
•
•
Patient’s IgG level has been provided, and is
< 500mg/dL
The patient has history of severe bacterial infections
Dose does not exceed 400mg/kg every 3-4 weeks
If criteria is met, approve for 3 months.
Bone marrow transplantation
•
•
•
Confirmed bone marrow transplant within last 100
days.
Patient’s IgG level has been provided, and is
< 400mg/dL
Dose does not exceed 500mg/kg/wk for the first 100
days post- transplant
If criteria is met, approve for 3 months.
Pediatric HIV
OR
•
•
•
Diagnosis of HIV
Patient is < 13 years of age
Patient’s IgG level has been provided, and is
< 400mg/dL
•
Clinically significant deficiency of humoral immunity
as evidenced by ONE of the following:
Documented inability to produce an
adequate immunologic response to
specific antigens.
Patient has history of recurrent bacterial
infections despite prophylactic antibiotics
Dose does not exceed 400mg/kg every 28 days
•
If criteria is met, approve for 3 months.
Multifocal motor neuropathy (MMN)
•
•
•
Duration of symptoms has been at least 1 month
with disability.
Documentation submitted includes nerve
conduction studies were completed to rule out
other possible conditions, and confirms the
diagnosis of MMN.
Dose does not exceed 2g/kg/month. This dose can
be given over two to five days.
If criteria is met, approve for up to 5 days for 3 months.
Chronic inflammatory demyelinating neuropathy
(CIDP)
•
•
•
84
Duration of symptoms has been at least 2 months
with disability.
Documentation submitted includes nerve
conduction studies were completed or nerve biopsy
to rule out other possible conditions, and confirms
the diagnosis of CIDP.
Patient has documented trial and failure of
•
corticosteroids, or has a documented medical
reason why they are not able to use corticosteroids
to treat the condition. In addition, if
documentation is provided that patient has severe
and fulminant CIDP, IVIG can be approved as initial
therapy
Dose does not exceed 2g/kg/month. This dose can
be given over two to five days.
If criteria is met, approve for up to 5 days for 3 months.
Guillain-Barre syndrome
•
•
•
Documentation submitted indicates severe disease
with the inability to walk without aid
Onset of symptoms within the last 4 weeks
Dose does not exceed 2g/kg/month
If criteria is met, approve for 3 months.
Any other medically accepted indication
•
•
Review/Revision Date 11/2016
For any other indication, medical recommendation
must have a I, IIa or IIb recommendation, and be
used for a medical condition that is supported by
the medical compendium (Micromedex, American
Hospital Formulary Service, Drug Points, and Drug
Package Insert) as defined in the Social Security Act
1927, and/or per recognized standard of care
guidelines.
Patient has documented trial and failure of all other
standard of care therapies as defined per recognized
guidelines, or has a documented medical reason
why patient is not able to utilize other standard of
care therapy.
If criteria is met, approve for 3 months
85
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Injectable/Infusible Osteoporosis Agents
Boniva® Injection (Ibandronate), Forteo® (teriparatide), Prolia™
(denosumab), Reclast® (zoledronic acid) or any other newly marketed
agent
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
“See other criteria”
N/A
N/A
If all of the conditions are met, requests will be approved for a 1 year.
***FORTEO REQUESTS WILL ONLY BE APPROVED FOR A
TOTAL DURATION OF 24 MONTHS***If the conditions are not
met, the request will be sent to a Medical Director/clinical reviewer
for medical necessity review.
• If diagnosis is osteoporosis, documentation was submitted
indicating patient is postmenopausal woman or a male patient
with a bone mineral density (BMD) value consistent with
osteoporosis (T-scores equal to or less than –2.5) or has had an
osteoporotic fracture, OR patient is over age of 50 with a Tscore between -1 and -2.5 at the femoral neck or spine and a 10
year hip fracture probability >3% or a 10 year major
osteoporosis-related fracture probability >20%, based on the
US-adapted WHO absolute fracture risk model
• The patient has a documented (consistent with pharmacy
claims) adequate trial of an oral bisphosphonate or has a
medical reason (e.g. intolerance, hypersensitivity,
86
•
•
•
•
Revision/Review Date
8/2016
contraindication, etc.) for not using an oral bisphosphonate
If request is for Forteo (teriparatide) the patient has not
exceeded a total of 24 months of therapy AND one of the
following applies to patient:
patient has documented trial and failure of Boniva
(Ibandronate) injection, Reclast (zoledronic acid) or
Prolia (denosumab) or has a medical reason (e.g.
intolerance, contraindication, etc.) why these therapies
are not suitable to be used
has SEVERE osteoporosis (T-Score -3.5 or below, or
T-Score of -2.5 or below plus a fragility fracture)
If diagnosis is Paget’s disease, documentation (within 60 days
of request) was submitted including patient’s serum alkaline
phosphatase level of ≥ two times the upper limit of normal, the
patient is symptomatic OR there is documentation of active
disease
The patient is taking calcium and vitamin D
The medication is FDA approved for indication and is being
requested at an FDA approved dose
Physician/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
87
Field Description
Field Name
Prior Authorization
Group
Drugs
Injectable Bisphosphonates & Skeletal Related Events
Preferred: Pamidronate disodium (Aredia®), Zoledronic Acid
(Zometa ®), Nonpreferred: Denosumab (Xgeva®)
Covered Uses
The request is for an FDA approved indication or for a medically
accepted indications as defined or as supported by the medical compendium (Micromedex,
American Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI) , Drug Package Insert) as defined in the
Social Security Act 1927, or per the National Comprehensive Cancer Network (NCCN), the
American Society
of Clinical Oncology (ASCO), or the National Institutes of Health
(NIH) Consensus Panel standard of care guidelines.
Exclusion Criteria
N/A
Required
See “Other Criteria”
Age
Restrictions
Medical
Information
Prescriber
Restrictions
Coverage Duration
N/A
Other Criteria
Prescriber is an oncologist
6 months
•
•
•
•
The request is for an approved/accepted indication at an
approved dose
Documentation has been provided that patient has a creatinine clearance >
30mL/min
If the request is for a brand name agent, the patient has a documented trial and
failure of generic Pamidronate (Aredia) OR zoledronic acid (Zometa) that is
consistent with claims history, or has a documented medical reason (intolerance,
hypersensitivity, contraindication, etc) for not utilizing one of these agents to manage
their medical condition
If the request is for denosumab (Xgeva) for treating Giant cell tumor of bone,
documentation has been submitted that the tumor is unresectable or that surgical
resection is likely to result in morbidity
If these conditions are not met, the request will be sent to a
Medical Director/clinical reviewer for medical necessity review.
Revision/ Review
Date: 2/2017
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
88
PERF ORM RX N AT IO N AL P A C RIT ERI A
AMNESTEEM® (isotretinoin) Capsules: 10mg, 20mg, 40mg
FORMULARY ST ATUS: Form ulary (generic)
ABSORIC A™ (isotretinoin) Capsules: 10 mg, 20 mg, 25 mg 30 mg, 35 mg 40 mg
CLAR AVIS® (isotretinoin) Capsules: 10mg, 20mg, 30 mg, 40mg
™
MYORISAN (isotretinoin) Capsules: 10 mg, 20 mg, 40 mg
ZENAT ANE® (isotretinoin) Capsule: 10 mg, 20mg, 30 mg, 40 mg
PA CRITERI A FOR APPROV AL :
• Diagnosis of severe recalcitrant nodular acne.
AND
• Documented treatment with a therapeutic trial and failure or intolerance to oral antibiotic therapy first line therapy
(e.g. doxycycline, minocycline, tetracycline, erythromycin) for at least 4 weeks (28 days) of therapy in the
previous 60 days.
If the above conditions are met, the request will be approved for up to a 6 month duration with generic medication; if
the above conditions are not met, the request will be referred to a Medical Director for medical necessity review.
FDA INDIC ATION:
Isotretinoin is indicated for the treatment of severe recalcitrant nodular acne. Because of significant adverse effects
associated with its use, isotretinoin should be reserved for patients with severe nodular acne who are unresponsive to
conventional therapy, including systemic antibiotics. In addition, isotretinoin is indicated only for those females who
are not pregnant because isotretinoin can cause severe birth defects.
DOSAGE AND ADMINISTRATION:
Dosage is adjusted and individualized according to side effects and disease response. Recommended course of
therapy: Initial dose is 0.5 to 1 mg/kg/day (range is 0.5 to 2 mg/kg/day) divided into 2 doses with food, for 15 to 20
weeks. Failure to take isotretinoin with food will significantly decrease absorption. The safety of once daily dosing has
not been established. Once-daily dosing is not recommended. Patients whose disease is very severe or is primarily
manifested on the body may require up to the maximum dose. If the total nodule count decreases by > 70% prior to
15 weeks, the drug may be discontinued. After a period of > 2 months off therapy, and if warranted by persistent or
recurring severe nodular acne, a second course of therapy may be initiated.
BLACK BOX W ARNING AND ADDITION AL W ARNINGS :
Isotretinoin must not be used by females who are or may become pregnant. There is an extremely high risk that
severe birth defects will result if pregnancy occurs while taking isotretinoin in any amount, even for short periods of
time. Potentially any fetus exp osed during pregnancy can be affected. There are no accurate means of determining
whether an e xposed fetus has been affected.
Birth defects which have been documented following isotretinoin exposure include abnormalities of the face, eyes,
ears, skull, central nervous system, cardiovascular system, and thymus and parathyroid glands. Cases of IQ scores
less than 85 with or without other abnormalities have been reported. There is an increased risk of spontaneous
abortion, and premature births have been reported.
Documented external abnormalities include: skull abnormality, ear abnormalities (including anotia, micropinna, small
or absent external auditory canals); eye abnormalities (including microphthalmia); facial dysmorphia; cleft palate.
Documented internal abnormalities include: CNS abnormalities (including cerebral abnormalities, cerebellar
malformation, hydrocephalus, microcephaly, cranial nerve deficit); cardiovascular abnormalities; thymus gland
abnormality; parathyroid horm one deficiency. In some cases death has occurred with certain of the abnormalities
previously noted.
If pregnancy does occur during treatment of a female patient who is taking isotretinoin, isotretinoin must be
discontinued immediately and she should be referred to an obstetrician-gynecologist experi enced in reproductive
toxicity for further evaluation and counseling.
Because of isotretinoin’s teratogenicity and to minimize fetal exposure, isotretinoin is approved for marketing only
under a special restricted distribution program approved by the Food and Drug Administration. This program is called
TM
iPLEDGE . Isotretinoin must only be prescribed by prescribers who are registered and activated with the iPLEDGE
program. Isotretinoin must only be dispensed by a pharmacy registered and activated with iPLEDGE, and must only
be dispensed to patients who are registered and meet all the requirements of iPLEDGE. Meeting the requirements for
a female patient of childbearing potential signifies that she:
89
• Has been counseled and has signed a patient information/informed consent about birth defects form that
contains warnings about the risk of potential birth defects if the fetus is exposed to isotretinoin. The patient
must sign the informed consent form before starting treatment and patient counseling must also be done at
that time and on a monthly basis thereafter.
• Has had two negative urine or serum pregnancy tests with a sensitivity of at least 25mIU/mL
before receiving the initial isotretinoin prescription. The first test (a screening test) is obtained by
the prescriber when the decision is made to pursue qualification of the patient for isotretinoin. The
second pregnancy test (a confirmation test) must be done in a CLIA-certified laboratory. The
interval between the two tests should be at least 19 days.
o For patients with regular menstrual cycles, the second pregnancy test should be done
during the first 5 days of the menstrual period immediately preceding the beginning of
isotretinoin therapy and after the patient has used 2 forms of contraception for one month.
o For patients with amenorrhea, irregular cycles, or using a contraceptive method that
precludes withdrawal bleeding, the second pregnancy test must be done immediately
preceding the beginning of isotretinoin therapy and after the patient has used 2 forms of
contraception for one month.
• Has had a negative result from a urine or serum pregnancy test in a CLIA-certified laboratory
before receiving each subsequent course of isotretinoin. A pregnancy test must be repeated every
month, in a CLIA-certified laboratory, prior to the female patient receiving each prescription.
• Has selected and has committed to use 2 forms of effective contraception simultaneously, at least
one of which must be a primary form, unless the patient commits to continuous abstinence from
heterosexual contact, or the patient has undergone a hysterectomy or bilateral oophorectomy, or
has been medically confirmed to be post-menopausal. Patients must use two effective forms of
effective contraception for at least one month prior to initiation of isotretinoin therapy, during
isotretinoin therapy, and for one month after discontinuing isotretinoin therapy. Counseling about
contraception and behaviors associated with an increased risk of pregnancy must be repeated on a
monthly basis.
Primary contraception includes: tubal sterilization; partner’s vasectomy; intrauterine device;
hormonal (combination oral contraceptives, transdermal patch, injectables, implantables, or vaginal
ring). Secondary forms include male latex condoms (with or without spermicide), diaphragms,
cervical caps, and vaginal sponges all of which must be used with spermicide. Any birth control
method can fail. There have been reports of pregnancy from female patients who have used oral
contraceptives, as well as transdermal patch/injectable/implantable/vaginal ring hormonal birth
control products; these pregnancies occurred while these patients were taking isotretinoin. These
reports are more frequent for female patients who use only a single method of contraception. There
for it is critically important that female patients of childbearing potential use 2 effective forms of
contraception simultaneously. Patients must receive written warnin gs about the rates of possible
contraception failure.
If a pregnancy does occur during isotretinoin treatment, isotretinoin must be discontinued
immediately. The patient should be referred to an obstetrician-gynecologist experienced in
reproductive toxicity for further evaluation and counseling. Any suspected fetal exposure during or
one month after isotretinoin therapy must be reported immediately to the FDA via the MedW atch
number 1-800-FDA-1088 and also to the iPLEDGE pregnancy registry at 1-866-495-0654 or via the
internet (www.ipledgeprogram.com)
• Patients should be prospectively cautioned not to self-medicate with the herbal supplement St.
John’s W ort because a possible interaction has been suggested with hormonal contraceptives
based on reports of breakthrough bleeding on oral contraceptives shortly after starting St. John’s
W ort. Pregnancies have been reported by users of combined hormonal contraceptives who also
used some form of St. John’s W ort
To receive isotretinoin all patients must meet all of the following conditions:
• Must be registered with the iPLEDGE program by the prescriber
• Must understand that severe birth defects can occur with the use of isotretinoin by female patients
• Must be reliable in understanding and carrying out instructions
• Must sign a patient information/informed consent (for all patients) form that contains warnings
about the potential risks associated with isotretinoin
• Must fill the prescription within 7 days of the of the date of specimen collection for the pregnancy
test for female patients of childbearing potential
• Must fill and pick up the prescription within 30 days of the office visit for male patients and female
patients not of childbearing potential
• Must not donate blood while on isotretinoin and for one month after treatment has ended
90
• Must not share isotretinoin with anyone, even someone who has similar symptoms
In addition to the requirements for all patients described above, female patients of childbearing potential
must meet the following conditions:
• Must not be pregnant or breast-feeding
• Must comply with the required pregnancy testing at a CLIA-certified laboratory
• Must fill and pick up the prescription within 7 days of the date of specimen collection for the
pregnancy test
• Must be capable of complying with the mandatory contraceptive measures required for isotretinoin
therapy, or commit to continuous abstinence from heterosexual intercourse, and understand
behaviors associated with an increased risk of pregnancy
• Must understand that it is her responsibility to avoid pregnancy one month before, during, and one
month after isotretinoin therapy
• Must have signed an additio nal patient information/informed consent about birth defects (for
female patients who can get pregnant) form before starting isotretinoin that contains warnings
about the risk of potential birth defects if the fetus is exposed to isotretinoin
• Must access the iPLEDGE program via the internet or telephone before starting isotretinoin, on a
monthly basis during therapy, and one month after the last dose to answer questions on the
program requirements and to enter the patient’s two chosen forms of contraception
• Must have been informed of the purpose and importance of providing information to the iPLEDGE
program should she become pregnant while taking isotretinoin or within one month of the last dose
To dispense isotretinoin, pharmacies must be registered and activated with the pregnancy risk management
program iPLEDGE. To dispense isotretinoin, the pharmacist must:
• Be trained by the Responsible Site Pharmacist concerning the iPLEDGE program requirements.
• Obtain authorization from iPLEDGE via the internet or telephone for every isotretinoin
prescription. Authorization signifies that the patient has met all program requirements and is
qualified to receive isotretinoin
• W rite the Risk Management Authorization (RMA) number on the prescription.
• Isotretinoin must only be dispensed:
o In no more than a 30-day supply
o W ith an isotretinoin Medication Guide
o After authorization from the iPLEDGE program
o Prior to the “do not dispense to patient after” date provided by the iPLEDGE system
(within 30 days of the office visit for male patients and female patients not of childbearing
potential and within 7 days of the date of specimen collection for female patients of
childbearing potential)
o W ith a new prescription for refills and another authorization from the iPLEDGE program
(No automatic refills are allowed)
Psychiatric disorders: Isotretinoin may cause depression, psychosis, and, rarely, suicidal ideation, suicide
attempts, suicide, and aggressive and/or violent behaviors. No mechanism of action had been established
for these events. Health care providers should read the brochure, Recogni zi ng Psychiatric Disorders in
Adolescents and Young Adults: A Guide for Prescribers of Isotretinoin. Health care providers should be alert
to the warning signs of psychiatric disorders to guide patients to receive the help they need. Therefore, prior
to initiation of isotretinoin therapy, physicians should ask patients and family members about any history of
psychiatric disorder, and at each visit during therapy, assess patients for symptoms of depression, mood
disturbance, psychosis, or aggression to determine if further evaluation may be necessary.
REFERENCES:
1. Is Accutane really dangerous? Med Lett Drugs Ther 2002 Sep 16;44(1139):82
2. Strauss JS, Krowchuk DP, Leyden JJ, et al. Guidelines of Care for Acne Vulgaris Management.
American Academy of Dermatology Association. J Am Acad Dermatol. 2007. Apr;56(4):651-53.
3. W ysowski DK, Swann J, Vega A. Use of isotretinoin (Accutane) in the United States: rapid increase
from 1992 through 2000. J Am Acad Dermatol 2002 Apr;46(4):505-9.
4. Leyden JJ. A review of the use of combination therapies for the treatment of acne vulgaris. J Am
Acad Dermatol 2003;45 (3S):S200-S210.
5. Enders SJ, Enders JM. Isotretinoin and psychiatric illness in adolescents and young adults. Ann
Pharmacother 2003;37 (8): 1124-1127.
6. Young D. FDA, Roche to implement new dispensing procedures for isotretinoin. Am J Health Syst
Pharm 2001 Dec 15;58(24):2359-60.
91
7.
8.
9.
10.
11.
12.
13.
14.
Jacobs DG, Deutsch NL,Brewer M. Suicide, depression, and isotretinoin: is there a causal link? J
Am Acad Dermatol 2001 Nov;45(5):S168-75.
Product information, Amnesteem. Mylan Pharmaceuticals Inc, Revised May 2012.
Product information, Claravis. Barr Laboratories Inc, Revised Ma y 2012
Prescribing Information, Absorica. Ranba xy Laboratories , Inc. May 2012
Prescribing Information, Myorisan. VersaPharm, Inc. May 2012
Prescribing Information, Sotret. Ranbaxy Laboratories, Inc. February 2010
Facts and Comparisons, St. Louis, 2011 eFacts CliniSphere Version ISBN 1-57439-0368.
Lexi-Comp OnlineTM, Le xi-Drugs Online, Hudson, Ohio: Lexi-Comp, Inc.; Accessed September 10,
2015. Available from:
http://online.lexi.com.libpro xy.t emple.edu/lco/action/doc/retrieve/docid/patch_f/7127
Revision/Revie w Date: 11/201 5
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the
requested item is medicall y necessar y.
92
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Juxtapid®/Kynamro®
PREFERRED STATUS: Non-Preferred- REQUIRE Prior Authorization
Juxtapid ® (lomitapide)
Kynamro® (Mipomersen Sodium)
INITIAL CRITERIA FOR JUXTAPID®/KYNAMRO®:
Patient is 18 year of age or older.
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted includes patient’s complete medical history /co-morbidities.
Patient must have a confirmed diagnosis of familial hypercholesterolemia (FH) with chart notes
or clinical labs including 3 of the following:
• Autosomal Dominant Hypercholesterolemia Genetic Testing Reflex Panel (ADHP Panel)
• an initial fasting lipid panel prior to treatment ≥ 190mg/dL (lab results must be provided) ,
and two additional fasting lipid panel laboratory reports within the past 9 months with
abnormal LDLcholesterol levels after treatment with other lipid lowering agents *** If patient
has been on high dose atorvastatin 80mg or Rosuvastatin 40mg for a minimum of 3 months,
then only one additional fasting lipid panel in the last 6 months with abnormal LDL is
required.***
• documented strong (first and second degree relatives) family history of high levels of
LDL and/or heart attack and relationship to member
• documented chart notes of clinical manifestations of FH such as xanthomas or inflamed
tendons
Documented claim history or chart notes showing consistent therapy (3 months) with
atorvastatin 80mg OR Crestor (Rosuvastatin) 40mg* (*OR documentation has been provided
that patient is of Asian descent in which Crestor 20mg is the max dose) with inadequate
response OR a documented medical reason (e.g. intolerance, hypersensitivity) for not utilizing
one of these therapies to manage their medical condition.
If request indicates that the patient is “statin intolerant”, documentation was provided including
description of the side effects, duration of therapy, “wash out”, re-trial, and then change of
agents.
Documentation has been submitted that provider has counseled patient to follow a “heart
healthy” diet.
Documentation submitted indicates the patient is a non-smoker or provider has counseled patient
regarding smoking cessation.
If the request is for Juxtapid®, the patient has had an inadequate response or a documented
medical reason (e.g. intolerance, hypersensitivity) for not utilizing Repatha®AND THEN
Kynamro® to manage their medical condition.
If the request is for Kynamro®, the patient has had an inadequate response or a documented
medical reason (e.g. intolerance, hypersensitivity) for not utilizing Repatha®to manage their
condition.
If all of the above conditions are met, the request will be approved for a
3 month duration; if all of the above criteria are not met, the request is referred to a clinical
reviewer for medical necessity review.
REAUTHORIZATION CRITERIA:
93
Prescriber must be cardiologist or a specialist
in the treatment of lipid disorders.
Documentation submitted indicates that the member has obtained clinical benefit from the
medication including repeat fasting lipid panel lab report.
The patient’s claim history shows consistent therapy (i.e. monthly fills)
If all of the above conditions are met, the request will be approved for a 6 month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional judgment, the
requested items medically necessary.
Revision/Review Date: 9/2016
94
Field Name
Prior Authorization Group
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
®
KUVAN
Kuvan® (Sapropterin Dihydrochloride)
*Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information for
the Healthcare Professional (USP DI) , and the Drug Package Insert).
None
See “Other Criteria”
None
Specialist experienced in treating PKU
Initial: If the criterion is met, the request will be approved for a duration of 1
month; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
1st Reauthorization: If the criteria is met, the request will be approved for a
duration of 1 month for patients who require a dose increase to 20 mg/kg/day
due to non-responsiveness and for all other patients the request will be
approved for a duration of 3 months; if the above conditions are not met, the
request will be referred to a clinical reviewer/Medical Director for medical
necessity review.
2nd Reauthorization and Thereafter: If the criterion is met, the request will
be approved for a duration of 4 months; if the above conditions are not met,
the request will be referred to a clinical reveiwer/Medical Director for medical
necessity review.
