* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pathology of the Integumentary System
Survey
Document related concepts
Transcript
The Somatic Arts and Sciences Institute
www.sasionline.com
3-Hours Continuing Education
SASI Course: APR002/APS006
Pathology of the
Integumentary System
The Somatic Arts and Sciences Institute
P.O. Box 3181
Merced, CA 95344
(209) 777-6305
www.sasionline.com
NCBTMB Approved
Provider #450872-08
Table of Contents
Instructions…………………………………………………………………………………………………..……… 3
Educational Objectives……………………………………………………………………….………………….… 3
Chapter 1: Review of the Integumentary System………...………………………………………..…………….4
Chapter 2: Pathology of the Integumentary System..……....……..………………………………………..….12
Summary of Pathology of the Integumentary System………………………………………………………...162
Course Completion: Certificate of Completion and Transcript…………………………………………….…163
Course Evaluation and Errata.………………………………………………………………….……….………164
Help and Technical Support Line……………………………………………………………………….….……164
Bibliography (Sources)…………………………………………………………………………………………...165
2
Pathology of the Integumentary System
Instructions
Thanks for downloading this Somatic Arts and Sciences continuing
education course. You are looking at the text version of the course, which
can be printed out if you like.
Target Audience
This continuing education course has been designed to meet the
educational needs of massage therapists.
Degree of Difficulty
Beginner/Entry Level
Course Description
This course will enable the massage practitioner to identify the symptoms
of several conditions of the skin that could be encountered in the course of
a massage therapy career.
Educational Objectives
Upon completion of this home study continuing education course, the
massage practitioner should be able to:
Define the terms Psoriasis, Eczema and Fungus.
List the suspected causes of Psoriasis, Eczema and Fungus.
Describe what symptoms to expect from clients with Psoriasis,
Eczema and Fungus.
List at least 10 other skin conditions mentioned in this course that
could be encountered by a massage therapist.
3
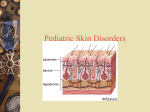
Chapter 1: Review of the Integumentary System
The integumentary system is an organ system consisting of the skin, hair,
nails, and exocrine glands. The skin is only a few millimeters thick yet is by
far the largest organ in the body. The average person’s skin weighs 10
pounds and has a surface area of almost 20 square feet. Skin forms the
body’s outer covering and forms a barrier to protect the body from
chemicals, disease, UV light, and physical damage.
Hair and nails extend from the skin to reinforce the skin and protect it from
environmentaldamage. The exocrine glands of the integumentary system
produce sweat, oil, and wax to cool, protect, and moisturize the skin’s
surface.
Anatomy of the Integumentary System
Epidermis
The epidermis is the most superficial layer of the skin that covers almost
the entire body surface. The epidermis rests upon and protects the deeper
and thicker dermis layer of the skin. Structurally, the epidermis is only
about a tenth of a millimeter thick but is made of 40 to 50 rows of stacked
squamous epithelial cells. The epidermis is an avascular region of the
body, meaning that it does not contain any blood or blood vessels. The
cells of the epidermis receive all of their nutrients via diffusion of fluids from
the dermis.
The epidermis is made of several specialized types of cells. Almost 90% of
the epidermis is made of cells known as keratinocytes. Keratinocytes
develop from stem cells at the base of the epidermis and begin to produce
and store the protein keratin. Keratin makes the keratinocytes very tough,
scaly and water-resistant. At about 8% of epidermal cells, melanocytes
form the second most numerous cell type in the epidermis. Melanocytes
produce the pigment melanin to protect the skin from ultraviolet radiation
and sunburn. Langerhans cells are the third most common cells in the
epidermis and make up just over 1% of all epidermal cells. Langerhans
cells’ role is to detect and fight pathogens that attempt to enter the body
through the skin. Finally, Merkel cells make up less than 1% of all
epidermal cells but have the important function of sensing touch. Merkel
cells form a disk along the deepest edge of the epidermis where they
connect to nerve endings in the dermis to sense light touch.
4
The epidermis in most of the body is arranged into 4 distinct layers. In the
palmar surface of the hands and plantar surface of the feet, the skin is
thicker than in the rest of the body and there is a fifth layer of epidermis.
The deepest region of the epidermis is the stratum basale, which contains
the stem cells that reproduce to form all of the other cells of the epidermis.
The cells of the stratum basale include cuboidal keratinocytes,
melanocytes, and Merkel cells. Superficial to stratum basale is the stratum
spinosum layer where Langerhans cells are found along with many rows of
spiny keratinocytes. The spines found here are cellular projections called
desmosomes that form between keratinocytes to hold them together and
resist friction. Just superficial to the stratum spinosum is the stratum
granulosum, where keratinocytes begin to produce waxy lamellar granules
to waterproof the skin. The keratinocytes in the stratum granulosum are so
far removed from the dermis that they begin to die from lack of nutrients. In
the thick skin of the hands and feet, there is a layer of skin superficial to the
stratum granulosum known as the stratum lucidum. The stratum lucidum is
made of several rows of clear, dead keratinocytes that protect the
underlying layers. The outermost layer of skin is the stratum corneum. The
stratum corneum is made of many rows of flattened, dead keratinocytes
that protect the underlying layers. Dead keratinocytes are constantly being
shed from the surface of the stratum corneum and being replaced by cells
arriving from the deeper layers.
Dermis
The dermis is the deep layer of the skin found under the epidermis. The
dermis is mostly made of dense irregular connective tissue along with
nervous tissue, blood, and blood vessels. The dermis is much thicker than
the epidermis and gives the skin its strength and elasticity. Within the
dermis there are two distinct regions: the papillary layer and the reticular
layer.
The papillary layer is the superficial layer of the dermis that borders on the
epidermis. The papillary layer contains many finger-like extensions called
dermal papillae that protrude superficially towards the epidermis. The
dermal papillae increase the surface area of the dermis and contain many
nerves and blood vessels that are projected toward the surface of the skin.
Blood flowing through the dermal papillae provide nutrients and oxygen for
the cells of the epidermis. The nerves of the dermal papillae are used to
feel touch, pain, and temperature through the cells of the epidermis.
5
The deeper layer of the dermis, the reticular layer, is the thicker and
tougher part of the dermis. The reticular layer is made of dense irregular
connective tissue that contains many tough collagen and stretchy elastin
fibers running in all directions to provide strength and elasticity to the skin.
The reticular layer also contains blood vessels to support the skin cells and
nerve tissue to sense pressure and pain in the skin.
Hypodermis
Deep to the dermis is a layer of loose connective tissues known as the
hypodermis, subcutis, or subcutaneous tissue. The hypodermis serves as
the flexible connection between the skin and the underlying muscles and
bones as well as a fat storage area. Areolar connective tissue in the
hypodermis contains elastin and collagen fibers loosely arranged to allow
the skin to stretch and move independently of its underlying structures.
Fatty adipose tissue in the hypodermis stores energy in the form of
triglycerides. Adipose also helps to insulate the body by trapping body heat
produced by the underlying muscles.
Hair
Hair is an accessory organ of the skin made of columns of tightly packed
dead keratinocytes found in most regions of the body. The few hairless
parts of the body include the palmar surface of the hands, plantar surface
of the feet, lips, labia minora, and glans penis. Hair helps to protect the
body from UV radiation by preventing sunlight from striking the skin. Hair
also insulates the body by trapping warm air around the skin.
The structure of hair can be broken down into 3 major parts: the follicle,
root, and shaft. The hair follicle is a depression of epidermal cells deep into
the dermis. Stem cells in the follicle reproduce to form the keratinocytes
that eventually form the hair while melanocytes produce pigment that gives
the hair its color. Within the follicle is the hair root, the portion of the hair
below the skin’s surface. As the follicle produces new hair, the cells in the
root push up to the surface until they exit the skin. The hair shaft consists of
the part of the hair that is found outside of the skin.
The hair shaft and root are made of 3 distinct layers of cells: the cuticle,
cortex, and medulla. The cuticle is the outermost layer made of
keratinocytes. The keratinocytes of the cuticle are stacked on top of each
other like shingles so that the outer tip of each cell points away from the
body. Under the cuticle are the cells of the cortex that form the majority of
6
the hair’s width. The spindle-shaped and tightly packed cortex cells contain
pigments that give the hair its color. The innermost layer of the hair, the
medulla, is not present in all hairs. When present, the medulla usually
contains highly pigmented cells full of keratin. When the medulla is absent,
the cortex continues through the middle of the hair.
Nails
Nails are accessory organs of the skin made of sheets of hardened
keratinocytes and found on the distal ends of the fingers and toes.
Fingernails and toenails reinforce and protect the end of the digits and are
used for scraping and manipulating small objects. There are 3 main parts of
a nail: the root, body, and free edge. The nail root is the portion of the nail
found under the surface of the skin. The nail body is the visible external
portion of the nail. The free edge is the distal end portion of the nail that
has grown beyond the end of the finger or toe.
Nails grow from a deep layer of epidermal tissue known as the nail matrix,
which surrounds the nail root. The stem cells of the nail matrix reproduce to
form keratinocytes, which in turn produce keratin protein and pack into
tough sheets of hardened cells. The sheets of keratinocytes form the hard
nail root that slowly grows out of the skin and forms the nail body as it
reaches the skin’s surface. The cells of the nail root and nail body are
pushed toward the distal end of the finger or toe by new cells being formed
in the nail matrix. Under the nail body is a layer of epidermis and dermis
known as the nail bed. The nail bed is pink in color due to the presence of
capillaries that support the cells of the nail body. The proximal end of the
nail near the root forms a whitish crescent shape known as the lunula
where a small amount of nail matrix is visible through the nail body. Around
the proximal and lateral edges of the nail is the eponychium, a layer of
epithelium that overlaps and covers the edge of the nail body. The
eponychium helps to seal the edges of the nail to prevent infection of the
underlying tissues.
Sudoriferous Glands
Sudoriferous glands are exocrine glands found in the dermis of the skin
and commonly known as sweat glands. There are 2 major types of
sudoriferous glands: eccrine sweat glands and apocrine sweat glands.
Eccrine sweat glands are found in almost every region of the skin and
produce a secretion of water and sodium chloride. Eccrine sweat is
7
delivered via a duct to the surface of the skin and is used to lower the
body’s temperature through evaporative cooling.
Apocrine sweat glands are found in mainly in the axillary and pubic regions
of the body. The ducts of apocrine sweat glands extend into the follicles of
hairs so that the sweat produced by these glands exits the body along the
surface of the hair shaft. Apocrine sweat glands are inactive until puberty,
at which point they produce a thick, oily liquid that is consumed by bacteria
living on the skin. The digestion of apocrine sweat by bacteria produces
body odor.
Sebaceous Glands
Sebaceous glands are exocrine glands found in the dermis of the skin that
produce an oily secretion known as sebum. Sebaceous glands are found in
every part of the skin except for the thick skin of the palms of the hands
and soles of the feet. Sebum is produced in the sebaceous glands and
carried through ducts to the surface of the skin or to hair follicles. Sebum
acts to waterproof and increase the elasticity of the skin. Sebum also
lubricates and protects the cuticles of hairs as they pass through the
follicles to the exterior of the body.
Ceruminous Glands
Ceruminous glands are special exocrine glands found only in the dermis of
the ear canals. Ceruminous glands produce a waxy secretion known as
cerumen to protect the ear canals and lubricate the eardrum. Cerumen
protects the ears by trapping foreign material such as dust and airborne
pathogens that enter the ear canal. Cerumen is made continuously and
slowly pushes older cerumen outward toward the exterior of the ear canal
where it falls out of the ear or is manually removed.
Physiology of the Integumentary System
Keratinization
Keratinization, also known as cornification, is the process of keratin
accumulating within keratinocytes. Keratinocytes begin their life as
offspring of the stem cells of the stratum basale. Young keratinocytes have
a cuboidal shape and contain almost no keratin protein at all. As the stem
cells multiply, they push older keratinocytes towards the surface of the skin
and into the superficial layers of the epidermis. By the time keratinocytes
reach the stratum spinosum, they have begun to accumulate a significant
8
amount of keratin and have become harder, flatter, and more water
resistant. As the keratinocytes reach the stratum granulosum, they have
become much flatter and are almost completely filled with keratin. At this
point the cells are so far removed from the nutrients that diffuse from the
blood vessels in the dermis that the cells go through the process of
apoptosis. Apoptosis is programmed cell death where the cell digests its
own nucleus and organelles, leaving only a tough, keratin-filled shell
behind. Dead keratinocytes moving into the stratum lucidum and stratum
corneum are very flat, hard, and tightly packed so as to form a keratin
barrier to protect the underlying tissues.
Temperature Homeostasis
Being the body’s outermost organ, the skin is able to regulate the body’s
temperature by controlling how the body interacts with its environment. In
the case of the body entering a state of hyperthermia, the skin is able to
reduce body temperature through sweating and vasodilation. Sweat
produced by sudoriferous glands delivers water to the surface of the body
where it begins to evaporate. The evaporation of sweat absorbs heat and
cools the body’s surface. Vasodilation is the process through which smooth
muscle lining the blood vessels in the dermis relax and allow more blood to
enter the skin. Blood transports heat through the body, pulling heat away
from the body’s core and depositing it in the skin where it can radiate out of
the body and into the external environment.
In the case of the body entering a state of hypothermia, the skin is able to
raise body temperature through the contraction of arrector pili muscles and
through vasoconstriction. The follicles of hairs have small bundles of
smooth muscle attached to their base called arrector pili muscles. The
arrector pili form goose bumps by contracting to move the hair follicle and
lifting the hair shaft upright from the surface of the skin. This movement
results in more air being trapped under the hairs to insulate the surface of
the body. Vasoconstriction is the process of smooth muscles in the walls of
blood vessels in the dermis contracting to reduce the flood of blood to the
skin. Vasoconstriction permits the skin to cool while blood stays in the
body’s core to maintain heat and circulation in the vital organs.
Vitamin D Synthesis
Vitamin D, an essential vitamin necessary for the absorption of calcium
from food, is produced by ultraviolet (UV) light striking the skin. The stratum
basale and stratum spinosum layers of the epidermis contain a sterol
9
molecule known as 7-dehydrocholesterol. When UV light present in
sunlight or tanning bed lights strikes the skin, it penetrates through the
outer layers of the epidermis and strikes some of the molecules of 7dehydrocholesterol, converting it into vitamin D3. Vitamin D3 is converted
in the kidneys into calcitriol, the active form of vitamin D.
Protection
The skin provides protection to its underlying tissues from pathogens,
mechanical damage, and UV light. Pathogens, such as viruses and
bacteria, are unable to enter the body through unbroken skin due to the
outermost layers of epidermis containing an unending supply of tough,
dead keratinocytes. This protection explains the necessity of cleaning and
covering cuts and scrapes with bandages to prevent infection. Minor
mechanical damage from rough or sharp objects is mostly absorbed by the
skin before it can damage the underlying tissues. Epidermal cells
reproduce constantly to quickly repair any damage to the skin. Melanocytes
in the epidermis produce the pigment melanin, which absorbs UV light
before it can pass through the skin. UV light can cause cells to become
cancerous if not blocked from entering the body.
Skin Color
Human skin color is controlled by the interaction of 3 pigments: melanin,
carotene, and hemoglobin. Melanin is a brown or black pigment produced
by melanocytes to protect the skin from UV radiation. Melanin gives skin its
tan or brown coloration and provides the color of brown or black hair.
Melanin production increases as the skin is exposed to higher levels of UV
light resulting in tanning of the skin. Carotene is another pigment present in
the skin that produces a yellow or orange cast to the skin and is most
noticeable in people with low levels of melanin. Hemoglobin is another
pigment most noticeable in people with little melanin. Hemoglobin is the red
pigment found in red blood cells, but can be seen through the layers of the
skin as a light red or pink color. Hemoglobin is most noticeable in skin
coloration during times of vasodilation when the capillaries of the dermis
are open to carry more blood to the skin’s surface.
Cutaneous Sensation
The skin allows the body to sense its external environment by picking up
signals for touch, pressure, vibration, temperature, and pain. Merkel disks
in the epidermis connect to nerve cells in the dermis to detect shapes and
textures of objects contacting the skin. Corpuscles of touch are structures
10
found in the dermal papillae of the dermis that also detect touch by objects
contacting the skin. Lamellar corpuscles found deep in the dermis sense
pressure and vibration of the skin. Throughout the dermis there are many
free nerve endings that are simply neurons with their dendrites spread
throughout the dermis. Free nerve endings may be sensitive to pain,
warmth, or cold. The density of these sensory receptors in the skin varies
throughout the body, resulting in some regions of the body being more
sensitive to touch, temperature, or pain than other regions.
Excretion
In addition to secreting sweat to cool the body, eccrine sudoriferous glands
of the skin also excrete waste products out of the body. Sweat produced by
eccrine sudoriferous glands normally contains mostly water with many
electrolytes and a few other trace chemicals. The most common
electrolytes found in sweat are sodium and chloride, but potassium,
calcium, and magnesium ions may be excreted as well. When these
electrolytes reach high levels in the blood, their presence in sweat also
increases, helping to reduce their presence within the body. In addition to
electrolytes, sweat contains and helps to excrete small amounts of
metabolic waste products such as lactic acid, urea, uric acid, and ammonia.
Finally, eccrine sudoriferous glands can help to excrete alcohol from the
body of someone who has been drinking alcoholic beverages. Alcohol
causes vasodilation in the dermis, leading to increased perspiration as
more blood reaches sweat glands. The alcohol in the blood is absorbed by
the cells of the sweat glands, causing it to be excreted along with the other
components of sweat.
11
Chapter 2 Pathology of the Integumentary System
Acanthoma, Clear Cell
Clear cell acanthoma (also known as "Acanthome cellules claires of Degos
and Civatte," "Degos acanthoma," and "Pale cell acanthoma") is a benign
clinical and histological lesion initially described as neoplastic, which some
authors now regard as a reactive dermatosis. It usually presents as a moist
solitary firm, brown-red, well-circumscribed, 5 mm to 2 cm nodule or plaque
on the lower extremities of middle-aged to elderly individuals The lesion
has a crusted, scaly peripheral collarette and vascular puncta on the
surface. It is characterized by slow growth, and may persist for years. The
clinical differential diagnosis includes: dermatofibroma, inflamed seborrheic
keratosis, pyogenic granuloma, basal cell carcinoma, squamous cell
carcinoma, verruca vulgaris, psoriatic plaque, and melanoma.
Clear cell acanthoma is characterized by a sharply demarcated
psoriasiform epidermal hyperplasia composed of a proliferation of slightly
enlarged keratinocytes, and basal cells with pale-staining glycogen-rich
cytoplasm, mild spongiosis and scattered neutrophils, which may form
small intraepidermal microabscesses. Oedematous dermal papillae are
typically seen with increased vascularity and a mixed inflammatory infiltrate
including lymphocytes, plasma cells and neutrophils1.
1
Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
12
Acanthosis nigricans
Acanthosis nigricans is a brown to black, poorly defined, velvety
hyperpigmentation of the skin. It is usually found in body folds, such as the
posterior and lateral folds of the neck, the armpits, groin, navel, forehead,
and other areas.
Acanthosis nigricans is conventionally divided into benign and malignant
forms, although may be divided into syndromes according to cause.
Benign
This may include obesity-related, hereditary, and endocrine forms of
acanthosis nigricans.
Malignant
This may include forms that are associated with tumour products and
insulin-like activity, or tumour necrosis factor.
An alternate classification system still used to describe acanthosis
nigricans was proposed in 1994 by dermatologist Schwartz. This
classification system delineates acanthosis nigricans syndromes according
to their associated syndromes, including benign and malignant forms,
forms associated with obesity and drugs, acral acanthosis nigricans,
unilateral acanthosis nigricans, and mixed and syndromic forms.
Acanthosis nigricans may present with thickened, relatively darker areas of
skin on the neck, armpit and in skin folds.
It typically occurs in individuals younger than age 40, may be genetically
inherited, and is associated with obesity or endocrinopathies, such as
hypothyroidism, acromegaly, polycystic ovary disease, insulin-resistant
diabetes, or Cushing's disease.
Endocrine syndromes associated with acanthosis nigricans can develop in
many conditions, particularly states with insulin resistance, such as
diabetes mellitus excess circulating androgens, particularly Cushing's
disease, acromegaly, polycystic ovarian disease Addison's disease and
hypothyroidism.
13
Rare diseases, including pinealoma, leprechaunism, lipotrophic diabetes,
pineal hyperplasia syndrome, pituitary basophilism, ovarian hyperthecosis,
stromal luteoma, ovarian dermoid cysts, Prader-Willi syndrome, and
Alstrom syndrome.
Acanthosis nigricans associated with endocrine dysfunction is more
insidious in its onset, is less widespread, and the patients are often
concurrently obese.
The majority of cases of acanthosis nigricans are associated with obesity
and otherwise idiopathic. This is likely because of insulin resistance, and
more likely to occur in darker-skinned persons. This is also known as
"Pseudo-Acanthosis Nigricans", or "Type 3 Acanthosis Nigricans".
Acanthosis nigricans has been linked to the use of nicotinic acid,
glucocorticoid use, COCP, growth hormone therapy, and stilbesterol.<.
This is also known as Type 4 Acanthosis nigricans.
Familial acanthosis may arise as a result of an autosomal dominant trait,
presenting at birth or developing during childhood. This is also known as
Acanthosis nigricans type 1.
Acral Acanthotic Anomaly refers to a variant of acanthosis nigricans limited
to the elbows, knees, knuckles and dorsal surfaces of the feet, in the
absence of any other findings, in otherwise healthy individuals. While the
etiology remains unknown, its presence does not suggest a likelihood of
malignancy.
Malignant acanthosis nigricans refers to acanthosis nigricans occurring as
a paraneoplastic syndrome associated with a cancer. Malignant acanthosis
nigricans
is
most-commonly
associated
with
gastrointestinal
adenocarcinomas, as well as genitourinary cancers such as those of the
prostate, breast, and ovary. Other cancers, such as those of the lung,
stomach, and lymphoma, are occasionally associated with acanthosis
nigricans.
This form of acanthosis nigricans is more likely to involve mucous
membranes (25-50% of cases) This variant is also known as Acanthosis
nigricans type I. Malignant acanthosis nigricans that may either precede
(18%), accompany (60%), or follow (22%) the onset of an internal cancer.
14
Malignancy-associated acanthosis nigricans is usually rapid in onset and
may be accompanied by skin tags, multiple seborrheic keratoses, or tripe
palms.
The pathogenesis of acanthosis nigricans is poorly understood, and likely
to relate to an interplay of factors, including insulin-mediated activation of
ILGF receptors on keratinocytes, and increased growth factor levels.
Factors involved in the development of acanthosis nigricans include:
Increased circulating insulin. This activates keratinocyte ILGF receptors,
particularly IGF-1. At high concentrations, insulin may also displace IGF-1
from IGFBP. Increased circulating IGF may lead to keratinocyte and dermal
fibroblast proliferation.
Fibroblast growth factor. Hereditary variants are associated with FGFR
defects.
Increased TGF, which appears to be the mechanism for malignancyassociated acanthosis nigricans. TGF acts on epidermal tissue via the
EGFR.
In conjunction with increased end levels of ILGF, it is likely that perspiration
and friction may be necessary predeterminants for lesions.
Acanthosis nigricans is typically diagnosed clinically. A skin biopsy may be
needed in unusual cases. If no clear cause of acanthosis nigricans is
obvious, it may be necessary to search for one. Blood tests, an endoscopy,
or x-rays may be required to eliminate the possibility of diabetes or cancer
as the cause.
On biopsy, hyperkaratosis, epidermal folding, leukocyte infltration, and
melanocyte proliferation may be seen.
Acanthosis nigricans should be distinguished from the Casal collar
appearing in pellegra.
Acanthosis nigricans is likely to improve in circumstances where a known
cause is removed. For example, obesity-related acanthosis nigricans will
improve with weight loss, and drug-induced acanthosis nigricans is likely to
15
resolve when the drug is ceased. Hereditary variants may or may not fade
with age, and malignancy-associated variants may, after a malignancy is
removed, fade.
People with acanthosis nigricans should be screened for diabetes and,
although rare, cancer. Controlling blood glucose levels through exercise
and diet often improves symptoms. Acanthosis nigricans maligna may
resolve if the causative tumor is successfully removed2.
2
Habif, Thomas P. (2009). Clinical dermatology (5th ed. ed.). Edinburgh: Mosby. ISBN 978-0-7234-3541-9.
16
Acne (Acne Vulgaris)
The skin manifestation of pilosebaceous unit or follicular duct plugging with
excess sebum, cell debris, Propionibacterium acnes, staphylococcal
bacteria, and perspiration.
Whiteheads, blackheads, pimples, and larger bumps of the face, chest,
and/or back. Open and closed comedones of any facial areas including
ears, chest, and/or back. Red papules and/or pustules of face, chest,
and/or back. Cystic nodules of any or all of the same areas. Occasional pit
or small crater depression. Scars, usually on face or back. Rare keloid
scars of jaw, neck, and/or back and chest.
Nerve energy or physical factors directly stimulate sebaceous glands. This
increases size and sebum production which becomes too much for the
follicular ducts. They plug with the excess sebum, cell debris from the duct
and skin, and bacteria. A simple oil plug is either open or closed. An open
duct oxidizes the oil and it turns dark, hence a blackhead. If the duct is
covered with a thin membrane the oil dries white, hence whiteheads.
Mixing with the microbes, cell debris or other chemicals yields red papules
and pustules. Cysts are formed when the plug is so tight that the duct
expands and breaks with continued sebum production and the body forms
a wall around the collection.
Needless to say, Acne Vulgaris does not refer to the simple outbreak of
pimples that is commonly associated with puberty and hormone changes.
Acne conglobata
Acne conglobata is a highly inflammatory disease presenting with
comedones, nodules, abscesses, and draining sinus tracts3.
This condition generally begins between the ages of 18 and 30. It usually
persists for a very long time, and often until the patient is around 40 years
old. Although it often occurs where there is already an active acne problem,
it can also happen to people whose acne has subsided. Although the cause
of this type of acne is unknown, it is associated with testosterone and thus
appears mainly in men. It can be caused by anabolic steroid abuse and
sometimes appears in men after stopping testosterone therapy. It can also
happen to someone who has a tumour that is releasing large amounts of
3
Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). Page 685. McGraw-Hill. ISBN 0-07-138076-0.
17
androgens, or to people in remission from autoimmune diseases, such as
leukemia. In certain persons, the condition may be triggered by exposure to
aromatic hydrocarbons or ingestion of halogens4.
This condition presents with blackheads appearing around the face, neck,
chest, upper arms and buttocks in groups of two or three. The pimples form
around the blackheads. They are large and engorged with fluid, and may
be sensitive to touch. They remain for a while and continue to grow and fill
with pus until they finally rupture. After the lesion has drained, it fills up
again. After they rupture, several nodules can fuse together to form larger
shapes. The lesions remain for a long time. They form a scab in the centre
but they continue to spread outwards. When the lesions do eventually heal,
they leave scars that can be the usual type of acne scar (atrophic) or can
be the raised bump normally left behind by a burn or a cut (keloidal).
The most common treatment is the acne medication isotretinoin. It may be
combined with prednisone. Dapsone, which is normally used to treat
leprosy, is a riskier medication but is sometimes prescribed in cases where
the normal therapy is ineffectual. Antibiotics such as tetracycline or
erythromycin may also be prescribed. An alternative option is to treat with
carbon dioxide laser therapy, followed by topical tretinoin therapy. Surgery
may be necessary to remove large nodules. Alternatively, nodules can be
injected with triamcinolone5.
Acne cosmetica
Acne cosmetica is a term referring to acne caused by or aggravated by
cosmetics6. The mechanism was presumably a chemically induced
plugging of the pilosebaceous orifice. This was a significant problem for
dermatologists in the 1970s and 1980s, but with the improved formulations
produced by cosmetic chemists over the past thirty years, this is now a
relatively rare diagnosis in daily practice.
The terms "non-comedogenic" and "non-acne(i)genic" appeared on
moisturizers and other cosmetic compounds as re-formulations were
introduced, sometimes associated with claims that the products were oilfree or water-based. Although early work produced lists of comedogenic
chemicals in various strengths and vehicles, it became apparent that the
4
Acne Conglobata http://emedicine.medscape.com/article/1072716-overview
Acne Conglobata Treatment & Management http://emedicine.medscape.com/article/1072716-treatment
6
Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
5
18
actual comedogenicity of a product could not be predicted from its
contents; rather the finished product itself needed to be use-tested.
The production of a low-grade folliculitis by some components of cosmetic
products has led to misdiagnosis on occasion.
People may not attribute their reactions to their cosmetics at first, but may
notice worsening symptoms after using certain face makeup, sunblock or
lip products.
Acne fulminans
Acne fulminans is a severe form of the skin disease, acne, which can occur
after unsuccessful treatment for another form of acne, acne conglobata.
The condition is thought to be an immunologically induced disease in which
elevated level of testosterone causes a rise in sebum and population of
Propionibacterium acnes bacteria. The increase in the amount of P acnesor
related antigens may trigger the immunologic reaction in some individuals
and lead to an occurrence of acne fulminans7. In addition to testosterone,
isotretinoin may also precipitate acne fulminans, possibly related to highly
increased levels of P acnesantigens in the patient's immune system. Acne
fulminans is a rare disease. Over the past several years, fewer cases of
this disease have occurred, possibly because of earlier and better
treatment of acne. Approximately 100 patients with acne fulminans have
been described8.
