* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Electrophysiology
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
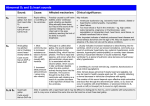
Cardiac Electrophysiology CMCs – atrial and ventricular There is a tight association between the CMC transmembrane potential and the isometric tension of cardiac muscle cell (CMC) contraction – both are initiated almost simultaneously and last for roughly 250ms. This is enabled by an effective refractory period (ERP) of 200ms which prevents the initiation of an AP before the decay of the preceding one as well as the relative refractory period (RRP) which lasts 50ms and only allows AP generation by a higher than normal stimulus (fig. 1). This way, tetanus cannot be achieved in cardiac muscle, thereby, enabling the heart to relax during diastole and fill up with blood. The cardiac AP comprises 4 distinct phases, each characterized by a change in transmembrane voltage attributed to the activation of different ion channels (fig. 2). Action potential 250 ms, almost the same duration as myocardial muscle contraction to prevent tetanus and to allow relaxation during diastole Effective refractory period the duration of which is 200 ms prevents another AP being generated by another stimulus. Relative refractory period lasts 50ms following the end of the ERF during which a bigger than normal stimulus can generate another AP. Maximum diastolic potential, the most negative transmembrane potential during the refractory period, is -50 mV Resting membrane potential is -80 to -90 mV (due to impermeability of negatively charged phosphates and amino acids in the cytosol) and depolarisation reaches its peak at 20 mV. In skeletal muscle the AP is 5 ms long with a 10 ms ERP and RRP while contraction duration is similar to the cardiac AP. This allows for titanic stimulation Phases and currents Phase 4 – resting membrane potential achieved by 3 background currents: the inward rectifying K current (IK1) which leaks K out of the cell down concentration gradient; the Na current (Ib) which takes Na into the cell down an electrochemical gradient and the NaK pump which allows 2K ions into the cell for an exchange of 3Na ions. These currents ensure a resting potential above EK. Phase 0 – rapid depolarization when -60mV threshold reached, mediated by the opening of Na channels and Na influx down the concentration gradient. Na channels and ICa inactivate. Phase 1 – Initial (partial) repolarisation phase maintained by IK1. Phase 2 – initial plateau maintained by L-type Ca channels that allow a small inward Ca current to oppose IK1. The late plateau phase is maintained by the forward mode NCX electrogenic pump that allows 3Na ions into the cell for every Ca ion. This current is increased by high sarcoplasmic Ca levels. The permeability of K channels decreases. Phase 3 – rapid repolarisation. Ca currents cease and the delayed rectifier (IK), also known as HERG, is slowly activated, expelling K ions out of the cell and restoring the resting membrane potential. IK1 is also activated. It is due to the HERG channel that the AP is long so as to prevent the tendency to generate dysrhythmias. Nodal cells – SAN, AVN and His bundle Action potential Spontaneous Less negative resting potential (-60 mV) and less positive depolarisation peak No inward rectification or Na channels Unlike CMCs nodal cells do not contribute to the ECG. Phases and currents Phase 4 – pacemaker potential that contributes to automaticity of the cell: slow depolarisation by influx of Na by non-selective If current. Phase 0 – rapid depolarisation by highly selective ICa which allows Ca into the cell, driving membrane potential towards ECa. Phase 3 – Ca channels close and HERG opens causing efflux of K and repolarising the cell back to – 60 mV which triggers the If channel, repeating the cycle. The AVN has some pacemaker activity as a potential compensatory mechanism in case of SAN malfunction EC coupling Nodal cells spindle shaped and mononucleate, with a low conduction velocity across nexus ( 5 – 10 cm/s) Purkinje cells binucleate with a 100 – 150 cm/s conduction velocity across intercalated disc. They connect to endocardial CMCs and conduct impulses to them. CMCs are binucleate with a conduction velocity of 50 cm/s across intercalated discs. Only CMCs are packed with contractile proteins and mitochondria A nexus is an electrical link whereas zona adherans (CMCs and Purkinje cells) is a mechanical link Orientation of CMCs changes throughout myocardial wall to ensure multidirectional impulse signal Channels and contraction Physical coupling to DHP (L-type Ca channels) on t-tubule sarcolemma opens them, causing an influx of Ca into the cell, activating RyR channels on SR membrane to release Ca into the cytosol. Backward mode NCX pump transports a Ca ion in for 3 Na ions out due to positive membrane potential. Ca in the cytosol binds to troponin C on the thin filament leading to cross bridging and contraction. Ca is removed from the sarcomere into the mitochondrion via the Ca uniporter, into the SR via SERCA (phospholamban) and out of the cell via the sarcolemmal Ca ATPase pump and forward mode NCX. An increased frequency in stimulation causes an accumulation of Ca in the cell due to the slow efflux via NCX and Ca ATPase, thus causing a positive ionotropic effect. Heart Anatomy RA Right auricle allows RA to distend upon increased VR (in left atrium auricle smaller) Pectinate muscles in auricle prevent blood from accumulating and clotting Fossa ovalis – a congenital septal hole that forms a membrane around after birth Ostium of coronary sinus drains blood from myocardium to the RA Eustachian valve of IVC forces blood to middle of RA so as not to accumulate below Valves Tricuspid valve has 3 leaflets: anterior posterior and septal Papillary muscles and chordae tendinae only in atrioventricular valves Semilunar valves have flaps around which blood flows, creating pressure and forcing the flaps to shut to prevent backflow into atria. Infundibulum – outlet leadint to PA Septomarginal trabeculations – septal and moderator bands that form the nerve bundle. Moderator band conveys bundle branch to anterior papillary to facilitate conduction time. Trabeculae carnae – like pectinate muscles only in RV RV Coronary arteries and Anastomoses Right dominance most common – PDA supplied by right coronary -> PDA blocked Left dominance more severe as supplies LAD and PDA -> both blocked and both usually supply anastomoses in the septum (septal perforators) Co-dominance most rare: PDA comes off whichever CA is dominant Cardiac cycle Starling’s law = ^ VR -> ^ Force Contraction -> ^SV ^ VR causes ^ VV which instantaneously causes ^ force contraction due to myocardial stretch. 