* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
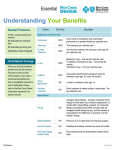
Download First Smile - EarlyCare Plan
Dental implant wikipedia , lookup
Calculus (dental) wikipedia , lookup
Dentistry throughout the world wikipedia , lookup
Dental hygienist wikipedia , lookup
Dental degree wikipedia , lookup
Focal infection theory wikipedia , lookup
Scaling and root planing wikipedia , lookup
Impacted wisdom teeth wikipedia , lookup
Special needs dentistry wikipedia , lookup
Remineralisation of teeth wikipedia , lookup
Periodontal disease wikipedia , lookup
Tooth whitening wikipedia , lookup
Endodontic therapy wikipedia , lookup
Crown (dentistry) wikipedia , lookup
Dental anatomy wikipedia , lookup
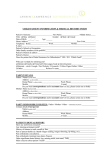
Schedule of Covered Procedures and Copayments First Smile - EarlyCare Plan Services when performed by a Dental Health Services participating dentist Code Description Copayment Deductible...................................................................................................................0 Individual out-of-pocket maximum................................................................... 350 Family out-of-pocket maximum......................................................................... 700 According to assigned Dental Failed (no show) appointment w/o notice.......................................Office Policy All copayments paid by, or on behalf of the enrollee, apply towards the enrollee’s annual out-of-pocket maximum. Dental Check-up For Children D0120 D0140 D0150 D0190 D0191 D0210 D0220 D0230 D0240 D0270 D0272 D0273 D0274 D0330 D0340 D0350 D0460 D0470 D1110 D1120 D1206 D1208 D1330 D1351 D9543 D9630 D9930 Periodic oral evaluation - established patient - once every 6 months.... 10 Limited oral evaluation - problem focused......................................... 10 Comprehensive oral evaluation - new or established patient........... 10 Screening of a patient - limit of 2 per calendar year................................ 10 Assessment of a patient - limit of 2 per calendar year............................ 10 Intraoral - complete series of radiographic images - once in a 3-year period............................................................................................. 10 Intraoral - periapical first radiographic image - once in a two-year period............................................................................................. 10 Intraoral - periapical each additional radiographic image - once in a two-year period...................................................................................... 10 Intraoral - occlusal radiographic image................................................ 10 Bitewing - single radiographic image................................................... 10 Bitewings - two radiographic images.................................................... 10 Bitewings - three radiographic images................................................. 10 Bitewings - four radiographic images - once every 12 months............... 10 Panoramic radiographic image - once in a 3 year period......................... 10 Cephalometric radiographic image - once in a 2 year period................. 10 Oral/facial photographic images obtained intraorally or extraorally......................................................................... 10 Pulp vitality tests - one test per visit.......................................................... 10 Diagnostic casts....................................................................................... 10 Prophylaxis - adult - once every 6 months................................................. 10 Prophylaxis - child - once every 6 months................................................. 10 Topical application of fluoride varnish................................................ 10 Topical application of fluoride - frequency is based on age of enrollee, see limitations............................................................................. 10 Oral hygiene instructions - Available for enrollees 8 and younger. Available once every 6 months, up to 2 times in a 12-month period................................................................................... 10 Sealant - per tooth - See limitations for details about frequency................. 10 Office Visit............................................................................................... 10 Other drugs and/or medicaments, by report..................................... 10 Treatment of complications (post-surgical) - unusual circumstances, by report......................................................................... 10 Code Description D1550 D1555 D2140 D2150 D2160 D2161 D2330 D2331 D2332 D2335 Re-cementation of space maintainer.................................................... 20 Removal of fixed space maintainer...................................................... 20 Amalgam - one surface, primary or permanent................................. 20 Amalgam - two surfaces, primary or permanent................................ 20 Amalgam - three surfaces, primary or permanent............................. 20 Amalgam - four or more surfaces, primary or permanent............... 20 Resin-based composite - one surface, anterior................................... 