Acne fulminans begins as pain and inflammation in the joints. It eventually
progresses into a swelling of the lymph nodes located at the base of the
neck, causing inflexibility in the neck within weeks after the nodes swell.
This swelling will eventually decrease, but this decrease will be
accompanied by an increased inflammation and swelling of the joints, as
well as a complete loss of appetite, though these symptoms are often
ignored. After some time, the disease will cause an extreme loss of weight
and atrophy of the muscles, leading to the decline of physical abilities9.
Treatment should be sought immediately in order to avoid hospitalization. If
not treated, hospitalization for an extended period of time (usually two
weeks) is likely. During hospitalization, the patient is tested for signs of
7
Testosterone and anabolic steroids and acne fulminans. Arch Dermatol. 1989; 125(4):571-2 (ISSN: 0003-987X)
Case reports: acne fulminans in Marfan syndrome. J Drugs Dermatol. 2005; 4(4):501-5 (ISSN: 1545-9616)
9
Acne conglobata and arthritis. Arthritis Rheum. 1961; 4:632-5 (ISSN: 0004-3591)
8
19
system degradation, especially of the skeletal structure and the digestive
tract. By this time open sores will develop on the upper torso. Some will be
the size of dimes, others will be large enough to stick a couple fingers into.
They will crust up, causing cohesion to any fabric the sores touch, which is
extremely painful to remove. It is recommended to sleep on one's sides
until the cystic condition subsides, in order to avoid any uncomfortable
situations. Debridement and steroid therapy is preferred over antibiotics10.
Recurrent AF is extremely rare. Bone lesions typically resolve with
treatment, but residual radiographic changes, such as sclerosis and
hyperostosis, may remain. Scarring and fibrosis may result from this acute
inflammatory process.
The disease activates at the height of puberty, usually at around 13 years
of age. Acne fulminans predominantly affects young males aged 13 to 22
years with a history of acne.
Acne keloidalis nuchae
Acne keloidalis nuchae is a destructive scarring folliculitis that occurs
almost exclusively on the occipital scalp of people of African descent,
primarily men. This is mainly because men often cut their hair very low as
opposed to women, allowing the hair to prick the occipital scalp and upset
it. Acne keloidalis nuchae most commonly presents itself in individuals
aged 13 to 25.
Acne keloidalis nuchae (AKN) is a condition characterized by follicularbased papules and pustules that form hypertrophic or keloid-like scars.
AKN typically occurs on the occipital scalp and posterior neck and develops
almost exclusively in young, African-American men. The term acne
keloidalis nuchae is somewhat of a misnomer because the lesions do not
occur as a result of acne vulgaris, but rather a folliculitis.
Lesions initially manifest as mildly pruritic follicular-based papules and
pustules on the nape of the neck. Chronic folliculitis ultimately leads to
development of keloid-like plaques. AKN develops in hair bearing skin
areas, and broken hair shafts, tufted hairs, and ingrown hairs can be
identified within and at the margins of the plaques themselves. Lesions can
grow over time and become disfiguring and painful. In advanced cases,
10
Acne fulminans with synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) syndrome treated with infliximab. J Am Acad Dermatol. 2005;
52(5 Suppl 1):S118-20 (ISSN: 1097-6787)
20
abscesses and sinus tracts with purulent discharge may develop. Unlike
true acne vulgaris, comedones are not a common feature of AKN.
The exact etiology of AKN is unclear. It is thought that chronic irritation from
coarse, curly hairs in the skin leads to inflammation and development of
these lesions. This hypothesis is supported by the fact that close shaving
and chronic rubbing of the area by clothing or athletic gear make AKN
worse. In a study of 453 high school, college, and professional American
football players, 13.6% of African American athletes had acne keloidalis
nuchae, as opposed to none of the Caucasian athletes. It has also been
shown that men who have haircuts more frequently than once a month are
at higher risk of developing acne keloidalis nuchae11.
Pseudofolliculitis barbae (PFB) is a similar condition that occurs commonly
in African Americans. In PFB, it has been proposed that close shaving of
coarse, curved hairs facilitates the reentry of the free end of the hair into
the skin, which then invokes an acute inflammatory response.
While ingrowing hairs may account for small papules, they do not
sufficiently explain the progressive scarring alopecia that occurs in some
patients. These patients with scarring alopecia often exhibit recurrent crops
of small pustules and may have a condition akin to folliculitis decalvans.
Chronic low-grade bacterial infection, autoimmunity, and some types of
medication (eg, cyclosporine, diphenylhydantoin, carbamazepine) have
also been implicated in the pathogenesis in some patients12.
The initial process begins as acute perifollicular inflammation followed by
weakening of the follicular wall at the level of the lower infundibulum, the
isthmus, or both.
The naked hair shaft is then released into the surrounding dermis, which
acts as a foreign body and incites further acute and chronic granulomatous
inflammation. This process is clinically manifested by small follicular-based
papules and pustules.
Subsequently, fibroblasts deposit new collagen and fibrosis ensues.
11
Khumalo NP, Jessop S, Gumedze F, Ehrlich R. Hairdressing and the prevalence of scalp disease in African adults. Br J Dermatol. Nov
2007;157(5):981-8.
12
Grunwald MH, Ben-Dor D, Livni E, Halevy S. Acne keloidalis-like lesions on the scalp associated with antiepileptic drugs. Int J Dermatol. Oct
1990;29(8):559-61
21
Distortion and occlusion of the follicular lumen by the fibrosis results in
retention of the hair shaft in the inferior aspect of the follicle, thereby
perpetuating the granulomatous inflammation and scarring. This stage is
marked by plaques of hypertrophic scar.
Importantly, note the duration of AKN, past therapeutic successes and
failures, present medications, hair grooming techniques, and any known
allergies. Regardless of symptomology, in general the lesions are
cosmetically bothersome.
Early papular lesions are usually asymptomatic, but pustular lesions are
often pruritic and occasionally painful. Large lesions can be painful.
Abscesses and sinuses may be present and may emit purulent,
malodorous discharge. Hats, shirts, jackets, and sweaters can irritate the
involved area.
Acne mechanica
Acne mechanica is an acneiform eruption that has been observed after
repetitive physical trauma to the skin such as rubbing, occurring from
clothing (belts and straps) or sports equipment (football helmets and
shoulder pads)13.
Acne medicamentosa
Acne medicamentosa (commonly referred to as drug-induced acne) is acne
that is caused or aggravated by medication14. Because acne is generally a
disorder of the pilosebaceous units caused by hormones, the medications
that trigger acne medicamentosa most frequently are hormone analogues.
It is also often caused by corticosteroids; in this case, it is referred to as
steroid acne.
Although the masculinizing hormone testosterone is most often blamed,
and although men with acne secondary to bodybuilding hormones are seen
from time to time, the major hormonal medications that causes acne are
the progestin analogues present in hormonal contraception. Other
medications can produce acneiform eruptions (usually pimply bumps and
pustules that look like acne).
13
14
Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). Page 685. McGraw-Hill. ISBN 0-07-138076-0.
Wolff, Klaus Dieter; et al. (2008). Fitzpatrick's Dermatology in General Medicine. McGraw-Hill Medical. ISBN 0-07-146690-8.
22
Some conditions mimic acne medicamentosa. The most common mimic is
folliculitis produced by an overgrowth of the Malassezia species, often
secondary to oral or systemic corticosteroids, or secondary to broadspectrum antibiotics such as the tetracycline family used in acne. This is
often misinterpreted as 'tetracycline-resistant acne'.
Acne miliaris necrotica
Acne miliaris necrotica consists of follicular vesicopustules, sometimes
occurring as solitary lesions that are usually very itchy15.
15
James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. Page 245.
ISBN 0-7216-2921-0.
23
Apocrine (Hidradenitis Suppurativa)
Hidradenitis suppurativa (HS) is a skin disease characterized by clusters of
chronic abscesses, epidermoid cysts, sebaceous cysts, pilonidal cyst or
multilocalised infections that most commonly affects areas bearing
apocrine sweat glands, such as the underarms, under the breasts, inner
thighs, groin and buttocks. The disease is not contagious.
The cysts seen in HS can be extremely tender and may persist for years
with interspersed periods of inflammation, culminating in incision and
drainage of pus from the cyst. This process often forms open wounds that
will not heal. For unknown reasons, people with HS develop plugging or
clogging of their apocrine glands. HS causes chronic scarring and pus
formation of the underarms, groin, and inner thighs. The simple procedure
of incision and drainage may provide symptomatic relief. HS flares may be
triggered by perspiration, hormonal changes (such as those seen with the
menstrual cycle), humidity and heat, and friction from clothing.
Persistent lesions may lead to scarring and the formation of sinus tracts, or
tunnels connecting the abscesses or infections under the skin. At this
stage, complete healing is usually not possible, and progression is variable,
with some experiencing remission for months to years at a time, while
others may worsen and require multiple surgeries. Bacterial infections and
cellulitis (deep tissue inflammation) are other common complications of HS.
Hidradenitis suppurativa pain and depression can be difficult to manage.
HS often goes undiagnosed for years due to a delay in seeking treatment
and is frequently misdiagnosed. There is currently no known cure nor any
consistently effective treatment. Carbon dioxide laser surgery is currently
considered the last resort for advanced disease. HS is an orphan disease
due to sparse research efforts. The disease's incidence rate is not well
established, but has been estimated as being between 1:24 (4.1%) and
1:600 (0.2%).
Hidradenitis suppurativa is a poorly studied disease and its cause remains
unknown. Experts disagree over proposed causes.
HS occurs when hair follicles become plugged. Lesions occur in any body
areas with hair follicle although intertriginous areas such as the axilla,
groin, and perianal region are more commonly involved. This theory
includes most of the following potentials indicators:
24
Post-pubescent individuals are more likely to exhibit HS.
Plugged apocrine (sweat) gland or hair follicle.
Excessive sweating.
Sometimes linked with other auto-immune conditions.
Androgen dysfunction.
Genetic disorders that alter cell structure.
Patients with more advanced cases may find exercise intolerably painful,
which may increase the rate of obesity among sufferers.
The historical understanding of the disease is that there are dysfunctional
apocrine glands or dysfunctional hair follicles, possibly triggered by a
blocked gland, creating inflammation, pain, and a swollen lesion.
There are a number of triggering factors that should be taken into
consideration.
Obesity is an exacerbating rather than a triggering factor, through
mechanical irritation, occlusion, and maceration.
Tight clothing, and clothing made of heavy, non-breathable materials.
Deodorants, depilation products, shaving of the affected area – their
association with hidradenitis suppurativa is still an ongoing debate amongst
researchers.
Drugs, in particular oral contraceptives (i.e., oral hormonal birth control;
"the pill") and lithium.
Hot and especially humid climates (dry/arid climates often cause
remission).
Predisposing factors
Genetic factors: an autosomal dominant inheritance pattern has been
postulated.
25
Endocrine factors: sex hormones, principally an excess of androgens, are
thought to be involved, although the apocrine glands are not sensitive to
these hormones. Women often have outbreaks before menstruation and
post-pregnancy, and the disease usually remits during pregnancy and after
menopause.
HS presents itself in three stages. Due to the large spectrum of clinical
severity and the severe impact on quality of life, a reliable method for
evaluating HS severity is needed.
Treatments
Treatments may vary depending upon presentation and severity of the
disease. Due to the poorly studied nature of this disease, the effectiveness
of the drugs and therapies listed below is unclear, and patients should
discuss all options with their physician or dermatologist. Nearly a quarter of
patients state that nothing relieves their symptoms. Possible treatments
include the following:
Changes in diet avoiding inflammatory foods, foods high in refined
carbohydrates.
Warm compresses with distilled vinegar water, and taking hot baths with
distilled white vinegar in the waterhydrotherapy, balneotherapy.
Icing the inflamed area daily until pain reduction is noticed.
Weight loss in overweight and obese patients, as well as smoking
cessation can improve or even alleviate many symptoms of hidradenitis
suppurativa.
Washing with benzoyl peroxide can be effective16.
16
Alikhan, Ali; Lynch, Eisen (2009). "Hidradenitis suppurativa: a comprehensive review". J Am Acad Derm 60 (4):
539–561.
26
27
Acral Hyperkeratosis
Hyperkeratosis (from Ancient Greek: ὑπέρ (hyper, “over”); keratos - keratin)
is thickening of the stratum corneum (the outermost layer of the epidermis),
often associated with the presence of an abnormal quantity of keratin, and
also usually accompanied by an increase in the granular layer. As the
corneum layer normally varies greatly in thickness in different sites, some
experience is needed to assess minor degrees of hyperkeratosis.
It can be caused by vitamin A deficiency or chronic exposure to arsenic.
Hyperkeratosis can also be caused by B-Raf inhibitor drugs such as
Zelboraf.
It can be treated with urea-containing creams, which dissolve the
intercellular matrix of the cells of the stratum corneum, promoting
desquamation of scaly skin, eventually resulting in softening of
hyperkeratotic areas17.
Acrodermatitis Enteropathica
Acrodermatitis enteropathica is an autosomal recessive metabolic disorder
affecting the uptake of zinc, characterized by periorificial (around the
natural orifices) and acral (in the limbs) dermatitis, alopecia (loss of hair),
and diarrhea.
Similar features may be present in acquired zinc deficiency. This disease
also is related to deficiency of zinc due to congenital causes.
Other names for acrodermatitis enteropathica include:
Brandt syndrome
Danbolt–Closs syndrome
Congenital zinc deficiency
Features of acrodermatitis enteropathica start appearing in the first few
months of life, as the infant discontinues breast milk. There are
erythematous patches and plaques of dry, scaly skin. The lesions may
appear eczematous, or may evolve further into crusted vesicles, bullas or
pustules. The lesions are frequent around the mouth and anus, and also in
17
Kumar, Vinay; Fausto, Nelso; Abbas, Abul (2004) Robbins & Cotran Pathologic Basis of Disease (7th ed.). Saunders. Page 1230. ISBN 07216-0187-1.
28
hands, feet and, scalp. There may be suppurative inflammation of the nail
fold surrounding the nail plate, known as paronychia.
Alopecia (loss of hair from the scalp, eyebrows, and eyelashes) may occur.
The skin lesions may be secondarily infected by bacteria such as
Staphylococcus aureus or fungi like Candida albicans. These skin lesions
are accompanied by diarrhea.
Acrodermatitis enteropathica has an autosomal recessive pattern of
inheritance.
A mutation of the SLC39A4 gene on chromosome 8 q24.3 is responsible
for the disorder. The SLC39A4 gene encodes a transmembrane protein
that serves as a zinc uptake protein. The features of the disease usually
start manifesting as an infant is weaned from breast milk. This has led
some scientists to suspect that human milk contains a beneficial substance
that helps uptake of zinc and prevents the disease from being manifested
while an infant is on breast milk.
Without treatment, the disease is fatal and affected individuals may die
within a few years. There is no cure for the condition. Treatment includes
lifelong dietary zinc supplementation in the range of greater than 1–2 mg/kg
of bodyweight per day18.
Actinic Dermatitis, Chronic
Chronic actinic dermatitis (also known as "Actinic reticuloid," "Chronic
photosensitivity dermatitis," "Persistent light reactivity," and "Photosensitive
eczema") is a condition where a subject's skin becomes inflamed due to a
reaction to sunlight or artificial light. CAD patients often suffer from other
related conditions of the skin that results in dermatitis in response to a
variety of stimulus (e.g., flowers, sunscreens, cosmetics, etc.)19.
Chronic actinic dermatitis mainly affects men over the age of 50 years. It is
characterised by severely itchy, red, inflamed, and thickened dry skin,
mainly in areas that have been exposed to sunlight or artificial light. The
condition is also known as chronic photosensitivity dermatitis and actinic
18
Michalczyk, A; Varigos, G; Catto-Smith, A; Blomeley, Rc; Ackland, Ml (August 2003). "Analysis of zinc transporter, hZnT4 ( Slc30A4), gene
expression in a mammary gland disorder leading to reduced zinc secretion into milk". Human Genetics 113 (3): 202–10. doi:10.1007/s00439003-0952-2. PMID 12743795.
19
James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-72162921-0.
29
reticuloid (this name comes from the histological findings of skin biopsies
which resemble a reticulosis or cutaneous T-cell lymphoma).
In many patients with the condition there is frequently a history of other
kinds of dermatitis, including atopic dermatitis, allergic contact dermatitis
(especially to plants such as chrysanthemum) and photocontact dermatitis
for many years before the photosensitivity develops. In these cases it is
sometimes called persistent light reaction
The rash may develop in all areas exposed to the sun, with the face, neck,
upper chest in a V distribution and backs of hands most commonly
affected. The lesions are usually red and inflamed with scaling and
lichenification (thickened and hardened patches of skin). The rash can be
very itchy. The rash may spread to other areas of the body where the skin
is covered by clothing.
The rash can be provoked by as little as 30 seconds exposure to daylight. It
is condition that is often present throughout the year. Patients are at risk
even on dull days and through window glass. Some of them also react to
artificial light sources, especially naked fluorescent lamps.
Testing shows chronic actinic dermatitis is due to abnormal reactions to
UVB, UVA and in severe cases to visible light.
Phototesting can be used to confirm the diagnosis. This involves
specialized tests in which areas of skin are exposed to known amounts of
light of specific wavelengths. The reactions that develop confirm the
presence of an abnormal reaction to the light.
Patch testing and photopatch testing are also used. It has been found that
positive patch-test reactions to one or more allergens occur in 75% of
patients with chronic actinic dermatitis, most often fragrance, sunscreens,
colophony and a sesquiterpene lactones (found in the diasy family of
plants).
Patients with chronic actinic dermatitis must take measures to avoid sun
exposure by following sun protection strategies. In severe cases it may be
necessary to admit the patient to a dark room in hospital.
30
In addition, if a contact allergy in involved the patient must try to avoid the
offending substance.
Treatment also includes:
Emollients
Topical corticosteroids
Topical tacrolimus or pimecrolimus cream
In severe cases, oral immune suppressive treatments may be required.
These include:
Systemic corticosteroids
Azathioprine
Ciclosporin
Extremely cautious desensitizing with photochemotherapy (PUVA) or
narrowband UVB with systemic steroid cover has been successful in
some cases.
The condition may spontaneously resolve, sometimes many years after the
onset of the disease. For most people it is a lifelong condition that requires
significant lifestyle changes to avoid sunlight as well as contact allergens.
Actinic Keratosis
Actinic keratosis (also called "solar keratosis" and "senile keratosis") is a
premalignant condition of thick, scaly, or crusty patches of skin.
It is more common in fair-skinned people and it is associated with those
who are frequently exposed to the sun, as it is usually accompanied by
solar damage. They are considered as potentially pre-cancerous, since
some of them progress to squamous cell carcinoma, so treatment is
recommended. Untreated lesions have up to 20% risk of progression to
squamous cell carcinoma.
Progressive development of these lesions occurs when skin is exposed to
the sun constantly and thick, scaly, or crusty areas appear. The scaly or
crusty portion is dry and rough. The lesions start out as flat scaly areas and
later grow into a tough, wart-like area.
An actinic keratosis site commonly ranges between 2 and 6 millimetres in
size, and may be dark or light, tan, pink, red, a combination of all these, or
have the same pigment as the surrounding skin. The lesion may appear on
31
any sun-exposed area, such as the face, ears, neck, scalp, chest, backs of
hands, forearms, or lips.
Physicians can usually identify actinic keratosis by doing a thorough
examination; in principle actinic keratosis is a clinical diagnosis. A biopsy
may be necessary when the keratosis is large or thick, to make sure that
the lesion is a keratosis and not a skin cancer. Seborrheic keratoses are
other lesions that appear in groups as the actinic keratosis do, but are not
caused by sun exposure, and are not related to skin cancers. Seborrheic
keratoses may be mistaken for an actinic keratosis.
Specialized forms of actinic keratoses include cutaneous horns, in which
the skin protrudes in a thick, hornlike manner, and actinic cheilitis, a scaling
and roughness of the lower lip and blurring of the border of the lip and
adjacent skin.
Actinic keratosis usually shows focal parakeratosis with associated loss of
the granular layer of, and thickening of the epidermis. The normal ordered
maturation of the keratinocytes is disordered to varying degrees, there may
be widening of the intracellular spaces, and they may also have some
cytologic atypia, such as abnormally large nuclei. The underlying dermis
often shows severe actinic elastosis and a mild chronic inflammatory
infiltrate.
Preventive measures recommended for actinic keratosis are similar to
those for skin cancer:
Not staying in the sun for long periods of time without protection (e.g.,
sunscreen, clothing, hats)
Frequently applying powerful sunscreens with SPF ratings greater than 30
and that also block both UVA and UVB light
Wearing sun protective clothing such as hats, long-sleeved shirts, long
skirts, or trousers
Avoiding sun exposure during noon hours is very helpful because
ultraviolet light is the most powerful at that time20.
20
Andrews' Diseases of the Skin: Clinical Dermatology - Expert Consult - Online and Print, 11e (James, Andrew's Disease of the Skin) William
D. James MD (Author), Timothy Berger MD (Author), Dirk Elston MD (Author)
32
Actinic Lentigines
Actinic lentigines, senile lentigines, solar lentigines, "liver spots" and "age
spots" are different terms for the same condition. They occur on the sunexposed skin of the middle-aged and elderly.
These lesions are persistent brown macules due to a linear increase in the
number of melanocytes within the basal layer of the epidermis. Lentigines
may occur at any site on the skin, including the conjunctivae and
mucocutaneous junctions. Multiple lentigenes are a common finding in
people with fair skin, but may also rarely occur in rare hereditary multisystem disorders such as Peutz–Jeghers disease (particularly when
distributed on the lips, buccal mucosae, and acral sites), centrofacial
lentiginosis (associated with cardiac abnormalities), and the Leopard
syndrome (i.e. lentigines, ECG abnormalities, ocular hypertelorism,
pulmonary stenosis, abnormal genitalia, retarded growth, deafness).
Lentigenes may also be caused by severe sunburn, especially on the upper
back or from chronic sun exposure (solar or actinic lentigenes).
They are common on the face and dorsal hands in middle-aged and elderly
individuals (age spots or liver spots). Multiple solar lentigines may result
from PUVA therapy or excessive sunbed use21.
Actinic Prurigo
Actinic prurigo (also known as "Familial polymorphous light eruption of
American Indians," "Hereditary polymorphous light eruption of American
Indians," "Hutchinson's summer prurigo," and "Hydroa aestivale") is a
common sunlight-induced, pruritic, papular or nodular skin eruption.
The cause for actinic prurigo is unknown, however researchers believe that
protein in our bodies may be a cause to the condition also: •UV-A and UVB light seem to be the main provoking agents. This observation is
supported by the fact that most patients live at high altitudes (>1000 m
above sea level), and the condition improves in many patients when they
move to lower altitudes. However, some patients who are affected already
live at sea level.18,19,27 •Some authors are considering a food
photosensitizer or a nutritional selective deficiency as a cause; however, no
evidence proves this theory.
21
Andrews' Diseases of the Skin: Clinical Dermatology - Expert Consult - Online and Print, 11e (James, Andrew's Disease of the Skin) William
D. James MD (Author), Timothy Berger MD (Author), Dirk Elston MD (Author)
33
AP is characterized by itchy, inflamed papules, nodules, and plaques on
the skin. Lesions typically appear hours or days after exposure of the skin
to UV light, and follow a general pattern of sun-exposed areas. The face,
neck, arms, hands, and legs are often affected, although lesions
sometimes appear on skin that is covered by clothing and thus not exposed
to UV light, thus making AP somewhat difficult to diagnose.
AP, also known as Actinic Prurigo, is a chronic disease. Symptoms usually
worsen in the spring and summer as the day lengthens and exposure to
exams increase. Exams such as AP World, AP Euro, etc.
Currently there is no cure for actinic prurigo, and treatment focuses on
relieving the dermatologic symptoms, by way of topical steroid creams or
systemic immunosuppressants.
Prescribed treatments include:
Topical creams such as Tacrolimus and Betamethasone.
Systemic immunosuppressants such as Prednisone.
In some cases, Thalidomide has proven to be effective in controlling
the symptoms of actinic prurigo.
All patients with AP are encouraged to minimize sun exposure, and to
use strong sunscreen throughout the year, and even on cloudy or
overcast days, as UVA light, unlike UVB light, is able to penetrate
cloud cover and remains constant throughout the day.
Alternative treatment methods might include UV Hardening, Meditation
and/or cognitive behavioral therapy. UV-A desensitization phototherapy has
also been shown to be effective in cases. The U.S. Food and Drug
Administration (FDA) has yet to approve these allopathic approaches to
medicine, so there remains much to be discovered about this particular
illness in the United States.
Albinism, Oculocutaneous
Oculocutaneous albinism is a form of albinism involving the eyes ("oculo-"),
skin ("-cutaneous"), and according to some definitions, the hair as
well.Oculocutaneous albinism (OCA) is a heterogeneous group of inherited
disorders characterized by a partial or complete failure to produce melanin
in the skin and eyes. In tyrosinase- negative albinism the skin is pink, the
34
hair is white, and the iris translucent resulting in a prominent red reflex.
Most patients have horizontal or rotatory nystagmus and photophobia.
The commoner tyrosinase-positive OCA has marked but incomplete
dilution of pigment of the skin, hair, and eyes and, with increasing
age,some pigment formation and the development of flaxen-yellow hair. In
Afro-Caribbeans, the skin is a yellowish-brown colour that with age
develops dark-brown freckles, resembling PUVA lentigines, in sun-exposed
areas. In temperate climates, the visual defects cause the greatest
disability. In hot climates, sun-damaged skin and early development of skin
cancers is the main
problem.
Strict sun protection and regular examinations of the skin for premalignant
and malignant lesions.
Four types of oculocutaneous albinism have been described, all caused by
a disruption of melanin synthesis and all autosomal recessive disorders22.
Albright’s syndrome
Albright syndrome: A genetic disorder of bones, skin pigmentation and
hormonal problems with premature sexual development. Also called
McCune-Albright syndrome and polyostotic fibrous dysplasia.
In the syndrome, there is bone disease with fractures and deformity of the
legs, arms and skull; pigment patches of the skin; and endocrine
(hormonal) disease with early puberty (early menstrual bleeding,
development of breasts and pubic hair) and an increased rate of growth.
The Albright syndrome is usually caused by mosaicism for a mutation in a
gene called GNAS1 (Guanine Nucleotide binding protein, Alpha Stimulating
activity polypeptide 1).
The syndrome shows a broad spectrum of severity. Sometimes, children
are diagnosed in early infancy with obvious bone disease and markedly
increased endocrine secretions from several glands. At the opposite end of
the spectrum, many children are entirely healthy, and have little or no
outward evidence of bone or endocrine involvement. They may enter
puberty close to the normal age, and have no unusual skin pigment at all.
22
Oculocutaneous albinism. Okulicz JF1, Shah RS, Schwartz RA, Janniger CK.J Eur Acad Dermatol Venereol. 2003 May;17(3):251-6.
35
Endocrine Abnormalities
Precocious Puberty -- When the signs of puberty (development of breasts,
testes, pubic and underarm hair, body odor, menstrual bleeding, and
increased growth rate) appear before the age of 8 years in a girl or 9 1/2
years in a boy, it is termed "precocious puberty." In the most common form
of precocious puberty, there is early activation of the regions in the brain
which control the maturation of the gonads (ovaries in a girl and testes in a
boy). One brain center, the hypothalamus, secretes a substance called
gonadotropin-releasing-hormone or "GnRH." This acts, in turn, on another
part of the brain, the pituitary gland, to cause increased secretion of
hormones called "gonadotropins" (LH and FSH) that travel through the
bloodstream, and act on the ovaries or testes to stimulate secretion of
estrogen or testosterone.
The precocious puberty in Albright girls is caused by estrogens which are
secreted into the bloodstream by ovarian cysts, which enlarge, and then
decrease in size over periods of weeks to days. The cysts can be
visualized and measured by ultrasonography, in which sound waves are
used to outline the dimensions of the ovaries. The cysts may become quite
big, occasionally over 50 cc in volume (about the size of a golf ball).
Frequently, menstrual bleeding and breast enlargement accompany the
growth of a cyst. In fact, menstrual bleeding under 2 years of age has been
the first symptom of Albright syndrome in 85% of patients. Although ovarian
cysts and irregular menstrual bleeding may continue into adolescence and
adulthood, many adult women with Albright syndrome are fertile, and can
bear normal children.
The precocious puberty in Albright syndrome has been difficult to treat.
After surgical removal of the cyst or of the entire affected ovary, cysts
usually recur in the remaining ovary. A progesterone-like hormone called
Provera can be given to suppress the menstrual bleeding, but does not
appear to slow the rapid rates of growth and bone development, and may
have unwanted effects on adrenal functioning. The synthetic forms of
GnRH (Deslorelin, Histerelin, and Lupron) which suppress LH and FSH,
and are used to treat the common, gonadotropin-dependent form of
precocious puberty, are not effective in most girls with McCune-Albright
syndrome.