INITIAL AUTHORIZATION:
• Documentation of a confirmed diagnosis of Phenylketonuria (PKU) by a
specialist experienced in treating PKU
• Documentation of the patient’s baseline blood Phe level. (within 30 days of
the request)
• Documentation consistent with order forms OR receipts (within 30 days of
request) that the patient is currently utilizing a Phe restricted diet with Phe-free
medical products/foods in conjunction with dietician or nutritionist. (Examples
include Phenyl-Free® (phenylalanine free diet powder), Loplex, Periflex,
Phlex-10, PKU 2, PKU 3, XPhe Maxamaid, XPhe Maxamum,)
• Documentation of the patient’s current weight.
• The medication is being prescribed at a dose no greater than the FDA
approved maximum initial dose of 10 mg/kg/day-20mg/kg/day.
PA CRITERIA FOR 1st REAUTHORIZATION:
Patients that were dosed at 20mg/kg/day (initial auth) and did not have a
decrease in Phe level of at least 30% from baseline, are considered NON
RESPONDERS and NO ADDITIONAL TREATMENT will be authorized.
• Documentation of the patient’s current weight.
• Documentation consistent with current order forms OR receipts that the
95
159
patient is currently utilizing a Phe restricted diet with Phe-free medical
products/foods in conjunction with dietician or nutritionist. (Examples include
Phenyl-Free® (phenylalanine free diet powder), Loplex, Periflex, Phlex-10,
PKU 2, PKU 3, XPhe Maxamaid, XPhe Maxamum,)
• Documentation of at least two separate blood Phe level results (within 30
days of request).
• The medication is being prescribed at an FDA approved dosage.
PA CRITERIAFOR 2nd REAUTHORIZATIONAND THEREAFTER:
• Documentation of the patient’s current weight.
• Documentation consistent with order forms OR receipts (within 30 days of
request) that the patient is currently utilizing a Phe restricted diet with Phe-free
medical products/foods in conjunction with dietician or nutritionist. (Examples
include Phenyl-Free® (phenylalanine free diet powder), Loplex, Periflex,
Phlex-10, PKU 2, PKU 3, XPhe Maxamaid, XPhe Maxamum, Low-Phe
natural foods, Low-protein specialty foods, Phe-free formula, or Phe-free
protein replacement bars, tablets, capsules, etc.)
• Documentation of at least two separate blood Phe level results (within 60
days of request).
• The medication is being prescribed at an FDA approved dosage
If the above conditions are met, the request will be approved for a duration of
4 months; if the above conditions are not met, the request will be referred to a
clinical reviewer/Medical Director for medical necessity review.
Last review 2/2017
NOTE: Clinical reviewer/Medical Director must override criteria when,
in his/her professional judgment, the requested item is medically
necessary.
96
160
Field Name
Field Description
Prior Authorization Group
Drug(s)
Covered Uses
LEMTRADA®
Lemtrada®
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex (DrugPoint or DRUGDEX), American
Hospital Formulary Service (AHFS – accessed via Lexicomp), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP DI), and the
Drug Package Insert.
Patients that are infected with HIV (Human Immunodeficiency Virus)
See “Other Criteria”
Patients must be 17 years age or older
Prescriber must be a neurologist
If all of the criteria are met, the initial request will be approved for 5 vials (60mg).
For continuation of therapy, if all criteria are met, the request will be approved for 3 vials
(36mg). If all of the above criteria are not met, the request is referred to a
Clinical Reviewer for medical necessity review.
***Note Lemtrada® is only available through a restricted distribution program that
both patient and physician must be enrolled.
INITIAL AUTHORIZATION:
The patient is ≥ 17 years old with a clinical diagnosis of a relapsing form of
multiple sclerosis.
Documentation of the following lab values have been submitted within 30 days of
request:
-HIV testing
-Thyroid function tests
-Complete blood count with differential
-Serum creatinine
-Urinalysis with cell counts
-ECG (within 3 months)
-baseline skin exam (for melanoma)
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescri ber Restrictions
Coverage Duration
Other Criteria
Clinical or diagnostic information was submitted that indicates that that patient has a
documented (consistent with pharmacy claims data OR for new members to the health
plan consistent with medical chart history) treatment failure after receiving an adequate
trial (including dates, doses of 6 months or more of each therapy) of glatiramer acetate
40mg (Copaxone®), AND teriflunomide (Aubagio®), AND THEN Tysabri®, or has a
documented medical reason (intolerance, hypersensitivity, etc) for not utilizing these
therapies for a minimum of 6 months each to manage their medical condition.
Documentation has been provided that the patient will be taking formulary anti- herpetic
prophylaxis for a minimum of 60 days beginning day one of treatment.
Lemtrada® is being prescribed at an FDA approved dosage
PA CRITERIA FOR REAUTHORIZATION:
The patient is ≥ 17 years old with a clinical diagnosis of a relapsing form of
multiple sclerosis.
A period of 12 months has elapsed since previous treatment.
Documentation of the following labs values have been submitted with request:
97
- HIV testing (within 30 days of request)
-Thyroid function tests (every 3 months from initial dose)
-Complete blood count with differential (every month from initial dose)
-Serum creatinine (every month from initial dose)
-Urinalysis with cell counts (every month from initial dose)
-ECG (within 3 months)
-annual skin exam (for melanoma)
Documentation has been provided that the patient will be taking formulary anti- herpetic
prophylaxis for a minimum of 60 days beginning day one of treatment.
Lemtrada® is being prescribed at an FDA approved dosage
Review Date 11/2016
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
98
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Lidoderm®
Lidoderm® (lidocaine)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization
•
Diagnosis of postherpetic neuralgia
AND
•
Revision/Review
Date 10/2016
Documented trial and failure or intolerance to the following
medications: amitriptyline or nortriptyline and gabapentin
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
99
Field Name
Field Description
Prior Authorization Group
Long Acting Injectable Antipsychotics
Drug(s)
risperidone (Risperdal Consta®), paliperidone palmitate (Invega Sustenna™, Invega
Trinza™), olanzapine pamoate monohydrate (Zyprexa Relprevv®), aripiprazole
monohydrate (Abilify Maintena®), aripiprazole lauroxil (Aristada™), or any newly
marketed long acting injectable antipsychotic
*Risperdal Consta®, Invega Sustenna™ and Invega Trinza™ are preferred agents
for this class
Covered Uses
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), and the Drug Package Insert).
Exclusion Criteria
N/A
Required Medical Information
Initial approval:
If documentation was provided (claim history or chart notes with dosage
and treatment dates) indicating the member has been stable on a long
acting antipsychotic other than the preferred agents, the request can be
approved as continuation of therapy.
Physician attestation indicating member has a long term history (>3
months) of noncompliance with oral antipsychotic medications AND/OR
member has a documented medical reason for not using oral formulary
atypical antipsychotic medications
Physician attestation indicating member has failed adherence measures to
improve compliance with oral formulary atypical antipsychotic medications
(i.e. problem-solving strategies, reminders, self- monitoring tools, cues,
reinforcements, supportive services, psychosocial interventions)
Physician attestation indicates member has had clinical decompensation or
is at high risk of clinical decompensation and functional impairment (e.g.
hospitalizations, safety risk, repeated relapses related to diagnosis)
Member has demonstrated tolerability to the oral agent of the drug that is
being requested without side effects
If the request is for any other product other than the preferred agents, the
member has a documented trial (consistent with pharmacy claims or chart
notes including 3 months or more of therapy) with one of the preferred
agents, OR has a documented medical reason such as intolerance,
hypersensitivity, contraindication, etc. OR documentation was provided
indicating member was previously established on a non-preferred agent
and prescriber feels changing patient to one of the preferred long acting
agents would cause detriment or patient decompensation.
If request is for Invega Trinza™, documentation has been provided that the
100
member has been stable on Invega Sustenna™ for 4 months, and at the
same dose for the last 2 months
Request is for FDA approved or a medically accepted indication at an
approved dose
Reauthorization:
Member has been compliant with filling their medication OR
documentation was provided indicating why member missed dosing
Documentation was provided that member is stable on medication
Request is for FDA approved or a medically accepted indication at an
approved dose
Age Restrictions
Member must be 18 years of age or older.
Prescriber Restrictions
Prescriber is a psychiatrist or in consultation with a psychiatrist.
Coverage Duration
If all of the conditions are met, the initial request will be approved for 6 month
duration; reauthorization requests will be approved for 12 months. If the above
conditions are not met, the request will be referred to a Medical Director/clinical
reviewer for medical necessity review.
Other Criteria
N/A
Review Date: 2/2017
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
101
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Field Description
Low Molecular Weight Heparins PA Criteria
Arixtra® (fondaparinux), Fragmin® (dalteparin), Lovenox®
(enoxaparin) and any newly marketed low molecular weight
heparin
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved:
• For the use in deep vein thrombosis (DVT) and/or pulmonary
embolism (PE) - for up to a 31-day duration (unless greater duration
of therapy is requested and medically necessary then will be
approved for up to a 6 month duration).
• For use in pregnant members – can be approved up to patient’s
expected due date .
• For use in members with cancer - for up to a 6 month duration.
If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Other Criteria
PA CRITERIA FOR APPROVAL FOR USE IN DEEP VEIN
THROMBOSIS (DVT) AND/OR PULMONARY EMBOLIS
(PE):
• The medication is being prescribed for the prevention and/or
treatment of a DVT and/or PE.
• Documentation of the patient’s current weight.
• The medication is being prescribed at a dose that is within FDA
approved guidelines.
• If the request is for a duration of therapy greater than 31 days
then a letter of medical necessity that provides a valid medical
reason why the member cannot be treated with warfarin, heparin
or a formulary direct thrombin inhibitor for long-term therapy
(>31 days) must be submitted.
PA CRITERIA FOR APPROVAL FOR USE IN A PREGNANT
MEMBER:
102
• The medication is being prescribed for the prevention or treatment
of a DVT and/or PE while the member is pregnant.
• Documentation of the patient’s current weight and expected due
date (EDD). If the request is to continue LMWH treatment
postpartum then documentation of the patient’s actual or expected
due date and current weight is required AND THEN up to 6 weeks
of additional treatment may be authorized.
• The medication is being recommended and prescribed by an
obstetrician or a hematologist at a dose that is within FDA
approved guidelines and/or is supported by the medical
compendium as defined by the Social Security Act.
PA CRITERIA FOR APPROVAL FOR USE IN MEMBER WITH
CANCER:
•
The medication is being prescribed for the prevention or
treatment of a venous thromboembolism (VTE) (a proximal DVT
and/or PE) for a member with cancer.
•
Documentation of the patient’s current weight.
• The medication is being recommended and prescribed by an
oncologist/hematologist at a dose that is within FDA approved
guidelines and/or is supported by the medical compendium as
defined by the Social Security Act and/or per the National
Comprehensive Cancer Network (NCCN) or American Society
of Clinical Oncology (ASCO) standard of care guidelines.
REAUTHORIZATION CRITERIA FOR APPROVAL FOR
USE IN MEMBER WITH CANCER BEYOND SIX
MONTHS:
Revision/Review
Date 2/2017
•
The medication is being for the prevention and/or treatment of a
VTE for a member with cancer.
•
Documentation of the patient’s current weight.
•
If the request for a duration of therapy greater than 6 months
then a letter of medical necessity that provides a valid medical
reason why the member needs to continue treatment and cannot
be treated with Coumadin for long-term therapy.
•
The medication is being recommended and prescribed by an
oncologist/hematologist at a dose that is within FDA approved
guidelines or is supported by the medical compendium as defined
by the Social Security Act and/or per the National Comprehensive
Cancer Network (NCCN) or American Society of Clinical
Oncology (ASCO) standard of care guidelines.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
103
Field Na me
Prior Authorization Group
Description
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Review Date 2/2016
Hydroxyprogesterone caproate
Field
Description
Makena®
Medicall y accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formular y Service (AHFS), United States
Pharmacopeia Drug Infor mation for the Healthcare Professional
(USP DI), or the Dru g Package Insert (PP I).
Patients pregnant with multiples, histor y of thrombosis or thromboembolic
disorders, histor y of breast cancer or other hormone sensitive cancer,
cholestatic jaundice of pregnanc y, liver tumors or active liver disease, or
uncontrolled h ypertension
See other criteria
Patient must be 16 years of age or older
Prescriber must be an obstetrician
If all of the criteria is met, the request will be approved for up to 21 weeks
• Documentation has been provided that patient has a history of preterm
birth before 37 weeks gestation
• Documentation that patient is pregnant with singleton
• Documentation that drug is being used for FDA approved indication
(begin treatment between 16 weeks gestation and continued weekl y
until week 37 gestation) at an FDA approved dose.
If all of the criteria is not met, the request is referred to a Medical
Director or clinical reviewer for medical necessity review.
104
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Mepron®
Mepron® (atovaquone) suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
• Diagnosis of Pneumocystis jirovecii pneumonia (PCP) or
diagnosis with the need to prevent PCP infection.
AND
• Documented trial and failure with therapeutic doses or
intolerance to trimethoprim- sulfamethoxazole (TMP-SMX) (first
line therap y).
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
105
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
04/2016
Field Description
Multaq®
Multaq® (dronedarone)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), the Drug Package Insert (PP I), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
Request must be from a cardiologist or electroph ysiologist.
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessit y review.
Initial Authorization:
• Diagnosis of parox ysmal or persistent arterial
fibrillation (AF) or atrial flutter (AFL) with a recent
episode.
• Must not have NYHA Class IV heart failure or
s ymptomatic heart failure with recent decompensation
requiring hospitalization or referral to a specialized heart
failure clinic
• Must have at least one of the following associated risk
factor(s):
▪ age > 70
▪ h ypertension
▪ diabetes
prior cerebrovascular accident
▪ left atrial diameter ≥50 mm or left ventricular ejection
fraction (LVEF) < 40%
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
106
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
SELF INJECTABLE DISEASE MODIFYING
IMMUNOMODULATORS FOR MULTIPLE SCLEROSIS (MS)
Interferon beta-1a (Avonex®, Rebif®), Interferon beta-1b
(Betaseron®, Extavia™), Glatiramer Acetate (Copaxone®,
Glatopa™), Peginterferon beta-1a (Plegridy®), Daclizumab
(Zinbryta™)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug
Package Insert (PPI), or disease state specific standard of care
guidelines.
Patients with primary progressive MS
See “Other Criteria”
Patient must be 18 years of age or older
Prescriber must be a neurologist
If all of the criteria are met, the initial request will be approved for 6
months. For continuation of therapy, if all criteria are met, the request
will be approved for 12 months. If all of the above criteria are not met,
the request is referred to a Medical Director/Clinical Reviewer for
medical necessity review
INITIAL AUTHORIZATION:
The patient is ≥ 18 years old with a clinical diagnosis of a relapsing
form of multiple sclerosis
If the medication request is for Avonex®, Rebif®, Betaseron®,
Extavia,® Zinbryta or any other Newly Marketed Self-Injectable
Disease-Modifying Immunomodulating MS Agent, the member has
a documented treatment failure to Copaxone 40mg® and
Aubagiowhich is consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history,
indicating they had received an adequate trial (including dates,
doses of 6 months or more of each therapy) of Copaxone® 40 mg
and Aubagio and/or has another documented clinically significant
medical reason (intolerance, hypersensitivity, contraindication, etc.)
for not taking Copaxone® 40 mg and Aubagio for a minimum of 6
months each to treat their medical condition
The medication is being prescribed by a neurologist at an FDA
approved dose
PA CRITERIA FOR REAUTHORIZATION:
The patient is ≥ 18 years old with a clinical diagnosis of a relapsing
form of multiple sclerosis
Documentation indicating the member has clinically benefited from
therapy
The medication is being prescribed by a neurologist at an FDA
approved dose
107
Revision/Review
Date 11/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
108
PERFORMRX PRIOR AUTHORIZATION CRITERIA
AUBAGIO® (teriflunomide)
®
GILENYA (fingolimod hcl)
TECFIDERA® (dimethyl fumarate)
PA CRITERIA FOR INITIAL APPROVAL:
•
The member is an adult (≥ 18 y/o) member with relapsing/remitting MS (RRMS) or secondary progressive MS (SPMS) with
a relapsing element.
•
If the medication request is for Gilenya, Tecfidera or any other newly marketed oral MS Agent, the member has a
documented treatment failure to Aubagio and Copaxone 40mg which is consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history, indicating they had received an adequate trial (including
dates, doses of 6 months or more of therapy) or has another documented clinically significant medical reason (intolerance,
hypersensitivity, contraindication, etc.) for not taking Aubagio and Copaxone 40mg for a minimum of 6 months to treat their
medical condition. New members to the health plan stable on Gilenya or Tecfidera will be permitted to continue therapy if
requested by provider.
•
The medication is being recommended and/or prescribed by a neurologist at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 6-month duration; if all of the above criteria are not
met, the request is referred to a Medical Director/Clinical reviewer for medical necessity review.
REAUTHORIZATION CRITERIA:
•
Documentation sent indicates that the member is an adult (≥ 18 y/o) and has one of the following types of MS: RRMS or
SPMS with a relapsing element.
•
Documentation indicating the member has clinically benefited from therapy.
•
The medication was prescribed at an FDA approved dosage.
•
Medication was recommended by a neurologist and/or prescribed by a neurologist.
If all of the above conditions are met, the request will be approved for up to a 12-month duration; if all of the above criteria are
not met, the request is referred to a Medical Director/Clinical reviewer for medical necessity review.
Revision/Review Date: 11/2016
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment, the requested item is medically
necessary.
1
109
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Oral Diabetic Agents: DPP-IV Inhibitors PA Criteria
Janumet® (sitagliptin/metformin), Janumet® XR
(sitagliptin/metformin), Januvia® (sitagliptin)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PP I), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration; If the conditions are not met, the request will be sent to
a Medical Director/clinical reviewer for medical necessit y review.
Initial authorization:
Diagnosis of T ype 2 diabetes mellitus.
AND
Documented trial and failure with therapeutic doses, contraindication, or
intolerance to metformin.
OR
Documented insulin therapy.
Revision/Review
Date 02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
110
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Natpara®
Natpara® (parathyroid hormone)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
Patients at risk for osteosarcoma, patients with hypoparathyroidism caused by
calcium-sensing receptor mutations or in patients with acute postsurgical
hypoparathyroidism.
See “other criteria”
Patient is 18 years of age or older
MD is an endocrinologist
If all of the conditions are met, the request will be approved for a 3 month
duration. If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
• Documentation has been submitted that the patient has a diagnosis of
chronic hypoparathyroidism who cannot maintain stable serum and
urinary calcium levels with calcium and vitamin D
• Documentation has been submitted (with dates of therapy) that the
patient has had an adequate trial with calcium and vitamin D
• Documentation has been submitted that the patient will take Natpara® in
combination with calcium and vitamin D
• Patient is NOT currently taking alendronate
• Current labs (within 30 days of request) have been submitted for the
following:
Serum calcium (must be above 7.5mg/dL to start therapy)
Vitamin D level (must be adequate to start therapy)
If these conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Revision/Review Date
11/2016
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
111
Field Na me
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Infor mation
Age Restrictio ns
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Non-Formulary/Prior Autho rization Required Medications Criteria
Medically accepted indications are defined using the follo wi ng sources: the
Food and Drug Ad ministration (FDA), Micro medex, Ameri can Hospital
For mular y Service (AHFS), United States Phar macopeia Drug Infor mation
for the Healthcare Professiona l (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criterion is met, the request will be approved for up to a 12 month
duration (depending on the dia gnosis and usual treat ment duration). If
criterion is not met, the request will be referred to a Clinician for medical
necessity revie w.
Initial Authorization:
•
•
Appropriate diagnosis/indicati on for requested non-preferred/prior
authorization required medication.
Appropriate dose of medicatio n based on age (i.e. pediatric and
elderly populations) and indication.
And patient meets one of the three follo wing criteria:
•
•
•
Revision/Review Date
07/2016
Docu mented trial and failure or intolerance with up to three
for mular y medications used to treat the docu mented diagnosis. For
medications where there is only one preferred agent, only that agent
must have been ineffective or not tolerated.
No other for mular y medicatio n has a medically accepted use for the
patient’s specific diagnosis as referenced in the medical co mpendia.
All other for mular y medications are contraindicated based on the
patient’s diagnosis, other medical conditions, or other medication
therap y.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
112
KF AHC AHNE Health Plan
NOVOSEVEN® RT (Factor VIIA): 1 mg, 2 mg, 5mg, 8 mg vials
P ROTOCOL FOR USE OF NOVOSEVEN FOR OFF LABELED INDICATIONS
• Documentation of the patient diagnosis and/or what was the indication of use for NovoSeven
• Documentation of the patient’s weight at the time that NovoSeven was administered.
• If available, a copy of the facility’s policy and procedures regarding the use of NovoSeven. If the
facility does have its own policy and procedures regarding the use of NovoSeven then documentation
must be submitted showing that all the necessary steps (i.e. laboratory values, indications,
consultations, prior medically or pharmacological interventions) where taken before utilization of
NovoSeven treatment.
• For facilities that do not have a preexisting policy and procedures document concerning the use of
NovoSeven then the following documentation must be submitted:
o That NovoSeven was not used as a first line treatment option OR if used then a rationale for
the unsuitability of other first line treatment options must be documented.
o If applicable, documentation that the patient is a Jehovah’s Witness or of another belief
system that does not accept any blood products for medical treatment.
o That all accepted and available surgical measures/embolization/blood products to control
bleeding were attempted. Also the following documentation must be submitted:
What surgical measures, if any, were employed for the patient
What amount of blood products were used (i.e. how many units of blood, fresh frozen
plasma).
And what was the timing of the surgical measures/embolization/blood products
utilized in respect to the use of NovoSeven (e.g. patient received 8 units of FFP one
hour before treatment of NovoSeven)
o If the available surgical measures/embolization/blood products were impossible/inappropriate
to be utilized or contraindicated then documentation of a valid medical reason of why is
required.
o If available, documentation of the patient’s laboratory results (e.g. APTT, INR)
o For any retreatment dose, documentation that a minimum of 30 - 60 minutes had elapsed
before retreatment with NovoSeven and then documentation must be submitted that severe
blood loss was still occurring and available surgical measures/embolization/blood products
either did not work and/or where medically impossible/inappropriate.
o For any retreatment dosing then, if available, documentation of the patient’s laboratory
results (e.g. APTT, INR)
• Off-label indications for which the use of NovoSeven will not be approved :
o Prophylactic administration of NovoSeven for elective surgery patients (unless the patient has
documented Factor VIII or Factor IX deficiency with an inhibitor, acquired hemophilia, FVII
deficiency, Glanzmann’s thrombasthenia, or other rare blood disorder).
o NovoSeven being administered to a patient in which the medical team felt was unsalvageable
or for whom treatment would generally be considered futile.
o A dose of greater than 90 mcg/kg of body weight (unless being used for indications due to
trauma).
F DA APP ROVED INDICATIONS
NovoSeven is indicated for:
• T reatment of bleeding episodes in hemophilia A or B patients with inhibitors to Factor VIII or Factor
IX and in patients with acquired hemophilia
• Prevention of bleeding in surgical interventions or invasive procedures in hemophilia A or B patients
with inhibitors to Factor VIII or Factor IX and in patients with acquired hemophilia
• T reatment of bleeding episodes in patients with congenital FVII deficiency
113
•
•
•
Prevention of bleeding in surgical interventions or invasive procedures in patients with congenital
FVII deficiency
T reatment of bleeding episodes in patients with Glanzmann’s thrombasthenia with refractoriness to
platelet transfusions, with or without antibodies to platelets.
Prevention of bleeding in surgical interventions or invasive procedures in patients with Glanzmann’s
thrombasthenia with refractoriness to platelet transfusions, with or without antibodies to platelets.
