* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download - SlideBoom
Survey
Document related concepts
Transcript
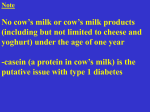
Tay Ju Lee MD INTI Diploma Pharmacology The Endocrine System We will be reviewing relevant pathophysiology & drugs related to Pancreas Sex Hormones Uterus related Hormones Thyroid Adrenal gland Today’s objectives Pancreas & Pancreatic Islet Hormones Insulin Control of Blood Glucose Diabetes Mellitus Insulin Treatment Oral Hypoglycemics The Pancreas Pancreas is exocrine AND endocrine Pancreatic Islet of Langerhans Hormones Four main cell types secreting peptide hormones A cells – glucagon B cells – insulin D cells – somatostatin PP cells – pancreatic polypeptide (unknown function) Other hormones briefly… Glucagon Fuel-mobilising hormone - gluconeogenesis and glycogenolysis – increase blood glucose. Lipolysis and proteolysis. Increases the force of contraction of the heart. Somatostatin Inhibits release of insulin and of glucagon Centrally inhibit growth hormones Octreotide is a long-acting analogue of somatostatin ○ Treatment of acromegaly & other several other endocrine tumors Clinical Uses of Glucagon Glucagon can be given intramuscularly or subcutaneously as well as intravenously. Treatment of hypoglycaemia in unconscious patients (who cannot drink) Treatment of acute cardiac failure precipitated by β-adrenoceptor antagonists Insulin is required for all animal life (excluding certain insects) Insulin synthesis in B cells Preproinsulin (RER) Proinsulin (GA) Insulin & C- peptide B l o o d Factors stimulating insulin B cells respond both to the absolute glucose concentration and to the rate of change of blood glucose. Insulin release include amino acids (particularly arginine and leucine), Fatty acids Parasympathetic nervous system Peptide hormones for the gut gastrin secretin cholecystokinin gastric inhibitory polypeptide (GIP) glucagon-like peptide (GLP) Diagram of factors effecting insulin secretion • Glucose enters B cells via Glut-2 - glucokinase makes glucose-6-phosphate traps glucose In cell. • As glucose metabolism proceeds, ATP is produced in the mitochondria. • Intracellular ATP closes KATP • Membrane depolarises – K + cannot leave. • Voltage-dependent calcium channels open - Ca2+ influx • Insulin exocytosis B cell action Glut-4 on muscle and fat cells Actually…. it’s much more complicated ..\Pharmacody namics & Pharmacokine tics 2011\Insulin Signaling (Signal Pathways).flv http://dolly.biochem.arizona.edu/Bioc462b_Honors_Spring_2009/abhik/MyoC1%20GLU T4.html Effects of insulin on carbohydrate, fat and protein metabolism Type of metabolism Carbohydrate metabolism Liver cells Fat cells Muscle ↓Gluconeogenesis ↑Glucose uptake ↑Glucose uptake ↓Glycogenolysis ↑Glycerol synthesis ↑Glycolysis ↑Glycolysis ↑Glycogenesis Effects of insulin on carbohydrate, fat and protein metabolism ↑Glycogenesis Fat metabolism ↑Lipogenesis ↓Lipolysis ↑Synthesis of triglycerides ↑Fatty acid synthesis ↓Lipolysis Protein metabolism ↓Protein breakdown - ↑Amino acid uptake ↑Protein synthesis Why is Blood Glucose controlled? BRAIN – glucose is obligatory source of energy for the brain Physiological control reflects need to maintain adequate fuel supplies Intermittent food intake Variable metabolic demands Excess stored as glycogen(safe shortterm storage) or fat(long-term storage) Two phase release to continuous glucose infusion. Long-term effects of insulin Insulin has long-term actions via altered enzyme synthesis. An important anabolic hormone during fetal development Stimulates cell proliferation Implicated in somatic and visceral growth and development Mitogenic actions of insulin are of great concern in the development of insulin analogues, because these are intended for long-term use and because mammary tumours develop in rats given one long-acting insulin analogue known as B10-asp insulin. Diabetes Mellitus Chronic metabolic disorder characterised by a high blood glucose concentration hyperglycaemia fasting plasma glucose > 7.0 mmol/l, plasma glucose > 11.1 mmol/l 2 hrs postprandial Caused by insulin deficiency, often combined with insulin resistance. It’s a Communication Breakdown Diabetes is often described as “starvation in the midst of plenty” Extracellular glucose is abundant but the missing insulin causes: Pancreas cannot says to cells to “take glucose in” Muscle cells say “we cannot make glycogen” Hepatic cells think everyone’s starving “let’s make more glucose” Fat cells “let’s burn fat” Then… Threshold for renal glucose reabsorption exceeded - glycosuria (sugar in urine) Glycosuria causes osmotic diuresis – polyuria Polyuria results in dehydration, thirst & increased drinking - polydipsia No insulin - muscle wasting Diabetic ketoacidosis (DKA) due to breakdown of fat in DM1 - emergency Types of Diabetes Type 