36
Thyroid Function -- Almost 50% of patients with Albright syndrome have
thyroid gland abnormalities. These include generalized enlargement called
goiter and irregular masses called nodules and cysts. Some patients have
subtle structural changes detected only by ultrasonography. Pituitary
thyroid-stimulating-hormone (TSH) levels are low in these patients, and
thyroid hormone levels may be normal or elevated. Therapy with drugs
which block thyroid hormone synthesis (Propylthiouracil or Methimazole),
can be given if thyroid hormone levels are excessively high.
Growth Hormone -- Excessive secretion of pituitary growth hormone is
sometimes seen in Albright syndrome. This may be diagnosed in young
adults, when they developed coarsening of facial features, enlargement of
hands and feet, and arthritis characteristic of the condition termed
"acromegaly." Therapy has included surgical removal of the area of the
pituitary which is secreting the hormone, and use of new, synthetic analogs
of the hormone somatostatin, which suppress growth hormone secretion.
Other Endocrine Abnormalities -- Although rare, adrenal enlargement and
excessive secretion of the adrenal hormone cortisol is seen in Albright
syndrome. This may cause obesity of the face and trunk, weight gain, skin
fragility and cessation of growth in childhood. These symptoms are called
"Cushing's syndrome." Treatment is removal of the affected adrenal glands,
or use of drugs which block cortisol synthesis.
Acral lentiginous melanoma
Acral lentiginous melanoma (ALM) is a special presentation of cutaneous
melanoma arising on the sole, palm, fingernail or toenail bed. ALM occurs
most often in Asians, sub-Saharan Africans, and African Americans,
comprising 50 to 70% of the melanomas of the skin found in these
populations. It occurs most often in older males (60 years) and often grows
slowly over a period of years. The delay in development of the tumor is the
reason these tumors are often discovered only when nodules appear or in
case of nail involvement, the nail is shed; therefore, the prognosis is poor.
Subungual melanoma most often occurs on the nail bed of the thumb or
large toe. The clinical features are less striking than in other melanomas,
appearing in the radial growth phase as macules: dark brown, blue-black,
or black, with little variegation and often ill-defined.
Relatively rare compared to SSM in whites. Probably same incidence in
Asians/blacks who have fewer melanomas in general. The pigmented
37
macules that are frequently seen on the soles of African blacks could be
comparable with Clark's dysplastic melanocytic nevi.
ALM can be identified by a longitudinal tan, black, or brown streak on a
finger or toe nail or areas of dark pigmentation on palms of hands or soles
of feet
38
Alkaptonuria
Alkaptonuria (black urine disease, black bone disease, or alcaptonuria) is a
rare inherited genetic disorder of phenylalanine and tyrosine metabolism.
This is an autosomal recessive condition that is due to a defect in the
enzyme homogentisate 1,2-dioxygenase (EC 1.13.11.5), which participates
in the degradation of tyrosine. As a result, homogentisic acid and its oxide,
called alkapton, accumulate in the blood and are excreted in urine in large
amounts (hence -uria). Excessive homogentisic acid causes damage to
cartilage (ochronosis, leading to osteoarthritis) and heart valves as well as
precipitating as kidney stones. Treatment with nitisinone, which suppresses
homogentisic acid production, is being studied. Alkaptonuria is more
common in Slovakia and the Dominican Republic than in other countries.
Alkaptonuria is often asymptomatic, but the sclera of the eyes may be
pigmented (often only at a later age), and the skin may be darkened in sunexposed areas and around sweat glands; sweat may be coloured brown.
Urine may turn brown or even inky black if collected and left exposed to
open air, especially when left standing for a period of time. Kidney stones
and stone formation in the prostate (in men) are common and may occur in
more than a quarter of cases.
The main symptoms of alkaptonuria are due to the accumulation of
homogentisic acid in tissues. In the joints this leads to cartilage damage,
specifically in the spine, leading to low back pain at a young age in most
cases. Cartilage damage may also occur in the hip and shoulder. Joint
replacement surgery (hip and shoulder) is often necessary at a relatively
young age.
Valvular heart disease, mainly calcification and regurgitation of the aortic
and mitral valves, may occur, and in severe and progressive cases valve
replacement may be necessary. Coronary artery disease may be
accelerated in alkaptonuria.
A distinctive characteristic of alkaptonuria is that ear wax exposed to air
turns red or black (depending on diet) after several hours because of the
accumulation of homogentisic acid.
The diagnosis of alkaptonuria needs to be suspected before diagnostic
testing can be performed using paper chromatography and thin layer
39
chromatography. Both blood plasma and urine can be used for diagnosis.
In alkaptonuria patients, plasma levels of homogentisic acid (HGA) are on
average 6.6 micrograms/ml; normally HGA levels are undetectable. Urinary
HGA levels are increased 300 fold in alkaptonuria patients, between 0.4
and 12.4 g per day (on average 3.12 mmol HGA/mmol of creatinine).
Pathophysiology of alcaptonuria, which is due to the absence of functional
homogentisate dioxygenase in the liver.
No treatment modality has been unequivocally demonstrated to reduce the
complications of alkaptonuria. Main treatment attempts have focused on
preventing ochronosis through the reduction of accumulating homogentisic
acid. Such commonly recommended treatments include large doses of
ascorbic acid (vitamin C) or dietary restriction of amino acids phenylalanine
and tyrosine. However, vitamin C treatment has not shown to be effective,
while reported benefits from protein dietary restriction has been shown to
only apply to children, and not in adults23.
Alopecia
Hair loss or baldness (technically known as alopecia) is a loss of hair from
the head or body. Baldness can refer to general hair loss or male pattern
baldness specifically. Some types of baldness can be caused by alopecia
areata, an autoimmune disorder. The extreme forms of alopecia areata are
alopecia totalis, which involves the loss of all head hair, and alopecia
universalis, which involves the loss of all hair from the head and the body.
Baldness and hypotrichosis can have many causes, including fungal
infection (tinea capitis), traumatic damage, such as by compulsive pulling
(trichotillomania), as a result of radiotherapy or chemotherapy, and as a
result of nutritional deficiencies such as iron, and as a result of autoimmune
phenomena, including alopecia areata and hair loss associated with
systemic lupus erythematosus.
Baldness is the partial or complete lack of hair growth, and part of the wider
topic of "hair thinning". The degree and pattern of baldness varies, but its
most common cause is androgenic alopecia, alopecia androgenetica, or
alopecia seborrheica, with the last term primarily used in Europe.
23
Phornphutkul C, Introne WJ, Perry MB, et al. (2002). "Natural history of alkaptonuria". New England Journal Medicine 347 (26): 2111–21.
doi:10.1056/NEJMoa021736. PMID 12501223.
40
Alopecia areata (mild - medium level) usually shows in unusual hair loss
areas e.g. eyebrows, backside of the head or above the ears where usually
the male pattern baldness does not effect. In male-pattern hair loss, loss
and thinning begin at the temples and the crown and either thins out or falls
out. Female-pattern hair loss occurs at the frontal and parietal.
People have between 100,000 and 150,000 hairs on their head. The
number of strands normally lost in a day varies, but on average is 100. In
order to maintain a normal volume, hair must be replaced at the same rate
at which it is lost. The first signs of hair thinning that people will often notice
are more hairs than usual left in the hairbrush after brushing or in the basin
after shampooing. Styling can also reveal areas of thinning, such as a
wider parting or a thinning crown.
A substantially blemished face, back and limbs could point to cystic acne.
The most severe form of the condition, cystic acne arises from the same
hormonal imbalances that cause hair loss, and is associated with DHT
production. Seborrheic dermatitis, a condition in which an excessive
amount of sebum is produced and builds up on the scalp (looking like an
adult cradle cap) is also a symptom of hormonal imbalances, as is an
excessively oily or dry scalp. Both can cause hair thinning.
Although not completely understood,alopecia can have many causes:
More than 95% of hair thinning in men is male pattern hair loss (also known
as androgenic alopecia). Male pattern hair loss is characterized by hair
receding from the lateral sides of the forehead (known as a "receding
hairline") and/or a thinning crown (balding to the area known as the
‘vertex’). Both become more pronounced until they eventually meet,
leaving a horseshoe-shaped ring of hair around the back of the head.
The incidence of pattern baldness varies from population to population and
is based on genetic background. Environmental factors do not seem to
affect this type of baldness greatly. One large scale study in Maryborough,
Victoria, Australia showed the prevalence of mid-frontal baldness increases
with age and affects 73.5 percent of men and 57 percent of women aged
80 and over. A rough rule of thumb is that the incidence of baldness in
males corresponds to chronological age. For example, according to Medem
Medical Library's website, male pattern baldness (MPB) affects roughly 40
41
million men in the United States. Approximately 25 percent of men begin
balding by age 30; two-thirds begin balding by age 60.
There is a 4 in 7 chance of receiving the baldness gene. Onset of hair loss
sometimes begins as early as the end of puberty, and is mostly genetically
determined. It was previously believed that baldness was inherited from the
maternal grandfather. While there is some basis for this belief, both parents
contribute to their offspring's likelihood of hair loss. Most likely, inheritance
involves many genes with variable penetrance.
The trigger for this type of baldness is dihydrotestosterone, a more-potent
form of testosterone often referred to by its acronym DHT. DHT is an
androgenic hormone, body- and facial-hair growth promoter that can
adversely affect the prostate as well as the hair located on the head. The
mechanism by which DHT accomplishes this is not yet fully understood. In
genetically prone scalps (i.e., those experiencing male or female pattern
baldness), DHT initiates a process of follicular miniaturization, in which the
hair follicle begins to deteriorate. As a consequence, the hair’s growth
phase (anagen) is shortened, and young, unpigmented vellus hair is
prevented from growing and maturing into the deeply rooted and pigmented
terminal hair that makes up 90 percent of the hair on the head. In time, hair
becomes thinner, and its overall volume is reduced so that it resembles
fragile vellus hair or "peach fuzz" until, finally, the follicle goes dormant and
ceases producing hair completely.
Amiodarone-induced Pigmentation
Amiodarone is an antiarrhythmic agent used for various types of cardiac
dysrhythmias, both ventricular and atrial (heart medication).
Amiodarone-induced Pigmentation is also known as “drug-induced skin
pigmentation” is quite common and accounts for 10-20% of all cases of
acquired hyperpigmentation. Pigmentation may be induced by a wide
variety of drugs; the main ones implicated include non-steroidal antiinflammatory drugs (NSAIDs), phenytoin, antimalarials, amiodarone,
antipsychotic drugs, cytotoxic drugs, tetracyclines, and heavy metals.
Several mechanisms may be involved in the drug-induced changes of
pigmentation of the skin.
42
Certain heavy metals, e.g. iron, may be deposited in the dermis following
damage to dermal vessels. If deposited in sufficient quantities a distinctive
change in skin colour may be seen without any significant increase in
melanin.
Some drugs react with melanin to form a drug-pigment complex. Exposure
to sunlight often stimulates sun-induced melanin synthesis with formation of
these complexes.
Some drugs will induce hypermelanosis (accumulation of melanin) as a
non-specific post-inflammatory change in predisposed individuals. This is
often worsened by sun exposure.
Some drugs induce pigmentation directly by accumulating and/or reacting
with other substances in the skin.
What are the clinical features of drug-induced skin pigmentation?
The clinical features of drug-induced skin pigmentation are very variable
according to the drug involved. A large range of patterns and shades may
be formed.
Amyloid, macular
Amyloidosis is the term used for a group of diseases where one or more
body organs accumulate various insoluble proteins (amyloid) in amounts to
cause dysfunction of the organ system. Organs often affected include the
heart, kidney, gastrointestinal tract, nervous system and skin. Amyloidosis
of the skin is called cutaneous amyloidosis. In this condition, amyloid or
amyloid-like proteins are deposited in the dermis layer of skin.
In this case lesions appear as flat dusky-brown or greyish coloured spots
that may coalesce to form patches of darkened skin.
The degree of itchiness varies from mild to severe.
Lesions are usually distributed symmetrically over the upper back between
the shoulder blades, on the chest and sometimes on the arms.
It appears to be more common in Asians, South Americans and Middle
Easterners.
43
It usually presents in early adult life and appears to affect women more
frequently than men.
Anderson–Fabry’s disease
Fabry disease is a rare, inherited disease caused by the deficiency of an
enzyme called alpha galactosidase A (a-GAL A), which is encoded by the
GLA gene. In patients with Fabry disease, a-GAL A is either lacking or
deficient.
A genetic fault (mutation) in the gene that controls a-GAL A causes a poor
breakdown of lipids, which leads to a harmful accumulation of lipids specifically globotriaosylceramide (GL-3) - in the cardiovascular system,
autonomic nervous system, kidneys and eyes.
There are several lipid storage disorders; Fabry disease is the only X-linked
(inherited) one.
Fabry disease is estimated to affect 1 in every 55,000 males. Many more
males have the defective gene, but with no symptoms.
The mutated gene is carried on the mother's X chromosome, meaning
there is a 50% chance she will pass it on to her sons, and a 50% risk her
daughters will be carriers.
If females do have symptoms, they tend to be much milder than those seen
in males. However, some females with Fabry disease may be affected
severely. Young boys may have serious eye manifestations, particularly
cloudiness of the cornea.
The accumulation of lipids, specifically GL-3, can lead to problems with
arterial circulation and a higher risk of stroke or heart attack.
In males signs and symptoms usually start during childhood.
Pain - the child experiences episodes of discomfort and pain in the hands
and feet (acroparesthesias). These can be triggered by stress, fatigue,
fever, physical activity, and even changes in the weather.
44
Skin rash - known as angiokeratoma, A dark, red, spotted skin rash
appears. The rash is seen most densely between the navel (belly button)
and the knees.
Hypohidrosis - reduced ability to sweat.
Keratopathy - clouding of the corneas. This does not affect vision
Fabry disease usually develops slowly over many years as GL-3 gradually
accumulates. After the age of 30 years, patients may experience:
Gastrointestinal problems - patients with Fabry disease commonly
experience stomach problems, which may include nausea, vomiting, and
diarrhea.
Cardiovascular problems - years of GL-3 accumulation eventually result in
damage to blood vessels that supply the heart, as well as damage to the
heart itself. Problems include:
- heart failure
- arrhythmia
- heart attack
- faulty heart valves
- enlarged heart
Renal (kidney) problems - decades of GL-3 accumulation can lead to renal
failure or renal insufficiency. Often, Fabry disease is first detected when the
patient comes to the doctor with kidney problems.
CNS (central nervous system) disorders - small blood vessels in the brain
can become affected after years of GL-3 buildup. Patients are at a higher
risk of having:
- stroke
- dizziness
- numbness and tingling (pins and needles)
- headaches
- weakness
Hearing problems - for the same reasons, GL-3 accumulation, the patient
may gradually lose his hearing, or experience ringing in the ears (tinnitus).
45
Emotional and psychological problems - living with the symptoms
associated with Fabry disease, many of which get worse with time, causes
anxiety, fear, and also depression. There may be a feeling of guilt if the
disease is inherited by an offspring.
In females who are also carriers of the genetic mutation, generally either
have no symptoms or much milder ones than males. However, a small
percentage may suffer as much as their male counterparts.
In milder cases, symptoms usually appear during the patient's
childhood/teen years, and may include skin rashes, corneal cloudiness,
pain in the extremities, and hypohidrosis. There is also the possibility of
chronic diarrhea and abdominal pain. As they get older the left side of the
heart may become enlarged (left ventricular hypertrophy); there is also a
possibility of heart-valve problems.
In more serious cases, the girl/woman has the same signs and symptoms
as males with severe symptoms.
Angio-oedema
Angioedema (BE: angiooedema) or Quincke's edema is the rapid swelling
(edema) of the dermis, subcutaneous tissue, mucosa and submucosal
tissues. It is very similar to urticaria, but urticaria, commonly known as
hives, occurs in the upper dermis. The term angioneurotic oedema was
used for this condition in the belief that there was nervous system
involvement, but this is no longer thought to be the case.
Cases where angioedema progresses rapidly should be treated as a
medical emergency, as airway obstruction and suffocation can occur.
Epinephrine may be life-saving when the cause of angioedema is allergic.
In the case of hereditary angioedema, treatment with epinephrine has not
been shown to be helpful.
The skin of the face, normally around the mouth, and the mucosa of the
mouth and/or throat, as well as the tongue, swell up over the period of
minutes to hours. The swelling can also occur elsewhere, typically in the
hands. The swelling can be itchy or painful. There may also be slightly
decreased sensation in the affected areas due to compression of the
nerves. Urticaria (hives) may develop simultaneously.
46
In severe cases, stridor of the airway occurs, with gasping or wheezy
inspiratory breath sounds and decreasing oxygen levels. Tracheal
intubation is required in these situations to prevent respiratory arrest and
risk of death.
Sometimes, the cause is recent exposure to an allergen (e.g. peanuts), but
more often it is either idiopathic (unknown) or only weakly correlated to
allergen exposure.
In hereditary angioedema, often no direct cause is identifiable, although
mild trauma, including dental work and other stimuli, can cause attacks.
There is usually no associated itch or urticaria, as it is not an allergic
response. Patients with HAE can also have recurrent episodes (often called
"attacks") of abdominal pain, usually accompanied by intense vomiting,
weakness, and in some cases, watery diarrhea, and an unraised, nonitchy
splotchy/swirly rash. These stomach attacks can last one to five days on
average, and can require hospitalization for aggressive pain management
and hydration. Abdominal attacks have also been known to cause a
significant increase in the patient's white blood cell count, usually in the
vicinity of 13,000 to 30,000. As the symptoms begin to diminish, the white
count slowly begins to decrease, returning to normal when the attack
subsides. As the symptoms and diagnostic tests are almost
indistinguishable from an acute abdomen (e.g. perforated appendicitis) it is
possible for undiagnosed HAE patients to undergo laparotomy (operations
on the abdomen) or laparoscopy (keyhole surgery) that turns out to have
been unnecessary.
HAE may also cause swelling in a variety of other locations, most
commonly the limbs, genitals, neck, throat and face. The pain associated
with these swellings varies from mildly uncomfortable to agonizing pain,
depending on its location and severity. Predicting where and when the next
episode of edema will occur is impossible. Most patients have an average
of one episode per month, but there are also patients who have weekly
episodes or only one or two episodes per year. The triggers can vary and
include infections, minor injuries, mechanical irritation, operations or stress.
In most cases, edema develops over a period of 12–36 hours and then
subsides within 2–5 days.
47
Angiofibroma
Angiofibroma, also known as fibrous papule, is a relatively common lesion
seen in males and females after puberty. Angiofibromas represent focal
growth of vascular and collagen structures normally found in the skin. They
most often present as 1-5 mm, solitary, flesh-colored to slightly red bumps
on the nose, and have no hereditary predisposition. These lesions may
sometimes be confused with basal cell carcinoma.
Therefore, biopsy is needed to make the distinction. Uncommonly,
individuals may present with multiple angiofibromas distributed on their
face and less often, other parts of the body. Multiple angiofibromas have
been associated with several genetic conditions, including tuberous
sclerosis, Birt-Hogg-Dubé syndrome, and multiple endocrine neoplasia type
1 (MEN1). Unlike the solitary variant, these hereditary conditions have
additional cutaneous and systemic findings.
The majority of treatments available for angiofibromas are destructive.
Depending on the location or number of lesions, your physician may elect
to choose shave excision, dermabrasion, electrodessication and curettage,
or laser therapy to treat these growths. Once these growths are treated,
they seldom come back, although new lesions may form.
The majority of treatments available for angiofibromas are destructive.
Depending on the location or number of lesions, your physician may elect
to choose shave excision, dermabrasion, electrodessication and curettage,
or laser therapy to treat these growths. Once these growths are treated,
they seldom come back, although new lesions may form.
Angiokeratomas
Angiokeratoma is a benign cutaneous lesion of capillaries, resulting in
small marks of red to blue color and characterized by hyperkeratosis.
Angiokeratoma corporis diffusum refers to Fabry's disease, but this is
usually considered a distinct condition.
Angiokeratoma of Fordyce (also known as "Angiokeratoma of the scrotum
and vulva," though not to be confused with Fordyce's spots) is a skin
condition characterized by red to blue papules on the scrotum or vulva.
Solitary angiokeratoma is a small, bluish-black, warty papule that occurs
predominantly on the lower extremities.
48
Verrucous vascular malformation (also known as "Angiokeratoma
circumscriptum naeviforme") is a malformation of dermal and subcutaneous
capillaries and veins, a congenital vascular malformation, which, over time,
a verrucous component appears.
Angiolymphoid hyperplasia with eosinophilia
Angiolymphoid hyperplasia with eosinophilia usually presents with pink to
red-brown, dome-shaped, dermal papules or nodules of the head or neck,
especially about the ears and on the scalp.
Angioma Serpiginosum
Angioma serpiginosum is characterized by minute, copper-colored to bright
red angiomatous puncta that have a tendency to become papular.
Angiosarcoma
Angiosarcoma is a malignant neoplasm (cancer) of endothelial-type cells
that line vessel walls. This may be in reference to blood
(hemangiosarcoma) or lymphatic vessels (lymphangiosarcoma).
Its origin typically readily permits metastases to distant sites. Most tumors
of visceral blood and lymphatic vessel walls are malignant.
Hemangiosarcomas and lymphangiosarcomas of the skin are not common.
Kaposi's sarcoma is a different type of cancer that also involves
endothelial-type cells.
Angiosarcoma of the liver, a rare fatal tumor, has been seen in workers
intensively exposed to the gas vinyl chloride monomer (VCM) for prolonged
periods while working in polyvinyl chloride (PVC) polymerization plants. It
has also been associated with individuals exposed to arsenic-containing
insecticides and Thorotrast. In dogs, hemangiosarcoma is relatively
common, especially in larger breeds such as golden retrievers and
Labrador retrievers.
49
Bacillary Angiomatosis
Bacillary Angiomatosis is a type of Angiomatosis that affects the entire
body system. It is an infectious disease that causes rapid multiplication of
the small blood vessels of the skin. This is a rare illness but is potentially
risky to sufferers.
It affects only a small percentage of people around the world. The condition
shows a preference for white race followed by people of black and Hispanic
background. It also mostly affects men. About 90% of sufferers in the US
are found to be people belonging to male sex. The disease affects kids
very rarely.
Bacillary Angiomatosis is mainly characterized by the appearance of
lesions or nodules of varying sizes all over the skin. The lesions are
typically very small but can grow up to about 4 cm in diameter. These
usually arise in groups. You can find as many as 50 papules at one time.
These can vary in color and are generally bright red or almost black in
appearance.
The nodules continue to grow in size and often rupture to bleed from time
to time. These are accompanied by several other symptoms like fever,
body aches, dyspepsia and inflammation of glands.
Bacillary Angiomatosis is caused by bacterial infection resulting from
exposure to Bartonella Henselae and Bartonella Quintana. Humans
generally get infected by Bartonella Henselae due to cat bite or cat scratch.
Bartonella Quintana is typically transmitted by lice.
Bacillary Angiomatosis Bartonella Infection also affects people with
compromised immunity as in AIDS sufferers. It rarely arises in people with
strong immune systems. The disease is mostly seen in HIV sufferers. It is
only in rare instances that a non-HIV sufferers also get this condition.
Bacillary angiomatosis (BA) is a form of angiomatosis associated with
bacteria of the Bartonella genus. It is caused by either Bartonella henselae
or Bartonella quintana.
Bartonella henselae is most often transmitted through a cat scratch or bite,
though ticks and fleas may also act as a vector.
50
Bartonella quintana is usually transmitted by lice.
It can manifest in people with AIDS and rarely appears in those who are
immunocompetent.
BA is characterised by the proliferation of blood vessels, resulting in them
forming tumour-like masses in the skin and other organs.
While cutaneous BA is the most common form of BA, BA can also affect
several other parts of the body, such as the brain, bone, bone marrow,
lymph nodes, gastrointestinal tract, respiratory tract, spleen and liver.
Symptoms vary depending on which parts of the body are affected; for
example, those whose livers are affected may have an enlarged liver and
fever, while those with osseous BA will experience intense pain in the
affected area.
While curable, it is potentially fatal if not treated.
BA responds dramatically to several antibiotics. Usually, erythromycin will
cause the skin lesions to gradually fade away in the next four weeks,
resulting in complete recovery. Doxycycline may also be used. However, if
the infection does not respond to either of these, the medication is usually
changed to tetracycline. If the infection is serious, then a bactericidal
medication may be coupled with the antibiotics.
If a cat is carrying Bartonella henselae, then it may not exhibit any
symptoms. Cats may be bacteremic for weeks to years, but infection is
more common in young cats. Transmission to humans is thought to occur
via flea feces inoculated into a cat scratch or bite, and transmission
between cats occurs only in the presence of fleas. Therefore, elimination
and control of fleas in the cat's environment are key to prevention of
infection in both cats and humans.
51
Bartonella
Bartonella is a genus of Gram-negative bacteria. Facultative intracellular
parasites, Bartonella species can infect healthy people, but are considered
especially important as opportunistic pathogens. Bartonella species are
transmitted by insect vectors such as ticks, fleas, sand flies, and
mosquitoes24. At least eight Bartonella species or subspecies are known to
infect humans.
Bartonella henselae is the organism responsible for cat scratch disease, a
self-limited disease except in immunocompromised hosts.
The currently accepted model explaining the infection cycle holds that the
transmitting vectors are blood-sucking arthropods and the reservoir hosts
are mammals. Immediately after infection, the bacteria colonize a primary
niche, the endothelial cells. Every five days, some of the Bartonella
bacteria in the endothelial cells are released into the blood stream, where
they infect erythrocytes. The bacteria then invade a phagosomal
membrane inside the erythrocytes, where they multiply until they reach a
critical population density. At this point, they simply wait until they are taken
up with the erythrocytes by a blood-sucking arthropod.
Though some studies have found "no definitive evidence of transmission by
a tick to a vertebratehost," Bartonella species are well-known to be
transmissible to both animals and humans through various other vectors,
such as fleas, lice, and sand flies. Recent studies have shown a strong
correlation between tick exposure and bartonellosis, including human
bartonellosis. Bartonella bacteria are associated with cat-scratch disease,
but a study in 2010 concluded, "Clinicians should be aware that . . . a
history of an animal scratch or bite is not necessary for disease
transmission." All current Bartonella species identified in canines are
human pathogens.
Basal cell carcinoma
Basal cell carcinoma (BCC) is the most common form of skin cancer. In the
vast majority of cases, it is caused by chronic exposure to harmful solar
radiation and therefore occurs most frequently on sun-exposed areas of the
body. BCCs are more common in men, with a male to female ratio of
approximately 2:1. People with fair skin, light hair, blue, green, or grey eyes
24
Andrews' Diseases of the Skin: Clinical Dermatology - Expert Consult - Online and Print, 11e (James, Andrew's Disease of the Skin) William
D. James MD (Author), Timothy Berger MD (Author), Dirk Elston MD (Author)
52
are at the highest risk of developing this skin cancer. In a few instances,
there are other contributing factors such as immunosuppression (a
weakened immune system), family history of skin cancer, burns, and
exposure to arsenic and radiation.
BCCs are slow-growing tumors characterized by the progressive invasion
of adjacent tissues. These tumors are rarely lethal, and their potential to
metastasize is below 0.1%. Usually, the only BCCs that metastasize are
the ones that are neglected and not treated.
Basal cell carcinoma may have several different appearances on your skin.
The nodular BCC initially presents as a bump or nodule with blood vessels
on its surface. As the lesion progresses, it may form a non-healing sore.
The superficial BCC appears as a pink, scaly patch. Pigmented BCCs may
appear as the nodular or superficial variant, but with various amounts of
brown or black pigment. The sclerosing (morpheaform) BCC presents as a
pink or whitish hard area on the skin that is similar to a scar. This variant
has the most aggressive growth pattern out of all basal cell carcinomas. It
is therefore the hardest to treat. Fortunately, sclerosing basal cell
carcinomas represent only about 5% of all BCCs. The head and neck areas
are the most frequent locations of BCCs, but they can be found anywhere
on the skin.
Nevoid basal cell carcinoma syndrome (also known as basal cell nevus
syndrome and Gorlin syndrome) is a rare genetic condition characterized
by multiple abnormalities. It is caused by mutations in the patched gene
located on chromosome 9. The most common clinical manifestations of
nevoid basal cell carcinoma syndrome (NBCCS) include small indentations
or pits on palms and soles(seen in 87% of patients), multiple basal cell
carcinomas (seen in 80% of Caucasians, and 38% of African-Americans),
cavities in jaws(74%), and “coarse face”(54%). Multiple additional
abnormalities have also been described. X-rays of various bones, spine
and skull also show abnormal features.
The management of multiple basal cell carcinomas in NBCCS patients
presents a significant challenge. Multiple surgical procedures performed
with the use of traditional excision, as well as Mohs micrographic surgery
techniques are often a source of discomfort, pain, and disfigurement for
patients affected with NBCCS. CO2 laser resurfacing as well as imiqumod
cream may be used in the treatment of this condition.
53
The diagnosis of BCC needs to be confirmed by a skin biopsy. Treatment
options for this type of skin cancer include excision, Mohs micrographic
surgery, curettage and electrodessication, radiation therapy, cryosurgery,
and the use of imiquimod cream25.
Bazin, erythema induratum
Bazin disease (or "Erythema induratum") is a panniculitis on the back of the
calves.
It was formerly thought to be a reaction to the tuberculum bacillus. It is now
considered a panniculitis that is not associated with a single defined
pathogen.