F DA APP ROVED DOSAGE AND ADMINISTRATION
NovoSeven RT is intended for intravenous bolus administration only. Coagulation parameters do not
necessarily correlate with or predict the effectiveness of NovoSeven.
Hemophilia A or B with Inhibitors:
o For bleeding episodes - the recommended dose of NovoSeven RT is 90 mcg/kg gi ven every
two hours by bolus infusion until hemostatis is achieved or until the treatment has been
judged to be inadequate. Adj ust dose and interval based on severity of bleeding and degree
of hemostasis achieved. Doses ranging from 35 to 120 mc g/kg have been used successfully.
T he minimum effective dose has not been established.
o For surgical interventions – an initial dose of 90 mcg/kg per body weight should be given
immediately before the intervention and repeated at 2 hour intervals for the duration of the
surgery. For minor surgery, post-surgical dosing by bolus injection should occur at 2 hour
intervals for the first 48 hours and then at 2 to 6 hour intervals until healing has occurred. For
maj or surgery, post-surgical dosing by bolus injection should occur at 2 hour intervals for 5
days, followed by 4 hour intervals until healing occurred. Additional bolus doses should be
administered if required.
Congenital Factor VII deficiency
o T he recommended dose range for treatment of bleeding episodes or for prevention of
bleeding in surgical interventions or invasive procedures in congenital Factor VII deficient
patients is 15 – 30 mcg/kg of body weight every 4 -6 hours until hemostasis is achieved.
Effective treatment has been achieved with doses as low as 10 mcg/kg. Dose and frequency
of injections should be adjusted to each individual. T he minimal effective dose has not been
determined.
Acquired Hemophilia
o T he recommended dose range for the treatment of patients with acquired hemophilia is 70 –
90 mcg/kg repeated every 2 – 3 hours until hemostasis is achieved. The minimum effective
dose in acquired hemophilia has not been determined. T he maj ority of the effective outcomes
were observed within the recommended dose range.
Glanzmann’s T hrombasthenia
o For surgical interventions the recommended initial dose is 90 mcg/kg given via bolus infusion
immediately prior to surgery and repeated every 2 hours for duration of procedure.
Postsurgically, 90 mcg/kg of NovoSeven RT should be given by intravenous bolus infusion
every 2 to 6 hours.
Reference:
1. Levi M, Peters M, Buller HR. Efficacy and safety of recombinant factor VIIa for treatment of severe
bleeding: A systemic review. Crit Care Med 2005; 33:885-92.
2. Dutton RP, McCuun M, Hyder M, etl al. Factor Vlla for Correction of Traumatic Coagulopathy. J
T rauma 2004; 57: 709-19.
3. Horton J D, Dezee KJ, Wagner M. Use of rFVIIa in the Trauma Setting – Practice Patterns in United
States Trauma Centers.
114
4. Karalapillai D and Popham P. Recombinant factor VIIa in massive postpartum haemorrhage.
International Journal of Obstetric Anesthesia 2007; 16: 39-34.
5. Chiara O, Cimbanassi S, Brioschi PR, et al. Treatment of Critical Bleeding in Trauma Patients.
Minerva Anestesiologica 2006; 72: 383-7.
6. NovoSeven® RT Prescribing Information. Novo Nordisk, Inc. Bagsvaerd, Denmark, J uly 2014.
7. Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, Crowther MA; American Society of
Hematology. T he American Society of Hematology 2011 evidence-based practice guideline for
immune thrombocytopenia. Blood. 2011;117(16):4190-4207.
8. Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and
manage ment of primary i mmune thrombocytopenia. Blood. 2010;115(2):168-186.
9. Baxter MS, Schroeder WS, Cheng Y, Bermstein ZP. Diminished response to recombinant factor VIIa
in a patient with idiopathic thrombocytopenic purpura. Ann Pharmacother. 2006;40(11):2053-2058.
10. Aguilar C, Lucía JF. Successful control of severe postoperative bleeding with recombinant factor
VIIa in a case of refractory idiopathic thrombocytopenic purpura. Am J Hematol. 2007;82(3):246247.
11. Hard y JF, Bélisle S, Van der Linden P. Efficac y and safet y of recombinant activated factor
VII to control bleeding in nonhemophiliac patients: a review of 17 randomized controlled
trials. Ann Thorac Surg. 2008; 86:1038-48.
Revision/Review Date: 9/2014
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Clinical reviewer must override criteria w hen, in his/her professional judgment, the
requested item is medically necessary.
115
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Nucala®
Field Description
Nucala® (mepolizumab) injection
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug
Package Insert (PP I), or disease state specific standard of care
guidelines.
When being used for relief of acute bronchospasm or status
asthmaticus, or for the treatment of other eosinophilic conditions.
See “other criteria”
Member must be 12 years of age or older
Prescriber must be an allergist or pulmonologist
If the above conditions are met, the initial request will be approved
with a 3 month duration. All subsequent requests will be approved
with a 6 month duration. If the criteria are not met, the request will be
referred to a clinical reviewer for medical necessity review.
Initial Authorization:
1. Confirmed diagnosis of eosinophilic asthma
2. Documentation has been provided (within 45 da ys of request)
with eosinophil count ≥ 150 cells/mcL
3. The patient has a documented baseline FEV1 < 80% of
predicted, or additional documentation has been provided to
justify medical necessit y
4. Documentation has been provided indicating patient still is
having significant s ymptoms with ≥ 2 exacerbations in the
previous 12 months requiring additional medical treatment,
(oral s ystemic steroids, emergenc y room visits, hospital
admissions) while compliant on a high-dose inhaled
corticosteroid with a long-acting B2 agonist ± a leukotriene
receptor antagonist or theophylline. If the patient has not
utilized these therapies, a documented medical reason must be
provided wh y patient is unable to do so.
5. Documentation has been provided that patient has been
immunized against varicella if medicall y appropriate or medical
reason for not vaccinating was provided.
6. The prescribed dose is within FDA approved dosing guidelines
Re-Authorization:
1. Documentation submitted indicates the member has clinically
benefited from the medication (FEV1, reduced exacerbations
etc.)
2. The prescribed dose is within FDA approved dosing guidelines
116
Revision/Review
Date 6/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
117
Field Name
Prior Authorization Group
Description
Drugs
Field Description
OPHTHALMIC ANTIHISTAM INES
FORM ULARY STATUS Formulary, Pays at Point-of-Sale
• Alaway OTC (ketotifen)
• Ketotifen OTC (ketotifen)
• Zaditor OTC (ketotifen)
• Zyrtec Itchy Eye OTC (ketotifen)
FORM ULARY STATUS Formulary, Requires Step Therapy (Second Line)
• Pataday (olopatadine)
Note: Patient must meet criteria #1 for approval of initial PA request
FORM ULARY STATUS Non-Formulary, Requires Prior Authorization (Second
Line)
• Bepreve (bepotastine besilate)
• Elestat (epinastine)
• Emadine (emedastine)
• Optivar (azelastine)
• Patanol (olopatadine)
• Lastacaft (alcaftadine)
Or any newly marketed ophthalmic antihistamine
Note: Patient must meet criteria #1 for approval of initial PA request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12 month
duration. If the criterion is not met, the request will be referred to a Clinician for
medical necessity review.
Initial Authorization:
1. Documented trial and failure or intolerance to Zaditor OTC,
Alaway OTC, Zyrtec Itchy Eye OTC or Ketotifen OTC (first
line agents) for at least 2 weeks (14 days) of therapy.
2. Documented trial and failure or intolerance to Pataday
(second line agent) for at least 2 weeks (14 days) of therapy.
Revision/Review Date
7/2016
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
118
123
PERF O RM RX PRIOR AUT HORIZ AT IO N CRIT ERI A
Opiate Dep end ence Agents
GENERIC BUPRENORPHINE/NALOXONE TABLETS ARE THE PREFERRED FORMULARY AGENT
All requests for BRAND or NON-FORMULARY PRODUCTS will REQUIRE DOCUMENTATION of a medical reason (e.g.
contraindication, hypersensitivity) why the generic form of the drug is not able to be used to treat the member’s condition.
Buprenorphine/Naloxone tablets-FORMULARY
Buprenorphine-Non-Formulary
Suboxone-Non-Formulary
Zubsolv-Non-Formulary
Bunavail-Non-Formulary
Any other newly marketed agent for opiate dependence-Non-Formulary
P A CRIT ERI A FOR AP PR OV AL:
INITIAL PA:
o
Patient age > or = 16 years old;
o
Physician meets all qualifications to prescribe buprenorphine/naloxone (Federal, State, and
Local);
o
Patient is diagnosed with opioid dependence and/or opioid addiction
o
The risks of using buprenorphine/naloxone with alcohol or benzodiazepines have been
explained to the patient;
o
No untreated or unstable psychiatric conditions that would interf ere with
buprenorphine/naloxone compliance;
o
No more than one (1) prior attempt to treat opiate addiction with buprenorphine/naloxone
within the prior 12 months (or if an individual has had more than 1 trial in that time frame, an
assessment is completed by a licensed provider indicating the need f or buprenorphine)
o
Negative pregnancy test (f or women, as indicated);
o
Documentation of referral to or active involvement in formal counseling b y a licensed
behavioral health provider (D&A counselor is preferred, but not required). 12-step program
participation, by itself, is not acceptable.
Dosing maximum of 16mg/day (f or Suboxone or buprenorphine) or 11.4mg/2.8mg/day (f or
o
Zubsolv) is requested. On a case-by-case basis clinical consideration can be given to a
dosage up to 24mg/day (Suboxone/buprenorphine) or 17.1/4.2mg (Zubsolv) on an initial
prescription.
If these criteria are met, then an initial maximum of 3 months of buprenorphine/naloxone (1 month
dispensed at a time) or up to a total of 4 week s of buprenorphine will be authorized, depending upon the
request of the physician. If the criteria are not met, psychiatrist review will be necessary to determine
whether other factors, such as age, co-morbidities, social situation, or prior treatment considerations,
would support medical necessity f or the initiation or re-initiation of buprenorphine/naloxone.
RENEWAL PA:
o
Consistent use of buprenorphine/naloxone during the prior 3 m onths, as verified with
pharmacy data. If inconsistent use is noted upon database search (this would NOT include
changes in buprenorphine/naloxone dosing), then written explanation as to wh y
buprenorphine/naloxone should be c ontinued despite apparent noncompliance would be
needed;
o
Documentation of regular (every one to t wo months) urine tests that are negative f or opiates
since previous authorization;
o
Documentation of consistent participation inf orm al counseling by a licensed behavioral
health provider since previous authorization (D&A counselor is preferred, but not required).
12-step program participation, by itself, is not acceptable;
o
Documentation of ongoing behavioral health care f or co-existing behavioral health disorders.
o
For patients consistently off opiates and taking buprenorphine/naloxone f or an extended
period of time and who have successfully completed prescribed f orm al D&A counseling
programs, documentation of active engagement in “after-care” program s, such as NA or AA
or equivalent, will be accepted instead of the above formal counseling requirement.
o
Documentation must be pro vided f or renewals af ter the f irst year that indicate the
prescriber has reevaluated the patient on an annual basis f or a dos age lower than
16m g/day.
If these criteria are met, then an additional 6 months of buprenorphine/naloxone will be authorized (1
125
119
month dispensed at a time). If the criteria are not met, physician review will be necessary to determine
whether other f actors would support medical necessity f or continuation of buprenorphine/naloxone.
REFERENCE:
1. Facts and Comparisons, St. Louis, 2015 eFacts CliniSphere Version ISBN 1-57439-036-8.
2. Suboxone/Subutex. Prescribing Information. Reck itt Benckiser Pharmaceuticals, Inc. Revised April
2014.
3. Zubsolv Prescribing Information. Orexo Pharmaceuticals, Inc. Revised Decem ber 2014.
Review Date: 02/2015
Associated Policy: Prior Authorization of Medications 236.200
NOT E: Physician re v ie w er must ov e rride crit eria w he n, in h is/h er pr ofe s sio n al jud g m ent, the
req u e s ted item is medicall y n ecessar y
126
120
PERFORM RX OR AL CHELATING AGENTS PRIOR AUT HORIZ AT ION CRITERIA
EXJ ADE® (Deferasirox) T ablet for Oral Suspension: 125m g, 250m g, & 500m g
JADENU®(Deferasirox) Tablet: 90mg, 180mg, 360m g
CRITERI A for chronic iron overload due to blood transfusions:
For Pediatric Population:
• Patient m ust be > 2 years old and < 21 years old
and
• Diagnosis of chronic iron overload due to blood transfusions
and
• Patient receiving blood transfusions on a regular basis/participating in blood transfusion program
and
• Serum Ferritin concentration is consistently > 1000 m cg/L. If the serum ferritin levels fall consistently
below 500 m cg/L, Exjade or Jadenu m ust be discontinued
and
• T he medication requested is being prescribed at an F DA approved dose
For Adult Population:
• Patient m ust be > 21 years old
and
• Diagnosis of chronic iron overload due to blood transfusions
and
• Patient receiving blood transfusions on a regular basis/participating in blood transfusion program
and
• Serum Ferritin concentration is consistently > 1000 m cg/L. If the serum ferritin levels fall consistently
below 500 m cg/L, Exjade or Jadenu m ust be discontinued
and
• Documented patient is unable to use Deferoxamine (Desferal) parenterall y
and
• T he medication requested is being prescribed at an F DA approved dose
If the above conditions are m et, the request will be approved for a 6 m onth duration; if the above
conditions are not m et, the request will be ref erred to a Medical Director/clinical reviewer for m edical
necessity review.
CRITERI A for chronic iron overload in non-transfusion dependent thalassemia
Syndromes:
• Patient m ust be ≥ 10 years old
and
• Diagnosis of thalassemia s yndrom e
and
• Liver iron content (LIC) b y liver biops y of ≥ 5 m g Fe/g dr y weight
and
• Serum ferritin level on ≥ 2 measurements one m onth apart of > 300m cg/L
and
• T he medication requested is being prescribed at an F DA approved dose
If the above conditions are m et, the request will be approved for a 3 m onth duration; if the above
conditions are not m et, the request will be referred to a Medical Director/clinical reviewer for m edical
necessity review.
Review/Revision Date 8/2016
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment, the requested item is
medically necessary.
121
PERF ORM RX N AT IO N AL PA CRIT ERI A
®
OXY C ONTIN (oxycodone extended release) T ablet: 10m g, 15m g, 20m g, 30m g, 40m g, 60m g, 80m g
FO RM UL ARY ST AT US: Non-Form ular y
P A C RIT ERI A FOR APPR OV AL:
Chronic Pain:
• Diagnosis of chronic pain requiring an opioid analges ic
AND
• Documented trial and failur e or intolerance to sustained-release m orphine sulf ate
AND
• Documented trial and failur e or intolerance to fentan yl patches
If the above conditions are m et, the request will be app roved with a 6 m onth dur ation; if the above conditions are
not m et, the request will be referred to a Medical Director f or m edical necessity review.
FD A IND IC AT IONS:
Management of moderate-to-severe pain when a continuous, around-the-clock analgesic is needed f or an
extended period of tim e. Not intended f or use as a prn analgesic.
Dosag e and Ad ministrati on
Initial dosage: 10 m g ever y 12 hours.
Dosage titration: Individually titrate to a dose that provides adequate analgesia and m inim izes adverse
reactions. As a guideline, the total dail y ox yc odone dose usually can be increased b y 25% to 50% of the current
dose, each tim e an increase is clinically indicated. Dosage adjustments m ay be done every 1 to 2 da ys.
OxyContin tablets are to be swallowed whole and are not to be brok en, chewed, or crushed. Tak ing brok en,
chewed, or crushed tablets leads to rapid release and absorption of a potentially f atal dose of ox yc odone.
Patients should be started on the lowest appropriate dose. OxyContin 60m g, 80mg, tablets, or a single dose
greater than 40m g, are f or use in opioid-tolerant patients onl y. A single dose greater than 40m g, or total dail y
doses greater than 80m g, may cause f atal respiratory depression when administered to patients who are not
tolerant to the respiratory depressant effects of opioid. The concomitant use of Oxyc ontin with C YP3A4
inhibitors m ay result in increased effects and potentially f atal respiratory depression.
BL ACK BOXED W AR NIN G:
• May cause potentially life-threatening respiratory depression even with t herapeutic use. Ensure proper
dosing and titration; m onitor f or respiratory depression especially within the f irst 24-72 hours of initiation
or dos e escalation.
• Accidental exposure m ay result in f atal overdose of oxycodone, especially in children.
• Healthcare provider should be alert to problem s of abuse, m isuse, and diversion. Patients should be
assessed f or risk of abuse or addiction prior to therapy and all patients should be m onitored f or signs of
misuse, abuse, and addiction. Risk of opioid abuse is increased in patients with a history or fam ily
history of alcohol or dru g abuse or m ental illness.
REFERENCES:
1. American Cancer Society (ACS). National Comprehensive Cancer Network (NCCN). Cancer Pain. Treatment
Guidelines f or Patients. Version II. August 2005.
2. W orld Health Organization. Geneva. 1996. Cancer Pain Relief. Second Edition. W ith a guide to Opioid
Availability.
3. National Institutes of Heath. National Heart, Lung and Blood Institute. Division of Blood Diseases and Resources.
The Management of Sickle Cell Disease. NIH Publication No. 02-02117. June 1997, Revised June 2002.
4. Schneir AB, et al. Massive OxyContin ingestion refractory to naloxone therapy. Ann Emerg Med 2002 Oct;40(4):
425-8.
5. W asserman S. States respond to growing abuse of painkiller. State Legis 2001 Oct-Nov;27(9):33-4.
6. Citron ML, et al. Long-term administration of controlled-release oxycodone tablets f or the treatment of cancer
pain. Cancer Invest 1998;16( 8):562-71.
7. Rischitelli DG, et al. Safety and efficacy of controlled-release oxycodone: a systematic literature review.
Pharmacotherapy 2002 Jul;22(7):898-904.
122
8. Stambaugh JE, et al. Double-blind, randomized co mparison of the analgesic and pharmacokinetic profiles of
controlled- and immediate-release oral oxycodone in cancer pain patients. J Clin Pharmacol 2001 May;41(5):500-6.
9. Neighbors DM, et al. Eco nomic evaluation of the fentanyl transdermal system f or the treatment of chronic
moderate to severe pain. J Pain Sympto m Manage 2001 Feb;21(2):129-43.
10. Mucci-LoRusso P, et al. Controlled-release oxycodone compared with controlled-release morphine in the
treatment of cancer pain: a randomized, double-blind, parallel-group study. Eur J Pain 1998;2(2):239-249.
11. OxyContin (oxycodone controlled release). Prescribing Information. Purdue Pharma L.P. July 2012.
12. Facts and Comparisons, St. Louis, 2015 eFacts CliniSphere Version ISBN 1-57439-036-8.
Revision/Review Date: 11/2015
Associated Polic y: Prior Authorization of Prescription Drugs 236.200
NOT E: Physi cian rev iew er must ov erride criteria w hen, in his/h er profession al judgm ent, the
requested item is m edicall y nece ssa ry.
123
PERFORMRx PRIOR AUTHORIZATION CRITERIA for PCSK9 Inhibitors
ALL PCSK9’s REQUIRE Prior Authorization
Repatha® (evolocumab)- Repatha® is PREFERRED AGENT
Praluent ® (alirocumab)
INITIAL CRITERIA FOR PCSK9 INHIBITORS:
Diagnosis of Familial Hypercholesterolemia (FH)
Patient is 13 year of age or older.
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted includes patient’s complete medical history /co-morbidities.
For patients with a confirmed diagnosis of familial hypercholesterolemia (FH) with chart notes
or clinical labs including 3 of the following:
Autosomal Dominant Hypercholesterolemia Genetic Testing Reflex Panel (ADHP Panel)
documented strong (first and second degree relatives) family history of high levels of
LDL and/or heart attack and relationship to member
documented chart notes of clinical manifestations of FH such as xanthomas or inflamed
tendons
an initial fasting lipid panel prior to treatment ≥ 190mg/dL or ≥ 160mg/dL in children
(lab results must be provided) , and two additional fasting lipid panel laboratory reports
within the past 9 months with abnormal LDL cholesterol levels after treatment with
other lipid lowering agents. ***If patient has been on high dose atorvastatin 80mg or
Rosuvastatin 40mg for a minimum of 3 months, then only one additional fasting lipid
panel in the last 6 months with abnormal LDL is required.***
Documented claim history or chart notes showing consistent therapy (3 months) with
atorvastatin 80mg OR Crestor (Rosuvastatin) 40mg* (*OR documentation has been provided
that patient is of Asian descent in which Crestor 20mg is the max dose) with inadequate
response OR a documented medical reason (e.g. intolerance, hypersensitivity) for not utilizing
one of these therapies to manage their medical condition.
If request indicates that the patient is “statin intolerant”, documentation was provided including
description of the side effects, duration of therapy, “wash out”, re-trial, and then change of
agents.
Documentation has been submitted that provider has counseled patient to follow a “heart
healthy” diet.
Documentation submitted indicates the patient is a non-smoker or provider has counseled
patient regarding smoking cessation.
If request is for Praluent®, documentation of trial and failure or a medical reason has been
provided as to why the member is not able to utilize Repatha® to manage their medical condition.
OR
Diagnosis of artherosclerotic cardiovascular disease (ASCVD)
Patient is 18 year of age or older.
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted includes patient’s complete medical history /co-morbidities.
124
For patients with a confirmed CLINICAL diagnosis of atherosclerotic cardiovascular disease
(ASCVD) requiring additional lowering of low-density lipoprotein (LDL) cholesterol :
documentation has been submitted that the patient is receiving and will continue to
receive maximally tolerated doses of statins
Patient has history of acute coronary syndromes, history of MI, stable or unstable angina,
coronary or other arterial revascularization, stroke, TIA, or peripheral arterial disease
presumed to be of atherosclerotic origin.
Documentation of two fasting lipid panel lab reports within the past 12 months with abnormal
LDL cholesterol levels (>70).
Documented claim history or chart notes showing consistent therapy (3 months) with
atorvastatin 80mg OR Crestor (Rosuvastatin) 40mg* (*OR documentation has been provided
that patient is of Asian descent in which Crestor 20mg is the max dose) with inadequate
response OR a documented medical reason (e.g. intolerance, hypersensitivity) for not utilizing
one of these therapies to manage their medical condition.
If request indicates that the patient is “statin intolerant”, documentation was provided including
description of the side effects, duration of therapy, “wash out”, re-trial, and then change of
agents.
Documentation has been submitted that provider has counseled patient to follow a “heart
healthy” diet.
Documentation has been submitted that the patient is a non-smoker or provider has counseled
patient regarding smoking cessation.
If request is for Praluent®, documentation of trial and failure or a medical reason has been
provided as to why the member is not able to utilize Repatha® to manage their medical condition.
If all of the above conditions are met, the request will be approved for a 3 month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
REAUTHORIZATION CRITERIA FOR PCSK9 INHIBITORS:
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted indicates that the member has obtained clinical benefit from the
medication including repeat fasting lipid panel lab report which shows improvement in LDL from
previous request.
The patient’s claim history shows consistent therapy (i.e. monthly fills)
If all of the above conditions are met, the request will be approved for a 6 month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment, the requested item
is medically necessary.
