* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 271 KB - International Medical Press
Survey
Document related concepts
Drug interaction wikipedia , lookup
Discovery and development of HIV-protease inhibitors wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Electronic prescribing wikipedia , lookup
Transcript
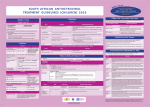
Antiviral Therapy 2012; 17:1385–1388 (doi: 10.3851/IMP2182) Case report Severe dyslipidaemia after the addition of raltegravir to a lopinavir/ritonavir-containing regimen Emily Huesgen1, Rodrigo Burgos1, Debra A Goldstein2, Blake Max1,3, Olamide D Jarrett4* Department of Pharmacy Practice, University of Illinois at Chicago, Chicago, IL, USA Department of Ophthalmology, University of Illinois at Chicago, Chicago, IL, USA 3 CORE Center, John H Stroger, Jr. Hospital of Cook County, Chicago, IL, USA 4 Division of Infectious Diseases, Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA 1 2 *Corresponding author e-mail: [email protected] We describe a 55-year-old HIV-1-infected male who developed severe dyslipidaemia (total cholesterol 600 mg/ dl, triglycerides >5,000 mg/dl, high density lipoprotein <5 mg/dl) after raltegravir was added to his lopinavir/ ritonavir-containing regimen. To our knowledge, this is the first reported case of severe dyslipidaemia associated with the addition of raltegravir to a lopinavir/ritonavir-based regimen, suggestive of a possible drug interaction. The lipid profile quickly normalized following discontinuation of lopinavir/ritonavir and continuation of raltegravir, suggesting that lopinavir/ritonavir was the primary driver for the adverse event. With increasing interest in nucleoside-sparing regimens, knowledge of clinically significant adverse events such as this is important for HIV clinicians when selecting regimens for patients with highly resistant virus or drug tolerability issues. Introduction There are currently 24 FDA-approved antiretroviral medications for the treatment of HIV-1 infection, resulting in a vast number of potential drug combinations. More than half of these drugs are metabolized by hepatic cytochrome P450 enzymes, of which inhibition or induction can alter drug pharmacokinetics leading to subtherapeutic or supratherapeutic plasma concentrations. Although the pharmaceutical industry has been vigilant in conducting preclinical drug-interaction and safety studies, data are limited due to the small size of these studies and the intra- and inter-patient variability. Clinicians depend on post-marketing data and case reports to add to the body of literature regarding potential drug interactions and adverse events from antiretroviral medications. We describe a patient who was diagnosed with lipaemia retinalis after a routine retinal exam. The acute onset of severe dyslipidaemia was evident after raltegravir (RAL) was added to his lopinavir/ritonavir (LPV/RTV)containing regimen, suggesting a possible drug–drug interaction that led to the significant adverse event. To our knowledge, this is the first reported case of severe dyslipidaemia associated with the addition of RAL, an HIV-1 integrase inhibitor, to an LPV/RTV-based regimen. ©2012 International Medical Press 1359-6535 (print) 2040-2058 (online) AVT-11-CR-2388_Huesgen.indd 1385 Case report A 55-year-old asymptomatic African American male with multidrug resistant HIV-1 infection developed breakthrough viraemia of 125 and 160 copies/ml on two consecutive clinic visits, over a 3 month interval, despite reported 100% adherence to antiretroviral therapy (ART). He previously had successful viral suppression for 3 years while receiving a regimen of LPV/RTV 400/100 mg twice daily, abacavir (ABC) 300 mg twice daily and tenofovir disoproxil fumarate (TDF) 300 mg once daily. Out of concern for evolving ABC resistance, given known history of multiple thymidine analogue mutations and the M184V mutation, ABC was discontinued and RAL was added. Emtricitabine (FTC) was also added as part of the fixed-dose combination of FTC/TDF to promote M184V-induced TDF hypersensitivity. He regained virological control to <48 copies/ml at the subsequent follow-up visit. In addition to HIV, the patient’s medical history included dyslipidaemia, hypertension, benign prostatic hyperplasia, hypogonadism, cataracts and mild renal insufficiency (estimated creatinine clearance of 60 ml/ min) and he was taking the following medications in addition to his