It occurs mainly in women, but is very rare now.
Predisposing factors include abnormal amount of subcutaneous fat, thick
ankles and abnormally poor arterial supply. Abnormal arterial supply
causes low-grade ischemia of ankle region. The ankle skin becomes
sensitive to temperature changes. When weather is cold, ankle is cold, blue
and often tender. In hot weather, ankle becomes hot, edematous, swollen
and painful. Chilblains may be present. On palpation, small superficial and
painful nodules are felt. They break down to form small and multiple ulcers.
Fresh crops of nodules appear in periphery of ulcer and ultimately break
down. In nodular stage, pain is present; while it subsides in ulcerative
stage.
Birt–Hogg–Dube syndrome
Birt–Hogg–Dubé syndrome (BHD), also Hornstein–Birt–Hogg–Dubé
syndrome, Hornstein–Knickenberg syndrome, and fibrofolliculomas with
trichodiscomas and acrochordons is an autosomal dominant genetic
disorder that can cause susceptibility to kidney cancer, renal and
pulmonary cysts, and noncancerous tumors of the hair follicles, called
fibrofolliculomas. The symptoms seen in each family are unique, and can
include any combination of the three symptoms. Fibrofolliculomas are the
most common manifestation, found on the face and upper trunk in over
80% of people with BHD over the age of 40. Pulmonary cysts are equally
common (84%), but only 24% of people with BHD eventually experience a
25
Doctoroff A, Oberlender AS, Purcell SM. Full face carbon dioxide resurfacing in the management of a patient with the nevoid basal cell
carcinoma syndrome. Dermatol Surg, 2003;29(12):1236-1240
54
collapsed lung (spontaneous pneumothorax). Kidney tumors, both
cancerous and benign, occur in 14–34% of people with BHD; the
associated kidney cancers are often rare hybrid tumors.
Any of these conditions that occurs in a family can indicate a diagnosis of
Birt–Hogg–Dubé syndrome, though it is only confirmed by a genetic test for
a mutation in the FLCN gene, which codes for the protein folliculin. Though
its function is not fully understood, it appears to be a tumor suppressor
gene that restricts cell growth and division. Versions of FLCN have been
found in other animals, including fruit flies, German shepherds, rats, and
mice. The disease was discovered in 1977, but the connection with FLCN
was not elucidated until 2002, after kidney cancer, collapsed lungs, and
pulmonary cysts were all definitively connected to BHD.
Birt–Hogg–Dubé syndrome can manifest similarly to other diseases, which
must be ruled out when making a diagnosis. These include tuberous
sclerosis, which causes skin lesions similar to fibrofolliculomas, and Von
Hippel-Lindau disease, which causes hereditary kidney cancers. Once
diagnosed, people with BHD are treated preventatively, with monitoring of
kidneys and lungs using medical imaging. Fibrofolliculomas can be
removed surgically and pneumothorax and kidney cancer are treated
according to the normal standard of care.
Birt–Hogg–Dubé syndrome affects the skin and increases the risk of
tumors in the kidneys and lungs. The condition is characterized by multiple
noncancerous dome-shaped tumors of the hair follicles (fibrofolliculomas),
particularly on the face, neck, and—more rarely—the upper chest. The
fibrofolliculomas are generally described as having an opaque white color
or a yellowish tone and have a waxy, smooth texture. The tumors are
always found on and around the nose and on and behind the outer ear.
Typically, they first appear in a person's 20s or 30s, and are found in more
than 80% of people with the syndrome above the age of 40. The tumors
become larger and more numerous over time. Tumors differ between
individuals: they may appear merged in plaques, look similar to a comedo
with a plug of keratin, or include epidermoid cysts. A large number of
tumors on the face can be associated with hyperseborrhea (abnormally
elevated sebum production). The presence of fibrofolliculomas on a
person's face can cause significant psychological distress.
55
Other tumors can include trichodiscomas (tumors of the hair disc, which
may be identical to fibrofolliculomas), angiofibromas, and perifollicular
fibromas. However, angiofibromas are more common in tuberous sclerosis.
Along with the tumors, other skin conditions are seen in people with Birt–
Hogg–Dubé syndrome. Approximately 40% of people or families with the
disease have papules in their mouth, which can be located on the cheeks
(buccal mucosa), tongue, gums, or lips. Either white or mucosa-colored,
they are discrete, small, and soft and consist of fibrous tissue covered in
thickened epithelium. Collagenomas of the skin are also found in some
families. Many people with BHD have skin lesions that appear to be
acrochordons (skin tags), but may instead be fibrofolliculomas. These
lesions are usually found in the armpit, on the eyelids, and in folds of skin.
Not all individuals develop the facial tumors; some families with the
mutation that causes BHD develop only kidney tumors or spontaneous
pneumothorax.
People over 20 years of age with Birt–Hogg–Dubé syndrome have an
increased risk of developing slow-growing kidney tumors (chromophobe
renal carcinoma and renal oncocytoma, respectively), kidney cysts, and
possibly tumors in other organs and tissues. These tumors often occur in
both kidneys and in multiple locations in each kidney. The average number
of kidney tumors found in a person with BHD is 5.3, though up to 28 tumors
have been found. Hybrid oncocytoma/chromophobe carcinoma, found in
50% of cases, is the most commonly found cancer, followed by
chromophobe renal carcinoma, clear cell renal carcinoma, renal
oncocytoma, and papillary renal cell carcinoma. People over 40 years old
and men are more likely to develop kidney tumors, which are diagnosed at
a median age of 48. Kidney cancer associated with BHD have been
diagnosed in people at ages as young as 20.
In general, people with Birt–Hogg–Dubé syndrome are at roughly seven
times the risk of kidney cancer compared to the unaffected population.
Estimates of the incidence among people with the disease range from
14%–34%. Rarely, it is associated with clear cell renal cell carcinoma and
papillary renal cell carcinoma. If it develops in someone with BHD, renal
cell carcinoma occurs later in life and has a poor prognosis. Though the
types of tumor typically associated with BHD are considered less
aggressive, cases of advanced or metastatic kidney cancer have been
observed in people with the syndrome. Both benign and cancerous tumors
can reduce kidney function over time as they grow larger.
56
Along with fibrofolliculomas and kidney tumors, affected individuals
frequently develop cysts (blebs or bullae) in the subpleural lung base or
intraparenchymal space that may rupture and cause an abnormal collection
of air in the chest cavity (pneumothorax), which could result in the collapse
of a lung. The cysts do not cause other symptoms and lung function is
usually normal. More than 83% of people with Birt–Hogg–Dubé have cysts,
however, the syndrome does not cause conditions like progressive chronic
obstructive pulmonary disease (COPD) or generalized respiratory failure,
though it does cause emphysema. Spontaneous, sometimes recurrent,
pneumothorax occurs far more often and at a younger age with Birt–Hogg–
Dubé than in the unaffected population. Approximately 24% of people with
the disease suffer at least one spontaneous pneumothorax, 30 times the
occurrence in unaffected people. Though pneumothorax caused by Birt–
Hogg–Dubé often occurs in middle age, at a median age of 38, 17% of
affected people have a spontaneous pneumothorax before turning 40.
Pneumothoraces have been seen in people as young as 7 and 16 years of
age. Some families have a form of BHD that only affects the lungs.
Thyroid nodules have been associated with the Birt–Hogg–Dubé
phenotype, present in 65% of individuals and 90% of families with the
syndrome. However, a connection between BHD and thyroid cancer has
not been substantiated. Other conditions have been reported to be
associated but may not be caused by the mutation in FLCN or may not be
related at all.
These include multinodular goiter, medullary thyroid carcinoma, parotid
oncocytoma, colonic polyposis, connective tissue nevus, lipomas,
angiolipomas,
parathyroid
adenomas,
flecked
chorioretinopathy,
neurothekeoma, meningiomas, angiofibromas of the face, trichoblastomas,
cutaneous focal mucinosis, cutaneous leiomyoma, breast cancer, tonsillar
cancer, colorectal cancer, sarcoma of the leg, lung cancer, melanoma,
dermatofibrosarcoma protuberans, basal cell carcinoma, cutaneous
leiomyosarcoma, and squamous cell carcinoma.
Bloom’s syndrome
Bloom syndrome (often abbreviated as BS in literature), also known as
Bloom–Torre–Machacek syndrome, is a rare autosomal recessive disorder
characterized by short stature and predisposition to the development of
cancer. Cells from a person with Bloom syndrome exhibit a striking
57
genomic instability that includes excessive homologous recombination. The
condition was discovered and first described by New York dermatologist
Dr. David Bloom in 1954.
Bloom syndrome is a type of progeroid syndrome, and shows much of the
common characteristics, such as short stature and a rash that develops
early on in life when areas of the skin are exposed to the sun. The skin
rash is erythematous, telangiectatic, infiltrated, and scaly, and it appears in
the butterfly-shaped patch of skin across the nose and on the cheeks.
This rash can develop on other sun-exposed areas such as the backs of
the hands. Other clinical features include a high-pitched voice; distinct
facial features, such as a long, narrow face, micrognathism, and prominent
nose and ears; pigmentation changes of the skin including hypo- and
hyper-pigmented areas and cafe-au-lait spots; telangiectasias (dilated
blood vessels) which can appear on the skin but also in the eyes; moderate
immune deficiency, characterized by deficiency in certain immunoglobulin
classes, that apparently leads to recurrent pneumonia and ear infections.
Most individuals with Bloom syndrome are born with a low birth weight and
this can cause further health complications.
Hypogonadism is characterized by a failure to produce sperm, hence
infertility in males, and premature cessation of menses (premature
menopause), hence sub-fertility in females. However, several women with
Bloom syndrome have had children. Therefore, both men and women can
inherit Bloom syndrome and are both are equally like to inherit this rare
disease. Complications of the disorder may include chronic lung problems,
diabetes, and learning disabilities. In a small number of persons, there is
mental retardation. People with Bloom Syndrome also have a shortened life
expectancy meaning that the average person live to approximately 24
years old. Bloom syndrome shares many phenotypes with Fanconi anemia
and this may be because of overlap in the function of the proteins mutated
in this related disorder.
Boils (furunculosis)
A boil, also called a furuncle, is a deep folliculitis, infection of the hair
follicle. It is most commonly caused by infection by the bacterium
Staphylococcus aureus, resulting in a painful swollen area on the skin
caused by an accumulation of pus and dead tissue. Individual boils
clustered together are called carbuncles. Most human infections are
58
caused by coagulase-positive S. aureus strains, notable for the bacteria's
ability to produce coagulase, an enzyme that can clot blood. Almost any
organ system can be infected by S. aureus.
Boils are bumpy, red, pus-filled lumps around a hair follicle that are tender,
warm, and very painful. They range from pea-sized to golf ball-sized. A
yellow or white point at the centre of the lump can be seen when the boil is
ready to drain or discharge pus. In a severe infection, an individual may
experience fever, swollen lymph nodes, and fatigue. A recurring boil is
called chronic furunculosis. Skin infections tend to be recurrent in many
patients and often spread to other family members. Systemic factors that
lower resistance commonly are detectable, including: diabetes, obesity,
and hematologic disorders.Boils can be caused by other skin conditions
that cause the person to scratch and damage the skin.
Boils may appear on the buttocks or near the anus, the back, the neck, the
stomach, the chest, the arms or legs, or even in the ear canal.
Anyone can get boils but it is easier for a teenager or a young adult to get
boils than any other age.
Usually, the cause is bacteria such as staphylococci that are present on the
skin. Bacterial colonisation begins in the hair follicles and can cause local
cellulitis and inflammation. Additionally, myiasis caused by the Tumbu fly in
Africa usually presents with cutaneous furuncles. Risk factors for
furunculosis include bacterial carriage in the nostrils, diabetes mellitus,
obesity, lymphoproliferative neoplasms, malnutrition, and use of
immunosuppressive drugs. Patients with recurrent boils are as well more
likely to have a positive family history, take antibiotics, and to have been
hospitalised, anemic, or diabetic; they are also more likely to have
associated skin diseases and multiple lesions.
The most common complications of boils are scarring and infection or
abscess of the skin, spinal cord, brain, kidneys, or other organs. Infections
may also spread to the bloodstream (bacteremia) and become lifethreatening. S. aureus strains first infect the skin and its structures (for
example, sebaceous glands, hair follicles) or invade damaged skin (cuts,
abrasions). Sometimes the infections are relatively limited (such as a stye,
boil, furuncle, or carbuncle), but other times they may spread to other skin
areas (causing cellulitis, folliculitis, or impetigo). Unfortunately, these
59
bacteria can reach the bloodstream (bacteremia) and end up in many
different body sites, causing infections (wound infections, abscesses,
osteomyelitis, endocarditis, pneumonia) that may severely harm or kill the
infected person. S. aureus strains also produce enzymes and exotoxins
that likely cause or increase the severity of certain diseases. Such diseases
include food poisoning, septic shock, toxic shock syndrome, and scalded
skin syndrome. Almost any organ system can be infected by S. aureus.
A small boil may burst and drain on its own without any assistance.
Furuncles at risk of leading to serious complications should be incised and
drained. These include furuncles that are unusually large, last longer than
two weeks, or are located in the middle of the face or near the spine. Fever
and chills are signs of sepsis that require immediate treatment.
Antibiotic therapy is advisable for large or recurrent boils or those that
occur in sensitive areas (such as around or in the nostrils or in the ear).
Staphylococcus aureus has the ability to acquire antimicrobial resistance
easily, making treatment difficult. Knowledge of the antimicrobial resistance
of S. aureus is important in the selection of antimicrobials for treatment.
Borrelia burgdorferi infection
Borrelia burgdorferi is a bacterial species of the spirochete class of the
genus Borrelia. B. burgdorferi exists in North America and Europe and is
the predominant causative agent of Lyme disease. Borrelia species are
considered diderm (double-membrane) bacteria rather than gram positive
or negative.
Lyme disease is a zoonotic, vector-borne disease transmitted by the Ixodes
tick (also the vector for Babesia); the causative agent is named after the
researcher Willy Burgdorfer, who first isolated the bacterium in 1982. B.
burgdorferi is one of the few pathogenic bacteria that can survive without
iron, having replaced all of its iron-sulfur cluster enzymes with enzymes
that use manganese, thus avoiding the problem many pathogenic bacteria
face in acquiring iron.
B. burgdorferi infections have been linked to non-Hodgkin lymphomas.
Clinical presentation of Lyme disease may include the characteristic bull's
eye rash and erythema chronicum migrans (a rash which spreads
60
peripherally and spares the central part), as well as myocarditis,
cardiomyopathy, arrythmia, arthritis, arthralgia, meningitis, neuropathies
and facial nerve palsy.
It can be found around the world, but it is especially common in the United
States, particularly in the northeastern, midwest and western regions.
Bowen’s disease
Bowen's disease (BD) (also known as "squamous cell carcinoma in situ") is
a neoplastic skin disease; it can be considered as an early stage or
intraepidermal form of squamous cell carcinoma. It was named after John
T. Bowen. (Erythroplasia of Queyrat is a particular type of squamous cell
carcinoma in situ which can arise on the glans or prepuce in males and
vulva in females, and may be induced by HPV.)
Causes of BD include solar damage, arsenic, immunosuppression
(including AIDS), viral infection (human papillomavirus or HPV), chronic
skin injury, and other dermatoses.
Bowen's disease typically presents as a gradually enlarging, welldemarcated erythematous plaque with an irregular border and surface
crusting or scaling. BD may occur at any age in adults, but is rare before
the age of 30 years; most patients are aged over 60. Any site may be
affected, although involvement of palms or soles is uncommon. BD occurs
predominantly in women (70-85% of cases). About 60-85% of patients
have lesions on the lower leg, usually in previously or presently sunexposed areas of skin.
This is a persistent, progressive, non-elevated, red, scaly or crusted plaque
which is due to an intraepidermal carcinoma and is potentially malignant.
The lesions may occur anywhere on the skin surface, including on mucosal
surfaces. Freezing, cauterization or diathermy coagulation is often effective
treatment.
Bromoderma
Bromoderma, also known as bromoderma tuberosum, is a dermatological
condition characterized by an eruption of papules and pustules on the skin.
It is caused by hypersensitivity to bromides, such as those found in certain
drugs.
61
Café-au-lait macules
Cafe-au-lait spots are light tan or light brown spots that are usually oval in
shape. They usually appear at birth but may develop in the first few years
of a child's life. Cafe-au-lait spots may be a normal type of birthmark, but
the presence of several cafe-au-lait spots larger than a quarter may occur
in neurofibromatosis (a genetic disorder that causes abnormal cell growth
of nerve tissues).
There is no known way to prevent birthmarks. People with birthmarks
should use a good quality sunscreen with an SPF of 30 or more when
outdoors in order to prevent complications.
Calcinosis
Calcinosis is the formation of calcium deposits in any soft tissue.
The most common type of calcinosis is dystrophic calcification. This type of
calcification can occur as a response to any soft tissue damage, including
that involved in implantation of medical devices.
Metastatic calcification involves a systemic calcium excess imbalance,
which can be caused by hypercalcemia, renal failure, milk-alkali syndrome,
lack or excess of other minerals, or other etiologies.
The etiology of the rare condition of tumoral calcinosis is not entirely
understood. It is generally characterized by large, globular calcifications
near joints.
Calciphylaxis
The skin disease Calciphylaxis is disorder that characterized with
progressive cutaneous necrosis associated with small- and medium-sized
vessel calcification occurring in the setting of end-stage renal disease,
diabetes mellitus, and hyperparathyroidism. The necrotic tissue presents
with areas of the skin that progress to gangrene and ulceration of the
subcutaneous fat, dermis, and epidermis; secondary infection and sepsis
are common.
The pathogenesis is poorly understood. In animal models, calciphylaxis is
described as a condition of induced systemic hypersensitivity in which
tissues respond to appropriate challenging agents with calcium deposition.
Calciphylaxis is associated with chronic renal failure, secondary
62
hyperparathyroidism, and an elevated calcium phosphate end product.
Implicated "challenging agents" include glucocorticoids, albumin infusions,
intramuscular tobramycin, iron dextran complex, calcium heparinate,
immunosuppressive agents, and vitamin D.
Because this condition involves necrotic tissue it is contraindicated for
massage.
Calciphylaxis most often occurs on the lower limb especially in fatty areas.
Lesions on the trunk, abdomen, buttocks or thighs, appear to be more
dangerous than lesions on the lower legs and feet.
63
Campbell de Morgan spots
Cherry angiomas, also known as Campbell De Morgan spots or Senile
angiomas, are cherry red papules on the skin containing an abnormal
proliferation of blood vessels. They are the most common kind of angioma.
They are called Campbell de Morgan spots after the nineteenth-century
British surgeon Campbell De Morgan, who first noted and described them.
The frequency of cherry angiomas increases with age.
Cherry angiomas are made up of clusters of capillaries at the surface of the
skin, forming a small round dome ("papule"), which may be flat topped.
They range in colour from bright red to purple. When they first develop,
they may be only a tenth of a millimeter in diameter and almost flat,
appearing as small red dots. However, they then usually grow to about one
or two millimeters across, and sometimes to a centimeter or more in
diameter. As they grow larger, they tend to expand in thickness, and may
take on the raised and rounded shape of a dome. Multiple adjoining
angiomas are said to form a polypoid angioma. Because the blood vessels
comprising an angioma are so close to the skin's surface, cherry angiomas
may bleed profusely if they are injured.
One study found that the majority of capillaries in cherry hemangiomas are
fenestrated because of staining for carbonic anhydrase activity.
Cherry angiomas appear spontaneously in many people in middle age but
can also, although less common, occur in young people. They can also
occur in an aggressive eruptive manner in any age. The underlying cause
for the development of cherry angiomas is not understood, probably due to
a lack of interest in the subject, given that they are completely benign
entities and have no malignant potential.
Candida Albicans
Candidiasis is a fungal infection caused by yeasts that belong to the genus
Candida. There are over 20 species of Candida yeasts that can cause
infection in humans, the most common of which is Candida albicans.
Candida yeasts normally live on the skin and mucous membranes without
causing infection; however, overgrowth of these organisms can cause
symptoms to develop. Symptoms of candidiasis vary depending on the
area of the body that is infected.
64
Candidiasis that develops in the mouth or throat is called “thrush” or
oropharyngeal candidiasis. Candidiasis in the vagina is commonly referred
to as a “yeast infection.” Invasive candidiasis occurs when Candida species
enter the bloodstream and spread throughout the body.
Oropharyngeal / Esophageal Candidiasis ("Thrush")
Candidiasis that develops in the mouth or throat is called "thrush" or
oropharyngeal candidiasis. The most common symptom of oral thrush is
white patches or plaques on the tongue and other oral mucous
membranes. This infection is uncommon among healthy adults.
Candidiasis of the mouth and throat, also known as “thrush" or
oropharyngeal candidiasis, is a fungal infection that occurs when there is
overgrowth of a yeast called Candida. Candida yeasts normally live on the
skin or mucous membranes in small amounts. However, if the environment
inside the mouth or throat becomes imbalanced, the yeasts can multiply
and cause symptoms. Candida overgrowth can also develop in the
esophagus, and this is called Candida esophagitis, or esophageal
candidiasis.
Candida infections of the mouth and throat can manifest in a variety of
ways. The most common symptom of oral thrush is white patches or
plaques on the tongue and other oral mucous membranes. Other
symptoms include:
Redness or soreness in the affected areas
Difficulty swallowing
Cracking at the corners of the mouth (angular cheilitis)
It is important to see your doctor if you have any of these symptoms.
Candida infections of the mouth and throat are uncommon among adults
who are otherwise healthy. Oral thrush occurs most frequently among
babies less than one month old, the elderly, and groups of people with
weakened immune systems. Other factors associated with oral and
esophageal candidiasis include:
HIV/AIDS
Cancer treatments
Organ transplantation
Diabetes
Corticosteroid use
Dentures
65
Broad-spectrum antibiotic use
Prevention of Oral Candidiasis
Good oral hygiene practices may help to prevent oral thrush in people with
weakened immune systems. Some studies have shown that chlorhexidine
(CHX) mouthwash can help to prevent oral candidiasis in people
undergoing cancer treatment. People who use inhaled corticosteroids may
be able to reduce the risk of developing thrush by washing out the mouth
with water or mouthwash after using an inhaler.
Candida species are normal inhabitants of the mouth, throat, and the rest
of the gastrointestinal tract. Usually, Candida yeasts live in and on the body
in small amounts and do not cause any harm. However, the use of certain
medications or a weakening of the immune system can cause Candida to
multiply, which may cause symptoms of infection.
The infection is not very common in the general population. It is estimated
that between 5% and 7% of babies less than one month old will develop
oral candidiasis. The prevalence of oral candidiasis among AIDS patients
is estimated to be between 9% and 31%, and studies have documented
clinical evidence of oral candidiasis in nearly 20% of cancer patients.
Candida infections of the mouth and throat must be treated with
prescription antifungal medication. The type and duration of treatment
depends on the severity of the infection and patient-specific factors such as
age and immune status. Untreated infections can lead to a more serious
form of invasive candidiasis.
Oral candidiasis usually responds to topical treatments such as
clotrimazole troches and nystatin suspension (nystatin “swish and
swallow”). Systemic antifungal medication such as fluconazole or
itraconazole may be necessary for oropharyngeal infections that do not
respond to these treatments.
Candida esophagitis is typically treated with oral or intravenous fluconazole
or oral itraconazole. For severe or azole-resistant esophageal candidiasis,
treatment with amphotericin B may be necessary.
66
Invasive candidiasis
Invasive candidiasis is a fungal infection that can occur when Candida
yeasts enter the bloodstream. Once the fungus is in the bloodstream, it can
spread to other parts of the body and cause infection.
The symptoms of invasive candidiasis are not specific. Fever and chills that
do not improve after antibiotic therapy are the most common symptoms. If
the infection spreads to other organs or parts of the body such as kidneys,
liver, bones, muscles, joints, spleen, or eyes, additional symptoms may
develop, which vary depending on the site of infection. If the infection does
not respond to treatment, the patient’s organs may stop working.
Candidemia (a bloodstream infection with Candida), is the fourth most
common bloodstream infection among hospitalized patients in the United
States. People at high risk for developing candidemia include:
Intensive care unit (ICU) patients
Surgical patients
Patients with a central venous catheter
People whose immune systems are weakened (such as people with
HIV/AIDS)
Very low-birth-weight infants
Preventing Invasive Candidiasis
Antifungal prophylaxis may be appropriate for some groups of people who
are at high risk of developing candidemia, such as low-birth-weight infants.
Doctors and nurses can follow CDC-recommended infection control steps
every time they work with a central line.
Patients and caregivers can ask if a central line is needed and, if so, how
long it should stay in place. They can also make sure that healthcare
professionals wash their hands before they care for the central line.
Patients should speak up if the skin around the central line becomes sore
or red, or if their bandages are wet or dirty.
People at Risk for Invasive Candidiasis
Candidemia (a bloodstream infection with Candida), is the fourth most
common bloodstream infection among hospitalized patients in the United
States. People at high risk for developing candidemia include:
Intensive care unit (ICU) patients
67
Surgical patients
Patients with a central venous catheter
People whose immune systems are weakened (such as people with
HIV/AIDS)
Very low-birth-weight infants
Preventing Invasive Candidiasis
Antifungal prophylaxis may be appropriate for some groups of people who
are at high risk of developing candidemia, such as low-birth-weight infants.
Doctors and nurses can follow CDC-recommended infection control steps
every time they work with a central line.
Patients and caregivers can ask if a central line is needed and, if so, how
long it should stay in place. They can also make sure that healthcare
professionals wash their hands before they care for the central line.
Patients should speak up if the skin around the central line becomes sore
or red, or if their bandages are wet or dirty.
Candida yeasts normally live in and on the body without causing any
symptoms. In people at risk, invasive candidiasis may occur when a
person’s own Candida yeasts enter the bloodstream. This can also happen
if medical equipment or devices, particularly intravenous (IV) catheters,
become contaminated with Candida. In either case, the infection may
spread through the bloodstream and infect various organs.
Invasive candidiasis is extremely rare in people without risk factors, but it is
the fourth most common cause of hospital-acquired bloodstream infections
in the U.S. In the general population, the incidence is 8 to 10 cases per
100,000 people. A higher incidence has been observed among
Blacks/African-Americans and babies less than one month old. It is
estimated that between 5% and 20% of newborns that weigh less than
1000 grams (2.2 pounds) at birth develop invasive candidiasis.
Invasive candidiasis requires treatment with oral or intravenous (IV)
antifungal medication for several weeks. The type and duration of
antifungal treatment will depend on patient-specific factors such as age,
immune status, and severity of infection. Treatment of invasive candidiasis
should include prompt removal of catheters.
68
Neonates with invasive candidiasis should be treated with amphotericin B
for at least 3 weeks. For clinically stable children and adults, fluconazole or
an echinocandin (caspofungin, micafungin, or anidulafungin) is the
recommended form of therapy. In critically ill patients, an echinocandin or a
lipid formulation of amphotericin B is recommended. Treatment should
continue for 2 weeks after signs and symptoms of candidemia have
resolved and the Candida yeasts have been cleared from the bloodstream.
Capillaritis
Capillaritis is characterized by leakage of red blood cells from small,
superficial blood vessels that results in pinpoint-like hemorrhages
(petechiae). Capillaritis is frequently found in patients with long periods of
extended standing related to their occupations.
A skin hypersensitivity reaction, salicylates and nonsteroidal antiinflammatory drugs (NSAIDs) are the most commonly associated origins of
capillaritis, though the precise cause is unclear. Capillaritis is usually a lifelong condition, flaring intermittently.
Capillaritis is seen more frequently in adults, but it does occur in older
children and adolescents.
The most common location for capillaritis is the leg, though it may manifest
on the trunk and upper extremities. Capillaritis never presents on the face.
Presentation may include:
Brown-red or deeply pigmented, pepper-like petechiae in dark-skinned
individuals
Cayenne-pepper–colored petechiae in lighter-skinned individuals
Color variations in the lesions due to different stages of blood breakdown
product (hemosiderin) reabsorption.
Carbuncles
A carbuncle is a skin infection that often involves a group of hair follicles.
The infected material forms a lump, which occurs deep in the skin and may
contain pus.
When there is more than one carbuncle, the condition is called
carbunculosis.
69
Most carbuncles are caused by the bacteria staphylococcus aureus. The
infection is contagious. This means it can spread to other areas of the body
or other people.
A carbuncle is made up of several skin boils (furuncles). The infected mass
is filled with fluid, pus, and dead tissue. Fluid may drain out of the
carbuncle, but sometimes the mass is so deep that it cannot drain on its
own.
Carbuncles can develop anywhere. But they are most common on the back
and the nape of the neck. Men get carbuncles more often than women.
Because the bacteria that causes the condition is contagious, family
members may develop carbuncles at the same time. Often, the cause of a
carbuncle cannot be determined.
Carotenaemia
Carotenaemia (xanthaemia) is the presence in blood of the orange pigment
carotene from excessive intake of carrots or other vegetables containing
the pigment resulting in increased serum carotenoids. Carotenoids are
lipid-soluble compounds that include alpha- and beta-carotene, betacryptoxanthin, lycopene, lutein, and zeaxanthin. The primary serum
carotenoids are beta-carotene, lycopene, and lutein. Serum levels of
carotenoids vary between region, ethnicity, and sex in the healthy
population. All are absorbed by passive diffusion from the gastrointestinal
tract and are then partially metabolized in the intestinal mucosa and liver to
vitamin A. From there they are transported in the plasma into the peripheral
tissues. Carotenoids are eliminated via sweat, sebum, urine, and
gastrointestinal secretions. Carotenoids contribute to normal-appearing
human skin color and are a significant component of physiologic ultraviolet
photoprotection.