Revision/Review Date: 2/2017
125
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
8/2016
Field Description
Injectable/Specialty Medications Without Specific Prior Authorization
Protocol
Any injectable or specialty medication that does not have criteria specific to
the drug***PLEASE NOTE FOR ONCOLOGY MEDICATIONS there is
either specific criteria or follow the ONCOLOGY WITHOUT SPECIFIC
CRITERIA POLICY***
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information
for the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
“see other criteria”
N/A
N/A
If all of the conditions are met, requests will be approved for a 6 months. If
the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
• For Non-Formulary agents documentation has been provided that
patient has tried and failed the formulary agents as indicated in
covered uses OR a medical reason has been provided as to why these
agents are unable to be used to treat the patient’s condition (e.g.
intolerance, contraindication, etc.)
• Dosing is appropriate
Physician/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
126
Field Name
Prior Authorization
Group Description
Drugs
Field Description
PEDICULICIDES
FORMULARY STATUS Formulary, Pays at Point-of-Sale
• Permethrin OTC: Lotion / cream rinse and liquid
• Pyrethrins/Piperonyl Butoxide OTC: Shampoo
FORMULARY STATUS Formulary, Requires Step Therapy
(Second Line)
• Natroba (spinosad): Topical Suspension
Note: Patient must meet #1 & #2 criteria for approval of
initial PA request
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Second Line)
• Eurax (crotamiton): Cream and Lotion
• Lindane: Shampoo
• Lycelle: Gel
• Ovide (malathion): Lotion
• Sklice (ivermectin): Lotion
• Or any newly marketed pediculicide
Note: Patient must meet criteria #1, #2 & #3 for approval of
initial PA request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA),
Micromedex, American Hospital Formulary Service (AHFS),
United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI), the Drug Package Insert
(PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
Prescriber Restrictions N/A
Coverage Duration
If the criterion is met, the request will be approved for initial
authorization. For re – authorization, a maximum of 2
treatments in a 30 day period will be approved. If the criterion is
not met, the request will be referred to a Clinician for medical
necessity review.
127
Other Criteria
Initial Authorization:
1. Diagnosis of pediculus capitus (head lice and its eggs)
2. Documented intolerance or hypersensitivity to a first
line agent OR
Documented trial and failure of a first line agent within
the previous 45 days, but no earlier than 7 days after the
original fill.
3. Documented intolerance or hypersensitivity to a
second line agent
OR
Documented trial and failure of a second line agent
within the previous 45 days, but no earlier than 7 days
after the original fill
Re - Authorization:
• Natroba can be approved for a second treatment if live
lice are present 7 days after the initial treatment.
• Ovide can be approved for a second treatment if live lice
are present 7-9 days after the initial treatment.
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria
when, in his/her professional judgement, the requested item
is medically necessary.
128
Field Name
Prior Authorization
Group Description
Drugs
Field Description
PROTON PUMP INHIBITORS (PPIs)
FORMULARY STATUS Formulary, Pays at Point-of-Sale
PRILOSEC (omeprazole) capsule; tablet (generic OTC only)
PRILOSEC (omeprazole) packet for oral suspension (for
members <8 years old only)
PROTONIX (pantoprazole) tablet
FORMULARY STATUS Formulary, Requires Step Therapy
PREVACID/PREVACID 24HR OTC (lansoprazole) capsule:
ZEGERID OTC (omeprazole/sodium bicarbonate) capsule
NEXIUM 24HR OTC (esomeprazole) capsule
Note: Patient must meet criteria #1 & # 2 for approval of the PA
request.
FORMULARY STATUS Non-Formulary, Requires Prior Authorization
ACIPHEX
ACHIPHEX SPRINKLES
DEXILANT (dexlansoprazole)
NEXIUM (esomeprazole) capsules & packet for oral
suspension
PRILOSEC OTC (omeprazole)
PREVACID (lansoprazole) solutabs
Omeprazole Magnesium capsule (generic OTC)
PROTONIX (pantoprazole) packet for oral suspension
ZEGERID (omeprazole/sodium bicarbonate)
Note: Patient must meet criteria #1, # 2 & #3 for approval of the PA
request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
129
Restrictions
Coverage Duration
Other Criteria
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be
referred to a clinical reviewer for medical necessity review.
Initial Authorization
1. Presumed or documented diagnosis of duodenal ulcer,
H.pylori, gastritis, gastric ulcer, GERD, erosive esophagitis,
Barrett’s disease or hypersecretory disease.
2. Documented trial and failure or intolerance with omeprazole
20mg or pantoprazole tablets once daily for a minimum of 3
weeks of therapy within the previous 60 days.
3. Documented trial and failure or intolerance with Prevacid or
Zegerid OTC once daily for a minimum of 3 weeks of therapy.
Doses Greater Than Once Daily After Meeting Criteria For PPI:
1. Confirmed diagnosis of GERD, erosive esophagitis, or
hypersecretory disease.
OR
2. Evaluation made by gastroenterologist and / or
otolaryngologist recommending higher doses of PPI.
Revision/Review
Date 07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
130
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
2/2017
Field Description
Pulmicort® Respules (budesonide)
Pulmicort® Respules (budesonide) inhalation suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration. If the conditions are not met, the request will be sent
to a Medical Director/clinical reviewer for medical necessity review.
Diagnosis of chronic asthma for patients of ages 12 months to 8
years will process at the point of sale without prior authorization
required if dosed within appropriate dosing guidelines as follows:
o 0.25mg/2mL once daily
o 0.5mg/2mL once daily or twice daily
o 1.0mg/2mL once daily
A dose of 0.25mg/2mL twice daily will be approved if prescriber
indicates that once daily dosing is not efficacious and determines
that increasing the dose (i.e. 0.5mg/2mL once daily) is not
appropriate for the patient.
All other requests will be referred to a Medical Director/clinical
reviewer for medical necessity review.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
131
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Pulmonary Arterial Hypertension (PAH) PA Criteria
Adcirca® (tadalafil), Letairis™ (ambrisentan), Revatio® (sildenafil),
Tracleer® (bosentan), Opsumit ® (macitentan), Orenitram™
(Treprostinil Diolamine), Adempas ® (riociguat), Uptravi® (selexipag),
**Flolan® (epoprostenol), **Remodulin® (Treprostinil), **Tyvaso®
(Treprostinil), **Ventavis ® (Iloprost) and any other newly marketed
PAH treatment agents.
** These agents are normally NOT reviewed by PerformRx for KF, AHC, and AHNE
as they are reviewed through the home infusion department.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formular y Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PP I), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
Prescriber must be pulmonologist or cardiologist
If all of the above conditions are met, the request will be approved for 6
month duration, with the exception of Orenitram™ or Uptravi® requests
Orenitram™ and Uptravi® requests will be initially approved for 28 da y
(approve Uptravi ® for an initial 200mcg bottle of #140 for 28 da ys,
subsequent refill with Titration Pack for 28 days or documentation that
patient has achieved highest tolerated dose. Orenitram™ requests
should be approved for 28 days using dose the proper tablets required
according to the titration schedule) Once patient has achieved
maintenance dosing, further refills can be approved for 6 month
duration. Patients new to the plan would be approved for 6 months with
documentation patient is stable on dose. If the conditions are not met,
the request will be sent to a Medical Director/clinical reviewer for
medical necessit y review.
Initial Authorization:
• Documentation of a confirmed diagnosis of pulmonar y arterial
hypertension (PAH) World Health Group (WHO Group I), and
functional class.
• Medication is being used for an FDA approved functional class.
• Documentation that the patient has undergone acute vasoreactivit y
testing and whether or not the results were favorable. For those
patients who demonstrated a favorable response to the acute
vasoreactivit y testing (defined as a fall in mean pulmonary arterial
pressure [PAPm] of at least 10 mm Hg to < 40 mm Hg with an
increased or unchanged cardiac output), then documentation that
his/her pulmonary h ypertension has progressed despite maximal
132
medical treatment with a calcium channel blocker, or documentation
has been provided of medical reason wh y patient is not able to use a
calcium channel blocker.
• Documentation of the patient’s current weight.
• The medication is being recommended and prescribed b y a
pulmonologist or a cardiologist at a dose that is within FDA approved
guidelines.
• If the request is for Revatio® oral suspension, documentation has
been submitted as to wh y patient is unable to use sildenafil or tablets
(e.g. difficult y swallowing)
• If the request is for Opsumit® or Tracleer® the patient must have a
documented trial and failure or intolerance to Letairis™.
• If the provider is requesting combination therap y with two agents
then documentation must be submitted as to why patient is unable to
be treated with monotherap y. (e.g. worsening of the symptoms of
dyspnea or fatigue, decline in functional class b y at least one class or
in 6-minute walk test (6MWD) by greater than 30 minutes)
• If the provider is requesting combination therap y with three agents
then documentation must be submitted of an adequate trial of
therap y with two agents of different mechanism, documentation that
the patient has been compliant with the dual therapy agents, and
documentation that the patient has clinicall y deteriorated (e.g.
worsening of the s ymptoms of dyspnea or fatigue, decline in
functional class b y at least one class or in 6-minute walk test
(6MWD) by greater than 30 minutes) while on dual therap y.
• For Orenitram™ and Uptravi® requests, documentation of current
dosing and titration schedule is required.
• If the request is for Uptravi®, and the patient has functional class II,
documentation has been provided that the patient has tried and failed
an adequate trial (3 months) of a phosphodiesterase-5 inhibitor (e.g.
sildenafil) in combination with an endothelin receptor antagonist (e.g.
Letairis) or a medical reason has been submitted why the patient is
not able to use BOTH of these therapies before starting Uptravi®.
• If the request is for Uptravi®, and the patient has functional class III,
documentation has been provided that the patient has tried and failed
an adequate trial (3 months) of a phosphodiesterase-5 inhibitor (e.g.
sildenafil) in combination with an endothelin receptor antagonist (e.g.
Letairis) AND epoprostenol, or a medical reason has been submitted
why the patient is not able to use ALL of these therapies before
starting Uptravi ®.
Re-authorization:
• Documentation has been submitted indicating the clinical benefit of
133
therap y (e.g. improvement in functional class, improvement in 6minute walk test, exercise capacit y, or hemod ynamics).
• If dosing is being increased, documentation of the medical necessit y
to increase the dosage is provided.
• For Orenitram™ and Uptravi® requests, documentation of current
dosing and titration schedule is required.
• The medication is being recommended and prescribed b y a
pulmonologist or a cardiologist at a dose that is within FDA approved
guidelines.
Revision/Review
Date 4/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgment, the requested item is medically
necessary.
134
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Infor mation
Age Restrictio ns
Prescriber Restrictions
Coverage Duration
Other Criteria
Restasis®
Restasis ® (cyclosporine)
Medically accepted indications are defined using the follo wi ng sources: the Food
and Drug Ad ministration (FDA), Micro medex, American H ospital For mular y
Service ( AHFS), United States Pharmacopeia Drug Infor mati on for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
Prescriber must be an opto metrist, ophthalmologist or rheumatologist.
If the criterion is met, the request will be approved for a one month supply of the
medication with up to a 6 month authorization. If the criterion is not met, the
request will be referred to a Clinician for medical necessity revie w.
Initial Aut horization:
•
•
Diagnosis o f dr y eye syndro me (decreased tear production) whose lack of
tear production is presu med to be suppressed due to ocular inflammation
associated with keratoconjunctivitis sicca.
AN D
Docu mented trial and failure or intolerance to a therapeutic trial of
artificial tear therap y for a period of 3 months.
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
Revision/Review Date
07/2016
135
PERF OR M RX N AT I ON AL PRIOR AUT HORIZ ATION CRIT ERI A
SEDATIVE HYPNOTICS
FORMULARY ST ATUS Form ulary (generic), Pays at Point-of-Sale (First Line)
AMBIEN® (zolpidem) Tablet: 5mg, 10mg
SONAT A® (zaleplon) Capsule: 5mg, 10mg
FORMULARY ST ATUS Formulary, Requires Step Therapy (Second Line)
ROZEREM® (ramelteon) Tablet: 8mg
NOTE: Patient must meet criteria #1 & #2 for approval of initial PA request.
FORMULARY ST ATUS Non-Formulary, Requires Prior Authorization (Third Line)
AMBIEN CR® (zolpidem extended-release) Tablet: 6.25mg, 12.5mg
EDLUAR™ (zolpidem) Sublingual Tablet: 5mg, 10mg
LUNESTA® (eszopiclone) Ta blet: 1mg, 2mg, 3mg
INTERMEZZO® (zolpidem) Sublingual Tablet: 1.75mg, 3.5mg
ZOLPIMIST™ (zolpidem) Oral Solution: 5mcg/actuation, 7.7ml
NOTE: Patient must meet criteria #1, #2 & #3 for approval of initial PA request.
PA CRITERI A FOR APPROV AL :
1. Diagnosis of insomnia.
2. Documented trial and failure or intolerance to Ambien (zolpidem) or Sonata (zaleplon) for at least 2 weeks (14
days) of therapy.
3. Documented trial and failure or intolerance to Rozerem for at least 2 weeks (14 days) of therapy.
NOTE: Rozerem can be approved as a first line agent if there is a history of substance abuse.
If the above conditions are met, the initial request will be approved with a 6 month duration with generic medication. If
the above conditions are not met, the request will be referred to a Medical Director for medical necessity review.
NOTE: Rene wal requests are approvable for up to a 12 month duration.
FDA INDIC ATIONS :
• Ambien: Short-term treatment of insomnia characterized by difficulties with sleep initiation.
• Ambien CR: Treatment of insomnia characterized by difficulties with sleep onset and/or sleep maintenance (as
measured by wake time after sleep onset).
• Edluar: Short-term treatment of insomnia characterized by difficulties with sleep initiation.
• Lunesta: Treatment of insomnia with difficulty of sleep onset and/or sleep maintenance.
• Rozerem: Treatment of insomnia characterized by difficulty with sleep onset.
• Sonata: Short-term treatment of insomnia (7-10 days).
• Intermezzo: For use as needed for the treatment of insomnia when a middle-of-the-night awakening is followed
by difficulty returning to sleep. Not indicated for the treatment of middle-of-the-night insomnia when the patient
has fewer than 4 hours of bedtime remaining before the planned time of waking
• Zolpimist: Short-term treatment of insomnia characterized by difficulties with sleep initiation.
DOSAGE AND ADMINISTRATION:
• Ambien: 5 mg (females) or 5-10 mg (males) immediately before bedtime; max dose: 10 mg daily
• Ambien CR: 6.25 mg (females) or 6.25-12.5 mg (males) immediately before bedtime
• Edluar: 5 mg (females) or 5-10 mg (males) immediately before bedtime; max dose: 10 mg daily For the elderly,
debilitated patients, and patients with hepatic impairment, the recommended dose is 5mg once daily immediately
before bedtime. Edluar sublingual tablet should be placed under the tongue, where it will disintegrate. The tablet
should not be swallo wed and the tablet should not be taken with water. Edluar should not be administered with or
immediately after a meal.
• Lunesta: The recommended starting dose for Lunesta for most non-elderly adults is 2 mg immediately before
bedtime. Dosing can be initiated at or raised to 3mg if clinically indicated, since 3mg is more effective for sleep
maintenance. The recommended starting dose of Lunesta for elderly patients whose primary complaint is
difficulty falling asleep is 1mg immediately before bedtime. In these patients, the dose may be increased to 2mg if
clinically indicated. For elderly patients whose primary complaint is difficulty staying asleep, the recommended
dose is 2mg immediately before bedtime.
• Rozerem: The recommended dose is 8mg taken within 30 minutes of going to bed.
• Sonata: The recommended dose for adults is 10mg immediately before bedtime or after the patient has gone to
bed and has experienced difficulty falling asleep. For certain individuals, 5mg may be a sufficient dose.
• Intermezzo: The recommended and maximum dose of Intermezzo is 1.75 mg for women and 3.5 mg for men,
taken only once per night as needed if a middle-of-the-night awakening is followed by difficulty returning to sleep.
The recommended doses for women and men are different because women clear zolpidem from the body at a
lower rate than men.
• Zolpimist: 5 mg (females) or 5-10 mg (males) immediately before bedtime; max dose: 10 mg
136
REFERENCES:
1. Ambien. Prescribing Information. Sanofi-Aventis. April 2013
2. Ambien CR. Prescribing Information. Sanofi-Aventis. April 2013
3. Edluar. Prescribing Information. Meda Pharmaceuticals. April 2013
4. Lunesta. Prescribing Information. Sepracor, Inc. February 2014
5. Rozerem. Prescribing Information. Takeda Pharmaceuticals America, Inc. November 2010.
6. Sonata. Prescribing Information. W yeth Pharmaceuticals, Inc. May 2013
7. Facts and Comparisons, St. Louis 2011 2012 eFacts CliniSphere Version ISBN 1-57439-036-8.
8. Intermezzo. Prescribing Information. Transcept Pharmaceuticals. July 2012
9. Zolpimist. Prescribing Information. ECR Pharmaceuticals. September 2010.
10. Lexicomp. April 2014
Revision/Revie w Date: 6/2014
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the requested item is
medicall ynecessar y.
137
PERFORMRX NATIONAL PRIOR AUTHORIZ ATION CRITERIA
SEROTONIN RECEPTOR AGONISTS (TRIPTANS)
•
•
•
FORMULARY ST ATUS Formulary, Pays at Point-of-Sale (First Line)
IMITREX (sumatriptan) (generic)
MAX ALT (rizatriptan)
MAX ALT-MLT (rizatriptan)
FORMULARY ST ATUS Non-Formulary, Requires Prior Authorization (Second Line)
•
AMERGE (naratriptan)
•
AXERT (almotriptan)
•
FROVA (frovatriptan)
•
RELPAX (eletriptan)
•
SUMAVEL DOSEPR O (sumatriptan)
•
TREXIMET (sumatriptan/naproxen)
•
ZOMIG (zolmitriptan)
•
ZOMIG-ZMT (zolmitriptan)
NOTE: Patient must meet criteria #1, #2 & #4 for approval of initial PA request.
PA CRITERI A FOR APPROV AL
1.
Diagnosis of migraine headaches.
2.
Diagnosis of cluster headaches (sumatriptan injection only).
3.
An automatic approval for sumatriptan (generic) or rizatriptan at the point-of-sale will occur if the quantities
prescribed do not exceed 12 tablets per 30 days, 2 injection kits (4 injections) per 30 days, and 6 nasal spray units (1
box) per 30 days.
4.
Documented trial and failure at therapeutic doses or intolerance to sumatriptan or rizatriptan.
If the above conditions are met, the request will be approved with a 12 month duration for quantities not to exceed 12
tablets per 30 days, 2 injection kits (4 injections) per 30 days, and 6 nasal spray units (1 box) per 30 days; if the
above conditions are not met, the request will be referred to a Medical Director for medical necessity review.
Quantities Greater Than Allow ed Per 30 Da ys :
If the patient requires doses greater than the set limits after meeting approval, the request will be referred to a
Medical Director for medical necessity review.
FDA INDIC ATIONS
•
Serotonin receptor agonists are indicated for the acute treatment of migraine attacks with or without aura in
adults.
•
Serotonin receptor agonists are not indicated for prophylactic therapy of migraine or for use in the management
of hemiplegic or basilar migraine.
•
Imitrex injection is also indicated for treatment of cluster headache episodes in adults.
DOSAGE AND ADMINISTRATION
IMITREX:
•
Tablet: 25, 50 or 100mg with fluid at onset of headache; may repeat after 2 hours. Do not exceed 200mg in
a 24 hour period.
•
Nasal Spray: 5, 10 (5 mg dose in each nostril) or 20mg (1 spray) at onset of headache, may repeat after 2
hours. Do not e xceed 40mg in a 24 hour period.
• Subcutaneous Injection: 4 or 6mg subcutaneously at onset of headache; may repeat in 1 hour. Do not
exceed 6mg/dose and 12mg in a 24 hour period.
•
Transdermal: Apply 1 patch (6.5mg per 4 hours), may apply a second patch after 2 hours after activation of
first patch. Do not exceed 2 patches per 24 hours
AMERGE :
•
Tablet: 1 or 2.5mg at onset of headache; may repeat after 4 hours. Do not to exceed 5mg in a 24 hour period.
AXERT :
•
Tablet 6.25 or 12.5mg at onset of headache; may repeat after 2 hours. Do not exceed 2 do ses in a 24 hour
period (max 25mg in a 24 hour period).
138
FROVA:
•
Tablet 2.5mg at onset of headache; may repeat after 2 hours. Do not exceed 7.5mg in a 24 hour period.
MAX ALT:
•
Tablet: 5 or 10mg at onset of headache; may repeat after 2 hours. Do not e xceed 30mg in a 24 hour period.
•
Orally Disintegrating Tablet: 5 or 10mg at onset of headache; may repeat after 2 hours. Do not exceed 30mg in
a 24 hour period.
RELPAX :
•
Tablet: 20 or 40mg at onset of headache; may repeat after 2 hours. Do not e xceed a 40mg/dose or 80mg in a
24 hour period.
TREXIMET:
•
Tablet: 85mg/500mg at onset of headache; may repeat after 2 hours. Do not e xceed 170mg/1000mg in a 24
hour period.
SUMAVEL DOSEPRO:
•
Subcutaneous Injection: 6mg subcutaneously at onset of headache; may repeat in 1 hour. Do not exceed 12mg
in a 24 hour period.
ZOMIG:
•
Tablet: 2.5 or 5mg at onset of headache; may repeat after 2 hours. Do not e xceed 10mg in a 24 hour period.
•
Orally Disintegrating Tablet: 2.5 or 5mg at onset of headache; may repeat after 2 hours. Do not exceed 10mg in
a 24 hour period.
•
Nasal Spray: 2.5mg (1 spray) per nostril, max 5mg (2 sprays) at onset of headache; may repeat after 2 hours.
Do not e xceed 10mg in a 24 hour period.
REFERENCES
1.
Amerge Prescribing Information. GlaxoSmithKline. October 2013
2.
Axert (almotriptan) [pres cribi ng information]. Ti tusville, NJ: Janssen Pharmaceuticals Inc; August 2014.
3.
Frova Prescribing Information. Endo Pharmaceuticals, Inc. October 2013
4.
Imitrex (Tablets and Nasal Spray) Prescribing Information. GlaxoSmithKline. November 2013
5.
Imitrex (Subcutaneous Injection) Prescribing Information. GlaxoSmithKline. November 2013
6.
Ma xalt and Ma xalt- ML T Prescribing Information. Merck & Co., Inc. January 2013
7.
Relpa x Prescribing Information. Pfizer. November 2013
8.
Tre ximet Prescribing Information. GlaxoSmithKline. March 2012
9.
Sumavel DosePro Prescribing Information. Zogenix, Inc. February 2014
10.
Zomig, Zomig-ZMT, and Zomig Nasal Spray Prescribing Information. AstraZeneca
Pharmaceuticals.September 2013
11. Facts and Comparisons, St. Louis, 2013 eFacts CliniSphere Version ISBN 1-57439-036-8.
12. Lexi-Comp Online. Available from: http://online.lexi.com.db.usip.edu/crlonline. Updated 4/2015
13. Micromede x Online Available from: http://www.thomsonhc.com.db.usip.edu/hcs/librarian.Updated 4/2015
Revision/Revie w Date: 6/2015
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment,
the requested item is medicall ynecessar y.
139
PerformRx Rituxan Prior Authorization Criteria
RITUXAN® (rituximab
P A CRITERIA F OR APPROVAL FOR USE IN RHEUMATOID ARTHRITIS:
• The medication is being recommended and prescribed by a rheumatologist.
• The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of rheumatoid arthritis.