20 Resin-based composite - two surfaces, anterior.................................. 20 Resin-based composite - three surfaces, anterior............................... 20 Resin-based composite - four or more surfaces or involving incisal angle (anterior)...................................................... 20 Resin-based composite crown, anterior............................................... 20 Resin-based composite - one surface, posterior................................. 20 Resin-based composite - two surfaces, posterior............................... 20 Resin-based composite - three surfaces, posterior............................. 20 Resin-based composite - four or more surfaces, posterior............... 20 Crown - resin-based composite (indirect)........................................... 20 Recement inlay, onlay, or partial coverage restoration....................... 20 Recement cast or prefabricated post and core.................................... 20 Recement crown...................................................................................... 20 Prefabricated porcelain/ceramic crown – primary tooth................. 20 Prefabricated stainless steel crown - primary tooth........................... 20 Prefabricated stainless steel crown - permanent tooth...................... 20 Prefabricated resin crown...................................................................... 20 Prefabricated stainless steel crown with resin window...................... 20 Prefabricated esthetic coated stainless steel crown - primary tooth............................................................................ 20 Core buildup, including any pins when required................................ 20 Post and core in addition to crown, indirectly fabricated................. 20 Prefabricated post and core in addition to crown.............................. 20 pulp cap - indirect (excluding final restoration).................................. 20 Therapeutic pulpotomy (excluding final restoration) - removal of pulp coronal to the dentinocemental junction and application of medicament - Not offered on permanent teeth............................................................................................ 20 Pulpal debridement, primary and permanent teeth - Not offered on primary teeth and excludes teeth 1, 16, 17, and 32...................... 20 Pulpal therapy (resorbable filling) - anterior, primary tooth (excluding final restoration) - Only for permanent anterior teeth................................................................................................ 20 Pulpal therapy (resorbable filling) - posterior, primary tooth (excluding final restoration)......................................... 20 Apexification/recalcification – initial visit (apical closure/calcific repair of perforations, root resorption, pulp space disinfection, etc.) - Only for permanent anterior teeth............ 20 Apexification/recalcification - interim medication replacement (apical closure/calcific repair of perforations, root resorption, pulp space disinfection, etc.).................................... 20 Retrograde filling - per root................................................................... 20 Gingivectomy or gingivoplasty - one to three contiguous teeth or tooth bounded spaces per quadrant...................................... 20 Periodontal scaling and root planing - four or more teeth per quadrant - Available for patients 13 and older. Once per quadrant per two year period.......................................................... 20 Periodontal scaling and root planing - one to three teeth per quadrant - Available for patients 13 and older. Once per quadrant per two year period.......................................................... 20 Periodontal maintenance (limited to 1 per 6 months)....................... 20 D2390 D2391 D2392 D2393 D2394 D2710 D2910 D2915 D2920 D2929 D2930 D2931 D2932 D2933 D2934 D2950 D2952 D2954 D3120 D3220 D3221 D3230 D3240 D3351 D3352 D3430 D4211 D4341 Basic Dental Care - Child D4342 D1510 Space maintainer - fixed - unilateral..................................................... 20 D1515 Space maintainer - fixed - bilateral........................................................ 20 D4910 01.14WAFSECLX | Current Dental Terminology © 2013 American Dental Association. All rights reserved. Copayment Code Description D5410 D5411 D5421 D5422 D5510 D5520 Adjust complete denture - maxillary.................................................... 20 Adjust complete denture - mandibular................................................ 20 Adjust partial denture - maxillary......................................................... 20 Adjust partial denture - mandibular..................................................... 20 Repair broken complete denture base.................................................. 20 Replace missing or broken teeth - complete denture (each tooth)................................................................................ 20 Repair cast framework............................................................................ 20 Add tooth to existing partial denture................................................... 20 Add clasp to existing partial denture.................................................... 