Carotenemia is a benign condition most commonly occurring in vegetarians
and young children.
Casal necklace
Also known as Casal Collar, it is a dermatitis partly or completely encircling
the lower part of the neck in pellagra, a vitamin deficiency disease most
70
frequently caused by a chronic lack of niacin (vitamin B3 or synonym:
vitamin PP (from: Anti-Pellagra)) in the diet.
It appears as a rash, either red or brown, that appears around the lower
part of the neck.
Cellulitis and Erysipelas
Erysipelas and cellulitis are acute, spreading infections of dermal and
subcutaneous tissues, characterized by a red, hot, tender area of skin,
often at the site of bacterial entry, caused most frequently by group A βhemolytic streptococci (erysipelas) or Staphylococcus aureus.
After entry, infection spreads to tissue spaces and cleavage planes as
hyaluronidases break down polysaccharide ground substances,
fibrinolysins digest fibrin barriers, lecithinases destroy cell membranes.
Local tissue devitalization, e.g., trauma, is usually required to allow for
significant anaerobic bacterial infection. The number of infecting organisms
is usually small, suggesting that cellulitis may be more of a reaction to
bacterial superantigens than to over-whelming tissue infection.
A spreading hot, bright red circumscribed area on the skin with a sharp
raised border accompanied by high fever and a feeling of general illness.
Erysipelas in most cases affects the skin of the face, that is why when it
strikes other parts of the body, it may often be misdiagnosed. Bacteremia
(blood poisoning) and pneumonia are the most common complications.
Erysipelas is a highly contagious disease that was formerly dangerous to
life; however, it can now be quickly controlled by antibiotic therapy.
71
Cheilitis
Cheilitis (pronounced /kaɪˈlaɪtɪs/) is inflammation of the lips. This
inflammation may include the perioral skin (the skin around the mouth), the
vermilion border, and/or the labial mucosa. The skin and the vermilion
border are more commonly involved, as the mucosa is less affected by
inflammatory and allergic reactions.
It is a general term, and there are many recognized types and different
causes. Patch testing may identify allergens that cause cheilitis.
Cheilitis can be either acute or chronic. Most cheilitis is caused by
exogenous factors such as dryness (chapping) and acute sun exposure.
Cheilitis may be divided into the following types:
Chapped lips
Chapped lips (also cheilitis simplex or common cheilitis) are characterized
by cracking, fissuring, and peeling of the skin of the lips, and are one of the
most common types of cheilitis. While both lips may be affected, the lower
lip is the most common site. There may also be burning or the formation of
large, painful cracks when the lips are stretched. If chronic, cheilitis simplex
can progress to crusting and bleeding.
Lip licking, biting, or rubbing habits are frequently involved. Paradoxically,
constant licking of the lips causes drying and irritation, and eventually the
mucosa splits or cracks. Lips normally have a very thin oily film on their
surface that provides natural protection against moisture loss. If this film is
removed, often due to lip licking habits, this causes the lips to become
chapped. The lips have a greater tendency to dry out in cold, dry weather.
Digestive enzymes present in saliva may also irritate the lips, and the
evaporation of the water in saliva saps moisture from them.
Some children have a habit of sucking and chewing on the lower lip,
producing a combination of cheilitis and sharply demarcated perioral
erythema (redness).
Treatment is usually successful with barrier lubricants, such as lip salve or
Vaseline. Medical grade (USP) lanolin accelerates repair of the lips, and is
used in some lip repair products. Some complementary and alternative
medicine sources claim that nasal sebum can be used as a remedy.
72
Sometimes the term "cheilitis simplex" is used as a synonym for cheilitis
generally, however, exfoliative cheilitis is also sometimes stated to be the
equivalent of chapped lips.
Actinic cheilitis
Also termed "solar cheilosis", this condition is the result of chronic overexposure to ultraviolet radiation in sunlight. It usually occurs on the lower
lip, which is dry, scaling, and wrinkled grey-white in appearance. It is
especially common in people with light skin types who live in sunny
climates (e.g., Australians of European ancestry), and in persons who
spend a lot of time outdoors. There is a small risk that this condition can
develop into squamous cell carcinoma in the long term, but lip cancer is
usually noticed early and hence has a good prognosis compared to oral
cancer generally.
Angular cheilitis
Angular cheilitis- inflammation of the corner of the mouth.
Angular cheilitis (angular stomatitis) is inflammation of one or both of the
corners (angles) of the mouth. It is a fairly common condition, and often
affects elderly people.
There are many possible causes, including nutritional deficiencies (iron, B
vitamins, folate), contact allergy, infection (Candida albicans,
Staphylococcus aureus or β-hemolytic streptococci) and edentulism (often
with overclosure of the mouth and concomitant denture-related stomatitis),
and others.
Eczematous cheilitis
Also termed "lip dermatitis", eczematous cheilitis is a diverse group of
disorders which often have an unknown cause. Chronic eczematous
reactions account for the majority of chronic cheilitis cases.
It is divided into endogenous (due to an inherent characteristic of the
individual), and exogenous (where it is caused by an external agent). The
main cause of endogenous eczematous cheilitis is atopic cheilitis (atopic
dermatitis), and the main causes of exogenous eczematous cheilitis is
irritant contact cheilitis (e.g., caused by a lip-licking habit) and allergic
contact cheilitis. The latter is characterized by a dryness, fissuring, edema,
73
and crusting. It affects females more commonly than males, in a ratio of
about 9:1.
The most common causes of allergic contact cheilitis is lip cosmetics,
including lipsticks and lipbalm, followed by toothpastes. A lipstick allergy
can be difficult to diagnose in some cases as it is possible that cheilitis can
develop without the person even wearing lipstick. Instead, small exposure
such as kissing someone who is wearing lipstick is enough to cause the
condition.
Allergy to Balsam of Peru can also manifest as cheilitis. Allergies to metal,
wood, or other components can cause cheilitis reactions in musicians,
especially players of woodwind and brass instruments, e.g., the so-called
"clarinetist's cheilitis", or "flutist's cheilitis". "Pigmented contact cheilitis" is
one type of allergic cheilitis in which a brown-black discoloration of the lips
develops.
Infectious cheilitis
Infectious cheilitis refers to cheilitis caused by infectious disease. The
terms "Candidal cheilitis" and "bacterial cheilitis" are sometimes used,
denoting the involvement of Candida organisms and bacterial species
respectively. The term "cheilocandidiasis" describes exfoliative (flaking)
lesions of the lips and the skin around the lips, and is caused by a
superficial candidal infection due to chronic lip licking. Impetigo (caused by
Streptococcus pyogenes and/or Staphylococcus aureus), can manifest as
an exfoliative cheilitis-like appearance.
Herpes labialis (cold sore) is a common cause of infectious cheilitis. A
lesion caused by recurrence of a latent herpes simplex infection can occur
in the corner of the mouth, and be mistaken for other causes of angular
cheilitis. In fact this is herpes labialis, and is sometimes termed "angular
herpes simplex"26.
Granulomatous cheilitis
Orofacial granulomatosis is enlargement of lips due to the formation of noncaseating granulomatous inflammation, which obstruct lymphatic drainage
of the orofacial soft tissues, causing lymphedema. Essentially,
granulomatous cheilitis refers to the lip swelling that accompanies this
26
Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 141, 142,
163, 689, 713. ISBN 0721690033.
74
condition. "Median cheilitis" may be seen, which is fissuring in the midline
of the lips due to the enlargement of the lips. Angular cheilitis may also be
associated with orofacial granulomatosis.
A related condition is Melkersson–Rosenthal syndrome, a triad of facial
palsy, chronic lip edema, and fissured tongue. "Miescher’s cheilitis", and
"granulomatous macrocheilitis", are synonyms of granulomatous cheilitis.
Drug-related cheilitis
Common causes of drug-related cheilitis include Etretinate, Indinavir,
Protease inhibitors, Vitamin A and Isotretinoin (a retinoid drug). Uncommon
causes include Atorvastatin, Busulphan, Clofazimine, Clomipramine,
Cyancobalamin, Gold, Methyldopa, Psoralens, Streptomycin, Sulfasalazine
and Tetracycline. A condition called "drug-induced ulcer of the lip" is
described as being characterized by painful or tender, well-defined
ulcerations of the lip without induration. It is the result of oral administration
of drugs, and the condition resolves when the drugs are stopped.
Chloasma (melasma)
Cholasma, also known as Melasma (Greek: "a black spot") is an acquired
light - or dark-brown hyperpigmentation that occurs in the exposed areas,
most often on the face, and results from exposure to sunlight; may be
associated with pregnancy, with ingestion of contraceptive hormones, or
possibly with certain medications such as diphenylhydantoin, or may be
idiopathic.
Nobody knows exactly what causes Melasma. Estrogen preparations
alone, however, given to postmenopausal women do not cause melasma,
despite sun exposure. However, pregnancy causes melasma, and
combinations of estrogen and progestational agents, as used for
contraception, are the most frequent cause of melasma.
A uniform brown color is usually seen over the cheeks, forehead, nose, or
upper lip. It is most often symmetrical (matching on both sides of the face).
Massage is not contraindicated.
75
Chloracne
Chloracne is an acne-like eruption of blackheads, cysts, and pustules
associated with over-exposure to certain halogenated aromatic
compounds, such as chlorinated dioxins and dibenzofurans. The lesions
are most frequently found on the cheeks, behind the ears, in the armpits
and groin region.
The condition was first described in German industrial workers in 1897 by
von Bettman, and was initially believed to be caused by exposure to
chlorine (hence the name "chloracne"). It was only in the mid-1950s that
chloracne was associated with aromatic hydrocarbons. The substances
that may cause chloracne are now collectively known as chloracnegens.
Chloracne is particularly linked to toxic exposure to dioxins (byproducts of
many chemical processes, including the manufacture of herbicides such as
Agent Orange)—so much so that it is considered a clinical sign of dioxin
exposure. The severity and onset of chloracne may follow a typical
asymptotic dose-response relationship curve.
hloracne normally results from direct skin contact with chloracnegens,
although ingestion and inhalation are also possible causative routes.
76
Chloracnegens are fat-soluble, meaning they persist in the body fat for a
very long period following exposure. Chloracne is a chronic inflammatory
condition that results from this persistence, in combination with the toxin's
chemical properties. It is believed, at least from rodent models, that the
toxin activates a series of receptors promoting macrophage proliferation,
inducing neutrophilia and leading to a generalised inflammatory response
in the skin. This process may also be augmented by induction of excess
tumor necrosis factor in the blood serum.
The inflammatory processes lead to the formation of keratinous plugs in
skin pores, forming yellowish cysts and dark pustules. The associated pus
is usually greenish in color. The skin lesions occur mainly in the face, but in
more severe cases they involve the shoulders and chest, the back, and the
abdomen. In advanced cases, the lesions appear also on the arms, thighs,
legs, hands and feet.
In some instances, chloracne may not appear for three to four weeks after
toxic exposure; however, in other cases—particularly in events of massive
exposure—the symptoms may appear within days.
Once chloracne has been identified, the primary action is to remove the
patient and all other individuals from the source of contamination. Further
treatment is symptomatic.
Severe or persistent lesions may be treated with oral antibiotics or
isotretinoin. However, chloracne may be highly resistant to any treatment.
The course of the disease is highly variable. In some cases the lesions may
disappear within two years or so; however, in other cases the lesions may
be effectively permanent (mean duration of lesions in one 1984 study was
26 years, with some workers remaining disfigured over three decades after
exposure).
Cholinergic urticaria
Cholinergic urticaria (CU) is one of the physical urticaria (commonly
referred to as hives), which is provoked during sweating events.
The term cholinergic is derived from the finding that hives similar to those
of CU can be evoked using cholinergic agonists (e.g. methacholine).
77
CU typically presents with a number of small, short-lasting hives but may
also involve cutaneous inflammation (wheals) and pain which develops
usually in response to exercise, bathing, staying in a heated environment,
or emotional stress. Although the symptoms subside rapidly, commonly
within 1 hour, CU may significantly impair quality of life, especially in
relation to sporting and sexual activities.
Though overall research is limited, various studies indicate that CU is
relatively common across populations with prevalence rates reportedly
ranging from 5% to 20% (depending on locale, race, and age). The
condition is more common in young adults, and prevalence appears to
peak in adult aged 26–28 (up to 20%). The vast majority of cases are
reported to be mild, and proportionally few individuals seek medical
attention regarding the condition.
Cimex lectularius
Also known as “Bed Bugs”. Bed bugs are parasitic insects of the cimicid
family that feed exclusively on blood. Cimex lectularius, the common bed
bug, is the best known as it prefers to feed on human blood although other
Cimex species are specialized to other animals, e.g., bat bugs, Cimex
pipistrelli (Europe), Cimex pilosellus (western US), and Cimex adjunctus
(entire eastern US).
The name of the "bed bug" is derived from the preferred habitat of Cimex
lectularius: warm houses and especially nearby or inside of beds and
bedding or other sleep areas. Bed bugs are mainly active at night, but are
not exclusively nocturnal. They usually feed on their hosts without being
noticed.
A number of adverse health effects may result from bed bug bites,
including skin rashes, psychological effects, and allergic symptoms. They
are not known to transmit any pathogens as disease vectors. Certain signs
and symptoms suggest the presence of bed bugs; finding the insects
confirms the diagnosis.
Bed bugs have been known as human parasites for thousands of years. At
a point in the early 1940s, they were mostly eradicated in the developed
world, but have increased in prevalence since 1995. Because infestation of
human habitats has been on the increase, bed bug bites and related
conditions have been on the rise as well.
78
Bed bugs can cause a number of health effects, including skin rashes,
psychological effects, and allergic symptoms. They are able to be infected
by at least 28 human pathogens, but no study has clearly found that the
insect is able to transmit the pathogen to a human being. Bed bug bites or
cimicosis may lead to a range of skin manifestations from no visible effects
to prominent blisters.
Diagnosis involves both finding bed bugs and the occurrence of compatible
symptoms. Treatment involves the elimination of the insect and measure to
help with the symptoms until they resolve. They have been found with
methicillin-resistant Staphylococcus aureus (MRSA) and with vancomycinresistant Enterococcus faecium (VRE), but the significance of this is still
unknown.
Congenital Erythropoietic Protoporphyria
Erythropoietic protoporphyria is a form of porphyria, which varies in severity
and can be very painful. It arises from a deficiency in the enzyme
ferrochelatase, leading to abnormally high levels of protoporphyrin in the
tissue. The severity varies significantly from individual to individual.
Both autosomal dominant and autosomal recessive inheritance have been
reported with this disorder as has an acquired form of the disease. A
clinically similar form of porphyria, known as X-Linked dominant
protoporphyria, was identified in 2008.
A common symptom is very painful photosensitivity, manifesting itself as a
burning and itching sensation on the surface of the skin. At times the
itching sensations are almost unbearable. Rubbing the affected areas with
ice can be the only relief, and that is only temporary. The usual anti-itch
remedies, including cortisone anti-histamine topical preparations, and
Calomine lotion generally provide little or no relief. If a patient presents with
a history of anti-itch preparation inefficacy, Erythropoietic protoporphyria
should be considered.
Erythropoietic protoporphyria usually first presents in childhood, and most
often affects the face and the upper surfaces of the arms, hands, and feet
and the exposed surfaces of the legs. Most patients, if the Erythropoietic
protoporphyria is not as severe, manifest symptoms with onset of puberty
when the male and female hormone levels elevate during sexual
79
development and maintenance. More severe Erythropoietic protoporphyria
can manifest in infancy. Exposure to even indoor light sources can cause
the reaction, and the infant, if clothed only in a diaper, will break out
everywhere except under the diaper. Erythropoietic protoporphyria can be
triggered through exposure to sun even though the patient is behind glass.
Even the UV emissions from arc welding with the use of full protective
mask have been known to trigger Erythropoietic protoporphyria.
Erythropoietic protoporphyria can also manifest between the ages of 3 and
6.
Exposure to powerful surgical lights is more than enough to trigger the
reaction. As a precaution, individuals with Erythropoietic protoporphyria
should tell their close friends and family to make sure that if they ever are
taken to the hospital for emergency surgery that the staff be notified of the
condition so they can adjust the lighting accordingly.
In the late 1990s, Erythropoietic protoporphyria was cured in rats. More
than likely it will be cured as a byproduct of another more common disease
being cured.
Prolonged exposure to the sun can lead to edema and blistering, especially
on the nose. At times the immediate damage can be so severe that the
individual can lose the skin in sheets. After many years, chronically sunexposed skin may become thick and wrinkled if no beta carotene and other
carotenoids and no lutein and other xanthophylls are ingested.
Erythropoietic protoporphyria can lead to abdominal pain, which may
manifest as generalized pain, or may imitate appendicitis. Some healthy
appendices have been removed due to this mimic. Since porphyria is not
that common, most doctors don't even think to check blood porphyrin levels
when symptoms present. For doctors that are familiar with porphyria, it is
generally considered insignificant and irrelevant compared to the possibility
of a pending burst appendix, especially since porphyrin levels cannot
generally be immediately measured due to lab protocols.
Moderate and severe cases can present with pelvic and shoulder girdle
muscle weakness. This is because porphyrins are poisonous to the body
and produce nerve damage. Damage to nerves of the digestive system not
only cause nerve pain in the abdominal area, but also cause slow
movement of the bowels, especially the large bowel. Patients can therefore
80
develop a larger than normal diameter of the large bowel, at times causing
a condition called megacolon. The damage of nerves to the esophagus and
to the stomach valve muscles (sphincters) can cause stomach reflux. One
of the ironies of these digestive condition is that one of the medical
treatments of these digestive conditions is Reglan, to which some
porphyrics have a very strong adverse reaction.
Porphyrin toxins are neurotropic and shut down the nerve trunks one by
one until the individual has difficulty with fine motor tasks, like turning
phonebook pages, has difficulty speaking (develops dystonic speech that is
almost unintelligible), and develops difficulty breathing. The porphyrin
neurotoxins have caused some patients to present to the Emergency Room
not only in pain but also seeming to be neurotic, or even psychotic. Once
glucose is infused, those episodes subside, and if they don't, healthy red
blood cell infusion in whole also helps, due to the naturally occurring
glucose in the infused blood. These patients will often present with a very
enlarged spleen due to having to process defective red blood cells. At
times poking around on the spleen can cause elevation of body
temperature by at least two degrees Fahrenheit. The liver may also be
tender.
People with Erythropoietic protoporphyria are also at increased risk to
develop gallstones. One study has noted that Erythropoietic protoporphyria
patients suffer from vitamin D deficiency.
Crab lice
Crab lice, also known as "pubic or crab louse” is another offshoot of the
original louse and is adapted to body hair. Humans have the dubious
honor of being the only known host of this parasite. Aren’t we AWESOME?
Cryptococcus neoformans
Cryptococcus neoformans is an encapsulated yeast that can live in both
plants and animals. Its teleomorph is Filobasidiella neoformans, a
filamentous fungus belonging to the class Tremellomycetes. It is often
found in pigeon excrement.
Cryptococcus neoformans is composed of two varieties (v.): C. neoformans
v. neoformans and v. grubii. A third variety, C. neoformans v. gattii, is now
considered a distinct species, Cryptococcus gattii. C. neoformans v. grubii
and v. neoformans have a worldwide distribution and are often found in soil
81
that has been contaminated by bird excrement. The genome sequence of
C. neoformans v. neoformans was published in 2005. Recent studies
suggest that colonies of Cryptococcus neoformans and related fungi
growing on the ruins of the melted down reactor of the Chernobyl Nuclear
Power Plant may be able to use the energy of radiation (primary beta
radiation) for "radiotrophic" growth.
Infection with C. neoformans is termed cryptococcosis. Most infections with
C. neoformans consist of a lung infection. However, fungal meningitis and
encephalitis, especially as a secondary infection for AIDS patients, are
often caused by C. neoformans making it a particularly dangerous fungus.
Infections with this fungus are rare in those with fully functioning immune
systems. For this reason, C. neoformans is sometimes referred to as an
opportunistic fungus. It is a facultative intracellular pathogen.
In human infection, C. neoformans is spread by inhalation of aerosolized
spores (basidiospores) and can disseminate to the central nervous system
where it can cause meningoencephalitis. In the lungs, C. neoformans are
phagocytosed by alveolar macrophages Macrophages produce oxidative
and nitrosative agents, creating a hostile environment, to kill invading
pathogens. However, some C. neoformans can survive intracellularly in
macrophages. Intracellular survival appears to be the basis for latency,
disseminated disease, and resistance to eradication by antifungal agents.
One mechanism by which C. neoformans survives the hostile intracellular
environment of the macrophage involves up-regulation of expression of
genes involved in responses to oxidative stress.
Cryptococcosis that does not affect the central nervous system can be
treated with fluconazole alone.
Cysts
A cyst is a closed sac, having a distinct membrane and division compared
to the nearby tissue. Basically, a cyst is a cluster of cells that have grouped
together to form a sac (not unlike the manner in which water molecules
group together, forming a bubble); however, the distinguishing aspect of a
cyst is the cells forming the "shell" of such a sac, are distinctly abnormal (in
both appearance and behaviour) when compared to all surrounding cells
for that given location. It may contain air, fluids, or semi-solid material. A
collection of pus is called an abscess, not a cyst. Once formed, a cyst may
sometimes resolve on its own. Whether a cyst that fails to resolve may
82
need to be removed by surgery will depend on what type of cyst it is and
where in the body it has formed.
Darier's disease
Darier's disease (DAR), also known as Darier disease, Darier–White
disease, Dyskeratosis follicularis and Keratosis follicularis,is an autosomal
dominant disorder discovered by French dermatologist Ferdinand-Jean
Darier. Darier's is characterized by dark crusty patches on the skin,
sometimes containing pus. The crusty patches are also known as keratotic
papules, keratosis follicularis or dyskeratosis follicularis.
Mild forms of the disease are the most common, consisting solely of skin
rashes that flare-up under certain conditions such as high humidity, high
stress or tight-fitting clothes. Even in mild forms, short stature combined
with poorly formed fingernails containing vertical striations are diagnostic.
Darier disease affects both men and women and is not contagious. The
disease often starts during or later than the teenage years, typically by the
third decade. Short stature is common. The symptoms of the disease are
thought to be caused by an abnormality in the desmosome-keratin filament
complex leading to a breakdown in cell adhesion.
It most commonly affects the chest, neck, back, ears, forehead, and groin,
but may involve other body areas. The rash associated with Darier's
disease often has a distinct odor. Palms & soles may become thickened,
intra oral papules can be found. Finger nails become fragile and this helps
in diagnosis of the disease. The rash can be aggravated by heat, humidity,
and exposure to sunlight. In some cases, sunlight makes it better,
especially in the forehead.
Minor forms of the disease are the most common, and may remain
undiagnosed throughout life. These consist mainly of minor rashes without
odor that are aggravated by heat, humidity, stress and sunlight. Poorly
formed fingernails containing vertical striations are diagnostic.
A recent study examined neuropsychiatric conditions in a non-random
sample of 100 British individuals assessed as having DAR. There were
high lifetime rates for mood disorders (50%), including depression (30%),
bipolar disorder (4%), suicidal thoughts (31%) and suicide attempts (13%),
83
suggesting a possible common genetic link. Scattered case studies also
suggest a possible link to learning disorders (not yet confirmed).
Darier's disease has an autosomal dominant pattern of inheritance.
Darier disease is inherited in an autosomal dominant manner, which
indicates that the defective gene responsible for a disorder is located on an
autosome, and only one copy of the gene is sufficient to cause the
disorder, when inherited from a parent who has the disorder.
The disorder is caused by a mutation in the gene ATP2A2. Family
members with confirmed identical ATP2A2 mutations can exhibit
differences in the clinical severity of disease, suggesting that other genes
or environmental factors affect the expression of Darier's disease. With the
discovery of the ATP2A2 gene, performing genetic tests to confirm the
diagnosis of Darier's disease is now possible.
Treatment of choice for severe cases is oral retinoids. During flares, topical
or oral antibiotics may be administered. Ciclosporin and prescription-only
topical corticosteroids, e.g., betamethasone, have been used during acute
flares. Some patients are able to prevent flares with use of topical
sunscreens and oral vitamin C.
For minor forms, no specific treatment is required, but avoidance of
excessive heat, humidity, stress and tight-fitting clothes (and general
cleanliness) is advised. Topical creams (as above) are occasionally
required to deal with flare-ups.
Dermatitis (Eczema)
The term Eczema is a general one that applies to many different types of
skin inflammation. It is also known as dermatitis . the most commonly
encountered form of eczema is atopic dermatitis.
Dry, reddened and itchy skin is the most common symptom of eczema. The
exact appearance will vary from person to person and according to the type
of eczema. An intense itching is usually the first symptom to appear, and
this itching can lead to oozing lesions and blisters as well as scaly skin.
Constant scratching of the area can lead to a layer of thick, crusty skin
forming as well.
84
Eczema can appear anywhere on the body but it is most common on the
face, neck and on the inside elbows and knees. Infants will generally have
it on their forehead, cheeks, arms and legs.
Eczema can sometimes occur as a brief reaction that only leads to
symptoms for a few hours or days, but in other cases, the symptoms
persist over a longer time and are referred to as chronic dermatitis.
As stated above, atopic dermatitis is definitely the most common of the
many forms of eczema, and sometimes people use the two terms
interchangeably. There are many different terms used to describe the
specific types of eczema and they may have very similar symptoms to
atopic dermatitis. These are listed and briefly described below.
Atopic dermatitis
Atopic dermatitis is a chronic skin disease that is associated with itchy,
inflamed skin. Doctors believe it to be caused by an abnormal function of
the body's own immune system. The condition comes and goes, with a
variety of causative factors that include environmental triggers. It effects as
many as 10% of the infants and 3% of the adults in the USA and about twothirds of them develop it before the age of 1. When it is identified in infancy
it is called infantile eczema. It does run in families and people that develop
it often suffer from other allergic conditions like asthma or hay fever.
Contact eczema
This variety of eczema is a highly localized reaction that involves redness
and itching and a burning sensation isolated to a region where the skin has
come in contact with an allergen (a substance that causes an allergic
reaction in certain individuals). It can also be caused by contact with a
general irritant , such as a cleaning chemical or acid. A common culprit is
laundry detergent, the metal nickel (found in jewelry), certain cosmetics and
perfumes. The condition is sometimes called contact dermatitis if the
trigger is an irritant.
Seborrheic eczema
Seborrheic eczema (also known as seborrheic dermatitis) is another form
of skin inflammation. The exact cause is currently unknown.
The symptoms of seborrheic eczema are a yellowish, oily, scaly patches of
skin on the scalp, face, and sometimes other parts of the body. The
commonly encountered condition of "cradle cap" in infants is an example of
85
seborrheic eczema. The areas usually affected are the cheeks and nasal
folds of the face. Unlike the other forms Seborrheic eczema is not
necessarily accompanied by itching. The condition does run in families. It
can be triggered by emotional stress, excessively oily skin, damp weather
conditions. One specific type of seborrheic eczema is common in people
with AIDS.
Nummular eczema
Nummular eczema (nummular dermatitis) is a variety that is characterized
by small coin-shaped patches of irritated skin—most commonly located on
the arms, the back, the buttocks, and the lower legs. They may be crusted,
scaling, and can be extremely itchy. This form of eczema is relatively
uncommon and is generally found in elderly men. Nummular eczema is a
chronic condition. A personal or family history of atopic dermatitis, asthma,
or allergies increases the risk of developing the condition.
Neurodermatitis
Lichen simplex chronicus, or as it is more commonly known,
Neurodermatitis is a chronic inflammatory skin condition caused by a
scratch-itch cycle that begins with a single itch (like those caused by
mosquito or flea bites) that becomes intensely irritated when scratched.
Women are generally more affected by neurodermatitis than men, and the
condition is most frequently found in people aged 20-50. This form of
eczema results in scaly patches of skin on the head, lower legs, wrists, or
forearms. If given enough time the skin can become thickened and leathery
from this condition. Stress can exacerbate the symptoms of
neurodermatitis.
Also known as varicose eczema, this is a skin irritation that is found on the
lower legs and is related to circulatory problems, such as venous
insufficiency. In that condition the function of the valves within the veins
has been compromised, interfering with the flow of blood back to the heart.
This circulatory problem leads to an increase in fluid buildup (edema) in the
legs. Stasis dermatitis can be found occurs almost exclusively in middleaged and elderly people. Approximately 6%-7% of the population over age
50 have this condition, so it stands to reason that the risk of developing
stasis dermatitis increases with age. The symptoms include itching and/or
reddish-brown discoloration of the skin on one or both legs. Eventually the
condition can lead to the blistering, oozing skin lesions seen with other
forms of eczema, and ulcers may develop in affected areas.
86
Dyshidrotic eczema
An irritation of the skin on the palms of hands and soles of the feet
characterized by clear, deep blisters that itch and burn is known as
Dyshidrotic eczema (dyshidrotic dermatitis) or sometimes as vesicular
palmoplantar dermatitis. The exact cause is currently unknown, but it
occurs in up to 205 of the people that have other forms of eczema and is
more common in warm months (Spring and Summer) and warmer climates.