• The patient has a documented (consistent with pharmacy claims data, OR for new me mbers to the
health plan consistent with medical chart history) adequate trial (including dates and doses) of 3
®
months or more of therapy) of methotrexate AND then leflunomide (generic Arava ) and/or another
disease-modifying antirheumatic treatment option (i.e. combination therapy - methotrexate +
sulfasalazine and/or hydroxychloroquine) or has another documented medical reason (e.g. intolerance,
hypersensitivity) for not utilizing any of these therapies to manage their medical condition.
• T he patient has a documented (consistent with pharmacy claims data, OR for new members to the
health plan consistent with medical chart history) adequate trial (including dates, doses) of all preferred
biologics indicated for rheumatoid arthritis, or has documented medical reason (intolerance,
hypersensitivity, etc.) for not taking ALL of these therapies to manage their medical condition.
• Documentation indicating that Rituxan is being used concurrently with methotrexate.
• Documentation indicating that patient has been screen for HBV (hepatitis B virus) prior to initiation of
treatment
• Rituxan is being prescribed at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 1 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
P A CRITERIA F OR RE-AUTHORIZATION FOR USE IN RHEUMATOID ARTHRITIS
• The member has been receiving Rituxan and documentation is provided that a rheumatologist has
reevaluated the member and recommends continuation of therapy.
• Documentation was provided indicating that the patient had clinical benefit from receiving Rituxan
therapy.
• At least 16 weeks (4 months) has elapsed since the previous course of Rituxan therapy.
• Documentation indicating that Rituxan is being used concurrently with methotrexate.
• Rituxan is being prescribed at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 1 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
P A CRITERIA F OR INITIAL APPROVAL F OR USE IN NON-HODGKIN’S LYMPHOMA
(NHL) AND CHRONIC LYMPHOCYTIC LEUKEMIA (CLL):
• The medication is being recommended and prescribed by an oncologist.
• If the medication request is for Non-Hodgkin Lymphoma, documentation was submitted of confirmed
diagnosis of CD20-positive B-cell NHL
• If the medication request is for Chronic Lymphocytic Leukemia, documentation was submitted of
confirmed diagnosis of CD20-positive CLLand Rituxan is being using in concurrently with fludarabine and
cyclophosphamide (FC)
• Documentation indicating that patient has been screen for HBV (hepatitis B virus) prior to initiation of
treatment
• Rituxan is being prescribed at a dose that is within FDA approved guidelines and/or is supported
by the medical compendium as defined by the Social Security Act and/or the National
Comprehensive Cancer Network (NCCN) or American Society of Clinical Oncology (ASCO)
standard of care guidelines.
If all of the above conditions are met, the request will be approved for up to a 3 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
140
P A CRITERIA F OR RE-AUTHORIZATION FOR USE IN NON-HODGKIN’S LYMPHOMA
(NHL) AND CHRONIC LYMPHOCYTIC LEUKEMIA (CLL):
• The medication is being recommended and prescribed by an oncologist.
• Rituxan is being prescribed at a dose that is within FDA approved guidelines and/or is
supported by the medical compendium as defined by the Social Security Act and/or per the
NCCN or ASCO standard of care guidelines.
If all of the above conditions are met, the request will be approved for up to a 3 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
P A CRITERIA FOR INITIAL APPROVAL FOR USE IN GRANULOMATOSIS WITH
POLYANGIITIS (GP A) (WEGENER’S
GRANULOMATOSIS) AND MICROSCOPIC
POLYANGIITIS (MP A):
• The medication is being recommended and prescribed by a rheumatologist.
• The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of granulomatosis
with polyangiitis (GPA) (Wegener’s Granulomatosis) or microscopic polyangiitis (MPA).
• The patient has a documented (consistent with pharmacy claims data, OR for new me mbers
to the health plan consistent with medical chart history) adequate trial (including dates,
doses) of glucocorticoid (i.e. prednisone) AND methotrexate, OR glucocorticoid AND
cyclophosphamide (Cytoxan®) or documentation includes a medical reason (intolerance,
hypersensitivity, etc.) why patient is not able to use these therapies to manage their medical
condition.
• Documentation indicating that Rituxan is being used concurrently with glucocorticoids.
• Documentation indicating that patient has been screen for HBV (hepatitis B virus) prior to initiation of
treatment
• Rituxan is being prescribed at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 1 month duration; if
all of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer
for medical necessity review.
P A CRITERIA F OR INITIAL AUTHORIZATION FOR USE IN OTHER MEDICALLY
ACCEP TED INDICATIONS
• The medication is prescribed for a non-FDA approved indication but is considered to be a
medically accepted use of the medication per the medical compendia (Micromedex,
American Hospital Formulary Service (AHFS), DrugPoints, the Drug Package Insert as
defined in the Social Security Act and/or per the National Comprehensive Cancer Network
(NCCN), the American Society of Clinical Oncology (ASCO) or the American Academy of
Pediatrics (AAP) standard of care guidelines AND has a Class I or IIa recommendation.
• The medication is prescribed at a medically accepted dose per the medical compendia as
defined above.
• The medication is recommended and prescribed a specialist in the field to treat the member’s respective
medical condition.
• Documentation indicating that patient has been screen for HBV (hepatitis B virus) prior to initiation of
treatment
• Documentation was submitted indicating that the member has a documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with medical chart
history) adequate trial (including dates, doses of medications) of ALL first line medical
therapies as recommended by the medical compendia and standard care guidelines and/or has
another documented medical reason (e.g. intolerance, contraindications, etc.) for not receiving
or trying all first line medical treatment(s).
If all of the above conditions are met, the request will be approved for up to a 3 month duration. If
all of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer
for medical necessity review.
P A CRITERIA F OR RE-AUTHORIZATION FOR USE IN OTHER MEDICALLY ACCEPTED
INDICATIONS
141
• The medication is prescribed at a medically accepted dose per the medical compendia
• The medication is recommended and prescribed a specialist in the field to treat the me mber’s
respective medical condition.
• Documentation from medical chart was submitted indicating that the member has significantly
clinically benefited from the medication.
If all of the above conditions are met, the request will be approved for up to a 3 month duration. If all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
Revision/Review Date: 4/2016
NOTE: P hysician/clinical review er must override criteria w hen, in his/her professional
judgment, the requested item is medically necessary.
142
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Second Generation Antihistamines PA Criteria
FORMULARY STATUS Formulary, Pays at Point-of-Sale (First
Line)
®
ALLEGRA (fexofenadine) (generic) (Only children < 2 years old
will pay at point of sale)
CLARITIN® (loratadine) (generic) tablets, 10 mg orally
disintegrating tablets, oral syrup
ZYRTEC® (cetirizine) (generic) tablets, oral solution
ZYRTEC-D® 12 HOURS (cetirizine/pseudoephedrine) (generic)
CLARITIN-D® 12 HOUR (loratadine/pseudoephedrine) (generic)
CLARITIN-D® 24 HOUR (loratadine/pseudoephedrine) (generic)
FORMULARY STATUS Formulary, Requires Step Therapy (Second
Line)
®
ALLEGRA (fexofenadine) (generic) oral suspension and 180 mg
tablets only
ALLEGRA® (fexofenadine)
XYZAL® (levocetirizine) tablets
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Third Line)
ALLEGRA® (fexofenadine) 60 mg tablets
ALLEGRA-D® 12 HOUR (fexofenadine/pseudoephedrine)
ALLEGRA-D® 24 HOUR (fexofenadine/pseudoephedrine)
CLARITIN® (loratadine) (generic) 5 mg orally disintegrating tablets
CLARINEX® (desloratadine)
CLARINEX-D® 12 HOUR (desloratadine/pseudoephedrine)
SEMPREX-D (pseudoephedrine/acrivas)
XYZAL® (levocetirizine) oral solution
ZYRTEC® (cetirizine) (generic) chewable tablets, orally
disintegrating tablets, capsules
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug
Package Insert (PPI), or disease state specific standard of care
guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration; If the conditions are not met, the request will be sent to
143
a Medical Director/clinical reviewer for medical necessity review.
Other Criteria
NOTE: Patient must meet #1, #2, & #3 criteria for approval of PA
request.
PA CRITERIA FOR APPROVAL:
1. Diagnosis of seasonal allergic rhinitis with or without nasal
congestion, perennial allergic rhinitis with or without nasal
congestion, or urticaria.
2. Documented trial and failure or intolerance to a first line
loratadine AND cetirizine product for at least 4 weeks (28 days)
of therapy each within the past 12 months or a minimum of 2
weeks of therapy or intolerance to Claritin-D and Zyrtec-D
within the past 12 months.
3. Documented trial and failure or intolerance to fexofenadine or
levocetirizine tablets for at least 4 weeks (28 days) of therapy in
the past 12 months.
Revision/Review
2/2017
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
144
PERF ORMRX SEROSTIM P RIOR AUT HORIZ ATI ON CRITERIA
SEROSTIM® (somatropin) Formulary Status: Non-formular y
PA CRITE RI A FOR INITI AL APPR OV AL FOR HIV REL AT ED W AST IN G OR CAC HEXI A:
•
•
•
•
•
•
•
•
•
•
•
•
The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of HIV
Prescriber is HIV or infectious disease specialist
The patient is receiving optimal highly active antiretroviral therapy (HAART) as documented
by a recent (with in past 2 months) infectious disease specialist consultation or by recent (with in
past 2 months) laboratory blood analysis indicating plasma HIV RNA of less than 50 copies/ml
Documentation was submitted that indicates that the member does not have cancer (excluding
Kaposi’s sarcoma & Lymphoma)
Documentation was submitted that indicates that the member does not have any
psychiatric disorders, such as anxiety and depression, or documentation was submitted
that the member is receiving treatment for a psychiatric disorder
Documentation was submitted that indicates that the member does not have any active
opportunistic infections (thrush, MAC), diarrhea and GI infections, or that if they have any of
these conditions it is clinically resolved and stabilized with treatment
For male patients, laboratory values were submitted indicating testosterone levels are within
normal limits, or that the patient is receiving testosterone supplementation and documentation was
submitted indicated testosterone levels are within normal limits
The patient is receiving documented nutritional support
Documentation has been provided including patient’s weights, BMI (in kg/m2), and lean body
mass (LBM) by DEXA (baseline and repeat over the last six months)
Documentation provided demonstrates an involuntary weight loss >10% of baseline body
weight associated with either chronic diarrhea (two or more loose stools per day for ≥1
month) or chronic weakness and documented fever for ≥1 month that is not attributable to
a concurrent condition other than HIV infection itself or 2) current weight loss > 5% in a 1mo period or 3) actual BMI (in kg/m2) < 19
The patient has tried a 2 month or more course of therapy with megestrol acetate,
dronabinol or cyproheptadine for appetite stimulation in the past 2 months or has a
documented medical reason for not taking megestrol acetate, dronabinol or cyproheptadine.
The patient has tried a 2 month course of therapy with anabolic steroids (e.g., Oxandrin) in
the past 2 months or has a medical reason for not taking an anabolic steroid.
If all of the above conditions are met, the request will be approved with a 4-week duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
P A CRITERI A F OR RE- APPROV AL F OR HIV RELATED WASTING OR CACHEXIA:
• Documentation was sent in at the end of 4 weeks of a repeat BIA analysis that shows the
patient’s lean body mass has stabilized or improved
• If the last trial of Serostim® was in the distant past and was successful, then evaluate the
patient as naïve
If all of the above conditions are met, the request will be approved for 12 weeks. If all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
P A CRITERI A F OR INITIAL APPROVAL FOR HIV RELATED LIPODY STROPHYor
HIV ASSOCIATED ADIPOSE REDISTRIBUTION SY NDROME:
• The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of HIV.
• Documentation that the patient does not have diabetes mellitus and is not receiving any
insulin or insulin-sensitizing agents.
• Documentation that the patient is compliant with an unchanged HAART for at least 3
months prior to the initiation of therapy.
• Documentation was submitted that indicates that the member does not have an active
infection or malignancy(excludes patients with less than five cutaneous Kaposi’s sarcoma
lesions).
• Documentation that the patient does not have untreated or uncontrolled hypertension (i.e.
blood pressure > 140/90 mm Hg).
145
•
•
•
Prescriber is HIV or infectious disease specialist
A letter of medically necessity documenting the evidence of HIV related lipodystrophy.
The medication is prescribed at a medically accepted dose per the medical compendia (i.e.
Micromedex, DrugPoints and AHFS drug information) as defined by the Social Security
Act or per the standard of care guidelines.
If all of the above conditions are met, the request will be approved with a 12-week duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
P A CRITERI A F OR RE- APPROV AL F OR HIV RELATED LIPODYSTROPHY or
HIV ASSOCIATED ADIPOSE REDISTRIBUTI ON SY NDROME:
• Duration of therapy does not exceed 9 months.
•
The prescribing physician has provided documentation as to the clinical
benefits of the medication supporting continued treatment.
•
The medication is prescribed at a medically accepted dose per the medical compendia (i.e.
Micromedex, DrugPoints and AHFS drug information) as defined by the Social Security Act
or per the standard of care guidelines.
If all of the above conditions are met, the request will be approved with a 24-week duration (9
months total); if all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
P A CRITERIA FOR AUTHORIZATION FOR USE IN A NON-FDA APPROVED
MEDICALLY ACCEP TED INDICATION:
• The medication is recommended and prescribed by a specialist in the field to treat the
member’s respective medical condition.
•
The medication is prescribed for a non-FDA approved indication but is considered to be
a medically accepted use of the medication per the medical compendia (i.e. Micromedex,
DrugPoints and AHFS drug information) as defined by the Social Security Act or the
standard of care guidelines.
•
Documentation was submitted indicating that the member has a documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with medical chart
history) adequate trial (including dates, doses of medications) of all first line medical therapies as
recommended by the medical compendia and standard care guidelines or has another
documented medical reason (i.e. intolerance, contraindications) for not receiving or trying all
first line medical treatment(s).
• The medication is prescribed at a medically accepted dose per the medical compendia as defined
by the Social Security Act or per the standard of care guidelines.
If all of the above conditions are met, the request will be approved for up to a 12-week duration. If all
of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
P A CRITERIA FOR RE-AUTHORIZATION FOR USE IN A NON-FDA
APPROVED MEDICALLY ACCEPTED INDICATION:
• The medication is recommended and prescribed by a specialist in the field to treat the
member’s respective medical condition.
•
The medication is being prescribed at a medically accepted dose per the medical
compendia (i.e. Micromedex, DrugPoints and AHFS drug information) as defined by the
Social Security Act or per the NCCN or ASCO standard of care guidelines.
•
The prescribing physician has provided documentation as to the clinical benefits of the
medication supporting continued treatment, OR the medication is being continued in
accordance with the recommended time as defined by FDA drug package insert, or per
recommendations of the medical compendium as described above, or per the standard of
care guidelines.
If all of the above conditions are met, the request will be approved for up to a 12-week duration. If
all of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer
for medical necessity review.
NOTE: P hysician review /clinical reviewer must override criteria w hen, in his/her professional
judgement, the requested item is medically necessary.
146
Revision/Review Date: 8/2016
147
PERFORMRX SOLIRIS PRIOR AUTHORI ZATION CRITERIA
SOLIRIS®(Eculizumab)
Formulary Status: Non-formulary
PA CRITERIA FOR APPROVAL FOR Paroxysmal nocturnal hemoglobinuria (PNH):
• Patient has a confirmed diagnosis of paroxys mal nocturnal hemo globinuria (PNH)
• Documentation was sub mitted with the follo wing lab results within 30 days of request: CBC with
differential, iron studies (serum iron, total iron binding capacity, and ferritin), the last pre-transfusio n
hemoglobin level, a Lactase dehydrogenase (LDH) level, a PNH type III erythrocyte level proportion of 10%
of more, serum creatinine, AST, and urinalysis
• Documentation sub mitted indicates that the patient has been vaccinated with the meningococcal vaccine
at least 2 weeks prior to initiation of Soliris therap y and/or revaccinated according to current medical
guidelines for vaccine use
• T he medication is being prescribed by a hematologist at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 6-month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
REAUTHORI ZATION CRITERIA for PNH:
• For first reauthorization requests: documentation fro m medical chart was sub mitted indicating that a
hematologist has evaluated the member and reco mmends continuation of therap y due to submitted
clinical/diagnostic documentat ion that demonstrates that the member has benefited fro m the medication (e.g.
reduced number of red blood cell transfusions, decreased LDH level, improved hemoglobin levels, increase
in PNH type III erythrocytes, improved fatigue or quality of life) since beginning therap y with Soliris.
• For additio nal reauthorization requests beyo nd 12 months of therap y: documentation fro m medical chart
was sub mitted indicating that a hematologist has evaluated the member and recommends continuation of
therapy due to the member has remained clinically stable while on Soliris (e.g. red blood cell transfusion
requirements have remained the stable or reduced, LDH level remained close to upper limits of normal, hemo
globin levels re maining stable, PNH type III erythrocytes stable or improved, lo w to no fatigue and continues
with improved quality of life) while taking Soliris therap y.
• Documentation was sub mitted indicating the date of the me mber’s last meningococcal vaccine.
• T he medication is being prescribed by a hematologist at an FDA approved dosage.
If all of the abo ve conditions are met, the request will be approved for up to a 6 -month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medic al necessity
review.
PA CRITERIA FOR APPROVAL for Atypical Hemolytic Uremic Syndro me (aHUS)
• Patient has a confirmed diagnosis of aHUS (e.g. genetic testing, chart notes or labs indicating
microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury)
• Documentation provided indicates disease is NOT caused by Shiga toxin E. coli related hemolytic
uremic syndrome (STEC-HUS)
• Documentation submitted indicates that the patient has been vaccinated with the meningococcal
vaccine at least 2 weeks prior to initiation of Soliris therapy and/or revaccinated according to current
medical guidelines for vaccine use
• The medication is being prescribed by a hematologist at an FDA approved dosage
• Documentation was submitted with the following lab results within 30 days of request: CBC with
differential, a Lactase dehydrogenase (LDH) level, serum creatinine, AST, and urinalysis
If all of the above conditions are met, the request will be approved for up to a 6-month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
148
REAUTHORI ZATION CRITERIA for aHUS:
For first reauthorizatio n requests:
• Documentation fro m medical chart was sub mitted indicating that a hematologist has evaluated the
me mber and recommends continuation of therap y due to submitted clinical/diagnostic documentation that
demonstrates that the me mber has benefited fro m the medication since beginning therap y with Soliris.
• Medication is being prescribed by a hematologist at an FDA approved dosage
For additional reauthorization requests beyond 12 months of therap y:
• Documentation fro m medical chart was sub mitted indicating that a hematologist has evaluated the member
and recommends continuation of therap y due to the member has remained clinically stable while on Soliris
• Documentation was sub mitted indicating the date of the me mber’s last meningococcal vaccine.
• T he medication is being prescribed by a hematologist at an FDA approved dosage.
FDA INDICATION:
Soliris is indicated for treatment of adult patients (18 y/o or older) with paroxys mal nocturnal
hemoglobuinuria (PNH) to reduce hemolysis and for the treatment of patients with atypical hemolytic uremic
syndro me (aHUS) to inhibit co mp lement-mediated thro mbotic microangiopathy.
Soliris is not indicated for the treatment of patients with Shiga toxin E. coli related he molytic uremic
syndro me (ST EC-HUS).
DOSAGE AND ADM INISTRATION:
Dosage Regimen - PNH:
600 mg as an IV infusion over 35 minutes given every 7 days for the first 4 weeks, follo wed by:
900 mg IV over 35 minutes for the 5 th dose 7 days later then,
900 mg IV over 35 minutes every 14 days thereafter.
Dosage Regimen - aHUS:
For patients ≥ 18 yo:
900 mg as an IV infusion over 35 minutes given ever y 7 days for the first 4 weeks, follo wed by
1200 mg IV over 35 minutes for the 5 th dose 7 days later then,
1200 mg IV over 35 minutes every 14 days thereafter.
For patients ≤ 18 yo:
Patient Body
40 kg and over
30 kg to less than
40 kg
20 kg to less than
30 kg
10 kg to less than
20 kg
5 kg to less than 10
kg
Induction
900 mg weekly x
4 doses
600 mg weekly x
2 doses
600 mg weekly x
2 doses
Maintenance
1200 mg at week 5; then
1200 mg every 2
900 mg at week 3; then 900
mg every 2 weeks
600 mg at week 3; then 600
mg every 2 weeks
300 mg at week 2; then 300
mg every 2 weeks
600 mg weekly x 1
dose
300 mg at week 2; then 300
mg every 3 weeks
300 mg weekly x 1
dose
149
Supplemental dose of Soliris after PE/PI (plas mapheresis or plasma exchange; or fresh frozen plasma
infusion):
Type of
Interventio
n
Plasmapheresis
or plasma
exchange
Fresh
frozen
plasma
infusion
Most Recent
Soliris Dose
300 mg
Supplemental Soliris
Dose
With Each PE/PI
Intervention
300 mg per each
plasmapheresis or plasma
600 mg or more 600 mg per each
plasmapheresis or plasma
300 mg or more
300 mg per each unit of
fresh frozen plasma
Timing of
Supplemental
Soliris Dose
Within 60
minutes after
each
plasmapheresis or
60 minutes prior
to each 1 unit of
fresh frozen
plasma infusion
REFERENCES:
1. Soliris® prescribing infor mation. Alexion Phar maceuticals, Inc. 1/2016
2. Hillmen P. Young NS. Schubert J. et al. T he complement inhibitor eculizumab in paroxysmal nocturnal
hemoglobinuria. T he New England Journal of Medicine. 2006;355:1233-1243.
3. Hill A. Richards SJ. Hillmen P. Recent develop ments in the understanding and management of
paroxysmal nocturnal haemoglobinuria. British Journal of Haematology. 2007;137:181-192.
4. Parker C. Omine M. Richards S. et al. Diagnosis and manage ment of paroxysmal nocturnal
hemoglobinuria. Blood. 2005;106(12):3699-3709.
5. http://www.nlm.nih.gov/medlineplus/ency/article/003471.htm. For Definition of LDH.
Revision/Review Date: 8/2016
NOTE: Clinical reviewer must override criteria when, in his/her
professional judg ment, the requested ite m is medically necessary.
150
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents for
Crohn’s Disease
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
REMICADE® (infliximab)
CIMZIA® (certolizumab)
ENTYVIO®(Vedolizumab)
STELARA® (ustekinumab
Or any newly marketed agent
PA CRITERIA FOR APPROVAL FOR CROHN’S DISEASE:
The member is (≥6y/o) and has a documented clinical diagnosis of moderate to severely active Crohn’s
disease.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health
plan consistent with medical chart history) adequate trial (including dates and doses) at therapeutic doses or
has a documented clinically significant medical reason for not receiving conventional oral therapy (e.g.
azathioprine, corticosteroids, 6-mercaptopurine) to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB infection
(i.e. tuberculin skin test) as indicated in package insert.
The medication requested has an FDA approved indication for use in patients with moderate to severe active
Crohn’s disease and is being recommended and prescribed by a gastroenterologist at an FDA-approved dosage
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial of the preferred biological
agents.
If all of the above conditions are met, the request will be approved for up to a 6 -month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR CROHN’S DISEASE:
The medication is being recommended and prescribed by a gastroenterologist for an FDA -approved indication
at an FDA-approved dosage.
For members who require Humira 40 mg SC weekly, documentation must be submitted indicating that the
member was compliant (consistent with pharmacy claims) with receiving at least 16 weeks of continuous Humira
therapy every other week prior to the request for weekly dosing of Humira.