20 Tissue conditioning, maxillary............................................................... 20 Tissue conditioning, mandibular........................................................... 20 Unspecified removable prosthodontic procedure, by report........... 20 Recement fixed partial denture............................................................. 20 Extraction, coronal remnants - deciduous tooth............................... 20 Extraction, erupted tooth or exposed root (elevation and/or forceps removal)...................................................... 20 Surgical removal of erupted tooth requiring removal of bone and/or sectioning of tooth, and including elevation of mucoperiosteal flap if indicated..................................... 20 Surgical removal of residual tooth roots (cutting procedure).......... 20 Placement of device to facilitate eruption of impacted tooth......... 20 Biopsy of oral tissue - soft..................................................................... 20 Brush biopsy - transepithelial sample collection................................ 20 Incision and drainage of abscess - intraoral soft tissue..................... 20 Removal of foreign body from mucosa, skin, or subcutaneous alveolar tissue............................................................. 20 Excision of pericoronal gingiva............................................................ 20 Palliative (emergency) treatment of dental pain - minor procedure................................................................................... 20 Deep sedation/general anesthesia - each additional 15 minutes.............................................................................. 20 Inhalation of nitrous oxide / anxiolysis, analgesia............................. 20 Intravenous conscious sedation/analgesia - each additional 15 minutes.................................................................. 20 Non-intravenous conscious sedation................................................... 20 Office visit - after regularly scheduled hours...................................... 20 Therapeutic parenteral drug, single administration............................ 20 Therapeutic parenteral drugs, two or more administrations, different medications................................................. 20 Behavior management, by report......................................................... 20 Office/outpatient visit, new - When performed by your participating general dentist or contracted specialist........................................ 20 Office/outpatient visit, established - When performed by your participating general dentist or contracted specialist........................................ 20 Subsequent hospital care - When performed by your participating general dentist or contracted specialist............................................................ 20 Office consultation - When performed by your participating general dentist or contracted specialist............................................................ 20 Inpatient consultation - When performed by your participating general dentist or contracted specialist............................................................ 20 D5620 D5650 D5660 D5850 D5851 D5899 D6930 D7111 D7140 D7210 D7250 D7283 D7286 D7288 D7510 D7530 D7971 D9110 D9221 D9230 D9242 D9248 D9440 D9610 D9612 D9920 99201 99211 99231 99241 99251 Copayment Major Dental Care - Child D2720 D2721 D2722 D2740 D2750 D2751 D2752 D3310 Crown - resin with high noble metal.................................................. 275 Crown - resin with predominantly base metal.................................. 275 Crown - resin with noble metal........................................................... 275 Crown - porcelain/ceramic substrate................................................. 275 Crown - porcelain fused to high noble metal................................... 275 Crown - porcelain fused to predominantly base metal.................... 275 Crown - porcelain fused to noble metal............................................ 275 Endodontic therapy, anterior tooth (excluding final restoration)................................................................. 275 D3320 Endodontic therapy, bicuspid tooth (excluding final restoration)................................................................. 275 D3330 Endodontic therapy, molar (excluding final restoration)................ 275 Code Description Copayment D3346 D3347 D3348 D3410 D4210 Retreatment of previous root canal therapy - anterior................... 275 Retreatment of previous root canal therapy - bicuspid.................. 275 Retreatment of previous root canal therapy - molar....................... 275 Apicoectomy - anterior - Only for anterior teeth.................................... 275 Gingivectomy or gingivoplasty - four or more contiguous teeth or tooth bounded spaces per quadrant............... 275 D5110 Complete denture - maxillary.............................................................. 275 D5120 Complete denture - mandibular.......................................................... 275 D5211 Maxillary partial denture - resin base (including any conventional clasps, rests and teeth)........................................... 