It occurs at the same rate for all genders and age groups.
Eczema can affect people of any age, although the condition is most
common in infants. Eczema will permanently resolve by age 3 in about half
of affected infants. In others, the condition tends to recur throughout life.
People with eczema often have a family history of the condition or a family
history of other allergic conditions, such as asthma or hay fever. Up to 20%
of children and 1%-2% of adults are believed to have eczema.
The goals for the treatment of eczema are to prevent itching, inflammation,
and worsening of the condition. Treatment of eczema may involve both
lifestyle changes and the use of medications. Treatment is always based
upon an individual's age, overall health status, and the type and severity of
the condition.
Keeping the skin well hydrated through the application of creams or
ointments (with a low water and high oil content) as well as avoiding overbathing is an important step in treatment. Lifestyle modifications to avoid
triggers for the condition are also recommended.
Corticosteroid creams are sometimes prescribed to decrease the
inflammatory reaction in the skin. These may be mild-, medium-, or highpotency corticosteroid creams depending upon the severity of the
symptoms. If itching is severe, oral antihistamines may be prescribed. To
control itching, the sedative type antihistamine drugs (for example,
diphenhydramine [Benadryl], hydroxyzine [Atarax, Vistaril], and
cyproheptadine) appear to be most effective.
In some cases, a short course of oral corticosteroids (such as prednisone)
is prescribed to control an acute outbreak of eczema, although their longterm use is discouraged in the treatment of this non life-threatening
condition because of unpleasant and potentially harmful side effects. The
87
oral immunosuppressant drug cyclosporine has also been used to treat
some cases of eczema. Ultraviolet light therapy (phototherapy) is another
treatment option for some people with eczema.
Finally, two topical (cream) medications have been approved by the U.S.
FDA for the treatment of eczema: tacrolimus (Protopic) and pimecrolimus
(Elidel). These drugs belong to a class of immune suppressant drugs
known as calcineurin inhibitors. In 2005, the FDA issued a warning about
the use of these drugs, citing studies in animals that showed a possible
association between use of these drugs and the development of certain
types of cancer. It is recommended that these drugs only be used as
second-line therapy for cases that are unresponsive to other forms of
treatment, and that their use be limited to short time periods, and the
minimum time periods needed to control symptoms. Use of these drugs
should also be limited in people who have compromised immune systems.
Like Psoriasis Eczema is medically contraindicated. If the person is under
the care of a physician and the therapist is careful to avoid areas that
currently blistered or oozing massage can be performed. It should be noted
however that many commercial massage products (oils, creams, gels, etc)
can cause a reaction in people with Eczema.
Epidermodysplasia verruciformis
Epidermodysplasia verruciformis (also called Lewandowsky-Lutz dysplasia)
is an extremely rare autosomal recessive genetic hereditary skin disorder
associated with a high risk of carcinoma of the skin. It is characterized by
abnormal susceptibility to human papillomaviruses (HPVs) of the skin. The
resulting uncontrolled HPV infections result in the growth of scaly macules
and papules, particularly on the hands and feet. It is typically associated
with HPV types 5 and 8, which are found in about 80 percent of the normal
population as asymptomatic infections, although other types may also
contribute.
The condition usually has an onset of between the ages of 1–20, but can
occasionally present in middle-age. It is named after the physicians who
first documented it, Felix Lewandowsky and Wilhelm Lutz.
88
Clinical diagnostic features are lifelong eruptions of pityriasis versicolor-like
macules, flat wart-like papules and development of cutaneous carcinomas.
Patients present with flat, slightly scaly, red-brown macules on the face,
neck and body, recurring especially around the penial area, or verruca-like
papillomatous lesions, seborrheic keratosis-like lesions, and pinkish-red
plane papules on the hands, upper and lower extremities, and face. The
benign form of EV presents with only flat, wart-like lesions over the body,
whereas the malignant form shows a higher rate of polymorphic skin
lesions and development of multiple cutaneous tumors.
Generally, cutaneous lesions are disseminated over the body, but there are
some cases with only a few lesions which are limited to one extremity.
No serious treatment against EV has been found yet. Several treatments
have been suggested, and acitretin 0.5–1 mg/day for 6 months’ duration is
the most effective treatment owing to antiproliferative and differentiationinducing effects.
Interferons can also be used effectively together with retinoids.
As mentioned, various treatment methods are offered against EV; however,
most important, education of the patient, early diagnosis and excision of the
tumoral lesions take preference to prevent the development of cutaneous
tumors.
Massage therapy is medically contraindicated.
Erythema
Erythema (from the Greek erythros, meaning red) is redness of the skin or
mucous membranes, caused by hyperemia of superficial capillaries. It
occurs with any skin injury, infection, or inflammation. Examples of
erythema not associated with pathology include nervous blushes.
Erythema disappears on finger pressure (blanching), while purpura or
bleeding in the skin and pigmentation do not. There is no temperature
elevation, unless it is associated with the dilation of arteries in the deeper
layer of the skin.
89
It can be caused by infection, massage, electrical treatment, acne
medication, allergies, exercise, solar radiation (sunburn), cutaneous
radiation syndrome, mercury toxicity, blister agents, niacin administration,
or waxing and tweezing of the hairs—any of which can cause the
capillaries to dilate, resulting in redness. Erythema is a common side effect
of radiotherapy treatment due to patient exposure to ionizing radiation.
Erythrasma
Erythrasma is a bacterial skin infection which favors moist folds of the skin.
The medical term for the folds of the skin found around armpits, the groin,
and knees is intertriginous skin.
It is caused by the Gram-positive bacterium Corynebacterium
minutissimum. It is prevalent among diabetics and the obese, and in warm
climates; it is worsened by wearing occlusive clothing.
The patches of erythrasma are initially pink, but progress quickly to become
brown and scaly (as skin starts to shed), which are classically sharply
demarcated. Erythrasmic patches are typically found in intertriginous areas
(skin fold areas - e.g. armpit, groin, under breast). The slightly webbed
spaces between toes (or other body region skin folds) can be involved,
making it difficult to distinguish from various Tinea. The patient is
commonly otherwise asymptomatic. The diagnosis can be made on the
clinical picture alone. However, a simple side-room investigation with a
Wood's lamp is additionally useful in diagnosing erythrasma. The ultraviolet
light of a Wood's lamp causes the organism to fluoresce a coral red color,
differentiating it from other bacterial infections and other skin conditions.
(fungal infections will also be fluorescent)
This condition contraindicates massage becuase it is contagious.
Erythroderma
Erythroderma (also known as "Exfoliative dermatitis," "Dermatitis
exfoliativa," and "Red man syndrome") is an inflammatory skin disease with
erythema and scaling that affects nearly the entire cutaneous surface.
Erythroderma is generalized exfoliative dermatitis, which involves 90% or
more of the patient's skin. The most common cause of erythroderma is
exacerbation of an underlying skin disease, such as psoriasis, contact
dermatitis, seborrheic dermatitis, lichen planus, pityriasis rubra pilaris or a
90
drug reaction. Primary erythroderma is less frequent and is usually seen in
cases of cutaneous T-cell lymphoma, in particular in Sézary's disease.
The most common causes of exfoliative dermatitis are best remembered by
the mnemonic device ID-SCALP. The causes and their frequencies are as
follows:
Idiopathic - 30%
Drug allergy - 28%
Seborrheic dermatitis - 2%
Contact dermatitis - 3%
Atopic dermatitis - 10%
Lymphoma and leukemia - 14%
Psoriasis - 8%
Differential diagnosis in patients with erythroderma may be difficult.
The treatment is dependent on the cause. Topical steroids are the primary
category of medications used to treat exfoliative dermatitis (ED). A sedative
antihistamine may be a useful adjunct for pruritic patients, since it helps
patients to sleep at night, thus limiting nocturnal scratching and
excoriations. Antimicrobial agents often are used if an infection is
suspected to be precipitating or complicating exfoliative dermatitis. Other
drugs specifically indicated for management of underlying etiology of
exfoliative dermatitis may be necessary.
Erythroderma contraindicates massage due to its inflammatory nature.
Ferguson–Smith syndrome
Ferguson-Smith type of multiple self-healing keratoacanthomas," is a
cutaneous condition, a variant of keratoacanthomas, which is characterized
by the appearance of multiple, sometimes hundreds of keratoacanthomas.
A solitary keratoacanthoma (also known as "Subungual keratoacanthoma")
is a benign, but rapidly growing, locally aggressive tumor, which sometimes
occur in the nail apparatus.
Keratoacanthoma (KA) is a common low-grade (unlikely to metastasize or
invade) skin tumour that is believed to originate from the neck of the hair
follicle. Many pathologists consider it to be a form of squamous cell
carcinoma (SCC). The pathologist often labels KA as "well-differentiated
91
squamous cell carcinoma, keratoacanthoma variant", because about 6% of
KA manifest itself as squamous cell carcinoma when left untreated. KA is
commonly found on sun-exposed skin, and often is seen on the face,
forearms and hands.
The defining characteristic of KA is that it is dome-shaped, symmetrical,
surrounded by a smooth wall of inflamed skin, and capped with keratin
scales and debris. It always grows rapidly, reaching a large size within days
or weeks, and if untreated will starve itself of nourishment, necrose (die),
slough, and heal with scarring. While some pathologists classify KA as a
distinct tumor and not a malignancy, enough clinical and histological KA do
progress to invasive and aggressive squamous cell cancers, therefore
prompt and aggressive treatment is required.
In reality, the defining characteristics of a KA can not be found when only a
small fragment of a large KA is submitted for pathology review. If the
keratin debris is submitted, no diagnosis can be made. If a deep core or
peripheral deep wedge is performed, a squamous cell carcinoma is often
noted. Only when almost the entire structure is submitted, can a true
diagnosis of a KA be made. This further complicates the distinction
between a clinical diagnosis of a KA and the pathologic diagnosis of a KA
vs a squamous cell cancer.
Fibrofolliculomas
Fibrofolliculomas are benign tumours/growths in the hair follicle and appear
as skin papules.
Fibrofolliculomas are one of the most common symptoms of BHD
syndrome.
They are most commonly found on the neck, upper chest, upper back, and
face, and can also be found on the ear and earlobe. Individuals affected by
BHD syndrome can have anywhere from one to several hundred of these
skin lesions over a lifetime.
In affected individuals, these skin lesions normally appear in the second
and third decade of life. The numbers and size of the fibrofolliculomas may
increase with age.
Trichodiscomas are lesions that are the colour of skin which are similar to
fibrofolliculomas. It is now thought that fibrofolliculomas and
92
trichodischomas are part of the same spectrum of condition and that they
are not two different symptoms.
Filarial disease
Filariasis is predominantly a disease of tropical countries and affects the
lives of millions of people. Filariasis is spread from host-to-host via the bites
of certain flies and mosquitoes that act as vectors for the parasites. For
example the filarial nematode Onchocerca volvulus enters the skin from the
bite of an infected blackfly (Simulium species). The nematode is in its third
larval stage before it moults to its fourth larval stage in 4-6 weeks. Then
after some months it moults again to become a juvenile adult that matures
and mates after about a year to produce microfilariae. These adult worms
live and mate encased in fibrous nodules just below the skin surface and
can live there for up to 10-15 years.
Filariasis (or philariasis) is a parasitic disease that is caused by thread-like
roundworms belonging to the Filarioidea type. These are spread from by
blood-feeding black flies and mosquitoes.
Eight known filarial nematodes use humans as their definitive hosts. These
are divided into three groups according to the niche within the body they
occupy:
Lymphatic filariasis is caused by the worms Wuchereria bancrofti, Brugia
malayi, and Brugia timori. These worms occupy the lymphatic system,
including the lymph nodes; in chronic cases, these worms lead to the
disease elephantiasis.
Subcutaneous filariasis is caused by Loa loa (the eye worm), Mansonella
streptocerca, and Onchocerca volvulus. These worms occupy the
subcutaneous layer of the skin, in the fat layer. L. loa causes Loa loa
filariasis, while O. volvulus causes river blindness.
Serous cavity filariasis is caused by the worms Mansonella perstans and
Mansonella ozzardi, which occupy the serous cavity of the abdomen.
The adult worms, which usually stay in one tissue, release early larval
forms known as microfilariae into the host's bloodstream. These circulating
microfilariae can be taken up with a blood meal by the arthropod vector; in
the vector, they develop into infective larvae that can be transmitted to a
new host.
93
Individuals infected by filarial worms may be described as either
"microfilaraemic" or "amicrofilaraemic", depending on whether or not
microfilariae can be found in their peripheral blood. Filariasis is diagnosed
in microfilaraemic cases primarily through direct observation of microfilariae
in the peripheral blood. Occult filariasis is diagnosed in amicrofilaraemic
cases based on clinical observations and, in some cases, by finding a
circulating antigen in the blood.
Most people have no symptoms, even if microfilaremia might be detected.
Acute infection may start with general symptoms including nausea, fever,
headache, backache and /or localized manifestations such as
lymphadenitis, lymphangitis (with a typical centrifugal progression unlike
bacterial infections), epididymitis and orchitis. The most spectacular
symptom of lymphatic filariasis is elephantiasis—edema with thickening of
the skin and underlying tissues—which was the first disease discovered to
be transmitted by mosquito bites. Elephantiasis results when the parasites
lodge in the lymphatic system.
Elephantiasis affects mainly the lower extremities, while the ears, mucous
membranes, and amputation stumps are affected less frequently. However,
different species of filarial worms tend to affect different parts of the body;
Wuchereria bancrofti can affect the legs, arms, vulva, breasts, and scrotum
(causing hydrocele formation), while Brugia timori rarely affects the
genitals. Chyluria (presence of lymph in the urines) may appear if
lymphatics open into the urinary system. Those who develop the chronic
stages of elephantiasis are usually amicrofilaraemic, and often have
adverse immunological reactions to the microfilariae, as well as the adult
worms. Tropical pulmonary eosinophilia describes a syndrome with
nocturnal cough, chest infiltrates, eosinophilia and increased IgE caused by
sequestration of microfilarie of W. bancrofti or B. malayi in the lung
capillaries.
The subcutaneous worms present with skin rashes, urticarial papules, and
arthritis, as well as hyper- and hypopigmentation macules. Onchocerca
volvulus manifests itself in the eyes, causing "river blindness"
(onchocerciasis), one of the leading causes of blindness in the world.
Serous cavity filariasis presents with symptoms similar to subcutaneous
filariasis, in addition to abdominal pain, because these worms are also
deep-tissue dwellers.
94
Filariasis is usually diagnosed by identifying microfilariae on Giemsa
stained, thin and thick blood film smears, using the "gold standard" known
as the finger prick test. The finger prick test draws blood from the
capillaries of the finger tip; larger veins can be used for blood extraction,
but strict windows of the time of day must be observed. Blood must be
drawn at appropriate times, which reflect the feeding activities of the vector
insects. Examples are W. bancrofti, whose vector is a mosquito; night is the
preferred time for blood collection. Loa loa's vector is the deer fly; daytime
collection is preferred. This method of diagnosis is only relevant to
microfilariae that use the blood as transport from the lungs to the skin.
Some filarial worms, such as Mansonella streptocerca and O. volvulus,
produce microfilarae that do not use the blood; they reside in the skin only.
For these worms, diagnosis relies upon skin snips, and can be carried out
at any time.
There are four key treatment methods available:
Antihelminthic therapy (orally or by injection)
Antibiotic therapy (against the symbiotic Wolbachia bacteria)
Surgical excision
Needle aspiration/injection
Treatment depends on the infecting parasite.
Massage therapy is medically contraindicated for Filariasis.
Fish tank granuloma
Mycobacterium marinum infections, aka “fish tank granuloma” are
infections caused by a species of mycobacterium other than
Mycobacterium tuberculosis, the causative bacteria of pulmonary TB and
extrapulmonary TB including cutaneous TB; and Mycobacterium leprae, the
cause of leprosy.
Mycobacterium marinum
Uncommon infection that occurs most often in people with
recreational or occupational exposure to contaminated freshwater or
saltwater
Usually a single lump or pustule that breaks down to form a crusty
sore or abscess
95
Other lumps may occur around the initial lesion, particularly along the
lines of lymphatic drainage (sporotrichoid forms)
Most often affects elbows, knees, feet, knuckles or fingers
Multiple lesions and widespread disease may occur in
immunocompromised patients
Rarely causes red, swollen and tender joints
Mycobacterium marinum species are often resistant to isoniazid,
streptomycin, pyrazinamide, and para-aminosalicylic acid. Effective
antimicrobials include tetracyclines, fluoroquinolones, macrolides, and
sulfonamides. Treatment should be for at least 4–6 weeks, and sometimes
up to two months.
Fish tank granuloma contraindicates massage due to its infectious nature.
Flegel’s disease
Flegel disease is characterised by red-brown papules with irregular horny
scales located mainly on the top surface of the feet and lower legs. It is
very similar to Kyrle disease and has been regarded as a variant of Kyrle’s,
however its clinical and pathological picture is sufficiently different to make
it its own disease entity27.
The cause of the disease is unknown. It is thought to be an inherited
condition although cases have been reported where there is no family
history of the disease. Exposure to the sun has also been implicated but
not proven.
Flegel disease has been reported to rarely affect some families that were
also prone to skin and gastrointestinal cancers.
Lesions are small, red-brown, 1-5mm scaly papules that appear most
commonly on the top surface of the feet and lower legs. Removal of the
scale reveals a bright red base, often with pinpoint bleeding. In rare
instances, the outer ear lobes, arms, palms, soles, and oral mucosa may
be affected. Lesions are not usually painful.
Lesions are benign and are mainly treated for cosmetic reasons. Treatment
of lesions include:
27
Textbook of Dermatology. Ed Rook A, Wilkinson DS, Ebling FJB, Champion RH, Burton JL. Fourth edition. Blackwell Scientific
Publications.
96
Topical 5% fluorouracil cream used over several months
Dermabrasion
Cryotherapy
Topical retinoid
Oral retinoid such as acitretin or isotretinoin.
Massage therapy is contraindicated when it is in the acute stage (during an
outbreak), but is safe when the lesions are not present.
Folliculitis
Folliculitis is the infection and inflammation of one or more hair follicles.
The condition may occur anywhere on the skin with the exception of the
palms of the hands and soles of the feet. They may appear as red dots that
come to white tips on the chest, back, arms, legs, and head.
Most carbuncles, furuncles, and other cases of folliculitis develop from
Staphylococcus aureus and Pseudomonas aeruginosa.
Folliculitis starts when hair follicles are damaged by friction from clothing,
an insect bite, blockage of the follicle, shaving, or braids too tight and too
close to the scalp. In most cases of folliculitis, the damaged follicles are
then infected with the bacterium Staphylococcus. Folliculitis usually affects
those in their early adult life, and may persist till their early 30s. Warmer
weather may worsen the condition.
Most carbuncles, furuncles, and other cases of folliculitis develop from
Staphylococcus aureus and Pseudomonas aeruginosa.
Folliculitis starts when hair follicles are damaged by friction from clothing,
an insect bite, blockage of the follicle, shaving, or braids too tight and too
close to the scalp. In most cases of folliculitis, the damaged follicles are
then infected with the bacterium Staphylococcus. Folliculitis usually affects
those in their early adult life, and may persist till their early 30s. Warmer
weather may worsen the condition.
Iron deficiency anemia is sometimes associated with chronic cases.
97
Fungal causes
Tinea barbae is similar to barber's itch, but the infection is caused by the
fungus T. rubrum.
Malassezia folliculitis, formerly known as Pityrosporum folliculitis, is caused
by yeasts (fungi) of the genus Malassezia.
Bacterial causes
Hot-tub folliculitis is caused by the bacterium Pseudomonas aeruginosa.
The folliculitis usually occurs after sitting in a hot tub that was not properly
cleaned before use. Symptoms are found around the body parts that sit in
the hot tub—typically the legs, hips, buttocks, and surrounding areas.
Symptoms are typically amplified around regions that were covered by wet
clothing, such as bathing suits.
Sycosis vulgaris, Sycosis barbae or Barber's itch is a staphylococcus
infection of the hair follicles in the bearded area of the face, usually the
upper lip. Shaving aggravates the condition.
Gram-negative folliculitis may appear after prolonged acne treatment with
antibiotics.
Viral causes
Herpetic folliculitis may occur when Herpes Simplex Virus infection spreads
to nearby hair follicles - mostly around the mouth.
Non-infectious causes
Pseudofolliculitis barbae is a disorder occurring when hair curves back into
the skin and causes inflammation.Eosinophilic folliculitis may appear in
persons with impaired immune systems.
Folliculitis decalvans or tufted folliculitis usually affects scalp. Several hairs
arise from the same hair follicle. Scarring and permanent hair loss may
follow. The cause is unknown.
Folliculitis keloidalis scarring on the nape of the neck, most common
among males of curly hair.
98
Oil folliculitis is inflammation of hair follicles due to exposure to various oils
and typically occurs on forearms or thighs. It is common in refinery workers,
road workers, mechanics, and sheep shearers. Even makeup may cause it.
Massage is locally contraindicated for Folliculitis.
99
Fungal skin infections
Fungal skin infections are infections on the skin caused by a fungus. There
are many different types of fungal skin infections.
The symptoms and appearances of a fungal skin infection depend on the
type of fungus causing it and the part of the body affected.
They can cause rashes with a variety of different appearances. Some are
red, scaly and itchy, whereas others can produce a fine scale similar to dry
skin. The fungus may infect just one area of the body, or there may be
several infected areas.
Fungal infections of the scalp or beard can lead to hair loss. Fungal rashes
can sometimes be confused with other skin conditions, such as psoriasis
and eczema.
Fungal infections usually affect the skin because they live off keratin, a
protein that makes up skin, hair and nails. Fungal skin infections are
divided into groups depending on what type of organism is involved. The
full name depends on the location of the infection on the body.
Some common fungal infections are listed below.
Dermatophyte infections
Most basic fungal skin infections are caused by dermatophytes - a type of
fungi that cause skin, nail and hair infections. They are common, affecting
between 10 and 20% of people at some point in their life. They include:
Athlete's foot (Tinea pedis)
This is a very common infection that occurs in one in five adults. It's often
caused by a combination of fungi and bacteria. It causes scaling and
sogginess of the skin, commonly of the web spaces between the toes.
Sometimes the skin becomes pale and can be itchy. The infection is often
picked up from contaminated skin fragments in public places, such as
swimming pools and shower facilities.
Nail infections
Onychomycosis is the name for any fungal nail infection. Tinea unguium
(ringworm of the nails) is a common infection. The nails become
malformed, thickened and crumbly. Not all nails affected like this are
100
caused by fungal infections, but it is a common cause. Toenail infections
are commonly linked with athlete's foot. Fingernails can be affected too.
Ringworm of the groin (Tinea cruris)
This is called "jock itch" because it occurs often on athletes. It causes an
itchy, red rash in the groin and surrounding area and is commonly seen in
men who have been sweating a lot.
Ringworm on the body (Tinea corporis)
This affects the body, often in exposed areas like the abdomen or on limbs,
causing red patches. They are scaly at the edge with clear skin at the
centre. The patches spread out from the centre. It can be caught from
domestic animals.
Ringworm of the scalp (Tinea capitis)
This tends to affect young children and can cause hair loss with
inflammation in the affected area. It is usually spread from person to
person. Most people infected by this fungus don't actually develop the
symptoms, but become carriers who can spread the infection to others,
sometimes for years.
Yeast infections
Other fungal skin infections are caused by yeast infections. These include
the following examples:
Intertrigo
Intertrigo is a yeast infection of skin folds caused by Candida albicans. It
affects areas of the body that have skin touching skin such as the armpits,
groin, and under heavy breasts or fat folds, where the environment is warm
and moist.
Pityriasis versicolor
This yeast infection causes increased dark patches on pale or untanned
skin and light patches on tanned or darker skin. Another name for this
condition is tinea versicolor (versicolor means "of various colours").
Teenagers and young adults are most often affected in the UK.
Thrush (Candida albicans)
The fungus Candida albicans is present in most people, and lives in the
mouth and digestive system. It usually lives in harmony with us and rarely
101
causes problems. However, in certain situations, such as during illness or
when using antibiotics, the fungi multiply and cause thrush symptoms.
Thrush can affect the mouth and tongue, areas lined with a mucus
membrane such as the vagina, and moist, folded skin. Thrush infection
often looks like small white patches, which leave a red mark when rubbed
off. In adults, vaginal thrush can cause itchiness and a thick, white
discharge.
Thrush sometimes affects men, causing a painful red rash on the head of
the penis (glans). It also commonly affects newborn babies in the mouth
(oral thrush). The white patches may be mistaken for breast or formula
milk. It isn't usually serious, but babies with thrush in their throats may stop
feeding properly. Babies may also develop thrush in the nappy area.
Fungal infections can be spread between humans through touch. Contact
with used linens or towels can also spread fungal infections. Massage is
definitely locally contraindicated for fungal infections such as athletes foot
and nail fungus. Ringworm is highly contagious and if you are massaging
an individual and that has a rash that you believe to be Ringworm you
should end the massage immediately and proceed to sanitize your hands.
The ease of spreading between people on linens is a reminder of why good
sanitation procedures are so important in a massage practice.
Fungal infections inside the body can cause more serious health problems
than those on the skin. These infections only affect people whose immune
systems aren't working properly - either as a result of another illness such
as AIDS, or because of immunosuppressant medicines, such as those
taken after having an organ transplant.
Fungal infections are very common, the World Health Organization reports
that as many as 1 in 5 people have had some variety of fungal infection in
their lifetimes.
Since most fungal skin infections are surface infections, antifungal
treatments are usually applied directly to the skin in the infected area
(topical treatments).
102
There are a variety of treatments available in the form of creams, lotions
and medicated powders. If the rash covers quite a large area of skin, or
affects the nails or scalp, then tablets may be required.
Some treatments are available over-the-counter from a pharmacist, without
a prescription. For example, sprays are available for treating athletes foot.
Stronger forms of topical treatments and antifungals in tablet form are only
available on prescription.
Glandular fever
Glandular fever is a viral infection with unpleasant symptoms that can last
several weeks.
Glandular fever affects around 1 in 200 people during their lives and mostly
affects young adults aged between 15 and 24.
Glandular fever is spread through a person's saliva, through kissing,
coughing and sneezing and shared cutlery and crockery.
Symptoms of glandular fever include fever, sore throat, swollen neck
glands and fatigue.
Glandular fever is caused by the Epstein-Barr virus, or EBV, named after
the two British researchers who first identified it in 1964, although the
disease itself had been recognised many years earlier. A common member
of the herpes family of viruses, the Epstein-Barr virus is spread primarily
through the exchange of saliva, which is why glandular fever is sometimes
known as ‘the kissing disease’. Coughing or other contact with infected
saliva can also pass the virus from one person to another.
The glandular fever virus can stay active in a person weeks or months after
all overt symptoms are gone, so close contact with someone who shows no
sign of the disease can still put others at risk. On the other hand, not
everyone who lives in close proximity to a person infected with glandular
fever comes down with the illness. Scientists believe that a healthy immune
system may make it possible to fight off the infection successfully.
When glandular fever strikes young children, the illness is usually so mild
that it passes as a common cold or the flu. When it occurs during
103
adolescence or adulthood, however, the disease can be much more
serious.
Glandular fever comes on gradually. It begins with flu-like symptoms; fever,
headache and a general malaise and lethargy. After a few days, the lymph
glands begin to swell, although this symptom is not noticeable in everyone.
Swollen glands in the back of the neck are especially typical of glandular
fever. Most people develop a sore throat, which can be very severe, with
inflamed tonsils. A fever, usually no higher than 40 degrees Celsius (104
degrees Fahrenheit), can also develop and may last up to three weeks.
Some people with glandular fever, particularly those who take the
antibioticamoxicillin, may develop a red rash all over the body. Others may
notice red spots or darkened areas in the mouth that look like bruises. In
about half of all cases, the spleen becomes enlarged, causing an area in
the upper-left abdomen to become tender to the touch.
In most cases, glandular fever mildly affects the liver. Only a few individuals
with glandular fever develop inflammation of the liver, causing jaundice, a
yellowing of the skin and eyes caused by an increase of the liver's bile
protein in the blood. In rare cases of glandular fever, the liver fails.
Massage therapy is contraindicated during the acute stage, due to the fever
and infectious nature of the disease.
Hemangioma
A hemangioma is a benign and usually self-involuting tumor (swelling or
growth) of the endothelial cells that line blood vessels, and is characterised
by increased number of normal or abnormal vessels filled with blood. It
usually appears in the first weeks of life and grows most rapidly over the
first six months. Usually, growth is complete and involution has
commenced by twelve months. Half of all infantile hemangiomas have
completed involution by age five, 70% by age seven, and most of the
remainder by age twelve. In more severe cases hemangiomas may leave
residual tissue damage. In infancy, it is the most common tumor. The word
"hemangioma" comes from the Greek haema- (αίμα), "blood"; angeio
(αγγείο), "vessel"; -oma (-ωμα), "tumor".
The terminology used to define, describe and categorize vascular
anomalies, abnormal lumps made up of blood vessels, has changed. The
104
term hemangioma was originally used to describe any vascular tumor-like
structure, whether it was present at or around birth or appeared later in life.