10 -15 min contraction shows positive staircase where a slow increase in CMC Ca levels causes increased and transient force of contraction. Increasing VP increases VR which increases VV and distends ventricles, increasing contraction and SV as blood is pushed out due to decrease in distension. SV increase shows Anrep effect – it progressively increases within 10-15 min due to a slow increase in force of contraction that pushes more blood out (positive staircase) Starling’s proof in isolated dog heart experiment: increasing CVP increased SV by 64% and decreasing ventricular distension had no effect on SV meaning an increase in contractility played a role in increasing SV. Cycle Cycle lasts 0.8 s of which, normally, 2/3 is diastole and 1/3 is systole. Normal vitals: HR = 70bpm, BP =120/80, CO = 5 l/min, SV = 70 ml/min Heart muscles are relaxed as heart fills up with blood. AV valves are open. Low pressure in heart but higher in atria so as to direct flow downwards into ventricles Diastole Atrial systole Ventricles filled with blood Ventricular systole Increase in ventricular volume causes distension and an increase in pressure, causing AV valves to shut as ventricular pressure now exceeds atrial. Isovolumetric contraction where volume in ventricles remains the same due to both AV and semilunar valves being shut, but an increase in pressure due to myocardial contraction. Semilunar valves are forced open and blood is ejected into pulmonary arteries/aorta. As ventricles empty, pressure in them is lower than beyond the semilunar valvues causing them to shut (dicrotic notch). Isovolumetric relaxation when end systolic volume in ventricles stays the same while pressure decreases below atrial. This causes AV valves to open. End systolic volume retained after each beat and end diastolic volume retained before each beat. PV loop Increased during exercise where VR is greater, increasing EDV, so force of contraction is greater and SV is greater. Sympathetic output to heart increases contractility but VV falls so loop increases but shifts to the left. Decreased during hemorrhage when increased HR causes an increase in circuitry, narrowing loop and a decrease in VR causes it to shift to the left. Anoxia causes heart to dilate, shifting loop to right, and making it smaller due to decreased contractility that exerts less pressure. The reason for this is increased pH due to lactic acid produced from anaerobic respiration of CMCs. A loop shifted too much to the right means Starling’s law does not apply and heart fails – dangerous for weak hearts. ECG P wave: depolarization of atrial CMCs. PR interval (120-200ms) represents time taken for SAN to activate AVN QRS complex (80-120ms): depolarization of ventricular CMCs. ST interval (80-120ms) interval represents isoelectric potential of depolarized ventricular CMCs. T wave (160ms): ERP/RRP of ventricular CMC repolarization. QT interval (~250ms) is when there is risk of arrhythmias. Defects and dysrhythmias VSDs In isolated VSDs, where the perimembranous ventricular septum thins and is disrupted by turbulent flow, blood is shunted from left to right as the LV generates more power. VSDs of the muscular septum are rarer as that part of the interventricular septum is the thickest. Tetralogy of Fallot Initial left to right shunt but due to rapid RV hypertrophy the shunt changes to right to left. Pulmonary stenosis Aorta overriding septum allowing deoxygenated RV blood to enter it As a result deoxygenated blood enters the systemic circulation during each beat and in severe cases metabolic O2 demand is not met. Dysrhythmias Classified by: Brady/tachy; ventricular/supraventricular/ transient/sustained; altered impulse formation/conduction Benign e.g sinus arrhythmia (positive chronotropic effect on inspiration); pathological e.g atrial fibrillation (risk of stroke, syncope, symptoms) and lifethreatening e.g ventricular fibrillation where defibrillation required to save life. Normal inward septal excitation followed by endocardial to epicardial excitation; abnormal ectopic excitation disrupts pattern causing slow and ineffective myocardial activation (shown by QRS complex of more than 140ms) Junctional ectopic tachycardia: impulse originates in AVN/His bundle Torsade de pointes: intermittent ventricular tachycardia AV nodal re-entrant tachycardia and SAN re-entrant tachycardia where SAN is re-excited (in Wolf Parkinson White syndrome due to retrograde conduction by fibrous flap) Long QT/Brugada syndrome: QT interval more than 250ms Atrial flutter/fibrillation and ventricular fibrillation AVN block Causes Congenital structural e.g WPWS Congenital channelopathies (due to polymorphisms in genes encoding channels causing variation in Ca concentrations and AP amplitudes Ischaemia e.g due to myocardial infarction Myocarditis causing poor beating Enlarged hearts e.g in athelets Electrolyte imbalance Antiarrhythmic drug side effects Self-perpetuating e.g atrial fibrillation causes more atrial fibrillation Catheter ablation (surgery) Defibrillation Antiarrhythmic drugs Pacemaker implantation Treatment SAN automaticity Increased by ischaemia and sympathetic outflow (either during emotional stress or exercise) -> beta receptors -> ^ pacemaker potential Decreased by vagal outflow -> M receptors -> decrease pacemaker potential or cause escape rhythm where pacemaker shifted to another atrial site due to SAN suppression. Bundle of Kent An AV bypass tract conducts impulses directly from atrium to ventricles, represented by delta wave which shortens the PR interval and shows early ventricular excitation – WPWS