If all of the above conditions are met, the request will be approved for a 6-month duration for Remicade requests and
for a 12 month duration for all other medications; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date: 11/2016
151
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for Ulcerative Colitis
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
REMICADE® (infliximab)
SIMPONI® (golimumab)
ENTYVIO®(Vedolizumab) Or any newly marketed agent
PA CRITERIA FOR APPROVAL FOR ULCERATIVE COLITIS:
The patient is (≥6 y/o) and has moderate to severe active ulcerative colitis.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) treatment failure after receiving an adequate trial of:
o Sulfasalazine (3 to 6 g/day for 3 months), or mesalamine (1.2 to 2.4 g/day for 3 months), or azathioprine
(2 to 2.5 mg/kg/day), or 6-mercaptopurine (1.5 to 2 mg/kg/day), or oral corticosteroids or has a
documented medical reason (GI intolerance, hypersensitivity, etc.) for not taking any of these
medications to treat their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB infection (i.e.
tuberculin skin test) as indicated in package insert.
The medication requested has a FDA approved indication for use in patients with moderate to severe active
ulcerative colitis and is being prescribed at an FDA-approved dosage and is recommended or prescribed by a
gastroenterologist.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial of the preferred biological
agents.
If all of the above conditions are met, the request will be approved for up to a 6 -month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR ULCERATIVE COLITIS:
The medication is being recommended and prescribed by a gastroenterologistt for an FDA-approved indication at
an FDA-approved dosage.
The member has been receiving the medication and documentation was provided that the prescriber has
evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the medication.
If all of the above conditions are met, the request will be approved for a 6-month duration for Remicade requests and
for a 12 month duration for all other medications; if all of the above criteria are not met, the request is referred to a
Medical Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/Clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date: 11/2016
152
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for Psoriasis
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
REMICADE® (infliximab)
OTEZLA® (Apremilast
COSENTYX® (Secukinumab)
STELARA® (ustekinumab) TALTZ (Ixekizumab)
Or any newly marketed agent
PA CRITERIA FOR APPROVAL FOR PSORIASIS:
The member is an adult (≥18 y/o) and has a documented clinical diagnosis of moderate to severe plaque
psoriasis.
Documentation that the patient has had (consistent with pharmacy claims data, OR for new members to the
health plan consistent with medical chart history) adequate trials (including dates and dose s) of at least 3 of the
treatment bullet points listed below:
o The use of topical steroids or has a documented medical reason for not using this therapy to manage
their medical condition.
®
®
o The use of a topical medication [i.e. Dovonex (calcipotriene), Tazorac (tazorotene), anthralin or a coal
tar preparation] that is indicated for the treatment of psoriasis or has a documented medical reason for
not using any of these therapies to manage their medical condition.
o The use of methotrexate or has a documented medical reason (e.g. history of liver or kidney disease,
pregnancy, severe cytopenia, alcoholism) for not using this therapy to manage their medical
condition.
o The use of cyclosporine or has a documented medical reason for not using this therapy to manage their
medical condition.
®
o The use of Soriatane (acitretin) or has a documented medical reason for not using this therapy to
manage their medical condition.
o The use of UVB phototherapy or PUVA (psoralen – oral or topical methoxsalen plus UVA therapy) or
has a documented medical reason (e.g. pregnancy, skin cancer, hypersensitivity due to preexisting
disease state - e.g. systemic lupus erythematus, cataracts) for not undergoing UVB phototherapy or
PUVA to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB infection (i.e.
tuberculin skin test) as indicated in the package insert.
The medication requested has an FDA approved indication for use in patients with moderate to severe plaque
psoriasis and is being recommended or prescribed by a dermatologist at an FDA-approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) If the request is for a non-preferred agent,
documented (consistent with pharmacy claims data, OR for new members to the health plan consistent with
medical chart history) adequate trial of the preferred biological agents.
If all of the above conditions are met, the request will be approved for up to a 6 month duration. If all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR PSORIASIS:
The medication is being recommended and prescribed by a dermatologist at an FDA-approved dosage.
The member has been receiving the medication and documentation was provided that the prescriber has
evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the medication.
If all of the above conditions are met, the request will be approved for a 6-month duration for Remicade requests and for
a 12 month duration for requests for all other medications. If all of the above criteria are not met, the request is referred
to a Medical Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date: 11/2016
153
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for Polyarticular Juvenile Idiopathic Arthritis
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
ACTEMRA® (tocilizumab)
ORENCIA® (abatacept)
Or any newly marketed agent
PA CRITERIA FOR APPROVAL FOR POLYARTICULAR JUVENILE IDIOPATHIC ARTHRITIS:
The patient is a child (< 17 y/o), within the FDA approved age range for the medication
requested, and has a documented clinical diagnosis of juvenile idiopathic arthritis.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the
health plan consistent with medical chart history) adequate trial (includi ng dates and doses) of 2
months or more of therapy with at least one disease-modifying anti-rheumatic drug (DMARD) (e.g.
methotrexate), or has a documented medical reason (e.g. intolerance, hypersensitivity) for not
utilizing any of these therapies to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB
infection (i.e. tuberculin skin test) as indicated in package insert.
The medication requested has an FDA approved indication for use in patients with juvenile
idiopathic arthritis and is being recommended and prescribed by a rheumatologist or pediatric
rheumatologist at an FDA-approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with medical chart history) adequate
trial of the preferred biological agents.
If all of the above conditions are met, the request will be approved for up to a 6 -month duration; if
all of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer
for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR POLYARTICULAR JUVENILE IDIOPATHIC ARTHRITIS:
The medication is being recommended and prescribed by a rheumatologist or pediatric
rheumatologist at an FDA-approved dosage.
The member has been receiving the medication and documentation was provided that the
prescriber has evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the
medication.
If all of the above conditions are met, the request will be approved for a 12 month duration for requests
for all other medications. If all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date: 11/2016
154
PERFORMRX PRIOR AUTHORIZATION CRITERIA for Specialty Biological
Agents for Systemic Juvenile Idiopathic Arthritis
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
ACTEMRA® (tocilizumab)
ORENCIA® (abatacept)
Or any newly marketed agent
PA CRITERIA FOR APPROVAL FOR SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS:
The patient is a child (< 17 y/o), within the FDA approved age range for the medication requested,
and has a documented clinical diagnosis of systemic juvenile idiopathic arthritis.
Documentation was submitted indicating that the member was evaluated for active or latent TB
infection (i.e. tuberculin skin test) as indicated in the package insert.
The medication requested has an FDA approved indication for use in patients with systemic juvenile
idiopathic arthritis and is being recommended and prescribed by a rheumatologist or a pediatric
rheumatologist at an FDA - approved dosage.
If all of the above conditions are met, the request will be approved for a 6-month duration. If all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS:
The medication is being recommended and prescribed by a rheumatologist or pediatric
rheumatologist at an FDA-approved dosage.
The member has been receiving the medication and documentation was provided that the
prescriber has evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the
medication.
If all of the above conditions are met, the request will be approved for a 12 month duration for requests
for all other medications. If all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
Revision/Review Date: 11/2016
155
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for FDA (if no indication specific criteria) and NON-FDA Approved Medically
Accepted Indications
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
ACTEMRA® (tocilizumab)
CIMZIA® (certolizumab)
KINERET® (anakinra)
ORENCIA® (abatacept)
SIMPONI® (golimumab)
STELARA® (ustekinumab)
ENTYVIO® (Vedolizumab)
OTEZLA® (Apremilast)
COSENTYX® (Secukinumab)
REMICADE® (infliximab)
XELJANZ® (tofacitinib)
TALTZ (Ixekizumab)
Or any newly marketed agent
PA CRITERIA FOR AUTHORIZATION FOR OTHER FDA or NON-FDA APPROVED MEDICALLY
ACCEPTED INDICATIONS:
The medication is prescribed for a non-FDA approved indication that is considered a medically
accepted use of the medication per the medical compendia (i.e. Micromedex, DrugPoints, AHFS drug
information) as defined by the Social Security Act.
The medication is prescribed at a medically accepted dose per the medical compendia as defined by
the Social Security Act.
The medication is recommended and prescribed by a specialist in the field to treat the member’s
respective medical condition.
Documentation was submitted indicating that the member has a documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with medical chart
history) adequate trial (including dates, doses of medications) of all first line medical therapi es as
recommended by the medical compendia and standard of care guidelines or has another
documented medical reason (e.g. intolerance, contraindications) for not receiving or trying all first
line medical treatment(s).
Documentation was submitted indicating that the member was evaluated for active or latent TB
infection (i.e. tuberculin skin test) as indicated in package insert.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data,
OR for new members to the health plan consistent with medical chart history) adequate trial of
at least two preferred biological agents (if possible).
If all of the above conditions are met, the request will be approved for up to a 6 month duration. If all
of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR OTHER NON-FDA APPROVED MEDICALLY ACCEPTED
INDICATIONS:
The medication is prescribed at a medically accepted dose per the medical compendia as
defined by the Social Security Act.
The medication is recommended and prescribed by a specialist in the field to treat the member’s
respective medical condition.
Documentation submitted indicates that the member has obtained clinical benefit from the
medication.
If all of the above conditions are met, the request will be approved for a 6 -month duration. If all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
156
Revision/Review Date: 11/2016
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for Rheumatoid Arthritis
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
ACTEMRA® (tocilizumab) CIMZIA® (certolizumab) KINERET®
(anakinra)
ORENCIA® (abatacept)
SIMPONI® (golimumab)
REMICADE® (infliximab)
XELJANZ® (tofacitinib)
Or any newly marketed agent
PA CRITERIA FOR APPROVAL FOR RHEUMATOID ARTHRITIS:
The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of rheumatoid arthritis.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health
plan consistent with medical chart history) adequate trial (including dates and doses) of 3 months or more of
therapy with methotrexate AND then leflunomide (generic Arava®) or another disease -modifying
antirheumatic drug (DMARD) option (i.e. combination therapy consisting of methotrexate + sulfasalazine or
hydroxychloroquine) or has a documented medical reason (e.g. intolerance, hypersensitivity) for not utilizing
any of these therapies to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB infection
(i.e. tuberculin skin test) as indicated in package insert.
The medication requested has an FDA approved indication for use in patients with rheumatoid arthritis
and is being recommended and prescribed by a rheumatologist at an FDA -approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data, OR for
new members to the health plan consistent with medical chart history) adequate trial of the preferred
biological agents.
If all of the above conditions are met, the request will be approved for up to a 6 -month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR RHEUMATOID ARTHRITIS:
The member has been receiving the medication and documentation was provided that a rheumatologist has
evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the medication.
For members who require Humira 40 mg SC weekly documentation must be submitted indicating that the
member was compliant (consistent with pharmacy claims) with receiving at least 16 weeks of continuous Humira
therapy every other week prior to the request for weekly dosing of Humira AND the member has a medical
reason (e.g. intolerance, hypersensitivity, contraindication) for not receiving concomitant methotrexate.
The medication is being prescribed for an FDA-approved indication at an FDA-approved dosage.
If all of the above conditions are met, the request will be approved for a 6 -month duration for Remicade requests and
for a 12 month duration for requests for all other medications; if all of the above criteria are not met, the request is
referred to a Medical Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/Clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date: 11/2016
157
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for Ankylosing Spondylitis
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
CIMZIA® (certolizumab)
SIMPONI® (golimumab)
REMICADE® (infliximab)
COSENTYX (secukinumab)
Or any newly marketed agent
PA CRITERIA FOR ANKYLOSING SPONDYLITIS
The patient is an adult (≥18 y/o) and has documented ankylosing spondylitis.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial of or has a documented medical reason for not taking at
least two nonsteroidal anti-inflammatory drugs (NSAIDS) to manage their medical condition.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial of or has a documented medical reason for not taking a
cyclo-oxygenase (COX)-2-selective inhibitors to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB infection (i.e.
tuberculin skin test) as indicated in package insert.
The medication requested has an FDA approved indication for use in patients with ankylosing spondylitis and is
being recommended and prescribed by a rheumatologist at an FDA approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial of the preferred biological
agents.
If all of the above conditions are met, the request will be approved for up to a 6-month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR ANKYLOSING SPONDYLITIS:
The medication is being recommended and prescribed by a rheumatologist at an FDA-approved dosage.
The member has been receiving the medication and documentation was provided that the prescriber has
evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the medication.
If all of the above conditions are met, the request will be approved for a 6-month duration for Remicade requests and
for a 12 month duration for requests for all other medications. If all of the above criteria are not met, the request is
referred to a Medical Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date: 11/2016
158
PERFORMRx PRIOR AUTHORIZATION CRITERIA for Specialty Biological Agents
for Psoriatic Arthritis (PsA)
PREFERRED STATUS: Preferred Biological Agents- Require Prior Authorization
ENBREL® (etanercept)
HUMIRA® (adalimumab)
INFLECTRA (infliximab-dyyb)
PREFERRED STATUS: Non-Preferred Biological Agents- Require Prior Authorization (Second Line)
CIMZIA® (certolizumab)
SIMPONI® (golimumab
REMICADE® (infliximab)
OTEZLA® (Apremilast)
STELARA® (ustekinumab)
COSENTYX (Secukinumab)
Or any newly marketed agent
PA CRITERIA FOR PSORIATIC ARTHRITIS (PsA):
The patient is an adult (≥18 y/o) and has documented psoriatic arthritis.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial of 2 g/day for 3 months of sulfasalazine or has a
documented medical reason for not taking sulfasalazine (e.g. predominantly axial symptoms, hepatotoxicity, GI
intolerance) to manage their medical condition.
The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial (3 months without any improvement at maximum doses) of
methotrexate or has another documented medical reason for not taking methotrexate (e.g. predominantly axial
symptoms, liver toxicity) to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or latent TB infection (i.e.
tuberculin skin test), as indicated in the package insert.
The medication requested has a FDA approved indication for use in patients with psoriatic arthritis and is being
recommended and prescribed by a rheumatologist or a dermatologist at an FDA-approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) If the request is for a non-preferred agent,
documented (consistent with pharmacy claims data, OR for new members to the health plan consistent with
medical chart history) adequate trial of the preferred biological agents.
If all of the above conditions are met, the request will be approved for up to a 6 -month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR PSORIATIC ARTHRITIS (PsA):
The medication is being recommended and prescribed by a rheumatologist or dermatologist at an FDA-approved
dosage.
The member has been receiving the medication and documentation was provided that the prescriber has
evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from the medication.
If all of the above conditions are met, the request will be approved for a 6-month duration for Remicade requests and
for a 12 month duration for requests for all other medications. If all of the above criteria are not met, the request is
referred to a Medical Director/clinical reviewer for medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Revision/Review Date 11/2016
159
PERFORMRX PRIOR AUTHORIZATION CRITERI A
®
ST ADOL NS (butorphanol) Nasal Spra y:
FO R M UL ARY ST AT US: Non-Form ulary (generic)
P A C RIT ERI A FOR AP PR OV AL:
PAIN:
o Diagnosis of pain.
AND
o Documented trial and f ailur e with therapeutic doses or intolerance to at least three oral
narcotic m edications including: ox ycodone, oxycodone/acetaminophen, hydrom orphone,
hydrocodone/acetaminophen, acetaminophen/codeine, and m orphine sulfate (f irst line
therapies).
If the above conditions are m et, the request will be app roved with up to a 3 m onth duration with
generic m edication (quantity limit of 1 bottle/30 da ys); if the above conditions are not m et, the
request will be referred to a Medical Director f or m edical necessity review.
MIGRAINE HEADACHE:
o Diagnosis of pain f rom migraine headache.
AND
o Documented trial with therapeutic doses of at least one recommended m igraine
preventative therapy (topiramate, propranolol, tim olol, divalproex sodium, am itript yline,
nortriptyline, and verapam il).
AND
o Documented trial and f ailure with therapeutic doses or intolerance to abortive therap y
®
including at least one triptan and Migranal (unless contraindicated).
AND
o Documented trial and f ailur e with therapeutic doses or intolerance to at least three oral
narcotic m edications including: ox ycodone, oxycodone/acetaminophen, hydrom orphone,
hydrocodone/acetaminophen, acetaminophen/codeine, and m orphine sulf ate.
If the above conditions are m et, the request will be app roved with a up to a 3 m onth duration of
generic m edication (quantity limit of 1 bottle/30 da ys); if the above conditions are not m et, the
request will be referred to a Medical Director f or m edical necessity review.
P A C RIT ERI A FOR RENE W AL
o Patient currently under the care of a neurologist or pain managem ent specialist.
AND
o Documentation s ubm itted b y neurologist or pain management specialist supporting reevaluation of patient.
OR
o Medical necessity of continued use of m edication.
If the above conditions are m et, the request will be approved with up to a 6 m onth duration of
generic m edication (quantit y lim it of 1 bottle/30 da ys) ; if the above conditions are not m et, the
request will be referred to a Medical Director f or m edical nec essity review.
W ARNING:
Drug abuse, dependence, and withdrawal: Because of its opioid antagonist properties,
butorphanol is not recommended f or use in patients dependent on narcotics. Such patients
should have an adequate p eriod of withdrawal f rom opioid drugs prior to beginning butorphanol
therap y. Butorphanol tartrate, b y all routes of administration, has been associated with episodes
of abuse. Of the cases received, there were m ore reports of abuse with the nasal spra y
form ulation than with the inj ectable form ulation. Prolonged, continuous use of butorphanol
160
tartrate m ay result in ph ysic al dependence or tolerance. Abrupt cessation of use b y patients with
ph ysical dependence m ay result in s ym ptom s of withdr awal.
REFERENCES:
1. Matchar DB, Young W B, Rosenberg JH, et al. Evidence based guidelines f or the
managem ent and prevention of m igraine headache in the primary care setting. Am erican
Academ y of Neurology. Septem ber 2000
2. Hoffert MJ; Couch JR; Diam ond S; Elk ind AH; Goldstein J; Kohlerman NJ; Saper JR;
Solom on S. Transnasal butorphanol in the treatm ent of acute m igraine. Headache 1995
Feb;35(2):65-9
3. Edm eads JG, Gawel MJ, Vick ers J. Strategies f or diagnosing and m anaging m edicationinduced headache. Can Fa m Physician. 1997; 43:1249-1254.
4. Mathew NT . Transformed m igraine, analgesic rebound, and other chronic dail y headaches.
Neurologic Clinics. 1997; 15 (1)167-186.
5. Silberstein SD. Practice parameter: evidence-based guidelines f or m igraine headache (an
evidence-based revie w): report of the Quality Standards Subcommittee of the Am erican
Academ y of Neurology. Neurology. 2000;55:754–762.
6. Moore KL, Noble SL. Drug treatm ent of m igraine: Part 1. Acute therapy and drug-rebound
headache. Am Fam Physician. 1997; 56 (8): 2039-204 8.
7. Edm eads J. Headaches in older people. Postgrad Med 1997 101(5): 91-100.
8. Fisher MA, Glass S. Butorphanol (Stadol): A study in problem s of current drug inform ation
and control JNeurolog y. 1997:48:1156-1160.
9. Stadol Drug Inform ation. Microm edex 2015
10. Facts and Comparisons, St. Louis, 2014 eFacts CliniSphere Version ISBN 1-57439-036-8
11. Butorphanol Tartrate Nasal Spra y Prescribing Information. Roxane Laboratories, Inc. Revised
Septem ber 2014.
12. Hildreth CJ, L ynm C, Glass RM. Migraine Headache. JAMA 2009;301(24):2608.
Revision/Review Date: 4/2 015
Associated Polic y: Prior Authorization of Prescription Drugs 236.200
NOT E: Physi cian review er must ov erride criteria w hen, in his/her professional judgment,
the re quest ed item is m e d ically necessar y.
161
PERFORM RX PRIOR AUTHORIZATION SYNAGIS CRITERIA
SYNAGIS (palivizumab): 50mg vial, 100mg vial
All requests require documentation of the following
Child’s gestational age at birth, chronological age, and current weight
Pertinent medical risk factors
Approval requires that Synagis is ordered for the FDA approved indication of Respiratory
Syncytial Virus (RSV) infection prophylaxis in high risk patients and that it is requested at the
FDA approved dose of 15mg/kg/dose every 30 days.
PLEASE NOTE: Synagis prophylaxis is NOT recommended for otherwise healthy infants born after
29 weeks, 0 days gestation, OR for patients greater than 24 months old.
If an infant or child who is receiving Synagis immunoprophylaxis experiences a breakthrough
RSV infection, monthly prophylaxis should be discontinued.
Synagis requests are approvable if the patient meets one of the following:
If child has a chronological age of < 12 months old:
1. The child was born prematurely with a gestational age of 28 weeks & 6 days or less, and the
child’s current chronological age is less than or equal to 1 year at the beginning of RSV season
(November 1st).
2. The child was born with a Gestational Age (GA) of <32 weeks, 0 days and required > 21%
oxygen for at least 28 days after birth, AND has confirmed diagnosis of chronic lung disease of
prematurity (CLD) a.k.a. bronchopulmonary dysplasia (BPD), (Dx Code 770.7).
3. The child was born with significant heart disease requiring medication to control CHF,
moderate to severe pulmonary hypertension, or cyanotic heart disease (see Table 1 & 2)
that could be complicated by pulmonary disease.
4. The child will be profoundly immunocompromised during the RSV season (see Table 3).
5. The child has a congenital abnormality of the airway or a neuromuscular disease that compromise
handling of respiratory secretions during the first year of life.
If child has a chronological age of 12 to 24 months old:
1. The child was born with a Gestational Age (GA) of <32 weeks, 0 days and required > 21 %
oxygen for at least 28 days after birth, AND has confirmed diagnosis of chronic lung disease of
prematurity (CLD) a.k.a. bronchopulmonary dysplasia (BPD), (Dx Code 770.7), AND continues
to require medical treatment with either supplemental oxygen, chronic corticosteroids,
bronchodilator or diuretic treatment within 6 months of the start of or during the current RSV
season.
2. The child will be profoundly immunocompromised during the RSV season (see Table 3).
3. The child will be undergoing cardiac transplantation during the RSV season.
162
4. If the patient meets criteria, the request will be approved with a quantity sufficient to
provide coverage from November 1st through March 31st (a maximum quantity of 5 doses).
If all of the above criteria are not met then, based on professional judgment, the Clinical
reviewer will issue a denial for the medication requested.
FDA INDICATIONS:
Synagis is indicated for the prevention of serious lower respiratory tract disease caused by respiratory
syncytial virus
(RSV) in pediatric patients at high risk of RSV disease.
DOSAGE AND ADMINISTRATION:
The recommended dose of Synagis is 15 mg/kg of body weight, and patients should receive monthly doses
throughout the RSV season. The first dose should be administered prior to commencement of the
RSV season if possible.
**MAXIMUM APPROVABLE DOSES**
ALL PATIENTS will receive Synagis treatment for a maximum of 5 doses per RSV season. There are
novalid clinical reasons for a 6th dose of Synagis and, therefore, all requests for a 6th dose will be denied.
Table 1.
EXAMPLES OF SIGNIFICANT AND APPROVABLE CARDIAC CONDITIONS
Examples of significant hemodynamic cyanotic congenital heart disease:
Tetralogy of Fallot, Transposition of the great vessels, Ebstein’s anomally, Tricuspid atresia, Total
anomalous pulmonary venous return, Truncus arteriosus, Hypoplastic left heart syndrome
Table 2.
NON-APPROVABLE CARDIAC CONDITIONS
Insignificant hemodynamic heart disease (and
therefore are NOT approvable indications):
Indications in which patients are NOT at an
increased risk for RSV (and therefore are
NOT approvable indications)
Secundum atrial septal defect, small ventricular
septal defect, pulmonic stenosis, uncomplicated
aortic stenosis, mild coarctation of the aorta, patent
ductus arteriosus
• Lesions adequately corrected by surgery (unless
the patient continues to require medications for
CHF)
• Mild cardiomyopathy who are NOT receiving
medical therapy
Table 3.