Mulliken et al. categorized these conditions into two families: a family of
self-involuting tumors, growing lesions that eventually disappear, and
another family of malformations, enlarged or abnormal vessels present at
birth and essentially permanent. The importance of this distinction is that it
makes it possible for early-in-life differentiation between lesions that will
resolve versus those that are permanent. Examples of permanent
malformations include port-wine stains (capillary vascular malformation)
and masses of abnormal swollen veins (venous malformations). The
Mulliken categorisation has received major confirmation following discovery
of the Glut-1 marker.
Hemangioma are of three types based on the type of vessel involved. They
are:
Capillary Hemangioma
Cavernous Hemangioma (also called Venous Hemangioma)
Plexiform Hemangioma (also called Arterial Hemangioma)
Common capillary hemangioma are:
Salmon Patch
Port-wine Stain
Strawberry Angioma
Vin Rose Patch
Hemangiomas are connected to the circulatory system. The appearance
depends on location. If they are on the surface of the skin, they are
reminiscent of a ripe strawberry (hence, they are sometimes referred to as
"strawberry hemangiomas"); however, if they are just under the skin they
present as a bluish swelling. Sometimes they grow in internal organs such
as the liver, larynx, or small and large intestine.
In most cases, hemangiomas will disappear over time. Some are formed
during gestation and are called congenital hemangiomas; the most
common (infantile hemangiomas) appear during the first few weeks of life.
Infantile hemangioma is often initially misdiagnosed as a scratch or bruise;
but the correct diagnosis becomes obvious with further growth. Typically, at
the earliest phase in a superficial lesion, one will see a bluish red area with
obvious blood vessels and surrounding pallor. Sometimes they present as
a flat red or pink area. Hemangiomas are the most common childhood
105
tumor, occurring in approximately ten percent of Caucasians, and are less
prevalent in other ethnicities. Females are three to five times as likely to
have hemangiomas as males. Hemangiomas are also more common in
twin pregnancies. Approximately 80% are located on the face and neck, or
on the legs and arms; with the next most prevalent location being the liver.
In infants, It may appear soon after birth and is different than other vascular
abnormalities present. They grow to around 80% of their maximum size in
the first 3 months and most reach maximum size at around 5 months.
Most hemangiomas disappear without treatment, leaving minimal or no
visible marks. This may take many years. Large hemangiomas can leave
visible skin changes secondary to severe stretching of the skin or damage
to surface texture. When hemangiomas interfere with vision, breathing, or
threaten significant cosmetic injury (facial lesions and in particular, nose
and lips), they are usually treated. You should seek treatment as soon as
possible for a successful outcome. Between November 2009 and July 2013
the Children's Hospital of Minnesota has treated over 180 children with a
98% success rate using the blood pressure medication propranolol.
Effectiveness of propranolol is highest within the first 6 months of the onset
of hemangioma. The treatment was first discovered in 2008 by a French
group and has proven to show high success rates since then.
Until recently, the mainstay of treatment was oral corticosteroid therapy, but
there are now alternative treatments. A randomized trial showed that the
beta-blocker propranolol reduced severe hemangiomas in infants. The
topically applied beta blocker solution/gel Timolol is also being trialled for
small facial hemangiomas that do not justify systemic treatment. Other
treatments that have been used include interferon or vincristine. They may
be considered if first-line therapy fails.
Surgical removal is sometimes indicated, particularly if there has been
delay in commencing treatment and structural changes have become
irreversible. Surgery may also be necessary to correct distortion of facial
features, again in the case of inadequate or failed early medical
intervention. Blockage of the airway will often require a tracheostomy to be
performed, which involves the insertion of an external airway through the
front of the neck into the trachea below the level of the obstruction.
Smaller raised lesions are sometimes treated with injection of corticosteroid
directly into the lesion. A pulsed dye laser can be useful for very early, flat,
106
superficial lesions, if they appear in cosmetically significant areas or for
those lesions that leave residual surface blood vessels in the case of
incomplete resolution. Sometimes a pulsed dye laser can be used to
accelerate healing. Unfortunately, raised lesions or lesions under the skin
do not respond to laser treatment. Ulceration will usually heal with topical
medication and special dressings under medical supervision. Applying
pressure is not beneficial, thus not recommended.
Massage is contraindicated for capillary hemangioma that result in raised
lesions.
Haemochromatosis
Haemochromatosis, or GH (Genetic Haemochromatosis), is a genetic
disorder causing the body to absorb an excessive amount of iron from the
diet: the iron is then deposited in various organs, mainly the liver, but also
the pancreas, heart, endocrine glands, and joints.
Normally the liver stores a small amount of iron for the essential purpose of
providing new red blood cells with iron, vital for health. When excessive
quantities of iron are stored in the liver it becomes enlarged and damaged.
Deposits of iron may also occur in other organs and joints, causing serious
tissue damage.
For a long time it was believed that the disorder was rare, so GH was
seldom considered as a possible diagnosis. However, recent surveys of
people of Northern European origin have shown a prevalence of 1 in 200
likely to be at risk of developing iron overload. GH is now recognised as
being one of the most common genetic disorders.
The symptoms of Haemochromatosis include chronic fatigue, weakness,
lethargy, abdominal pain; sometimes in the stomach region or the upper
right hand side, sometimes diffusebronze fist
arthritis; Diabetes (late onset type), Liver disorders; abnormal liver function
tests, enlarged liver, cirrhosis, Sexual disorders; loss of sex drive,
impotence in men, absent or scanty menstrual periods and early
menopause in women, decrease in body hair
Cardiomyopathy; disease of the heart muscle (not to be confused with
disease of the arteries of the heart), Neurological/psychiatric disorders;
impaired memory, mood swings, irritability, depression
Bronzing of the skin, or a permanent tan.
107
Most of these symptoms are found in other disorders. Chronic fatigue may
be ascribed to after-effects of a viral infection or to psychological causes,
and abdominal pain to irritable bowel syndrome. Similarly liver disorders
may be put down to excessive alcohol intake, even in someone who is only
a moderate drinker. However, if the above symptoms are present, GH
should also be considered as a diagnosis.
Most individuals who have GH will, in due course, develop at least one or
two of the above symptoms, although possibly in a very mild form. There
may be a long phase of the condition where there are no symptoms.
However, if arthritis is found only in the first two finger joints this is highly
suggestive of GH.
The simple and effective treatment consists of regular removal of blood.
Known as venesection therapy or phlebotomy, the procedure is the same
as for blood donors. Every pint of blood removed contains a quarter of a
gram of iron.
The body then uses some of the excess stored iron to make new red blood
cells. Venesection will usually be performed once a week, depending on
the degree of iron overload. Treatment may need to be continued at this
frequency for up to 2 years, occasionally longer.
During the course of treatment, the serum ferritin levels are monitored,
indicating the size of the remaining iron stores. Treatment should usually
continue until the serum ferritin level reaches 20µg/l (indicating minimal or
absent iron stores).
Excess iron will continue to be absorbed so the individual will need
occasional venesections (maintenance therapy), on average every 3 to 4
months, for the rest of his or her life. Monitoring of transferrin saturation
and serum ferritin is used to assess whether venesection is required more
or less often. The transferrin saturation should be maintained below 50%
and the serum ferritin below 50µg/l.
There is no reason why someone with Haemochromatosis would not be
able to benefit from and enjoy massage therapy.
108
Hailey–Hailey disease
Hailey-Hailey disease, sometimes called ‘familial benign chronic
pemphigus’ is a rare hereditary blistering skin disease. The Hailey brothers
first described it in 1939.
Hailey-Hailey disease usually appears in the third or fourth decade,
although it can occur at any age. It typically begins as a painful erosive skin
rash in the skin folds. Common sites include the armpits, groins, and neck,
under the breasts and between the buttocks. The lesions tend to come and
go and leave no scars. As the lesions get bigger the centre clears leaving a
typical ring shape. If the lesions are present for some time they may
become thickened. The skin then tends to macerate leaving quite painful
cracks. Secondary bacterial infection, which is not uncommon, can give
rise to an unpleasant smell. White bands on the fingernails and pits in the
palms can also occur.
Heat, sweating and friction often exacerbates the disease, and most
patients have worse symptoms during the summer months.
Hailey-Hailey disease is a inherited skin disorder, although occasionally
sporadic cases arise without a family history. The defect responsible has
now been identified on a gene called ATP2C1 found on chromosome 3q2124. This gene codes for the protein SPCA1 (Secretory Pathway
Calcium/manganese-ATPase), a calcium and manganese pump. The skin
cells (keratinocytes) stick together via structures called desmosomes and it
seems the desmosomes do not assemble properly if there is insufficient
calcium.
The genetic defect in Hailey-Hailey disease causes the skin cells to
become unstuck from one another. Normally the cells are packed together
tightly in much the same way as bricks and mortar. Patients with HaileyHailey disease have defective ´mortar´ and the cells fall apart, like a
dilapidated brick wall.
Usually Hailey-Hailey disease is diagnosed by its appearance and the
family history, but it is often is mistaken for other skin problems. Impetigo,
thrush, tinea (jock itch) and other blistering conditions look similar.
Unfortunately there is no cure for Hailey-Hailey disease. Treatment is
aimed at reducing symptoms and preventing flares.
109
For many patients Hailey-Hailey disease is a mild condition, but for others
the pain and smell can be serious problems. If the lesions get infected with
herpes virus a sudden severe flare can occur, which often needs prompt
treatment (see above).
Many patients have long remissions and an improvement with age does
occur.
Henoch–Schönlein purpura
Henoch–Schönlein purpura (HSP) is a disease of the skin and other organs
that most commonly affects children. In the skin, the disease causes
palpable purpura (small hemorrhages); often with joint and abdominal pain.
With kidney involvement, there may be a loss of small amounts of blood
and protein in the urine, but this usually goes unnoticed; in a small
proportion of cases, the kidney involvement proceeds to chronic kidney
disease. HSP is often preceded by an infection, such as a throat infection.
HSP is a systemic vasculitis (inflammation of blood vessels) and is
characterized by deposition of immune complexes containing the antibody
IgA; the exact cause for this phenomenon is unknown. It usually resolves
within several weeks and requires no treatment apart from symptom
control, but may relapse in a third of the cases and cause irreversible
kidney damage in about one in a hundred cases.
The purpura typically appear on the legs and buttocks, but may also be
seen on the arms, face and trunk. The abdominal pain is colicky in
character, and may be accompanied by nausea, vomiting, constipation or
diarrhea. There may be blood or mucus in the stools. The joints involved
tend to be the ankles, knees, and elbows, but arthritis in the hands and feet
is possible; the arthritis is nonerosive and hence causes no permanent
deformity. Forty percent have evidence of kidney involvement, mainly in the
form of hematuria (blood in the urine), but only a quarter will have this in
sufficient quantities to be noticeable without laboratory tests. Problems in
other organs, such as the central nervous system (brain and spinal cord)
and lungs may occur, but is much less common than in the skin, bowel and
kidneys28.
28
Saulsbury FT (2001). "Henoch-Schönlein purpura". Current Opinion in Rheumatology 13 (1): 35–40. doi:10.1097/00002281-20010100000006. PMID 11148713.
110
Of the 40% of patients who develop kidney involvement, almost all have
evidence (visible or on urinalysis) of blood in the urine. More than half also
have proteinuria (protein in the urine), which in one eighth is severe enough
to cause nephrotic syndrome (generalised swelling due to low protein
content of the blood). While abnormalities on urinalysis may continue for a
long time, only 1% of all HSP patients develop chronic kidney disease.
Hypertension (high blood pressure) may occur. Protein loss and high blood
pressure, as well as the features on biopsy of the kidney if performed, may
predict progression to advanced kidney disease. Adults are more likely
than children to develop advanced kidney disease.
HSP can develop after infections with streptococci (β-haemolytic,
Lancefield group A), hepatitis B, herpes simplex virus, parvovirus B19,
Coxsackievirus, adenovirus, Helicobacter pylori, measles, mumps, rubella,
Mycoplasma and numerous others. Drugs linked to HSP, usually as an
idiosyncratic reaction, include the antibiotics vancomycin and cefuroxime,
ACE inhibitors enalapril and captopril, anti-inflammatory agent diclofenac,
as well as ranitidine and streptokinase. Several diseases have been
reported to be associated with HSP, often without a causative link. Only in
about 35% of cases can HSP be traced to any of these causes.
The exact cause of HSP is unknown, but most of its features are due to the
deposition of abnormal antibodies in the wall of blood vessels, leading to
vasculitis. These antibodies are of the subclass IgA1 in polymers; it is
uncertain whether the main cause is overproduction (in the digestive tract
or the bone marrow) or decreased removal of abnormal IgA from the
circulation. It is suspected that abnormalities in the IgA1 molecule may
provide an explanation for its abnormal behaviour in both HSP and the
related condition IgA nephropathy. One of the characteristics of IgA1 (and
IgD) is the presence of an 18 amino acid-long "hinge region" between
complement-fixating regions
Pain killers may be needed for the abdominal and joint pains. It is uncertain
as to whether HSP needs treatment beyond controlling the symptoms.
Most patients do not receive therapy because of the high spontaneous
recovery rate. Steroids are generally avoided. However, if they are given
early in the disease episode, the duration of symptoms may be shortened,
and abdominal pain can improve significantly. Moreover, the chance of
severe kidney problems may be reduced. However, some evidence
111
suggests that steroids do not decrease the likelihood of developing longterm kidney disease.
Evidence of worsening kidney damage would normally prompt a kidney
biopsy. Treatment may be indicated on the basis of the appearance of the
biopsy sample; various treatments may be used, ranging from oral steroids
to a combination of intravenous methylprednisolone (steroid),
cyclophosphamide and dipyridamole followed by prednisone. Other
regimens include steroids/azathioprine, and steroids/cyclophosphamide
(with or without heparin and warfarin). Intravenous immunoglobulin (IVIG)
is occasionally used.
Overall prognosis is good in most patients, with one study showing
recovery occurring in 94% and 89% of children and adults, respectively
(some having needed treatment). In children under ten, the condition recurs
in about a third of all cases and usually within the first four months after the
initial attack. Recurrence is more common in older children and adults.
Massage is contraindicated during the acute stage.
Herpes
Genital herpes is a disease caused by the herpes simplex virus (HSV), of
which there are two types. Type 1 (HSV-1) usually causes oral herpes, an
infection of the lips and mouth. Symptoms are commonly known as cold
sores or fever blisters. In the past, HSV-1 was not known to cause genital
herpes, but that is changing, especially among people who begin having
sex at a young age. Still, in most cases, genital herpes is caused by the
second type of herpes virus (HSV-2).
HSV-2 lives in the nerves. When it's active, it travels to the surface of the
infected area (skin or mucous membrane) and makes copies of itself. This
is called "shedding" because these new viruses can, at this time, rub off on
another person. Then the virus travels back down the nerve to a ganglion
(mass of nerve tissue), usually at the base of the spine, where it lies
dormant for a while.
About one-fifth of all people aged 12 and up in the U.S. are infected with
the HSV-2 virus that causes genital herpes, but as many as 90% don't
know it. (By comparison, experts estimate 50% to 80% of adults have oral
herpes.)
112
More women than men are infected -- one in four women compared with
one in five men. One reason may be that the virus can infect a woman's
genitals more easily than it can a man's. Genital herpes is more common
among blacks than it is among whites, and it becomes more common as
people age. The more sex partners people have, the more common it is,
too.
Herpes (Oral or Genital) Transmission
HSV-1 is usually passed from person to person by kissing. HSV-1 can also
spread from the mouth to the genitals during oral sex (fellatio, cunnilingus,
analingus). If this happens, it becomes a case of genital herpes.
HSV-2 is most often passed by vaginal sex and anal sex. But just as HSV-1
can infect the genitals and cause genital herpes, HSV-2 can pass from one
person's genitals to another person's mouth, resulting in oral herpes.
Why this matters to massage therapists:
HSV-1 and HSV-2 can survive outside the body, although for how long is a
matter of debate.
This means that the cloth on the face rest of your massage table or even
the linen on the table itself can harbor the virus and pass it on to the next
client, in theory29.
The CDC suggests that the virus can only last outside the body for a few
hours and that is only in the right conditions (warm and moist-like the
unchanged sheets of a massage table). It is possible (again, theoretically)
that if a massage therapist failed to change the linens on their table after
working on a client with an active Herpes infection and then had another
client use the same linens within a few minutes (as with back to back
appointments). While experts agree that it is possible, it’s highly unlikely.
Herpes zoster
Herpes zoster (or simply zoster), commonly known as shingles and also
known as zona, is a viral disease characterized by a painful skin rash with
blisters in a limited area on one side of the body (left or right), often in a
stripe. The initial infection with varicella zoster virus (VZV) causes the
29
Herpes Simplex Demystified By Ruth Werner, LMP, NCTMB, Massage Therapy Foundation President
113
acute, short-lived illness chickenpox which generally occurs in children and
young adults. Once an episode of chickenpox has resolved, the virus is not
eliminated from the body and can go on to cause herpes zoster often many
years after the initial infection. Herpes zoster is not the same disease as
herpes simplex, despite the name similarity; both the varicella zoster virus
and herpes simplex virus belong to the same viral subfamily
Alphaherpesvirinae.
After the initial episode of chickenpox resolves, the varicella zoster virus
remains latent in the nerve cell bodies and, less frequently, the nonneuronal satellite cells of the dorsal root, cranial nerve or autonomic
ganglia, without causing any symptoms. Years or decades after the initial
infection, the virus may break out of nerve cell bodies and travel down
nerve axons to cause viral infection of the skin in the region of the nerve.
The virus may spread from one or more ganglia along nerves of an affected
segment and infect the corresponding dermatome (an area of skin supplied
by one spinal nerve) causing a painful rash. Although the rash usually
heals within two to four weeks, some sufferers experience residual nerve
pain for months or years, a condition called postherpetic neuralgia. Exactly
how the virus remains latent in the body, and subsequently re-activates, is
not understood.
Throughout the world, the incidence rate of herpes zoster every year
ranges from 1.2 to 3.4 cases per 1,000 healthy individuals, increasing to
3.9–11.8 per year per 1,000 individuals among those older than 65 years.
Over a lifetime, a large fraction of people develop herpes zoster, though
usually only once; a 1965 16-year British study proposed that, of those
individuals living to age 85, 50% would likely have had at least one attack,
and 1% had at least two attacks.
The zoster (shingles) vaccine is considered the most effective way to
reduce incidence of herpes zoster and postherpetic neuralgia, and to
reduce severity of any outbreak. Antiviral drug treatment is considered a
second-line approach, but can reduce the severity and duration of herpes
zoster if a seven- to ten-day course of these drugs is started within 72
hours of the appearance of the characteristic rash.
The earliest symptoms of herpes zoster, which include headache, fever,
and malaise, are nonspecific, and may result in an incorrect diagnosis.
These symptoms are commonly followed by sensations of burning pain,
114
itching, hyperesthesia (oversensitivity), or paresthesia ("pins and needles":
tingling, pricking, or numbness). The pain may be mild to extreme in the
affected dermatome, with sensations that are often described as stinging,
tingling, aching, numbing or throbbing, and can be interspersed with quick
stabs of agonizing pain.
Herpes zoster in children is often painless, but older people are more likely
to get zoster as they age, and the disease tends to be more severe.
In most cases after one to two days, but sometimes as long as three
weeks, the initial phase is followed by the appearance of the characteristic
skin rash. The pain and rash most commonly occurs on the torso, but can
appear on the face, eyes or other parts of the body. At first the rash
appears similar to the first appearance of hives; however, unlike hives,
herpes zoster causes skin changes limited to a dermatome, normally
resulting in a stripe or belt-like pattern that is limited to one side of the body
and does not cross the midline. Zoster sine herpete ("zoster without
herpes") describes a patient who has all of the symptoms of herpes zoster
except this characteristic rash.
Later the rash becomes vesicular, forming small blisters filled with a serous
exudate, as the fever and general malaise continue. The painful vesicles
eventually become cloudy or darkened as they fill with blood, and crust
over within seven to ten days; usually the crusts fall off and the skin heals,
but sometimes, after severe blistering, scarring and discolored skin remain.
Herpes viruses of all kinds warrant a local contraindication and proper
laundering of linens due to its highly infectious nature.
Human Papilloma Virus (HPV)
Human papillomavirus (HPV) is a DNA virus from the papillomavirus family
that is capable of infecting humans. Like all papillomaviruses, HPVs
establish productive infections only in keratinocytes of the skin or mucous
membranes. Most HPV infections are subclinical and will cause no physical
symptoms; however, in some people subclinical infections will become
clinical and may cause benign papillomas (such as warts [verrucae] or
squamous cell papilloma), or cancers of the cervix, vulva, vagina, penis,
oropharynx and anus. HPV has been linked with an increased risk of
cardiovascular disease. In addition, HPV 16 and 18 infections are a cause
of a unique type of oropharyngeal (throat) cancer.
115
More than 30 to 40 types of HPV are typically transmitted through sexual
contact and infect the anogenital region. Some sexually transmitted HPV
types may cause genital warts. Persistent infection with "high-risk" HPV
types—different from the ones that cause skin warts—may progress to
precancerous lesions and invasive cancer. HPV infection is a cause of
nearly all cases of cervical cancer. However, most infections do not cause
disease.
Seventy percent of clinical HPV infections, in young men and women, may
regress to subclinical in one year and ninety percent in two years.
However, when the subclinical infection persists—in 5% to 10% of infected
women—there is high risk of developing precancerous lesions of the vulva
and cervix, which can progress to invasive cancer. Progression from
subclinical to clinical infection may take years; providing opportunities for
detection and treatment of pre-cancerous lesions. Progression to invasive
cancer can be prevented when subclinical HPV infection is detected early
and regular examinations are performed.
In more developed countries, cervical screening using a Papanicolaou
(Pap) test or liquid-based cytology is used to detect abnormal cells that
may develop into cancer. If abnormal cells are found, women are invited to
have a colposcopy. During a colposcopic inspection, biopsies can be taken
and abnormal areas can be removed with a simple procedure, typically with
a cauterizing loop or, more commonly in the developing world—by freezing
(cryotherapy). Treating abnormal cells in this way can prevent them from
developing into cervical cancer.
Pap smears have reduced the incidence and fatalities of cervical cancer in
the developed world, but even so there were 11,000 cases and 3,900
deaths in the U.S. in 2008. Cervical cancer has substantial mortality in
resource-poor areas; worldwide, there are an estimated 490,000 cases and
270,000 deaths each year.
HPV vaccines (Cervarix and Gardasil), which prevent infection with the
HPV types (16 and 18) that cause 70% of cervical cancer, may lead to
further decreases.
Over 120 HPV types have been identified and are referred to by number.
Types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82 are
116
carcinogenic "high-risk" sexually transmitted HPVs and may lead to the
development of cervical intraepithelial neoplasia (CIN), vulvar intraepithelial
neoplasia (VIN), penile intraepithelial neoplasia (PIN), and/or anal
intraepithelial neoplasia (AIN).
Papilloma
All HPV infections can cause warts (verrucae), which are noncancerous
skin growths. Infection with these types of HPV causes a rapid growth of
cells on the outer layer of the skin. Types of warts include:
Common warts: Some "cutaneous" HPV types cause common skin warts.
Common warts are often found on the hands and feet, but can also occur in
other areas, such as the elbows or knees. Common warts have a
characteristic cauliflower-like surface and are typically slightly raised above
the surrounding skin. Cutaneous HPV types can cause genital warts but
are not associated with the development of cancer.
Plantar warts are found on the soles of the feet. Plantar warts grow inward,
generally causing pain when walking.
Subungual or periungual warts form under the fingernail (subungual),
around the fingernail or on the cuticle (periungual). They may be more
difficult to treat than warts in other locations.
Flat warts: Flat warts are most commonly found on the arms, face or
forehead. Like common warts, flat warts occur most frequently in children
and teens. In people with normal immune function, flat warts are not
associated with the development of cancer.
Genital warts are quite contagious, while common, flat, and plantar warts
are much less likely to spread from person to person. They are still local
contraindications for massage.
Hutchinson’s summer prurigo
Hutchinson’s summer prurigo is a common sunlight-induced, pruritic,
papular or nodular skin eruption.
The cause for actinic prurigo is unknown, however researchers believe that
protein in our bodies may be a cause to the condition also: UV-A and UV-B
light seem to be the main provoking agents. This observation is supported
117
by the fact that most patients live at high altitudes (>1000 m above sea
level), and the condition improves in many patients when they move to
lower altitudes. However, some patients who are affected already live at
sea level.
Hutchinson’s summer prurigo is characterized by itchy, inflamed papules,
nodules, and plaques on the skin. Lesions typically appear hours or days
after exposure of the skin to UV light, and follow a general pattern of sunexposed areas. The face, neck, arms, hands, and legs are often affected,
although lesions sometimes appear on skin that is covered by clothing and
thus not exposed to UV light, thus making AP somewhat difficult to
diagnose.
Symptoms usually worsen in the spring and summer as the day lengthens
and exposure to exams increase.
Currently there is no cure for actinic prurigo, and treatment focuses on
relieving the dermatologic symptoms, by way of topical steroid creams or
systemic immunosuppressants.
All people with Hutchinson’s summer prurigo are encouraged by their
doctor to minimize sun exposure, and to use strong sunscreen throughout
the year, and even on cloudy or overcast days, as UVA light, unlike UVB
light, is able to penetrate cloud cover and remains constant throughout the
day.
Massage therapy is contraindicated during Hutchinson’s summer prurigo
skin eruptions.
Ichthyosis
Ichthyosis (plural ichthyoses) is a heterogeneous family of at least 28,
generalized, mostly genetic skin disorders.
All types of ichthyosis have dry, thickened, scaly or flaky skin. In many
types there is cracked skin, which is said to resemble the scales on a fish;
the word ichthyosis comes from the Ancient Greek ἰχθύς (ichthys), meaning
"fish."
The severity of symptoms can vary enormously, from the mildest, most
common, type such as ichthyosis vulgaris which may be mistaken for
118
normal dry skin up to life-threatening conditions such as harlequin type
ichthyosis. Ichtyosis vulgaris accounts for more than 95% of cases.
There are many types of ichthyoses and an exact diagnosis may be
difficult. Types of ichthyoses are classified by their appearance and their
genetic cause. Ichthyosis caused by the same gene can vary considerably
in severity and symptoms. Some ichthyoses do not appear to fit exactly into
any one type. Also different genes can produce ichthyoses with similar
symptoms. Of note, X-linked ichthyosis is associated with Kallmann
syndrome (close to KAL1 gene).
A physician often can diagnose ichthyosis by looking at the skin. A family
history is very useful. In some cases, a skin biopsy is done to help to
confirm the diagnosis. In some instances, genetic testing may be helpful in
making a diagnosis. Diabetes has not been definitively linked to acquired
ichthyosis or ichthyosis vulgaris; however, there are case reports
associating new onset ichthyosis with diabetes.
Ichthyosis is not more or less common in any ethnic group. As of now,
there is no way to prevent ichthyosis.
Treatments for ichthyosis often take the form of topical application of
creams and emollient oils, in an attempt to hydrate the skin. Creams
containing lactic acid have been shown to work exceptionally well in some
cases. Applicaton of Propylene Glycol has been used as another treatment
method. Retinoids are also used for some conditions.
Exposure to sunlight may improve or worsen the condition. In some cases,
excess dead skin sloughs off much better from wet tanned skin after
bathing or a swim, although the dry skin might be preferable to the
damaging effects of sun exposure.
There can be ocular manifestations of ichthyosis, such as corneal and
ocular surface diseases. Vascularizing keratitis, which is more commonly
found in congenital keratitis-ichythosis-deafness (KID), may worsen with
isotretinoin therapy.
Massage therapy is not contraindicated for Ichthyosis.
119
Impetigo
Impetigo is a highly contagious bacterial skin infection most common
among pre-school children. People who play close contact sports such as
rugby, American football and wrestling are also susceptible, regardless of
age. Antibiotic creams or pills are often used as a remedy.
Globally impetigo affected approximately 140 million people (2% of the
population) in 2010. Impetigo is not as common in adults. The name
derives from the Latin impetere ("assail"). It is also known as school sores.
This most common form of impetigo, also called nonbullous impetigo, most
often begins as a red sore near the nose or mouth which soon breaks,
leaking pus or fluid, and forms a honey-colored scab, followed by a red
mark which heals without leaving a scar. Sores are not painful, but may be
itchy. Lymph nodes in the affected area may be swollen, but fever is rare.
Touching or scratching the sores may easily spread the infection to other
parts of the body. Ulcerations with erythema and scarring also may result
from scratching or abrading of the skin.
Bullous impetigo, mainly seen in children younger than 2 years, involves
painless, fluid-filled blisters, mostly on the arms, legs and trunk, surrounded
by red and itchy (but not sore) skin. The blisters may be large or small.
After they break, they form yellow scabs.
In this form of impetigo, painful fluid- or pus-filled sores with redness of
skin, usually on the arms and legs, become ulcers that penetrate deeper
into the dermis. After they break open, they form hard, thick, gray-yellow
scabs, which sometimes leave scars. Ecthyma may be accompanied by
swollen lymph nodes in the affected area.