275 D5212 Mandibular partial denture - resin base (including any conventional clasps, rests and teeth)........................................... 275 D5710 Rebase complete maxillary denture.................................................... 275 D5711 Rebase complete mandibular denture................................................ 275 D5720 Rebase maxillary partial denture......................................................... 275 D5721 Rebase mandibular partial denture..................................................... 275 D5750 Reline complete maxillary denture (laboratory)................................ 275 D5751 Reline complete mandibular denture (laboratory)............................ 275 D5760 Reline maxillary partial denture (laboratory)..................................... 275 D5761 Reline mandibular partial denture (laboratory)................................. 275 D5863 overdenture – complete maxillary...................................................... 275 D5864 overdenture – partial maxillary............................................................ 275 D7220 Removal of impacted tooth - soft tissue........................................... 275 D7230 Removal of impacted tooth - partially bony..................................... 275 D7240 Removal of impacted tooth - completely bony................................ 275 D7241 Removal of impacted tooth - completely bony, with unusual surgical complications................................................... 275 D7270 Tooth reimplantation and/or stabilization of accidentally evulsed or displaced tooth.............................................. 275 D7280 Surgical access of an unerupted tooth............................................... 275 D7285 Biopsy of oral tissue - hard (bone, tooth)......................................... 275 D7320 Alveoloplasty not in conjunction with extractions - four or more teeth or tooth spaces, per quadrant......................... 275 D7410 Excision of benign lesion up to 1.25 cm........................................... 275 D7471 Removal of lateral exostosis (maxilla or mandible)......................... 275 D7472 Removal of torus palatinus.................................................................. 275 D7473 Removal of torus mandibularis........................................................... 275 D7485 Surgical reduction of osseous tuberosity........................................... 275 D7520 Incision and drainage of abscess - extraoral soft tissue.................. 275 D7880 Occlusal orthotic device, by report.................................................... 275 D7960 Frenulectomy - also known as frenectomy or frenotomy - separate procedure not incidental to another procedure Pre-authorization is not needed for members 6 and under............................ 275 D7963Frenuloplasty - Pre-authorization is not needed for members 6 and under............................................................................................... 275 D7970 Excision of hyperplastic tissue - per arch......................................... 275 D7972 Surgical reduction of fibrous tuberosity............................................ 275 D9220 Deep sedation/general anesthesia - first 30 minutes....................... 275 D9241 Intravenous conscious sedation/analgesia - first 30 minutes......... 275 D9410 House/extended care facility call - Up to 2 calls per facility per provider................................................................................................ 275 D9420 Hospital or ambulatory surgical center call - Up to 1 call per provider, per day................................................................................... 275 D9940 Occlusal guard, by report..................................................................... 275 Congenital Anomalies Coverage for the treatment of congenital anomalies is available utilizing the services and copayments listed above. Orthodontia - Child Medically necessary orthodontia - member pays $350/year prorated monthly starting with the first month of treatment, with a maximum lifetime copayment of $700. Orthodontic Services will only be approved for enrollees with a malocclusion associated with: a. Cleft lip and palate, cleft palate, or cleft lip with alveolar process involvement; b. Craniofacial anomalies for: • Hemifacial microsomia; • Craniosynostosis syndromes; • Arthrogryposis; or • Marfan syndrome. Must be prior approved. For more detailed information on the terms of your coverage, please consult your Exclusions and Limitations document. Please note: The listed procedures and copayments apply when service is received at your participating general dentist. Not every dentist will perform all services. If your dentist refers you to a specialist, please contact your Member Service Specialist before proceeding. All procedures are available from Dental Health Services participating specialists. All specialty services must be pre-authorized with Dental Health Services through a referral from your participating dentist. If you ever have questions about your dental coverage, call your Member Service Specialist at [800-637-6453]. We are happy to help you. Exclusions and Limitations Limitations: Diagnostic Services are covered with the following