EXAMPLES OF SEVERE IMMUNODEFICIENCIES/IMMUNOSUPPRESSION:
HIV positive, Transplant, Chemotherapy, Severe Combined
Immunodeficiency (SCID)
163
REFERENCES:
1. Respiratory Syncytial Virus, Pickering et al., Red Book Rep Comm Inf Dis, 1 (1), p. 609
2. American Academy of Pediatrics: Committee on Infectious Diseases and Committee on Fetus and
Newborn, Prevention of respiratory syncytial virus infections: Indications for the use of
Palivizumab and update on the use of RSV-IGIV. PEDIATRICS November 1998; Vol.102 No.
5:1211-1215.
3. American Academy of Pediatrics. [chapter title]. In: Pickering LK, Baker CJ, Long SS, McMillan
JA, eds. Red Book: 2009 Report of the Committee on Infectious Diseases American Academy of
Pediatrics; 2009: 562-568.
4. Facts and Comparisons, St. Louis, 2014 eFacts CliniSphere Version ISBN 1-57439-036-8.
5. NREVSS: RSV Surveillance: Trends in the U.S. April 14, 2008. Available at :
http://www.cdc.gov/surveillance/nrevss/index.htm. Accessed August 2014.
6. Update: Respiratory Syncytial Virus Activity—United States, 1995-96 Season. December 8, 1995:
44(48); 900-902. Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/00039753.htm.
Accessed August 2014.
7. RSV Surveillance 2005-2006: A Nationwide Hospital and Office-Based RSV Epidemiology Pilot
8. Study. Pan American Society for clinical Virology. March 2007: 34; 1-9.
9. Synagis® Package Insert, MedImmune, Inc/Ross, Gaithersburg, MD. March 2014.
American Academy of Pediatrics: Committee on Infectious Diseases and Broncholitis
10. Guidelines Committee, Updated Guidance for Palivizumab Prophylaxis Among Infants and
11. Young Children at Increased Rick of Hospitalization for Respiratory Syncytial Virus
12. Infection PEDIATRICS July 28, 2014 DOI: 10.1542/peds.201413. 1665. http://pediatrics.aappublications.org/content/early/2014/07/23/peds.2014-1665
Revision/Review Date: 11/2016
NOTE: Medical Director/Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary
164
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
THIAZOLIDINEDIONES (TZDs)
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization
ACTOS (pioglitazone)
ACTOPLUS MET (metformin/pioglitazone)
ACTOPLUS MET XR (metformin/pioglitazone)
AVANDAMET (metformin/rosiglitazone)
AVANDARYL (glimepiride/rosiglitazone)
AVANDIA (rosiglitazone)
DUETACT (glimepiride/pioglitazone)
OSENI (alogliptin/pioglitazone)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred to
a clinical reviewer for medical necessity review.
Initial Authorization
1. Diagnosis of Type 2 diabetes mellitus
AND
2. Documented trial and failure with therapeutic doses or
intolerance to metformin (first-line therapy)
AND
3. Documented trial and failure with therapeutic doses or
intolerance to Januvia, Janumet, or Onglyza (second-line
therapy). If member has a history of Januvia, Janumet, or
Onglyza or is currently taking an insulin product or currently
taking Byetta, Symlin, or Victoza, this step is not required.
4. NOTE: Only prescribers enrolled in the AVANDIARosiglitazone Medicines Access Program can prescribe
rosiglitazone containing products.
Revision/Review
Medical Director/clinical reviewer must override criteria when, in
165
Date 10/2016
his/her professional judgement, the requested item is medically
necessary.
166
167
ESRD.
BLACK BOX W ARNING :
•
ACTOS® (pioglitazone), ACTOPLUS MET® ACTOPLUS MET XR®
(metformin/pioglitazone), DUETACT® (glimepiride/pioglitazone),
™
OSENI (alogliptin/pioglitazone): Thiazolidinediones, including pioglitazone, may cause or
exacerbate heart failure; closely monitor for signs and symptoms of heart failure (eg, rapid weight
gain, dyspnea, edema), particularly after initiation or dose increases. Not recommended for use
in any patient with symptomatic heart failure. In the U.S., initiation of therapy is contraindicated in
patients with NYHA class III or IV heart failure; if used in patients with NYHA class II (systolic)
heart failure, initiate at lowest dosage and monitor closely. In Canada, use is contraindicated in
patients with any stage of heart failure (NYHA I, II, III, IV). Use with caution in patients with
edema; may increase plasma volume and/or cause fluid retention. Dose reduction or
discontinuation is recommended if heart failure suspected
®
®
®
•
ACTOPLUS MET ACTOPLUS MET XR (metformin/pioglitazone), AVAND AMET
(metformin/rosiglitazone): Lactic acidosis is a rare, but serious complication that can occur due
to metformin accumulation. The risk increases with conditions such as sepsis, dehydration,
excess alcohol intake, hepatic insufficiency, renal impairment, and acute congestive heart failure.
The onset is often subtle, accompanied only by nonspecific symptoms such as malaise,
myalgias, respiratory distress, increasing somnolence, and nonspecific abdominal distress.
Laboratory abnormalities include low pH, increased anion gap and elevated blood lactate. If
acidosis is suspected, ACTOPLUS MET or ACTOPLUS MET XR should be discontinued and the
patient hospitalized immediately.
®
®
•
AV ANDI A (rosiglitazone), AVAND AMET (metformin/rosiglitazone): Thiazolidinediones,
including rosiglitazone, may cause or exacerbate congestive heart failure; closely monitor for
signs and symptoms of congestive heart failure (eg, rapid weight gain, dyspnea, edema),
particularly after initiation or dose increases. Not recommended for use in any patient with
symptomatic heart failure. In the U.S., initiation of therapy is contraindicated in patients with
NYHA class III or IV heart failure; in Canada, use is contraindicated in patients with any stage of
heart failure (NYHA I, II, III, IV). Use with caution in patients with edema; may increase plasma
volume and/or cause fluid retention. A higher frequency of cardiovascular events has been noted
in patients with NYHA class I or II heart failure treated with rosiglitazone. Use may also be
associated with an increased risk of angina and MI. Use with caution in patients at risk for
cardiovascular events and monitor closely. Discontinue if any deterioration in cardiac status
occurs.
Rosiglitazone (Avandia®): M odification of the Risk Evaluation and Mitigation
Strateg y (REMS) - Ma y 2011
Because of the potential increased risk of myocardial infarction, AVANDIA is
available only through a restricted distribution program called the AVANDIARosiglitazone Medicines Access Program]. Both prescribers and patients must
enroll in the program to be able to prescribe or receive AVANDIA, respectively.
AVANDIA will be available only from specially certified pharmacies
participating in the program. As part of the program, prescribers will be
educated about the potential increased risk of myocardial infarction and the
need to limit the use of AVANDIA to eligible patients. Prescribers will need to
discuss with patients the risks and benefits of taking AVANDIA. To enroll, call
1-800-AVANDIA or visit www. AVANDIA.com.
REFERENCES
1. Actos. Prescribing Information. Takeda Pharmaceuticals America, Inc. Nov 2013
2. Actoplus Met. Prescribing Information. Takeda Pharmaceuticals America, Inc. September 2012
3. Actoplus Met XR. Prescribing Information. Takeda Pharmaceuticals America, Inc. Nov 2013
4. Avandamet. Prescribing Information. GlaxoSmithKline. Sep 2013
5. Avandaryl. Prescribing Information. GlaxoSmithKline. Sep 2013
6. Avandia. Prescribing Information. GlaxoSmithKline Sep 2013
7. Duetact. Prescribing Information. Takeda Pharmaceuticals America, Inc. Nov 2013
8. Facts and Comparisons, St. Louis, 2015 eFacts Clini Sphere Version ISBN 1-57439-036-8.
9. American Association of Clinical Endocrinologists/American College of Endocrinology Consensus Panel
on Type 2 Diabetes Mellitus: An Algorithm for Glycemic Control. Endocrine Practice 2009;1 5(6):540-59.
168
2010;33(suppl 1):S11-S61.
11. Lexicomp online. Updated Sept 2015
12. Oseni. Prescribing Information. Takeda Pharmaceuticals. June 2013
Revision/Revie w Date: 11/201 5
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the
requested item is medicall y necessar y.
169
Field Na me
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Infor mation
Age Restrictio ns
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Transder m-Scop ®
®
Transder m-Scop (scopolamine)
Medically accepted indications are defined using the follo wi ng sources: the
Food and Drug Ad ministration (FDA), Micro medex, Ameri can Hospital
For mular y Service (AHFS), U nited States Phar macopeia Drug Infor mation
for the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved for the treat ment of
motion sickness for a one (1) month duratio n and for the treatment of
sialorrhea for a 12 month duration; if the criteria are not met, the request will
be referred to a clinical revie wer for medical necessity review.
Initial Authorization:
Mo tion Sickness
• Diagnosis of nausea and vomiting associated with
motion sickness or recovery from anesthesia.
AND
• Documented trial and failure at therapeutic doses,
intolerance or contraindication to meclizine,
diphenhydramine and dimenhydrinate.
Sialorrhea
• Docu mented trial and failure at therapeutic doses, intoler ance or
contraindication to glycop yrro late.
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
170
PERFORMRX NATIONAL PA CRITERIA
RETIN-A (tretinoin) Cream: 0.025%, 0.05%, 0.1%; Gel: 0.01%, 0.025%, 0.04 %, 0.1 %
FORMULARY STATUS: Formulary (generic)
®
PA CRITERIA FOR APPROVAL:
Diagnosis of acne vulgaris in patients 21 years of age or older (patients less than 21 years, an
automatic approval at the point of service for generic medication will process).
If the above conditions are met, the request will be approved with a up to a 6 month duration with generic
tretinoin; if the above conditions are not met, the request will be referred to a Medical Director for medical
necessity review.
FDA INDICATIONS:
Acne: Topical treatment of acne vulgaris.
DOSAGE AND ADMINISTRATION:
Acne treatment: Apply once a day before bedtime or in the evening. Cover the entire affected area
lightly. Therapeutic results should be seen after 2 to 3 weeks, but may not be optimal until after 6
weeks. Once lesions have responded satisfactorily, it may be possible to maintain the improvement
with less frequent applications or other dosage forms.
Children >12 years and Adults: Begin therapy with a weaker formulation of tretinoin (0.025% cream
or 0.01% gel) and increase the concentration as tolerated; apply once daily before retiring or on
alternate days; if stinging or irritation develop, decrease frequency of application.
REFERENCES:
1.
2.
3.
4.
5.
6.
7.
8.
Webster GF. Topical tretinoin in acne therapy. J Am Acad Dermatol 1998 Aug;39(2 Pt 3):S38-44.
Guidelines of Care for Acne Vulgaris. American Acaemy of Dermatology Association. J Am Acad
Dermatol. 1990. 22:676-80.
Drake, LA et al. Guidelines of care for nevi (nevocellular nevi and sehorrheic keratoses). JAm Acad Derm:
April 1992; 26(4): 629-631.
Verschoore M. et al. Topical Retinoids. Their Uses in Dermatology. Derm Ther. Jan 1993; 99(I):107-115.
Facts and Comparisons, St. Louis, 2015 eFacts CliniSphere Version ISBN 1-57439-036-8.
Retin-A® Prescribing Information. Ortho Dermatological. May 2006.
Winston MH, Shalita AR, “Acne Vulgaris, Pathogenesis and Treatment,” Pediatr Clin North Am, 1991,
38(4):889-903.
Lexicomp online. Accessed September 10, 2015.
Revision/Review Date: 10/2016
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Physician reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
171
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
TYSABRI
Field Description
®
Tysabri®
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
Member does not have a history of progressive multifocal
leukoencephalopathy (PML) or have a compromised immune system.
Documentation consistent with pharmacy claims data was submitted
indicating the patient is not currently using any antineoplastic,
immunosuppressant, or immunomodulating medications
See “Other Criteria”
Patients must be 18 years age or older
See “Other Criteria”
If all of the criteria are met, the initial request for Crohn’s Disease will
be approved for 3 months of treatment. For all other requests and for
continuation of therapy the request will be approved for 6 months of
treatment If all of the above criteria are not met, the request is referred
to a Clinical Reviewer for medical necessity review.
Documentation on request form indicates that the medication is
prescribed is authorized by the TOUCH™ program to prescribe
Tysabri® and that the patient is enrolled in the TOUCH™ program and
has agreed to comply with the requirements for receiving Tysabri®
AND
Tysabri® is being prescribed at an FDA approved dosage.
PA CRITERIA FOR INITIAL AUTHORIZATION FOR USE IN
MULTIPLE SCLEROSIS (MS):
The member has a clinical diagnosis of a relapsing form of multiple
sclerosis.
Clinical or diagnostic information was submitted that indicates that
that patient has a documented (consistent with pharmacy claims data
OR for new members to the health plan consistent with medical
chart history) treatment failure after receiving an adequate trial
(including dates, doses of 6 months or more of each therapy) of,
glatiramer acetate (Copaxone® 40 mg) AND teriflunomide
(Aubagio®), or has a some other documented medical reason
(intolerance, hypersensitivity, etc.) for not utilizing these therapies
172
for a minimum of 6 months each to manage their medical condition.
Tysabri® is being prescribed by a neurologist
PA CRITERIA FOR INITIAL AUTHORIZATION FOR USE
IN CROHN’S DISEASE:
The member has a documented clinical diagnosis of moderate to
severely active Crohn’s Disease
The patient has a documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with
medical chart history) adequate trial (including dates and doses) at
therapeutic doses or has some documented clinically significant
medical reason for not receiving oral conventional therapy to
manage their medical condition.
The patient has a documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with
medical chart history) adequate trial (including dates and doses)
with therapeutic doses of or has some documented clinically
significant medical reason for not receiving Humira®
(adalimumab).
Tysabri® is being prescribed by a gastroenterologist
PA CRITERIA FOR INITIAL AUTHORIZATION FOR USE IN
OTHER MEDICALLY ACCEPTED INDICATIONS
The medication is recommended and prescribed by a specialist in
the field to treat the member’s respective medical condition.
The medication is prescribed at a medically accepted dose per
the medical compendia as defined in the covered uses above .
PA CRITERIA FOR RE-AUTHORIZATION
The medication is recommended or prescribed by a specialist for
the respective treated disease state.
Diagnostic or clinical documentation was submitted (e.g.
improved disease activity index, quality of life, blood work,
radiographic evidence) that indicates the member has
significantly clinically benefited from receiving Tysabri®
therapy.
Revision/Review
Date 11/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
173
PERFORMRX PRIOR AUTHORIZATION CRITERI A
URINARY ANTISPASMODIC AGENTS
FORMULARY ST ATUS Formulary, Pays at Point-of-Sale (First Line)
®
DETROL (tolterodine) (generic) Tablets
®
DITROPAN (ox ybut ynin) (generic) Tablet & Syrup
®
DETROL LA (tolterodine) Capsules
®
SANCTUR A (trospium) (generic) Tablet
®
DITROPAN XL (ox ybut ynin) (generic) Tablets:
FORMULARY ST ATUS Formulary, Requires Step Therapy (Second Line)
®
TOVIAZ (fesoterodine) Tablets
NOTE: Patient must meet #1 criterion to meet step therap y.
FORMULARY ST ATUS Non-Formulary, Requires Prior Authorization (Third Line)
ENABLEX® (darifenacin) Tab lets
®
SANCTUR A XR (trospium) Capsule
®
GELNIQUE (ox ybut yn in) Gel:
®
OXYTROL (ox ybut ynin) Pat ch
®
URISPAS (fla voxate) Tablet
®
VESICARE (solifenacin) Tablets
NOTE: Patient must meet #1 and #2 criteria for approval of PA request.
PA CRITERI A FOR APPROV AL :
1. Documented trial and failure or intolerance to a first line generic product for at least 4 weeks (28 days) of therapy
within the past 3 months.
2. Documented trial and failure or intolerance to a first and a second line therapy for at least 4 weeks (28 days) of
therapy in the past 6 months each.
If the specified conditions are met, the request will be appro ved with up to a 12-month duration; if the above
conditions are not met, the request will be referred to a Medical Director for medical necessity review.
REFERENCES:
1. Detrol®. Prescribing Information. Pfizer. Revised August 2012.
2. Detrol® LA. Prescribing Information. Pfizer. Revised August 2012.
3. Ditropan®. Prescribing Information. Janssen Pharmaceuticals, Inc. Revised July 2013.
4. Ditropan® XL. Prescribing Information. Janssen Pharmaceuticals, Inc. Revised July 2013.
®
5. Oxytrol Patch. Prescribing Information. W atson Pharmaceutical. Revised October 2012.
6. Gelnique™. Prescribing Information. W atson Pharmaceutical. Revised January 2013.
7. Enable x®. Prescribing Information. W arner Chilcott (US), LLC. Revised October 2013.
8. Sanctura®. Prescribing Information. Allergan Pharmaceutical. Revised July 2012.
9. Sanctura XR™. Prescribing Information. Allergan Pharmaceutical. Revised August 2012.
®
10. Vesicare . Prescribing Information. Astellas Pharma US, Inc. Revised October 2013.
Revision/Revie w Date: 4/2015
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the requested item is
medicall ynecessa r y.
174
Field Na me
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Infor mation
Age Restrictio ns
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Vancocin
®
Vancocin® (vanco mycin) capsule
Medically accepted indications are defined using the follo wi ng sources: the
Food and Drug Ad ministration (FDA), Micro medex, Ameri can Hospital For
mular y Service (AHFS), United States Phar macopeia Drug Infor mation for
the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved for a 10 – 14 day
duration; if the criteria are not met, the request will be referred to a clinical
reviewer for medical necessity review.
Initial Authorization:
Staph ylo cocca l Enterocolitis:
• Diagnosis of enterocolitis caused by Staphylococcus aureus.
Pseudomembranous Colitis:
• Diagnosis of antibiotic associated pseudo me mbranous colitis
produced by C. difficile.
AND
For mild-to - mod erate infectio n:
• Docu mented trial and failure with therap eutic doses or intolerance to
metronidazole if mild-to-mod erate C. difficile infection (CDI).
For severe infectio n:
• With severe infection, vanco mycin is the drug of choice for initial
treatment.
For severe, co mp licated infection:
• Vanco mycin ad ministered orally with or without I.V. metronidazole is
the initial regi men of choice for treat ment of severe, co mplicated CDI.
Considerations for auto matic a pproval:
• Me mber is age 65 or greater
• Me mber has renal d ysfunction
• Recently discharged fro m hospital on PO vanco mycin
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
175
Field Na me
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Infor mation
Age Restrictio ns
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Dat e
07/2016
Field Description
Vfend
®
Vfend®(vorizonazole) tablets and oral suspension
Medically accepted indicatio ns are defined using the follo wi ng sources: the
Food and Drug Ad ministration (FD A), Micro medex, American Hospital
For mular y Service (AHFS), United States Phar macopeia Drug Infor mation
for the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
See “other criteria”
FD A reco mmends use in patie nts 12 years of age and older.
N/A
If the above conditions are met, the request will be approved with up to a 3
month duratio n depending upon the severity o f the infection; if the above
conditions are not met, the req uest will be referred to a clinical revie wer for
medical necessity revie w.
.
Initial Authorization:
• Diagnosis of invasive aspergillosis or a serious fungal
infection caused b y Scedosporium apiospermum and
Fusarium species.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
176
PERF OR M RX N AT I ON AL PRIOR AUT HORIZ AT ION CRIT ERI A
®
VICOPR OFEN (hydrocod one/ibuprofen) T ablet: 7.5/200m g
FORM UL ARY ST AT US: Non-Formulary (generic)
PA CRIT ERI A FOR APPR OV AL:
• Diagnosis of acute pain.
AND
• Documented trial and failur e or intolerance to at least three of the following m edications:
oxycodone/acetaminophen, hydrocodone/acetaminophen, acetaminophen/codeine, m orphine, and
h ydrom orphone.
If the above conditions are m et, the request will be app roved up to 3 m onth duration; if the above
conditions are not m et, the request will be referred to a Medical Director f or m edical necessity revie w.
FD A INDIC AT IONS:
®
Vicoprof en tablets are indicated f or the short term (generally less than 10 da ys) managem ent of acute
®
pain. Vicoprofen is not indicated f or the treatm ent of such conditions as osteoarthritis or rheum atoid
arthritis.
DOS AG E AND ADM INISTRAT ION
For the short term (generally less than 10 da ys) m anagement of acute pain.
Adult and adolescents (≥ 16 years) the recomm ended dose is one tablet every 4-6 hours, as necessar y.
Dosage should not exceed 5 tablets in a 24 hour perio d.
REFERENCE:
1. Palangio M, Morris E, Do yle RT , et al.Combination hydrocodone and ibuprofen versus com bination
oxycodone and acetaminophen in the treatm ent of m oderate or severe acute low b ack pain. Clin T her
(United States), Jan 2002, 24(1) p87-99.
2. Bark in RL.Acetaminophen, aspirin, or Ibuprof en in c om bination analgesic products.Am J T her
(United States), Nov-Dec 2001, 8(6) p433-42.
3. Facts and Com parisons, St. Louis, 2014 eFacts CliniSphere Version ISBN 1-57439-036-8.
®
4. Vicoprofen Prescribing Information. Abbott Laboratories. October 2009.
Revision/Review Date: 03/2014
Associated Polic y: Prior Authorization of Medications 236.200
NOTE: Physician review er must overrid e criteria w hen, in his/her profession al judgment, the
requested item is medical ly necessar y.
177
PerformRx Prior Authorization Criteria for Xolair
Xolair® (omalizu mab): 150 mg lyophilized po wder for injection
For mulary Status: Non For mular y
PA CRITERIA FOR INITIA L APPROVAL FOR ASTH M A:
• T he physician who has requested Xolair is pulmonologist or allergist or docu mentation (consultation) was
sub mitted with the request indicating that Xolair was recommended by a pulmo nologist or allergist.
• T he patient’s age is > 6 years old and the patient has a > 1 year history of moder ate-to-sever e asthma.
• T he patient’s total serum IgE ≥ 30 IU/ml to ≤ 700 IU/ml and the prescribed dose is within approved FDA dosing
guidelines.
• T he patient has a documented baseline FEV1 < 80% o f predicted or FEV1 /FVC that has been reduced b y at least
5% of nor mal for the patient age range (see T able 1 belo w).
• T he patient has a documented history o f one or more of the following: requires daily use of inhaled short acting B 2
agonists, history of daily or continual asthma sympto ms, limited physical activity or activity affected b y
exacerbations due to asthma, and frequent (> once per week) nighttime sympto ms.
• Documentation that the patient is still having significant symptoms (i.e. hospital admission, emergency room visits,
and/or the severe of asthma exacerbations) while co mpliant on a high-dose inhaled corticosteroid with a longacting B 2 agonists + a leukotriene receptor antagonist or theophylline. If the patient utilizing these therapies then
the patient must have a documented medical reaso n for not maxi mizing both high dose inhaled corticosteroids
with long acting bronco dilator medication (e.g. side effects, intolerance, and hypersensitivity).
• T he patient has a positive documented immediate response on RAST test and/or skin prick test to at least 1 co mmo n
allergen (e.g. der matophagoides farinae, der matop hagoides pteronyssinus, dog, cat, or ockro ach) and there is
documented evidence that the positive skin tested allergen(s) is an asthma trigger either from environmental exposure
or from testing or from attempted allergen immunotherap y.