ART: atorvastatin 10 mg daily, 1385 26/10/2012 14:34:44 E Huesgen et al. Figure 1. Fundus photographs of the patient’s retina A B (A) Lipaemia retinalis; creamy appearance of all retinal vessels and salmon-coloured choroidal vasculature and (B) return of normal retinal vasculature colour after normalization of triglycerides. Table 1. Lipid panel timeline in relation to changes in antiretroviral therapy Date 28/12/06 28/9/09 11/11/09 1/6/10 3/6/10 24/6/10 4/5/11 ART regimen ABC, TDF, – – TDF, FTC, – TDF, FTC, ETR, – LPV/RTV LPV/RTV, RAL RAL ART change– – ABC stopped; – LPV/RTV stopped; –– FTC, RAL added ETR added Cholesterol, mg/dl 225 143–600a 515 307 195 Triglycerides, mg/dl 449 193–5,364 5,168 90 198 HDL, mg/dl 43 36– <5 <5 67 43 LDL, mg/dl NA 68–NA NA 222 112 Random lipid profile. All other lipid profiles listed are fasting. ABC, abacavir; ART, antiretroviral therapy; ETR, etravirine; FTC, emtricitabine; HDL, high-density lipoprotein; LDL, low-density lipoprotein; LPV/RTV, lopinavir/ritonavir; NA, not able to calculate; RAL, raltegravir; TDF, tenofovir disoproxil fumarate. a ezetimibe 10 mg daily, fenofibrate 48 mg daily, hydrochlorothiazide (HCTZ)/triamterene 25/37.5 mg daily, feldopine ER 5 mg daily, tamsulosin 0.4 mg daily and testosterone patch 5 mg/24 h daily. Of note, no changes were made to these medications when his ART was changed. Seven months after starting his new ART regimen, the patient presented to an ophthalmology clinic for a routine follow-up visit to assess his cataracts. Dilated fundoscopic exam revealed bilateral creamy arterioles (Figure 1A), consistent with a diagnosis of lipaemia retinalis due to severe hypertriglyceridaemia. During physical examination the patient denied chest pain, abdominal pain, dyspnea, nausea/vomiting or headache. 1386 AVT-11-CR-2388_Huesgen.indd 1386 A stat lipid profile was obtained and the results confirmed the diagnosis of severe dyslipidaemia with total cholesterol 600 mg/dl, triglycerides 5,364 mg/dl and high-density lipoprotein (HDL) less than 5 mg/dl. A fasting lipid panel 48 h later confirmed the results with total cholesterol 515 mg/dl, triglycerides 5,168 mg/dl and HDL <5 mg/dl (Table 1). Of note, six weeks prior to the ART change, the patient’s total cholesterol was 143 mg/dl, triglycerides 193 mg/dl, HDL 36 mg/dl, and low-density lipoprotein (LDL) 68 mg/dl. Medication non-adherence and new alcoholism were ruled out as potential causes of the acute worsening of dyslipidaemia. Follow-up laboratory testing also ruled out new onset diabetes mellitus, hypothyroidism, pancreatitis and ©2012 International Medical Press 26/10/2012 14:34:48 Raltegravir and lopinavir/ritonavir-associated dyslipidaemia nephrotic syndrome as potential causes, with fasting glucose, haemoglobin A1C, thyroid stimulating hormone, lipase and random urine protein all within normal limits. Thus, the patient’s severe dyslipidaemia was believed to be due to the recent changes in his antiretroviral therapy. LPV/RTV was subsequently discontinued because it was felt to be the main driver of his lipid abnormalities and etravirine 200 mg twice daily was initiated. In addition, his fenofibrate was increased to 160 mg daily and he was started on omega-3 fatty acids 2 gm twice daily. The atorvastatin was held temporarily out of concern for increased risk of rhabdomyolysis when combined with high-dose fenofibrate. A repeat fasting lipid panel was performed two weeks later and his triglycerides had decreased to 90 mg/dl. His prior lipid-lowering regimen was resumed. The patient followed up with ophthalmology 4 months later and on exam the previous retinal findings had completely resolved (Figure 1B). Triglycerides, LDL-cholesterol and total cholesterol have remained well controlled since that time. Discussion Dyslipidaemia is a known side effect of RTV-boosted protease inhibitors (PI). The mechanism of action for PI-induced dyslipidaemia is not well understood. Genetics, prior use of PIs and boosting with RTV are thought to contribute to dyslipidaemia [1–3]. Some studies have shown a correlation between LPV concentrations and lipid abnormalities [4,5], however, a recent study did not find this association [6]. The onset of dyslipidaemia following initiation of LPV/ RTV typically occurs during the first 2–3 months of therapy and stabilizes thereafter [7–9]. Our patient had significant dyslipidaemia during LPV/RTV initiation, which required three-drug therapy