limitations: a. Intraoral complete series (D0210) is covered once in a three-year period unless a panoramic radiograph (D0330) for the same enrollee has been performed in the same three-year period. Additional D0210 and D0330 Intraoral complete series films or a panoramic film are only covered if deemed by an orthodontist or Oral Surgeon to be medically necessary; b. Periapical radiograph that are not included in a complete series for diagnosis in conjunction with definitive treatment are only covered when medically necessary; c. Panoramic radiograph (D0330) in conjunction with four bitewings (D0274), once in a three-year period, only when an intraoral complete series (D0210) for the same enrollee has not been paid in the same threeyear period. d. Radiographs with no specific limitation are on a case-by-case basis when medically necessary. e. Oral and facial photographic images (D0350) on a case-by-case basis. Preventive Services are covered with the following limitations: a. Dental Prophylaxis (D1110 & D1120) limited to once every 6 months for enrollees 18 and under, and once every 12 months for 19 years olds. b. Topical Fluoride Treatment (D1208) including fluoride rinse, foam or gel, including disposable trays for enrollees: a. 6 years of age and younger up to 3 times per 12-month period per enrollee; b. 7 to 18 years of age, up to 2 times per 12 month period per enrollee; c. Up to 3 times in a 12-month period per enrollee during orthodontic treatment; d. 19 years of age, once in a 12 month period. e. Additional applications on a case-by-case basis c. Sealants (D1351) is for enrollees 18 years or younger or up to 19 years old for developmentally disabled when used on mechanically and/or chemically prepared enamel surface once per tooth in a 3-year period for enrollees 18 and younger. For developmentally disabled performed in a two-year period. d. Space Maintainers (D1510, D1515, D1550, D1555) for enrollees 12 years of age and younger for fixed unilateral or bilateral space maintenance subject to one space maintainer per quadrant, for primary molars A, B, I, J, K, L, S and T. Restorative Services are covered with the following limitations: a. Two occlusal restorations for the upper molars on teeth 1, 2, 3, 14, 15, and 16 if, the restorations are anatomically separated by sound tooth structure; b. A maximum of five surfaces per tooth for permanent posterior teeth, except for upper molars and a maximum of six surfaces per tooth for teeth 1, 2, 3, 14, 15 and 16; c. A maximum of six surfaces per tooth for resin-based composite restorations for permanent anterior teeth; d. An indirect crown once every 5 years, per tooth, for permanent anterior teeth for enrollees from 12 through 19 years of age. Must be preauthorized; e. All recementations of permanent indirect crowns for enrollees from 12 through 19 years of age; f. Prefabricated stainless steel crowns for primary posterior teeth once every 3 years; g. Prefabricated stainless steel crowns for permanent posterior teeth excluding 1, 16, 17, and 32 once every 3 years; h. Core buildup, including pins, only on permanent teeth, when performed in conjunction with a crown; i. Case post and core or prefabricated post and core, on permanent teeth when performed in conjunction with a crown. Periodontal Services are covered with the following limitations: a. Surgical periodontal services and postoperative care for ginigivectomy/ gingivoplasty. b. Non-surgical periodontal scaling and root planning for the teeth scaled that are periodontically involved once per quadrant for enrollees aged 13 and older per enrollee per two year period when pre-authorized and evidenced by X-ray. c. Periodontal maintenance for enrollees aged 13 and older, once per enrollee per 12 month period with pre-authorization. Endodontic Services are covered with the following limitations: a. Therapeutic pulpotomy on primary teeth and pulpal debridement on permanent teeth only [excluding teeth 1, 16, 17, and 32]; b. Treatment with resorbable material for primary maxillary incisor teeth D,E,F, and G, if the entire root is present at treatment; c. Treatment for permanent anterior, bicuspid, and molar teeth [excluding teeth 1, 16, 17, and 32]. d. Retreatment for the removal of post, pin, old root canal filing material, and all procedures necessary to prepare the canal with placement of new filing material. Prosthodontic Services - Removable are covered with the following limitations: a. One resin based partial denture; replacement covered if provided at least three years after the seat date; b. One complete denture upper and lower and one replacement denture per lifetime after at least 5 years from the seat date; c. Rebasing and relining of complete or partial dentures once in a 3 year period, if performed at least 6 months from the seating date. d. Partial, Complete and Immediate dentures must be pre-approved. Other Limitations: a. Authorized treatment is rendered only by your selected participating dentist or participating specialist (prior authorization is required for services provided by a participating specialist). Services provided by a dentist other than the enrollee’s designated participating provider or authorized specialist, except for emergency dental conditions, are not covered. b. All Services performed