1 Autoimmune destruction of B cells - absolute deficiency of insulin. Usually onset young (children or adolescent) notobese Type 2 Accompanied both by insulin resistance Impaired insulin secretion later. Associated with obesity and usually present in adult life Complications of DM Macrovascular disease Due to dysfunction vascular endothelium ○ Oxygen-derived free radicals ○ Advanced glycation end (AGE) products Accelerated atheroma & thrombotic complication Microvascular disease Retina – Blindness, Glaucoma Kidneys - DM commonest cause of chronic renal failure (prevented by ACE & ARB) Peripheral nerve damage - Diabetic neuropathy caused by active metabolites of glucose by aldose reductase Treatment overview Type 1 Normalizing plasma glucose prevents diabetic complications. Type 2 Optimal control of BG rarely achieved Tight glucose control do not give as much benefit as in Type 1 - important in preventing microvascular complications Diet and increased exercise important Insulin Insulin used to be porcine or bovine but is now almost entirely human (made by recombinant DNA technology) Porcine and bovine insulins differ from human insulin in their amino acid sequence, and are liable to elicit an immune response. Pharmacokinetics Insulin is destroyed in the gastrointestinal tract, and must be given parenterally Subcutaneous Intravenous Occasionally intramuscularly in emergencies. Not currently used Inhaled insulin - not cost effective Intranasal insulin – 2010? Oral insulin – 2011? Insulin Administration Pharmacokinetics Different formulations vary in timing, peak effect and duration of action Soluble insulin – rapid and short Less soluble insulin (Insulin + protamine/zinc) – longer acting Isophane insulin Mixtures of different forms in fixed proportions are available Comparison of Human Insulins and Analogues Insulin Preparations Onset of Action Duration of Action Peak Lispro/Aspart 5-15 minutes 1-2 hours 3-5 hours Human Regular 30-60 minutes 2-4 hours 4-8 hours Human NPH/Lente 1-4 hours 4-12 hours 10-20 hours Human Ultralente 6-8 hours Unpredictable 16-20 hours Glargine 2-3 hours Flat ~24 hours The time course of action of any insulin may vary in different individuals, or at different times in the same individual. Because of this variation, time periods indicated here should be considered general guidelines only. 6- Unwanted effects Hypoglycaemia Treated with taking a sweet drink or snack Rebound hyperglycaemia - Somogyi effect Follows insulin-induced hypoglycaemia in early morning before breakfast Causes release of counter-regulatory hormones. What would you do? Allergy to human insulin - rare Oral Hypoglycemics Biguanides Metformin Sulfonylureas and other drugs that stimulate insulin secretion Tolbutamide, Glibenclamide, Nateglinide Thiazolidinediones Rosiglitazone, Pioglitazone α-Glucosidase inhibitor Acarbose Biguanides Sulfonylureas Thiazolidinediones α-Glucosidase inhibitor Biguanides - Metformin Biguanides lower blood glucose by mechanisms that are complex and incompletely understood. Increase glucose uptake and utilisation in skeletal muscle (reduce insulin resistance) Reduce hepatic glucose production Does not cause hypoglycaemia Reduces LDL and VLDL Half-life of about 3 hours and is excreted unchanged in the urine Metformin – Unwanted effects GI disturbance – anorexia, diarrhoea, nausea usually transient Lactic acidosis Contraindicated in patients with Renal disease Hepatic disease Hypoxic pulmonary disease Heart failure Shock Pregnancy Long-term use may interfere with absorption of vitamin B12 Metformin - Clinical Uses Does not stimulate appetite - decreases appetite First-line in obese Type 2 DM patients It can be combined with sulfonylureas, glitazones or insulin Prevent onset Biguanides Sulfonylureas Thiazolidinediones α-Glucosidase inhibitor Sulfonylureas The sulfonylureas were developed following the chance observation that a sulfonamide derivative (used to treat typhoid) caused hypoglycaemia Sulfonylureas - MOA Principal action of sulfonylureas is on B cells: Stimulating insulin secretion High-affinity receptors for sulfonylureas are present on the KATP channels Block by sulfonylurea drugs of KATP channel activation causes depolarisation, Ca2+ entry and insulin secretion. Sulfonylureas – Pharmacokinetics Well absorbed orally Most reach peak plasma concentrations within 2-4 hours All bind strongly to plasma albumin and are implicated in interactions with other drugs. Most sulfonylureas (or their active metabolites) are excreted in the urine Cross the placenta and enter breast milk Drug Relative potencya Duration of action and (half-life) (hours) Pharmacokinetic aspectsb General comments Tolbutamide 1 6-12 (4) Some converted in liver to weakly active hydroxytolbutamide; some carboxylated to inactive compound. Renal excretion. A safe drug; least