for management; however, this had been controlled with antilipidaemic medications for almost 3 years prior to the addition of RAL (Table 1). Emtricitabine is not known to cause dyslipidaemia, but was added at the same time as RAL, so it cannot be excluded. However, it is an unlikely contributor, as his lipid profile remained within normal limits while on this medication, following the discontinuation of LPV/RTV. In reviewing his non-HIV medications, HCTZ has been reported to cause lipid increases, but elevations typically occur within the first two weeks of initiation [10]. Our patient had been taking HCTZ for several years without any side effects and thus it is unlikely that HCTZ was associated with the acute lipid changes. The patient was never re-challenged with the LPV/RTV–RAL combination. However, the onset of dyslipidaemia after RAL initiation and rapid resolution following LPV/RTV cessation is suggestive of a combined effect of LPV/RTV and RAL on lipids. Antiviral Therapy 17.7 AVT-11-CR-2388_Huesgen.indd 1387 We believe that LPV/RTV was the main driver of our patient’s dyslipidaemia because his lipid profile rapidly normalized following discontinuation of LPV/RTV and continuation of RAL. Using the Naranjo Adverse Drug Reaction Probability Scale, a well-validated method for establishing causality of an adverse drug-related event, the calculated Naranjo score is 8, indicating a probable adverse drug event (definite adverse drug-related event defined as a score ≥9) [11]. The elevations in total cholesterol and triglycerides observed in our patient coincide with preliminary data from the PROGRESS Study, a safety and efficacy study comparing RAL plus LPV/RTV to LPV/RTV plus FTC/TDF in treatment-naive patients. Data at 48-weeks suggest that LPV/RTV in combination with RAL was associated with significant mean increases in triglycerides (99 versus 59 mg/dl; P=0.044), total cholesterol (46 versus 29 mg/dl; P=0.008) and HDL-cholesterol (12 versus 8 mg/dl; P=0.015) from baseline in comparison to LPV/RTV plus FTC/TDF, an unexpected finding [12]. Our patient, however, experienced a significant decrease in HDL-cholesterol in contrast to the HDL increases reported in the PROGRESS study. RAL has not been associated with hyperlipidaemia in large randomized clinical trials [13]. In the SWITCHMRK trials, patients who were switched from LPV/RTV to RAL had greater reductions in total cholesterol (-12.6% versus 1%), non-HDL cholesterol (-15% versus 2.6%) and triglycerides (-42.2% versus 6.2%) compared to patients that remained on regimens containing LPV/RTV (P<0.0001) [14]. Lipid data from two other nucleoside-sparing studies comparing RAL plus a PI (either unboosted atazanavir or boosted darunavir) to RAL plus FTC/TDF were similar between study arms, suggesting that lipid elevations observed in the PROGRESS study are unique to LPV/RTV plus RAL [15,16]. The mechanism for the lipid elevations observed in our patient and in the PROGRESS study is unknown. LPV is a known substrate of CYP3A4 and RTV is a potent inhibitor of multiple cytochrome P450 enzymes [17]. However, RAL has not been shown to be an inhibitor of CYP3A4 or P-glycoprotein mediated transport, so it is unlikely that RAL-induced increases in plasma LPV/RTV concentrations would explain the effect seen [13]. It is plausible that RAL and LPV/ RTV share an unknown efflux or uptake transport protein, which have been associated with unexpected interactions with other antiretrovirals [18,19]. If that is the case, then RAL could increase LPV/RTV levels through alternate pathways leading to the dyslipidaemia seen in our patient. Of particular concern is that our patient was asymptomatic when diagnosed with lipaemia retinalis 1387 26/10/2012 14:34:48 E Huesgen et al. so it is unknown how quickly our patient’s lipids reached such dangerously elevated levels in relation to his regimen change. HIV infection and dyslipidaemia are both known risk factors for cardiovascular disease, which can lead to life-threatening acute coronary syndromes [20]. Conclusion This is the first reported case of a possible drug interaction between RAL and LPV/RTV leading to severe dyslipidaemia. Clinicians should be alerted to the possibility that regimens containing this combination may greatly alter lipid profiles, even in patients that have tolerated LPV/RTV in the past. We recommend careful monitoring of fasting lipid profiles for patients on this antiretroviral combination. Further prospective safety studies with this antiretroviral combination are warranted. Disclosure statement The authors declare no competing interests. References 1. 