* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ca-Channel blockers:
Survey
Document related concepts
Transcript
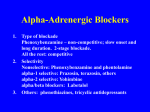
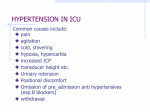
Ca-Channel blockers: They do not affect serum lipid concentrations Not cause sexual dysfunction. Diuretics enhance the efficacy of Cachannel blockers. Mechanism of action: Amlodipine, diltiazem, verapamil, felodipine, isradipine, nifedipine and nicardipine induce vasodilation and decrease peripheral resistance. 2. Pharmacologic effects: a. Verapamil, amlodipine, and diltiazem cause little change in heart rate, whereas the dehydropyridines produce an initial increase, which is reflex-mediated. b. Diltiazem and verapamil depress A-V conduction and should not be used with beta blockers. 3. Adverse effects: Verapamil can cause severe constipation. Vasodilators: decrease peripheral vascular resistance and arterial blood pressure. a. Their effect compensated by reflex sympathetic activity. b. They increase plasma renin activity. c. causes salt and water retention. d used in conjunction with diuretic and beta adrenergic blocking therapy. Hydralazine: a. Pharmacokinetics (1) given orally (long treatment) or IM. (2) It is subjected to first-pass hepatic metabolism. (3) It is metabolized by several pathways, including acetylation, which is subject to genetic variation. (4) Its duration of effect ranges from 2-6 hours. (5) Tolerance develops after 24 months of therapy. b. Therapeutic uses: (1) It is used to treat moderate to severe hypertension. (2) It is used in the treatment of acute and chronic CHF. c. Route of administration: (1) must be combined with beta-blocker to prevent tachycardia and increased renin secretion resulting from reflex sympathetic stimulation. (2) Oral hydralazine is combined with diuretic agent to prevent salt and water retention. Minoxidil: Potent than hydralazine. It decreases renal vascular resistance with no effect on renal blood flow. It is orally administered, excreted with urine. Used to treat sever hypertension (associated with renal impairment). It should be coupled with beta-blockers and diuretic to overcome sympathetic activation and salt retention. Adverse effects: pericardial effusion and tamponade in patients with renal impairment. Hirsutism occurs with no virilism or other endocrine abnormalities. Diazoxide: Reduce both systolic and diastolic pressure, inducing sympathetic activation. It relaxes other smooth muscle. It inhibits the release of insulin. Uses, Intravenous diazoxide is used for hypertensive emergencies. Diazoxide used orally to treat hypoglycemia that is caused by hyperinsulinemia. Diazoxide is given by rapid injection into a peripheral vein. Adverse effects (1) Severe hypotension. (2) Its reflex sympathetic stimulation can cause angina and worsen myocardial ischemia. (3) It inhibits the release of insulin and can produce hyperglycemia. (4) Edema caused by the retention of salt and water. Non selective (Arterial and venous vasodilators): These drugs reduce both arterial resistance and venous tone and markedly decrease arterial blood pressure. 1. Sodium nitroprusside Onset of action within 1 minute of IV. administration, duration within 5 minutes. It is rapidly inactivated by hepatic enzymes, first to cyanide and then to thiocyanate. No effect on other smooth muscle. Decreases myocardial oxygen demand. Renal blood flow is maintained with nitroprusside, and renin secretion is increased. Uses (1) Nitroprusside, used in hypertensive emergencies. It is preferable to diazoxide in patients with coronary insufficiency or pulmonary edema because, in contrast to diazoxide, it reduces cardiac preload and myocardial oxygen demand. (2) Used to produce controlled hypotension to minimize bleeding during surgery. (3) Nitroprusside can improve left ventricular function in patients with acute myocardial infarction and has benefit in the treatment of acute CHF. Route of administration (1) Na-nitroprusside is administered only as an intravenous infusion with sterile 5% dextrose in water. Once prepared, the solution must be protected from light and used within 4 hours. (2) Blood pressure must be monitored continuously while the drug is being given. Adverse effects (1) Hypotension, nausea, diaphoresis, headache, restlessness, palpitations, and retrosternal pain can occur secondary to excessive, rapid vasodilation. (2) It is metabolized to cyanide and to thiocyanate. cyanide toxicity can occur. (3) Accumulated thiocyanate during prolonged nitroprusside therapy, especially in patients with poor renal function greater than 10 mg/dl can cause weakness/ nausea/ muscle spasms and psychosis, as well as hypothyroidism caused by interference with iodine transport. 2. Prazosin: is a selective postsynaptic α one adrenergic receptor blocking agent that causes vasodilation of both the arteries and veins. a. Pharmacokinetics (1) Plasma half-life is usually 2-3 hours but can be prolonged by CHF. (2) Undergo significant first-pass metabolism. It is excreted in the feces and bile. b. Pharmacologic effects (1) it reduces peripheral vascular resistance. (2) Unlike nonselective α-adrenergic blockers, prazosin does not usually produce reflex tachycardia. (3) Unlike beta blockers, prazosin does not adversely affect insulin sensitivity or blood lipids. (4) It does not increase plasma renin activity. (5) Prazosin produces minimal changes in cardiac output, renal blood flow, and glomerular filtration rate. Therapeutic uses of prazosin: (1) treatment of mild to moderate hypertension alone or in combination., more effective in conjunction with a diuretic or an α-adrenergic blocking agent. (2) treatment of acute CHF. Route of administration: orally,2-3 times daily. Adverse effects (1) Dizziness, headache, drowsiness and palpitations can occur but disappear with continued therapy. (2) prazosin larger than 1 mg can induce postural hypotension and syncope due to a decreased venous return to the heart. (3) antinuclear factor become positive. 3. Terazosin is similar to prazosin with longer t1/2 (12 hours) and duration (24 hours). Terazosin is used to treat benign prostatic hyperplasia as well as hypertension. Mechanism of action: Terazosin is an αpostsynaptic adrenoreceptor blocker that rapidly relaxes smooth muscle tone in the arteries, bladder neck, prostate capsule and prostatic urethra. Pharmacokinetics rapidly and completely absorbed orally. (2) metabolized by the liver and excreted mainly in bile. Adverse effects: (1) Orthostatic hypotension and syncope. (2) Other adverse effects associated with αadrenergic blockers may occur, including nasal congestion and impotence. C