likely to cause hypoglycaemia. May decrease iodide uptake by thyroid. Contraindicated in liver failure. Glibenclamidec 150 18-24 (10) Some is oxidised in the liver to moderately active products and is excreted in urine; 50% is excreted unchanged in the faeces. May cause hypoglycaemia. The active metabolite accumulates in renal failure. Glipizide 100 16-24 (7) Peak plasma levels in 1 hour. May cause Most is metabolised in the liver to hypoglycaemia. inactive products, which are excreted Has diuretic action. Only inactive products accumulate in renal failure. in urine; 12% is excreted in faeces Sulfonylurea - Unwanted effects Hypoglycaemia – can be severe & prolonged Stimulates appetite – causing weight gain GI upset Allergic skin rashes can occur Bone marrow damage rare – can be severe Avoid in post-myocardial infarction patient Sulfonylurea - Drug Interactions Drugs that augment hypoglycaemic effect, due to competition with CYP2C9 & albumin binding NSAIDs Coumadin Alcohol MAO inhibitors Antibacterial – sulfonamides, trimethoprim & chloramphenical Uricosuric drugs – sulfinpyrazone Antifungals Agents that decrease the action of sulfonylureas on blood glucose include high doses of thiazide diuretics and corticosteroids. Other Insulin Secretagogues Repaglinide and Nateglinide Stimulating insulin By blocking the sulfonylurea receptor on KATP channels in pancreatic B cells Rapid absorption (55 minutes after an oral dose) Elimination (half-life approximately 3 hours), lead to short duration of action. Biguanides Sulfonylureas Thiazolidinediones α-Glucosidase inhibitor Thiazolidinediones – PPARγagonist Thiazolidinediones (or glitazones) were developed following the chance observation that a clofibrate analogue, ciglitazone, which was being screened for effects on lipids, unexpectedly lowered blood glucose Glitazones have serious side-effects Ciglitazone caused liver toxicity, Troglitazone – liver toxicity take off market (90 cases of liver failure (70 resulting in death or transplantation) before it was withdrawn in March, 2000) Rosiglitazone - 41,000 and 205,000 excess casualties may have resulted from cardiovascular events Pioglitazone – Bladder cancer risk? Glitazones - MOA Glitazones are exogenous agonists that Bind to a nuclear receptor the peroxisome proliferator-activated receptor-γ (PPARγ agonist) producing products important in insulin signaling e.g Glut-4. Differentiation of adipocytes Increases lipogenesis – update FA & glucose Promotes Na+ reabsorption Glitazones - Effects Maximum effect being achieved after only 1-2 months of treatment Reduce hepatic glucose output Increase glucose uptake into muscle Reductions in circulating insulin and free fatty acids – Triglycerides Weight gain 1-4 kg due to fluid retention stabilizing in 6-12 mths Anemia due to haemodilution Glitazones - Pharmacokinetics Rosiglitazone and Pioglitazone Rapidly and nearly completely absorbed Peak plasma concentration <2 hrs 99% plasma protein bound Elimination half-life <7 hrs parent drug Metabolised to metabolites with longer half-lives by CYP3A4(150hrs) - urine CYP2C(24hrs) - bile Glitazones – Unwanted effects Hepatic toxicity Weight gain Fluid retention – precipitate/worsen heart failure Headache, fatigue, GI disturbance Contraindicated in pregnant/breastfeeding women & in children. α-Glucosidase inhibitors - Acarbose An inhibitor of intestinal α-glucosidase Delays carbohydrate absorption, reduce post-prandial blood glucose Unwanted effects - flatulence, diarrhoea, abdominal pain & bloating May be coadministered with metformin Summary Biguanides (e.g. metformin): have complex peripheral actions in the presence of residual insulin, increasing glucose uptake in striated muscle and inhibiting hepatic glucose output and intestinal glucose absorption cause anorexia and encourage weight loss can be combined with sulfonylureas. Sulfonylureas and other drugs that stimulate insulin secretion (e.g. tolbutamide, glibenclamide, nateglinide): can cause hypoglycaemia (which stimulates appetite and leads to weight gain) are effective only if Bcells are functional block ATP-sensitive potassium channels in Bcells are well tolerated but promote weight gain. Summary Thiazolidinediones (e.g. rosiglitazone, pioglitazone) increase insulin sensitivity and lower blood glucose in type 2 diabetes can cause weight gain and oedema are peroxisome proliferator-activated receptor-γ (a nuclear receptor) agonists. α-Glucosidase inhibitor: acarbose reduces carbohydrate absorption causes flatulence and diarrhoea. References Lessons from the glitazones: a story of drug development Second time a farce, Rosiglitazone & Regulators http://www.fda.gov/Safety/MedWatch/Safet yInformation/SafetyAlertsforHumanMedical Products/ucm226257.htm Insulin Therapy – Thomas Repas DO Rang et al (2007) Rang & Dale’s Pharmacology 6th Ed.