2. 3. 4. 5. 6. Fauvel J, Bonnet E, Ruidavets JB, et al. An interaction between apoC-III variants and protease inhibitors contributes to high triglycerides/low HDL levels in treated HIV patients. AIDS 2001; 15:2397–2406. Martínez E, Domingo P, Galindo MJ, et al. Risk of metabolic abnormalities in patients infected with HIV receiving antiretroviral therapy that contains lopinavirritonavir. Clin Infect Dis 2004; 38:1017–1023. Calza L, Manfredi R, Farneti B, et al. Incidence of hyperlipidaemia in a cohort of 212 HIV-infected patients receiving a protease inhibitor-based antiretroviral therapy. Int J Antimicrob Agents 2003; 22:54–59. Gutiérrez F, Padilla S, Navarro A, et al. Lopinavir plasma concentrations and changes in lipid levels during salvage therapy with lopinavir/ritonavir-containing regimens. J Acquir Immune Defic Syndr 2003; 33:594–600. González de Requena D, Blanco F, Garcia-Benayas T, et al. Correlation between lopinavir plasma levels and lipid abnormalities in patients taking lopinavir/ritonavir. AIDS Patient Care STDS 2003; 17:443–445. Bierman WF, van Vonderen MG, Veldkamp AI, et al. The lopinavir/ritonavir-associated rise in lipids is not related to lopinavir or ritonavir plasma concentration. Antivir Ther 2011; 16:647–655. 7. Gathe J, da Silva BA, Cohen DE, et al. A once-daily lopinavir/ritonavir-based regimen is noninferior to twicedaily dosing and results in similar safety and tolerability in antiretroviral-naive subjects through 48 weeks. J Acquir Immune Defic Syndr 2009; 50:474–481. 8. Lafeuillade A, Hittinger G, Philip G, et al. Metabolic evaluation of HIV-infected patients receiving a regimen containing lopinavir/ritonavir (Kaletra). HIV Clin Trials 2004; 5:392–398. 9. Murphy RL, da Silvia BA, Hicks CB, et al. Sevenyear efficacy of a lopinavir/ritonavir-based regimen in antiretroviral-naive HIV-1-infected patients. HIV Clin Trials 2008; 9:1–10. 10. Hydrochlorothiazide. In: DRUGDEX® System. Version 5.1. Greenwood Village, CO: Thomson Reuters (Healthcare) Inc. 11. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981; 30:239–245. 12. Reynes J, Lawal A, Pulido F, et al. Lopinavir/ritonavir combined with raltegravir demonstrated similar antiviral efficacy and safety as lopinavir/ritonavir combined with tenofovir disoproxil fumarate/emtricitabine in treatment-naive HIV-1 infected subjects. 18th International AIDS Conference. 18-23 July 2010, Vienna, Austria. Abstract MAOB01. 13.Isentress. Package insert 2007. Merck & Co., Inc, Whitehouse Station, NJ, USA. 14. Eron JJ, Young B, Cooper DA, et al. Switch to a raltegravirbased regimen versus continuation of a lopinavirritonavir-based regimen in stable HIV-infected patients with suppressed viraemia (SWITCHMRK 1 and 2): two multicentre, double-blind, randomised controlled trials. Lancet 2010; 375:396–407. 15. Bedimo R, Drechsler H, Turner D, et al. RADAR study: raltegravir combined with boosted darunavir has similar safety and antiviral efficacy as tenofovir/emtricitabine combined with boosted darunavir in antiretroviral-naive patients. 6th IAS Conference. 17–20 July 2011, Rome, Italy. Abstract MOPE214. 16. Kozal MJ, Lupo S, DeJesus E, et al. The SPARTAN study: a pilot study to assess the safety and efficacy of an investigational NRTI- and RTV-sparing regimen of atazanavir (ATV) experimental dose of 300 mg BID plus raltegravir (RAL) 400 mg BID (ATV + RAL) in treatmentnaive HIV-infected subjects. 18th International AIDS Conference. 18–23 July 2010, Vienna, Austria. Abstract THLBB204. 17.Kaletra. Package insert 2000. Abbott Laboratories, North Chicago, IL, USA. 18. Huisman MT, Smit JW, Crommentuyn KM, et al. Multidrug resistance protein 2 (MRP2) transports HIV protease inhibitors, and transport can be enhanced by other drugs. AIDS 2002; 16:2295–2301. 19. Moss DM, Kwan WS, Liptrott NJ, et al. Raltegravir is a substrate for SLC22A6: a putative mechanism for the interaction between raltegravir and tenofovir. Antimicrob Agents Chemother 2011; 55:879–887. 20. Baker JV, Lundgren JD. Cardiovascular implications from untreated human immunodeficiency virus infection. Eur Heart J 2011; 32:945–951. Accepted 13 February 2012; published online 22 June 2012 1388 AVT-11-CR-2388_Huesgen.indd 1388 ©2012 International Medical Press 26/10/2012 14:34:48