• Docu mentation was sub mitted that the patient has received immunotherapy and despite this the patient had
documented clinical asthma recurrence/persistence precipitated b y the allergen(s) for which the patient is receiving
immunotherapy that had resulted in a hospital ad mission or emergency room visit. OR if the patient has not received
allergy shots they have a documented medical reason for not taking allergy shots (e.g. severe, unstable
asthma or severe, systemic injection reactions).
• Docu mentation was sub mitted indicating what environmental measures were atte mpted to avoid and/or mini mize
exposure to identified allergen asthma triggers OR a reason (e.g. unavoidable allergen) for not trying to avoid
asthma allergen trigger(s).
• T he patient is not receiving any medication (e.g. Beta Blockers or NSAIDs) that could cause bronchospas m or
cause an asthma exacerbation and if the patient is on a potential asthma inducing medication, that there is a
documented medical reason for continuing that medication as well as documentation that the medication is not a
cause for worsening asthma or causing any asthma sympto ms.
If all of the abo ve conditions ar e met, the request will be approved with a 4 -month duration; if all of the above criteria are
not met, the request is referred to a Medical Director/Clinical Reviewer for medical necessity revie w.
PA CRITERIA FOR INITIA L APPROVAL FOR CHRONIC IDIOPATHIC URTICA RIA:
• T he physician who has requested Xolair is an allergist, immunologist or dermatologist or documentation
(consultation) was sub mitted indicating that Xolair was reco mmended b y a specialist that treats urticaria.
• T he patient’s age is > 12 years old
• T he patient has a documented history of urticaria for at least 3 mo nths.
• T he patient requires oral steroids to control sympto ms.
• T he patient remains sympto matic despite adequate trials o f TWO formulary H1 antihistamines (1st generation-e.g.
hydroxyzine, cyproheptadine and 2nd generation –loratidine, cetirizine), a formulary H2 antihistamine (e.g.
famotidine, ranitidine)and Montelukast.
• T he prescribed dose is within a pproved FDA dosing guidelines.
If all of the abo ve conditions ar e met, the request will be approved with a 4 -month duration; if all of the above criteria are
not met, the request is referred to a Medical Director/Clinical Reviewer for medical necessity revie w.
PA CRITERIA FOR REA U THORIZA TI ON AFTER 4 MONTHS OF THERAPY F OR ASTHM A:
• Documentation sub mitted indicates that the member has significantly clinically benefited fro m the medication (e.g.
patient has marked improvement in pulmonary function tests such as FEV1 or peak expiratory flo w rate, decrease in
asthma exacerbations and/or a decrease in inhaled or oral corticosteroid use since receiving Xolair therap y).
• T he prescribed dose is within a pproved FDA dosing guidelines.
If all of the abo ve conditions are met, the request will be approved with a 6 -month duration; if all of the above criteria are
178
not met, the request is referred to a Medical Director/Clinical Reviewer for medical necessity revie w.
PA CRITERIA FOR REA U THORIZA TI ON AFTER 4 MONTHS OF THERAPY FOR CHRONIC URTICARIA:
• Documentation submitted indicates that the me mber has significantly clinically benefited fro m the medication.
• T he member has been receiving the medication and documentation was provided that the prescriber has evaluated
the member and recommends continuation of therap y.
• T he prescribed dose is within a pproved FDA dosing guidelines.
If all of the abo ve conditions ar e met, the request will be approved with a 6 -month duration; if all of the above criteria are
not met, the request is referred to a Medical Director/Clinical Reviewer for medical necessity revie w.
Table 1: Nor mal FEV1/FVC
Patients Age :
8 - 19 y/o
20 - 39 y/o
40 - 59 y/o
60 - 80 y/o
Normal Values:
85 %
80 %
75 %
70 %
Review Date: 8/2016
NOTE: Clinical review er must override criteria w hen, in his/her professional j udg ment, the requested ite m is
me dica lly necessary.
179
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Field Description
Xyrem®
Xyrem® (sodium oxybate)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
Medication is being taken along with sedative hypnotics or alcohol.
“See Other Criteria”
Patient must be 18 years of age or older.
MD is a neurologist or sleep specialist, or documentation has been
provided that provider has consulted with a neurologist or sleep
specialist.
Coverage Duration
If all of the conditions are met, the request will be approved for a 3
month duration. If the conditions are not met, the request will be sent
to a Medical Director/clinical reviewer for medical necessity review.
Other Criteria
Initial:
If patient has a history of substance abuse, documentation has
been provided that provider has referred the patient for substance
abuse disorder treatment.
Patient has documented trial and failure on two stimulant
medications (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history),
or a documented medical reason for not utilizing two stimulant
medications.
For patients with cataplexy: Patient also has a documented trial
and failure with a formulary tricyclic AND venlafaxine ER, or has
a documented medical reason (contraindication/intolerance) for
not utilizing a formulary tricyclic AND venlafaxine ER.
Medication is being prescribed at an FDA approved dose.
Continuation:
Documentation has been submitted indicating patient has
clinically benefited from treatment (i.e. improvement on Epworth
Sleepiness Score)
Medication is being prescribed at an FDA approved dose.
180
Revision/Review Date
11/2016
For patients with cataplexy: Documentation has been provided
that there has been a reduction in frequency of cataplexy attacks.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
181
PERF OR M RX PRIOR AUT HORIZ AT I ON CRIT ERI A
ZYVOX (linezolid) Tablet: 600mg; Suspension: 100mg/5mL
STATUS Non-Formulary
PA CRITERI A FOR APPROV AL
•
Diagnosis of vancomycin-resistant enterococcus faecium infection, nosocomial pneumonia, complicated skin and
skin structure infection (including diabetic foot infections, without concomitant osteomyelitis), uncomplicated skin
and skin structure infection, methicillin-resistant Staphylococcus aureus infection, or community-acquired
pneumonia.
And patient meets one of the tw o follow ing criteria:
•
Documented history of treatment with Zyvo x IV (continuation of therapy, IV to PO conversion).
•
Documentation that the infection is susceptible to Zyvox AN D the patient has failed treatment or is
contraindicated to treatment with antibiotics to which the organism is susceptible.
If the above conditions are met, the request will be approved with up to a 1 month duration depending on the type of
infection; if the above conditions are not met, the request will be referred to a Medical Director for medical necessity
review.
FDA INDIC ATIONS
•
Vancom ycin-Resistant Enterococcus Faecium Infections: Including cases with concurrent bacteremia.
•
Nosocomial Pneumonia: Caused by Staphylococcus aureus (methicillin-susceptible and methicillin-resistant
strains), or Streptococcus pneumoniae (including multi-drug resistant strains [MDRSP]*).
•
Complicated Skin and Skin Structure Infections, Including Diabetic Foot Infections, w ithout Concomitant
Osteom yelitis: Caused by Staphylococcus aureus (methicillin-susceptible and methicillin-resistant strains),
Streptococcus pyogenes, or Streptococcus agalactiae. Zyvox has not been studied in the treatment of decubitus
ulcers.
•
Uncomplicated Skin and Skin Structure Infections: Caused by Staphylococcus aureus (methicillinsusceptible only) or Streptococcus pyogenes.
•
Communit y- Acquired Pneumonia: Caused b y Streptococcus pneumoniae (including multi-drug resistant
strains [MDRSP]*), including cases with concurrent bacteremia, or Staphylococcus aureus (methicillinsusceptible strains only).
* MDRSP refers to isolates resistant to two or more of the following antibiotics: penicillin, second-generation
cephalosporins, macrolides, tetracycline, and trimethoprim/sulfamethoxazole.
NOTE: Zyvo x is not indicated for the treatment of Gram-negative infections. It is critical that specific Gram-negative
therapy be initiated immediately if a concomitant Gram-negative pathogen is documented or suspected.
NOTE: To reduce the development of drug-resistant bacteria and maintain the effectiveness of Zyvox and other
antibacterial drugs, Zyvox should be used only to treat or prevent infections that are proven or strongly suspected to
be caused by susceptible bacteria. W hen culture and susceptibility information are available, they should be
considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and
susceptibility patterns may contribute to the empiric selection of therapy.
DOSAGE AND ADMINISTRATION
Infection
Complicated skin and
skin structure infections
Community-acquired
pneumonia, including
concurrent bacteremia
Nosocomial pneumonia
Vancomycin-resistant
Enterococcus faecium
infections, including
concurrent bacteremia
Uncomplicated skin and
skin structure infections
Dosage and Route of Administration
Recommended
Duration of
Treatment
(Consecutive
Da ys)
Pediatric Patients (Birth through
11 Years of Age)
Adults and Adolescents (12
Years and Older)
10mg/kg IV or PO every 8 hours
600mg IV or PO every 12 hours
10-14
10mg/kg IV or PO every 8 hours
600mg IV or PO every 12 hours
14-28
<5 years: 10mg/kg PO every 8
hours
5-11 years: 10mg/kg PO every 12
hours
Adults: 400mg PO every 12 hours
Adolescents: 600mg PO every 12
hours
10-14
182
IV to PO Conversion:
Zyvox has appro ximately 100% bioavailability. For patients who are being converted to the oral formulation, refer to
the table below:
IV Dose
Oral Dose*
10mg/kg every 8 hours
10mg/kg every 8 hours
10mg/kg every 12 hours
10mg/kg every 12 hours
400mg every 12 hours
400mg every 12 hours
600mg every 12 hours
600mg every 12 hours
*Oral dosing using either oral suspension or tablets.
REFERENCES
1. Facts and Comparisons, St. Louis, eFacts 2015 CliniSphere Version ISBN 1-57439-036-8.
2. Zyvo x. Prescribing Information. Pfizer, Inc.January 2014. .
3. Stevens, Dennis, et al. Practice Guidelines for the Diagnosis and Management of Skin and Soft-Tissue
Infections. Clinical Infectious Diseases. 2005; 41:1373-406.
4. McAule y D. Zyvo x – Prescribing information. Updated 08/10/2011.
Revision/Revie w Date: 11/2015
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Ph ys ician re view er must override criteria w hen, in his/her professional judgment, the requested item
is medicall ynecessar y.
183
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Field Description
VIVITROL®
Naltrexone Intramuscular Injection
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
Patients receiving opioid analgesics, patients in acute opioid
withdrawal, patients with a positive urine screen, or patients with acute
hepatitis or liver failure.
See “other criteria”
Patient must be 18 years of age or older
See “Other Criteria”
If all of the conditions are met, the request will be approved with 3month duration. If all of the criteria are not met, the request is referred
to a clinical reviewer for medical necessity review.
184
Other Criteria
Initial Authorization:
• Negative pregnanc y test (for women, as indicated) within
30 days of request. If test is positive, request will be
denied and member should be treated with buprenorphine
if applicable.
• Prescriber is, or has consulted with a behavioral health or
licensed Drug and Alcohol (D&A) provider.
• Patient must have diagnosis of opioid dependence,
following opioid detoxification
OR
alcohol dependence and documentation has been provided that
patient is able to abstain from alcohol in an outpatient setting.
• Documentation is provided of an initial evaluation by a
D&A provider to recommend level of care.
• Documentation is provided of a referral to or participation
in a substance abuse or behavioral health treatment
program or behavioral health counseling b y a licensed
D&A provider.
• Documentation has been provided that the patient was
screened for depression and risk of suicide. If these
conditions are present, documentation is provided that the
patient was referred for treatment with a behavioral health
provider.
• Documentation is provided that the patient is free from
opioids (including tramadol) for a minimum of 7-10 days
before starting therap y, or for alcohol dependence the
patient is not actively drinking.
Re - Authorization:
• Documentation submitted includes participation in a substance
185
abuse or behavioral health counseling, treatment program, or
addictions recovery program with a licensed D&A or behavioral
health provider.
• Documentation of monthly urine drug screens that are
negative for opiates (specificall y including ox ycodone and
fentan yl) and also for licit and illicit drugs with the
potential for abuse. ( Lab results are required *unless
provider is a licensed DDAP Drug and Alcohol provider
verified on the state website by
accessing https://apps.ddap.pa.gov/gethelpnow/CareProvider.a
spx.) Once provider is verified as a licensed Drug and
Alcohol provider, provider may choose to supply
documentation
that regular drug screens are being performed and patient
is being monitored accordingly, and this will suffice as
documentation to fulfill this requirement)
• If diagnosis is alcohol dependence, documentation of
monthly blood alcohol (ethyl alcohol) testing is also
required.
• Negative pregnancy test (for women, as indicated) within
30 days of request. If test is positive, request will be
denied and member should be treated with buprenorphine
if applicable.
• If patient has symptoms of depression or is at risk for
suicide, documentation has been provided that the patient
is being treated b y a behavioral health provider.
Revision/Review Date
08/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
186
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Revision/Review
Date 8/2016
Field Description
WHITE BLOOD CELL STIMULATORS
FORMULARY STATUS Specialty Tier (PA required)
• Zarxio™ (Filgrastim-sndz)
• Neupogen® (Filgrastim)
• Neulasta® (Pegfilgrastim)
• Mozobil® (Plerixafor)
• Leukine® (Sargramostim)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
The request will be approved for up to 12 weeks. If all of the above
criteria are not met, the request is referred to a Medical Director/clinical
reviewer for medical necessity review.
• For Leukine® requests ONLY: Documentation is submitted of the
patient’s current diagnosis, current bodyweight, body surface area and
absolute neutrophil count (within 30 days of the request).
• For Neulasta® requests ONLY: If the medication request is being
ordered for a patient requiring dose dense chemotherapy (i.e. for a
documented diagnosis of breast cancer) no prior trials of any other white
blood cell stimulator is needed for that patient.
• For Neupogen® requests that are less than 180mcg, Neupogen® can
be approved. For all other requests for Neupogen® or Neulasta®: the
patient has a documented treatment failure {i.e. failure to reach and/or
maintain target ANC, prolonged febrile neutropenia, unplanned
hospitalization, infection requiring prolonged anti-infectives} which is
consistent with pharmacy claims data, with an adequate trial (including
dates, doses of therapy) of Zarxio™ and/or has another documented
medical reason (intolerance, hypersensitivity, or dose dense
chemotherapy, stem cell collection, etc.) for not using Zarxio™ to treat
their medical condition.
• For Mozobil® requests ONLY: documentation must be submitted that
the patient is using Mozobil® in combination with a granulocyte-colony
stimulating factor (G-CSF) agent (i.e. Zarxio™)
• Patients ANC (absolute neutrophil count) has been submitted with
request and prescribed dosing of medication is within FDA approved
dosing.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
187
Field Name
Prior Authorization
Group Description
Field Description
Oncology without specific criteria to be used with an oncology
diagnosis
Drugs
Oral and Injectable Oncology Medications (specialty or non-specialty)
without medication specific Criteria with an oncology diagnosis
Covered Uses
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI) , and the Drug Package Insert, and/or per the National
Comprehensive Cancer Network (NCCN)
Exclusion Criteria
N/A
Required Medical
Information
Age Restrictions
See “other criteria”
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
8/2016
N/A
Prescriber must be an oncologist
If the criteria are met, the request will be approved for up to 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
All of the following criteria must be met:
• Requested indication must be supported by NCCN Category 1
or 2A level of evidence. If the request is for a Category 2B
recommendation then medical documentation has been
provided as to why member is unable to utilize a treatment
regimen with a higher level of evidence (e.g. allergic reaction,
contraindication).
• Documentation provided of results of genetic testing where
required per drug package insert.
• Documentation provided of results of all required laboratory
values and patient specific information (e.g. weight, ALT/AST,
Creatinine Kinase, etc.) when recommended/required per drug
package insert.
• The medication is being prescribed at a dose that is within
FDA approved/NCCN
guidelines.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
188
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
12/2016
Field Description
Gender Dysphoria Medications if Prior Authorization is required
Formulary anti-androgens, progestins, GnRH agonists, estrogens,
testosterone medications if prior authorization is required
**See table that follows***
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information
for the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
“see other criteria”
Requests for members under the age of 16 must be sent to the Medical
Director for review.
N/A
If all of the conditions are met, requests will be approved for a 12 months.
If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
• The prescriber has submitted information that indicates (in
accordance with World Professional Association for Transgender
Health (WPATH)) Standards of Care that:
the member has had initial assessment by a mental health
professional
the member has the capacity to make a well-informed
decision
if significant medical or mental health issues are present, the
medical or mental issues are well-controlled
• If request is for a non-formulary agent, documentation of a medical
reason (e.g. intolerance, hypersensitivity, contraindication) was
submitted with request why the member is not able to use the
formulary alternatives
• If the member is under 16 years of age, the request must be sent to
the Medical Director for clinical review.
• Dosing is within the recommended range
Physician/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
***Recommended dosing next page
189
Hormone regimens in adult transsexual persons
Estrogen
Oral: estradiol (17β-estradiol valerate)
Transdermal: estradiol patch
2 to 6 mg/day
0.1 to 0.4mg/24 hours, changed once or twice
weekly depending on product
5 to 20mg every two weeks
2 to 10mg every week
Parenteral: estradiol valerate
estradiol cypionate
Antiandrogens
Oral: spironolactone
100 to 400mg/daily
GnRH agonists
Leuprolide
3.75 to 7.5mg IM depot monthly
Testosterone
Parenteral: testosterone enanthate or cypionate
50 to 100mg IM every week
OR
100mg to 200mg IM every two weeks
2.5 to 10 grams of gel per day (equivalent to 25 to
100mg/day testosterone)
2.5 to 7.5mg/day
Transdermal: testosterone gel 1%
•
•
testosterone patch
Dose of estrogen should be adjusted according to serum 17β-estradiol levels (i.e., 100 to 200 pg/mL) and
effect. Lower doses of estradiol are generally sufficient for feminization goals when combined with an antiandrogen, GnRH agonist, or after gonadectomy. Anti-androgen therapy is discontinued after gonadectomy.
Synthetic estrogens, e.g. ethinyl estradiol, are not recommended due to elevated risk of thromboembolic
disease, cardiovascular mortality and inability to regulate dose by measurement of serum levels.
Doses of testosterone should be adjusted according to serum testosterone levels (i.e., normal male range
320 to 1000 ng/dL) and effect. Time to onset of effect of parenteral preparations may be less than with
transdermal preparations.
Data from:
1. Tangpric ha, V. Treatment of transsexualism. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on July 5, 2016)
2. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine
Society clinical practice guideline. J Clin Endocrinol Metab 2009; 94:3132.
3. Gooren LJ. Clinical practice. Care of transsexual persons. N Engl J Med 2011; 364:1251.
4. Spack NP. Management of transgenderism. JAMA 2013; 309:478.
5. Knezevich EL, Viereck LK, Drincic AT. Medical management of adult transsexual persons. Pharmacotherapy 2012; 32:54.
190
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Short Acting Opioid Containing Products
***For New Starts Only***
(Members that have not filled a short acting opioid in the past 60 days)
***If the member has cancer, sickle cell or is on hospice please
automatically authorize for 12 months***
FORMULARY STATUS
1. Formulary short acting opioids >200 Morphine Milligram
Equivalents (MME) per day
2. Non-formulary short acting opioids >200 MME per day
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
Pain Specialist, Oncologist, Hospice physician, Hematologist, Surgeon,
or attestation that the requesting prescriber is working in consultation
with one of the above specialty types.
If the criteria are met, the request will be approved with up to one month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization for Short Acting Products:
1. The diagnosis is acute pain or break through pain
2. The request is for a short acting opioid product
3. The prescriber has explained medical necessity (i.e titration
down to a dose above 200MME)
4. For states with a PDMP, prescriber attests to checking the PDMP
5. Prescriber attests to titration of dose requested ***If using for
breakthrough pain, dose requested is 10-20% of total daily
analgesic dose***
6. Prescriber attests to discussing with the patient the level of risk
for opioid abuse/overdose with the dose/duration prescribed to
the patient
7. Prescriber attests to discussing concomitant psychological
disease and risks associated with opioid overdose/abuse.
8. Prescriber attests to discussing history of substance abuse and
191
Revision/Review
Date 10/2016
the risks associated with opioid overdose/abuse
9. Prescriber has the patient’s signature on file acknowledging
education regarding the risks of opioid therapy as listed in items
6, 7 and 8 above
10. If the request is for a non-formulary short acting opioid, patient
must meet criteria 1-9 AND try and fail 3 formulary alternatives
before approving non-formulary short acting opioid
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
192
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Ocaliva®
Ocaliva® (obeticholic acid)
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information
for the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
Exclusion Criteria
N/A
Required Medical
Information
See “other criteria”
Age Restriction
Field Description
18 and older
Prescriber
Hepatologist or Gastroenterologist
Restrictions
Coverage Duration If the criteria are met, the request will be approved for 5 mg once daily for a
3 month duration for initial authorization and up to 10mg once daily for up
to a 6 month duration for reauthorization; if the criteria are not met, the
request will be referred to a clinical reviewer for medical necessity review.
***If member has moderate or severe hepatic impairment, 5mg once weekly
will be approved for initial and 5mg twice weekly or 10mg twice weekly
will be approved for reauthorization, unless member is having adequate
response at once weekly dose.
193
Other Criteria
Initial Authorization:
1. Diagnosis of primary biliary cholangitis (PBC) with confirmation of
diagnosis by two of the following tests:
a) Positive antimitochondrial antibody test
b) Elevated serum alkaline phosphatase level
c) Liver biopsy
d) Ultrasound scan of the liver
AND
2. Patient is taking Ocaliva in addition to ursodeoxycholic acid (UDCA)
due to inadequate response for at least 1 year
OR
3. Patient is unable to tolerate UDCA and is taking Ocaliva as
monotherapy
AND
4. If patient has moderate or severe hepatic impairment, requested dose
is for 5mg once weekly
AND
5. Submission of the following test results within 30 days of request:
a) AST/ALT
b) Fasting lipid panel (LDL, HDL)
c) Serum alkaline phosphatase
d) Total bilirubin
Reauthorization:
1. Submission of the following test results within 30 days of request:
a) Fasting lipid panel (LDL, HDL)
b) ALT/AST
2. Submission of lab tests confirming a decrease in serum alkaline
phosphatase (ALP) and total bilirubin since beginning therapy
3. If patient has moderate or severe hepatic impairment, requested dose
is for 5mg twice weekly or 10mg twice weekly, unless member is
having adequate response at once weekly dose.
Revision/Review
Date
2/2017
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
194
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Cinqair®
Cinqair® (reslizumab) injection
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
When being used for relief of acute bronchospasm or status asthmaticus, or for the
treatment of other eosinophilic conditions.
See “other criteria”
Member must be 18 years of age or older
Prescriber must be an allergist or pulmonologist
If the above conditions are met, the initial request will be approved with a 3 month
duration. All subsequent requests will be approved with a 6 month duration. If the
criteria are not met, the request will be referred to a clinical reviewer for medical
necessity review.
Initial Authorization:
1. Confirmed diagnosis of eosinophilic asthma
2. Documentation has been provided (within 45 days of request) with
eosinophil count ≥ 400 cells/mcL
3. The patient has a documented baseline FEV1 < 80% of predicted, or
additional documentation has been provided to justify medical necessity
4. Documentation has been provided indicating patient still is having
significant symptoms with ≥ 2 exacerbations in the previous 12 months
requiring additional medical treatment, (oral systemic steroids, emergency
room visits, hospital admissions) while compliant on a high-dose inhaled
corticosteroid with a long-acting B2 agonist ± a leukotriene receptor
antagonist or theophylline. If the patient has not utilized these therapies, a
documented medical reason must be provided why patient is unable to do so.
5. The prescribed dose is within FDA approved dosing guidelines
Re-Authorization:
1. Documentation submitted indicates the member has clinically benefited from
the medication (FEV1, reduced exacerbations, etc.)
2. The prescribed dose is within FDA approved dosing guidelines
Revision/Review Date
2/2017
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
195
Revised April 2014