must be medically necessary and consistent with a diagnosis of dental disease or condition. c. Specialty services require a referral from your participating dentist and must be pre-authorized by Dental Health Services including a referral to a pediatric dentist. d. Optional services (all cases in which the enrollee selects a plan of treatment that is considered unnecessary by the provider). The enrollee is responsible for fee-for-service rates. This does not apply to standard covered restorative procedures which offer a choice of material. e. Cosmetic dentistry – services for appearance only. This includes such services as the replacement of clinically acceptable amalgam fillings, Veneers and Bonding. f. Unsatisfactory patient-doctor relationship: Dental Health Services providers reserve the right to limit or deny services to an enrollee who fails to follow the prescribed course of treatment, repeatedly fails to keep appointments, fails to pay applicable copayments, is abusive to the participating provider or their staff, or obtains services by fraud or deception. g. Submit claims within 60 days. Dental Health Services shall not be liable to pay a claim for emergency care or for any Dental Health services authorized treatment provided by a dentist other than a participating provider unless the enrollee submits the claim to Dental Health Services within 60 days after treatment. h. Denturists - Enrollees may elect to travel to the nearest participating denturist for services. Enrollees may be able to receive services from a participating denturist as long as service performed was within the lawful scope of the denturist’s license. i. Benefits are only available if work is completed at enrollee’s participating dentist’s office, a pre-authorized specialist or in the event of dental emergency at a non-network dentist. See your Evidence of Coverage pamphlet for more information. j. Not all participating dentists can perform all dental procedures, please verify what services your selected provider can perform for you. Some complicated extractions, periodontal treatment, osseous surgery and root canal treatment may be referred to a participating specialist at the discretion of the general dentist. k. Coverage for services only available during period of enrollment. l. Emergency dental condition – is the emergent and acute onset of a symptom or symptoms, including severe pain that would lead a prudent layperson acting reasonably to believe that dental condition exists that requires immediate, palliative care by a licensed dentist for the relief of pain, swelling or bleeding. This does not include routine, extensive or postponable treatment. Emergency dental care is limited to palliative treatment. Enrollee must attempt to contact their plan dentist. When an enrollee’s plan dentist is not able to be reached, emergency treatment can be sought at any participating dentist. In cases where a participating dentist cannot be reached, the treatment for the emergency dental condition can be completed at any licensed dentist. Plan will reimburse for procedures submitted on a standard claim form up to $150 after member has fulfilled any of their cost sharing requirements. m. Temporomandibular joint (TMJ) disorders and related disease treatment are limited to coverage for occlusal orthotic device for 12-20 months on a case by case basis. n. Dental procedure that cannot be performed in the dental office due to the general health and/or physical limitations of the enrollee are limited to covered services listed in this Schedule of Covered Services and Copayments. Exclusions: The following are not covered by your dental plan. a. Services not specifically listed in the “Schedule of Covered Services and Copayments.” b. Work in progress: Dental work in progress (non-emergency/temporary procedures started but not finished prior to the date of eligibility) is not covered. This includes crown preps prepared and temporized but not cemented, root canals in midtreatment, prosthetic cases post final impression stage (sent to the lab), etc. This does not include teeth slated for root canal treatment and/or canals filled during an emergency visit. c. This Plan does not provide benefits for services or supplies to the extent that benefits are payable for them under any motor vehicle medical, motor vehicle no-fault, uninsured motorist, underinsured motorist, personal injury protection (PIP), commercial liability, homeowner’s policy, or other similar type of coverage. Please note: The listed procedures and copayments apply when service is received at your participating general dentist. Not every dentist will perform all services. If your dentist refers you to a specialist, please contact your Member Service Specialist before proceeding. All procedures are available from Dental Health Services participating specialists. All specialty services must be pre-authorized with Dental Health Services through a referral from your participating dentist. If you ever have questions about your dental coverage, call your Member Service Specialist. We are happy to help you. Dental Health Services A Great Reason to Smile sm 100 W Harrison St., S-440, South Tower, Seattle, WA 98119 [800-637-6453] www.dentalhealthservices.com/WA 0714WM078 © 2014 Dental Health Services