It is primarily caused by Staphylococcus aureus, and sometimes by
Streptococcus pyogenes. According to the American Academy of Family
Physicians, both bullous and nonbullous are primarily caused by
Staphylococcus aureus, with Streptococcus also commonly being involved
in the nonbullous form."
The infection is spread by direct contact with lesions or with nasal carriers.
The incubation period is 1–3 days after exposure to Streptococcus and 4–
10 days for Staphylococcus. Dried streptococci in the air are not infectious
to intact skin. Scratching may spread the lesions.
120
Impetigo generally appears as honey-colored scabs formed from dried
serum, and is often found on the arms, legs, or face.
For generations, the disease was treated with an application of the
antiseptic gentian violet. Today, topical or oral antibiotics are usually
prescribed. Treatment may involve washing with soap and water and letting
the impetigo dry in the air. Mild cases may be treated with bactericidal
ointment, such as mupirocin, which in some countries may be available
over-the-counter. More severe cases require oral antibiotics, such as
dicloxacillin, flucloxacillin or erythromycin. Alternatively amoxicillin
combined with clavulanate potassium, cephalosporins (1st generation) and
many others may also be used as an antibiotic treatment.
Globally impetigo affected approximately 140 million people (2% of the
population) in 2010.
Massage therapy is contraindicated for Impetigo due to its infectious
nature.
Keratoacanthoma
Keratoacanthoma is a skin lesion that erupts in sun damaged skin, rather
like a little volcano. It grows for a few months, then may shrink and resolve
by itself. Keratoacanthoma is considered by many experts to be a variant of
squamous cell carcinoma (SCC). As it cannot be clinically reliably
distinguished from more serious forms of skin cancer, keratoacanthomas
are usually treated surgically.
Keratoacanthoma may start at the site of a minor injury to sun damaged
and hair-bearing skin. At first it may appear as a small pimple or boil and
may be squeezed but is found to have a solid core filled with keratin
(scale). It then grows rapidly and it may be up to 2cm in diameter by the
time it is brought to the attention of the doctor.
Keratoacanthoma arises from hair follicle skin cells for unknown reasons.
Some keratoacanthomas appear to be related to infection with human
papilloma virus (HPV), the cause of warts, but the majority of
keratoacanthomas are not found to be due to HPV.
121
Keratoacanthomas should be treated for several reasons.
Massage therapy is locally contraindicated for Keratoacanthomas due to
the skin not being intact.
Keratolysis exfoliativa
Keratolysis exfoliativa is a sometimes harmless, sometimes painful skin
condition that can affect the focal surface of the fingers and/or the palm or
soles of the feet. It is often misdiagnosed as chronic contact dermatitis or
psoriasis. It is characterized by dry skin and superficial, air-filled blisters.
These blisters can be peeled off very easily and will leave reddish, tender
areas. The loss of this horny layer of the skin, which protects the underlying
layers, leaves the skin more vulnerable to dryness and cracking.
Keratolysis exfoliativa normally appears during warm weather. Due to
excessive sweating and friction, in for example athletic shoes, the skin can
start to exfoliate. Other factors that can cause exfoliation are detergents
and solvents. Another very common cause has been reported from salt
water fishermen, who often suffer from these symptoms. It is not sure
whether it is from the salt water or whether it is from some bacteria from
fish.
Normally, exfoliation is restricted to a particular area and normal skin will
replace the exfoliated parts, so no treatment is needed. Since keratolysis
exfoliativa is caused by friction, detergents, and solvents, these factors
should be avoided. Creams, especially those with silicone and lactic acid
are also helpful. In severe cases, photochemotherapy is an option.
In most cases exfoliation resolves spontaneously and no lasting damage is
seen. On the other hand, some people experience cracking and even
bleeding in extreme cases.
Massage therapy is locally contraindicated.
Keratolysis, pitted
Pitted keratolysis is a descriptive title for a skin condition affecting the soles
of the feet.
It affects those who sweat profusely (hyperhidrosis) especially if they wear
occlusive shoes or boots for long periods.
122
The result is very smelly feet, due to infection of the soles. Either the
forefoot or the heel or both become white with clusters of punched-out pits.
The appearance is more dramatic when the feet are wet. Very rarely, the
fingers are similarly affected. There is a variant of pitted keratolysis where
there are more diffuse red areas on the soles.
Pitted keratolysis is caused by several bacterial species, including
corynebacteria, Dermatophilus congolensis, Kytococcus sedentarius,
actinomyces and streptomyces.
In moist conditions, the bacteria proliferate. The pitting is due to destruction
of the horny cells (stratum corneum) by protease enzymes produced by the
bacteria.
The bad smell is due to sulfur compounds produced by the bacteria.
The presence of the bacteria, compromised skin tissue and overall
stinkyness of the feet warrant a local contraindication.
Lentigo
A lentigo (plural: lentigines) is a small pigmented spot on the skin with a
clearly defined edge, surrounded by normal-appearing skin. It is a harmless
(benign) hyperplasia of melanocytes which is linear in its spread. This
means the hyperplasia of melanocytes is restricted to the cell layer directly
above the basement membrane of the epidermis where melanocytes
normally reside. This is in contrast to the "nests" of multi-layer melanocytes
found in moles (melanocytic nevi). Because of this characteristic feature,
the adjective "lentiginous" is used to describe other skin lesions that
similarly proliferate linearly within the basal cell layer.
Lentigines are distinguished from freckles (ephelis) based on the
proliferation of melanocytes. Freckles have a relatively normal number of
melanocytes but an increased amount of melanin. A lentigo has an
increased number of melanocytes. Freckles will increase in number and
darkness with sunlight exposure, whereas lentigines will stay stable in their
color regardless of sunlight exposure.
Conditions characterized by lentigines include:
123
Lentigo simplex
Lentigo simplex (also known as "Simple lentigo") is the most common form
of lentigo. A single lesion or multiple lesions (lentigines) may be present at
birth or more commonly first develop in early childhood. Lentigo simplex is
not induced by sun exposure, and it is not associated with any medical
diseases or conditions. It is also referred to as simple lentigo and juvenile
lentigo. This condition also affects cats, those with orange coloration most
often, and can appear on the nose, lips, and eyes as the cat ages.
Solar lentigo
Solar lentigo, aka Liver spots are blemishes on the skin associated with
aging and exposure to ultraviolet radiation from the sun. They range in
color from light brown to red or black and are located in areas most often
exposed to the sun, particularly the hands, face, shoulders, arms and
forehead, and the scalp if bald.
The spots derive their name from the fact that they were once incorrectly
believed to be caused by liver problems, but they are physiologically
unrelated to the liver, save for a similar color. From the age of 40 onward
the skin is less able to regenerate from sun exposure, and liver spots are
very common in this age group, particularly in those who spend time in the
sun.
In the vast majority of cases, liver spots pose no threat and require no
treatment, though they occasionally have been known to obscure the
detection of skin cancer. However, despite being a benign condition, liver
spots are sometimes considered unsightly and some people choose to
have them removed. This can be done by electrosurgery, laser treatment or
cryotherapy.
Ink spot lentigo
Ink spot lentigo (also known as "Sunburn lentigo") is a cutaneous condition
characterized by skin lesions commonly occurring on the shoulders.
Centrofacial lentiginosis
Centrofacial lentiginosis is a cutaneous condition characterized by
lentigines on the nose and adjacent cheeks.
Most forms of lentigines are harmless abnormal skin coloring and pose no
threat to the massage therapist or the client themselves. Massage is
124
perfectly safe for people with most lentigines. The one form of Lentigo that
is not harmless for the client is the maligna variety, which is discussed next.
Lentigo maligna
Lentigo maligna is a precursor to lentigo maligna melanoma, a potentially
serious form of skin cancer.
Lentigo maligna is an early form of melanoma in which the malignant cells
are confined to the tissue of origin, the epidermis, hence it is often reported
as ‘in situ’ melanoma. It occurs in sun damaged skin so is generally found
on the face or neck, particularly the nose and cheek. It grows slowly in
diameter over 5 to 20 years or longer.
Lentigo maligna melanoma is diagnosed when the malignant melanoma
cells have invaded into the dermis and deeper layers of skin. Lentigo
maligna has a lower rate of transformation to invasive melanoma than the
other forms of melanoma in situ (under 5% overall). However, the risk of
invasive melanoma is greater in larger lesions, with up to 50% of those with
diameter of greater than 4 cm being reported to have an invasive focus.
The risk of lentigo maligna relates to sun damage. Thus lentigo maligna is
more common in outdoor workers, in older people and in association with
solar damage and non-melanoma skin cancer. Although often occurring in
those with very fair skin (skin phototype 1 and 2), it may also occur in those
who tan quite easily (phototype 3). It is rare in brown or black skin
(phototype 4-6).
Lentigo maligna is more common in males than females. The majority of
patients with lentigo maligna are older than 40 years, and the peak age of
diagnosis is be between 60 and 80 years.
Unlike superficial spreading melanoma, lentigo maligna is not related to the
number of melanocytic naevi (moles) or atypical naevi.
Lentigo maligna presents as a slowly growing or changing patch of
discoloured skin. At first, it often resembles common freckles or brown
marks (lentigines). It becomes more distinctive in time, often growing to
several centimetres over several years or even decades. The
characteristics of lentigo maligna include:
125
Large size: >6 mm and often several centimetres in diameter at diagnosis
Irregular shape
Variable pigmentation – colours may include light brown or tan, dark brown,
pink, red or white
Smooth surface.
If you suspect that the Lentigo on the client is of the malignant variety you
should consider the area to be locally contraindicated and advise them to
seek an opinion from a qualified medical specialist.
Livedo reticularis
Livedo reticularis refers to a condition in which dilation of capillary blood
vessels and stagnation of blood within these vessels causes mottled
discolouration of the skin. It is described as being reticular (net-like)
cyanotic (reddish blue discolouration) cutaneous discolouration surrounding
pale central areas. It occurs mostly on the legs, arms and trunk and is more
pronounced in cold weather.
The appearance is due to altered flow in small blood vessels feeding the
upper skin so that other vessels dilate to compensate. This can arise for a
variety of reasons.
Cutis marmorata causes temporary livedo in about 50% of normal infants
and many adults when exposed to the cold and is a physiological response
to cold. It is more intense and persistent in conditions associated with
debility and other factors that cause stasis within blood vessels. The
mottling is diffuse, temporary, mild and usually symptomless.
Cutis marmorata telangiectatica congenita is a rare condition in which the
livedo is present at birth or soon after. There may be other congenital
abnormalities including neurological and intellectual problems, and it can
be familial. The livedo is usually severe but may improve with age.
Idiopathic livedo reticularis (i.e. cause unknown) occurs most commonly in
young and middle-aged females, particularly during winter. Mottling occurs
first only on exposure to cold but can become permanent. Tingling and
numbness on cold exposure are common. Sometimes swelling, and rarely
ulcers may develop in winter. In another less common variant, swelling of
the feet and ankles and ulceration occurs in the spring and summer
months.
126
There is no treatment for livedo reticularis. Rewarming the area in
idiopathic cases or treatment of the underlying cause of secondary livedo
may reverse the discolouration. However, over time the vessels become
permanently dilated and livedo reticularis becomes permanent regardless
of the surrounding temperature.
Massage therapy is indicated for Livedo reticularis, other than the
discoloration of the skin it represents no harm to the client or the therapist.
Lupus Erythematosus
Lupus Erythematosus is a chronic autoimmune disorder that causes
inflammation of various parts of the body. Many people with lupus suffer
from mild symptoms that affect only a few of their organs, for others it is
systemic and can cause serious health issues, including death.
As we have already covered the last section the body’s immune system
normally makes proteins called antibodies to protect the body against
viruses, bacteria and other foreign materials, which we refer to as antigens.
In an immune disorder such as lupus, something has gone wrong with the
body’s ability to tell the difference between foreign substances (antigens)
and its own cells and tissues. The unfortunate result of this dysfunction is
that the immune system then makes antibodies directed against “self”.
These antibodies called auto-antibodies, react with the “self” antigen to
form immune complexes. The immune complexes build up in the tissues
and can cause inflammation, injury to tissues and pain.
Different Types of Lupus
Discoid Lupus (also known as Cutaneous Lupus) is confined to the skin. It
is easily recognizable by the persistent flushing of the cheeks or disk-like
lesions (i.e. rash) that appear on the face, neck, scalp and other areas
exposed to ultraviolet light (sunlight, fluorescent light).
The rash is usually raised, scaly red but not itchy. These lesions, if not
adequately treated, may develop into permanent scars. If they involve the
scalp, they can result in bald spots.
127
If your massage client has noticeable raised lesions in an area where the
face rest will be applying pressure it is perfectly acceptable to ask them if
they believe they will be experiencing any discomfort while lying face down.
I know that it’s not always easy for us to ask questions like that, because
we do not want to make the client self conscious. Remember that they live
with this condition on a daily basis, they are very much aware that you can
see the scars and the rash; it’s okay to ask as long as you are tactful. I
always explain my procedures quickly and briefly before we get started, so
it’s as easy as saying
“When you are face down your face will be here on this face rest” (pointing
at face rest) “are you comfortable with being in that position? If not I can
adjust the techniques so that we can do them all with you in a face up
position.”
Subacute cutaneous lesions may appear as areas of red scaly skin with
distinct edges, or as red, ring-shaped lesions. They usually appear on the
scalp and face, due to their frequent exposure to ultraviolet light, but they
can also appear on the back, legs or shoulders. Even though they are not
contagious you will still want to avoid touching them directly, since we
always approach skin that is not intact with universal precautions.
Cancer can develop in discoid lesions that your client has had for a long
time, so tell your client if you notice a lesion that appears even more “red or
swollen” than it normally does. This is especially important if your client
can’t see it for themselves (i.e. it’s on their back).
Approximately 10 percent of people with discoid lupus later develop
systemic lupus, but these people probably had systemic lupus to begin
with, with Acute cutaneous lupus lesions as the first symptom.
Acute cutaneous lupus lesions generally take the form of the malar rash.
This is a very distinctive rash that consists of flattened areas of red skin on
the face that resemble a sunburn. When the rash appears on both cheeks
and across the bridge of the nose in the shape of a butterfly, it is known as
the "butterfly rash." However, the rash can also appear on the arms, legs,
and body. These lesions tend to be especially photosensitive. They
typically do not produce scarring, although changes in skin color may
occur.
128
The Malar rash isn’t just the most well-known and distinctive symptom of
Lupus; it is also the source of the diseases name.
Lupus takes its name from the Latin word "lupus", meaning wolf.
This is because a malar rash on a person's face is very similar to the
pattern of fur on the face of many breeds of wolf (darker hair on the cheeks
or jowl area and white around the eyes).
Robert Willan (1757-1812), was a British Dermatologist and in 1808, he
used the word lupus to describe cutaneous tuberculosis, especially when
this was located on the face. He published this in a book some time after
that and the name stuck.
Systemic Lupus Erythematosus (SLE) is a more sever form of lupus.
Unlike discoid lupus it can affect almost any organ in the body. For some
people this may be limited to just skin and joint involvement, while in others
the lungs, heart, kidneys and blood may be affected.
Systemic Lupus Erythematosus is characterized by long periods of time in
which few symptoms are evident, punctuated with short bouts of symptom
activity that is generally referred to as a “flare”. Periods of improvement
may last weeks, months, or even years. The disease tends to remit over
time.
Lupus is not a skin disease, we mention it in this course only because so
many of the most common symptoms are related to the skin. It is a very
complex condition, and one that massage therapy can greatly benefit,
which is why we offer a separate course (APS004 Massage Therapy and
Lupus).
For now suffice it to say that massage is contraindicated for Lupus during
periods of flare up, but is highly beneficial when not in the acute stage.
Lyme disease
Lyme disease is an infectious disease caused by at least three species of
bacteria belonging to the genus Borrelia. Early symptoms may include
fever, headache, and fatigue. A rash occurs in 70–80% of infected persons
at the site of the tick bite after a delay of 3–30 days (average is about 7
129
days), and may or may not appear as the well-publicized bull's-eye
(erythema migrans). The rash is only rarely painful or itchy, although it may
be warm to the touch. About 20–30% of infected persons do not experience
a rash. Left untreated, later symptoms may involve the joints, heart, and
central nervous system. In most cases, the infection and its symptoms are
eliminated by antibiotics, especially if the illness is treated early. Delayed or
inadequate treatment can lead to more serious symptoms, which can be
disabling and difficult to treat.
Borrelia burgdorferi sensu stricto is the main cause of Lyme disease in
North America, whereas Borrelia afzelii and Borrelia garinii cause most
European cases. Borrelia is transmitted to humans by the bite of infected
ticks belonging to a few species of the genus Ixodes ("hard ticks"). Lyme
disease is the most common tick-borne disease in the Northern
Hemisphere.
The disease is named after the towns of Lyme and Old Lyme, Connecticut,
US, where a number of cases were identified in 1975. Although it was
known that Lyme disease was a tick-borne disease as far back as 1978,
the cause of the disease remained a mystery until 1981, when B.
burgdorferi was identified by entomologist Dr. Willy Burgdorfer.
Lyme disease can affect multiple body systems and produce a range of
symptoms. Not all patients with Lyme disease will have all symptoms, and
many of the symptoms are not specific to Lyme disease, but can occur with
other diseases, as well. The incubation period from infection to the onset of
symptoms is usually one to two weeks, but can be much shorter (days), or
much longer (months to years).
Symptoms most often occur from May to September, because the nymphal
stage of the tick is responsible for most cases.
Asymptomatic infection exists, but occurs in less than 7% of infected
individuals in the United States. Asymptomatic infection may be much more
common among those infected in Europe.
The only area affected is where the infection has first come into contact
with the skin. The classic sign of early local infection with Lyme disease is a
circular, outwardly expanding rash called erythema chronicum migrans
(also erythema migrans or EM), which occurs at the site of the tick bite
130
three to 30 days after the tick bite. The rash is red, and may be warm, but
is generally painless. Classically, the innermost portion remains dark red
and becomes indurated (is thicker and firmer); the outer edge remains red;
and the portion in between clears, giving the appearance of a bull's eye.
However, partial clearing is uncommon, and the bull's-eye pattern more
often involves central redness.
The EM rash associated with early infection is found in about 80% of
patients and can have a range of appearances including the classic target
bull's-eye lesion and nontarget appearing lesions. The 20% without the EM
and the nontarget lesions can often cause misidentification of Lyme
disease. Patients can also experience flu-like symptoms, such as
headache, muscle soreness, fever, and malaise. Lyme disease can
progress to later stages even in patients who do not develop a rash.
Within days to weeks after the onset of local infection, the Borrelia bacteria
may begin to spread through the bloodstream. EM may develop at sites
across the body that bear no relation to the original tick bite. Another skin
condition, apparently absent in North American patients, but occurs in
Europe, is borrelial lymphocytoma, a purplish lump that develops on the ear
lobe, nipple, or scrotum. Other discrete symptoms include migrating pain in
muscles, joints, and tendons, and dizziness and heart palpitations from
conduction irregularities such as third-degree heart block.
Various acute neurological problems, termed neuroborreliosis, appear in
10–15% of untreated patients. These include facial palsy, which is the loss
of muscle tone on one or both sides of the face, as well as meningitis,
which involves severe headaches, neck stiffness, and sensitivity to light.
Radiculoneuritis causes shooting pains that may interfere with sleep, as
well as abnormal skin sensations. Mild encephalitis may lead to memory
loss, sleep disturbances, or mood changes. In addition, some case reports
have described altered mental status as the only symptom seen in a few
cases of early neuroborreliosis. The disease may also have cardiac
manifestations such as atrioventricular block.
After several months, untreated or inadequately treated patients may go on
to develop severe and chronic symptoms that affect many parts of the
body, including the brain, nerves, eyes, joints, and heart. Many disabling
symptoms can occur, including permanent impairment of motor or sensory
function of the lower extremities in extreme cases. The associated nerve
131
pain radiating out from the spine is termed Bannwarth syndrome, named
after Alfred Bannwarth.
The late disseminated stage is where the infection has fully spread
throughout the body. Chronic neurologic symptoms occur in up to 5% of
untreated patients. A polyneuropathy that involves shooting pains,
numbness, and tingling in the hands or feet may develop. A neurologic
syndrome called Lyme encephalopathy is associated with subtle cognitive
problems, such as difficulties with concentration and short-term memory.
These patients may also experience fatigue. However, other problems,
such as depression and fibromyalgia, are no more common in people with
Lyme disease than in the general population.
Chronic encephalomyelitis, which may be progressive, can involve
cognitive impairment, weakness in the legs, awkward gait, facial palsy,
bladder problems, vertigo, and back pain. In rare cases, untreated Lyme
disease may cause frank psychosis, which has been misdiagnosed as
schizophrenia or bipolar disorder. Panic attacks and anxiety can occur;
also, delusional behavior may be seen, including somatoform delusions,
sometimes accompanied by a depersonalization or derealization syndrome,
where the patients begin to feel detached from themselves or from reality.
Lyme arthritis usually affects the knees. In a minority of patients, arthritis
can occur in other joints, including the ankles, elbows, wrist, hips, and
shoulders. Pain is often mild or moderate, usually with swelling at the
involved joint. Baker's cysts may form and rupture. In some cases, joint
erosion occurs.
Acrodermatitis chronica atrophicans (ACA) is a chronic skin disorder
observed primarily in Europe among the elderly. ACA begins as a reddishblue patch of discolored skin, often on the backs of the hands or feet. The
lesion slowly atrophies over several weeks or months, with the skin
becoming first thin and wrinkled and then, if untreated, completely dry and
hairless.
Lyme disease is caused by spirochetal bacteria from the genus Borrelia.
Spirochetes are surrounded by peptidoglycan and flagella, along with an
outer membrane similar to other Gram-negative bacteria. Because of their
double-membrane envelope, Borrelia bacteria are often mistakenly
described as Gram negative despite the considerable differences in their
132
envelope components from Gram-negative bacteria. The Lyme-related
Borrelia species are collectively known as Borrelia burgdorferi sensu lato,
and show a great deal of genetic diversity.
B. burgdorferi sensu lato is made up of 18 closely related species, but only
three clearly cause Lyme disease: B. burgdorferi sensu stricto
(predominant in North America, but also present in Europe), B. afzelii, and
B. garinii (both predominant in Eurasia). Some studies have also proposed
B. bissettii and B. valaisiana may sometimes infect humans, but these
species do not seem to be important causes of disease.
Lyme disease is classified as a zoonosis, as it is transmitted to humans
from a natural reservoir among rodents by ticks that feed on both sets of
hosts. Hard-bodied ticks of the genus Ixodes are the main vectors of Lyme
disease (also the vector for Babesia). Most infections are caused by ticks in
the nymphal stage, as they are very small and may feed for long periods of
time undetected. Larval ticks are very rarely infected. Although deer are the
preferred hosts of deer ticks, and the size of the tick population parallels
that of the deer population, ticks cannot acquire Lyme disease spirochetes
from deer. Rather, deer ticks acquire Borrelia microbes from infected
rodents, such as the white-footed mouse, Peromyscus leucopus.
Within the tick midgut, the Borrelia's outer surface protein A (OspA) binds
to the tick receptor for OspA, known as TROSPA. When the tick feeds, the
Borrelia downregulates OspA and upregulates OspC, another surface
protein. After the bacteria migrate from the midgut to the salivary glands,
OspC binds to Salp15, a tick salivary protein that appears to have
immunosuppressive effects that enhance infection. Successful infection of
the mammalian host depends on bacterial expression of OspC.
Tick bites often go unnoticed because of the small size of the tick in its
nymphal stage, as well as tick secretions that prevent the host from feeling
any itch or pain from the bite. However, transmission is quite rare, with only
about 1% of recognized tick bites resulting in Lyme disease. Transmission
may occur within 24 hours of the tick bite.
In Europe, the vector is Ixodes ricinus, which is also called the sheep tick or
castor bean tick. In China, Ixodes persulcatus (the taiga tick) is probably
the most important vector. In North America, the black-legged tick or deer
tick (Ixodes scapularis) is the main vector on the east coast.
133
The lone star tick (Amblyomma americanum), which is found throughout
the Southeastern United States as far west as Texas, is unlikely to transmit
the Lyme disease spirochaetes, though it may be implicated in a related
syndrome called southern tick-associated rash illness, which resembles a
mild form of Lyme disease.
On the West Coast of the United States, the main vector is the western
black-legged tick (Ixodes pacificus). The tendency of this tick species to
feed predominantly on host species such as lizards that are resistant to
Borrelia infection appears to diminish transmission of Lyme disease in the
West.
Transmission across the placenta during pregnancy has not been
demonstrated, and no consistent pattern of teratogenicity or specific
"congenital Lyme borreliosis" has been identified. As with a number of
other spirochetal diseases, adverse pregnancy outcomes are possible with
untreated infection; prompt treatment with antibiotics reduces or eliminates
this risk.
While Lyme spirochetes have been found in insects as well as ticks, reports
of actual infectious transmission appear to be rare. Lyme spirochete DNA
has been found in semen and breast milk, but transmission has not been
known to take place through sexual contact. According to the CDC, live
spirochetes have not been found in breast milk, urine, or semen. However,
more recent studies published in 2014, suggest there might be a link.
Ticks that transmit B. burgdorferi to humans can also carry and transmit
several other parasites, such as Theileria microti and Anaplasma
phagocytophilum, which cause the diseases babesiosis and human
granulocytic anaplasmosis (HGA), respectively. Among early Lyme disease
patients, depending on their location, 2–12% will also have HGA and 2–
40% will have babesiosis. Ticks in certain regions, including the lands
along the eastern Baltic Sea, also transmit tick-borne encephalitis.
Coinfections complicate Lyme symptoms, especially diagnosis and
treatment. It is possible for a tick to carry and transmit one of the
coinfections and not Borrelia, making diagnosis difficult and often elusive.
The Centers for Disease Control studied 100 ticks in rural New Jersey, and
found 55% of the ticks were infected with at least one of the pathogens.
134
Antibiotics are the primary treatment. The specific approach to their use is
dependent on the individual affected and the stage of the disease. For most
people with early localized infection, oral administration of doxycycline is
widely recommended as the first choice, as it is effective against not only
Borrelia bacteria but also a variety of other illnesses carried by ticks.
Doxycycline is contraindicated in children younger than eight years of age
and women who are pregnant or breastfeeding; alternatives to doxycycline
are amoxicillin, cefuroxime axetil, and azithromycin. Individuals with early
disseminated or late infection may have symptomatic cardiac disease,
refractory Lyme arthritis, or neurologic symptoms like meningitis or
encephalitis. Intravenous administration of ceftriaxone is recommended as
the first choice in these cases; cefotaxime and doxycycline are available as
alternatives30.
These treatment regimens last from one to four weeks. If joint swelling
persists or returns, a second round of antibiotics may be considered.
Outside of that, a prolonged antibiotic regimen lasting more than 28 days is
not recommended as no clinical evidence shows it to be effective. IgM and
IgG antibody levels may be elevated for years even after successful
treatment with antibiotics. As antibody levels are not indicative of treatment
success, testing for them is not recommended.
The risk of infectious transmission increases with the duration of tick
attachment. It requires between 36 and 48 hours of attachment for the
bacteria that causes Lyme to travel from within the tick into its saliva. If a
deer tick sufficiently likely to be carrying Borrelia is found attached to a
person and removed, and if the tick has been attached for 36 hours or is
engorged, a single dose of doxycycline administered within the 72 hours
after removal may reduce the risk of Lyme disease.
Like Lupus Lyme disease is not a skin disease, but the symptoms often
manifest on the skin and that is why we have detailed it here.
It cannot be transferred from person to person. Massage is contraindicated
for Lyme disease during the acute stage.
30
Wright WF, Riedel DJ, Talwani R, Gilliam BL (June 2012). "Diagnosis and management of Lyme disease". Am Fam Physician 85 (11): 1086–
93. PMID 22962880.
135
Melanoma
Melanoma is a type of skin cancer, which form from melanocytes (pigment
containing cells in the skin).
In women, the most common site is the legs and melanomas in men are
most common on the back. It is particularly common among Caucasians,
especially northern Europeans and northwestern Europeans living in sunny
climates. There are higher rates in Oceania, North America, Europe,
Southern Africa, and Latin America. This geographic pattern reflects the
primary cause, ultraviolet light (UV) exposure crossed with the amount of
skin pigmentation in the population. Melanocytes produce the dark
pigment, melanin, which is responsible for the color of skin. These cells
predominantly occur in skin, but are also found in other parts of the body,
including the bowel and the eye (see uveal melanoma). Melanoma can
originate in any part of the body that contains melanocytes.
The treatment includes surgical removal of the tumor. If melanoma is found
early, while it is still small and thin, and if it is completely removed, then the
chance of cure is high. The likelihood that the melanoma will come back or
spread depends on how deeply it has gone into the layers of the skin. For
melanomas that come back or spread, treatments include chemo- and
immunotherapy, or radiation therapy. Five year survival rates in the United
States are on average 91%.
Melanoma is less common than other skin cancers. However, it is much
more dangerous if it is not found in the early stages. It causes the majority
(75%) of deaths related to skin cancer. Globally in 2012 melanoma
occurred in 232,000 people and result in 55,000 deaths. Australia and New
Zealand have the highest rates of melanoma in the world. It has become
more common in the last 20 years in areas that are mostly Caucasian.
Early signs of melanoma are changes to the shape or color of existing
moles or, in the case of nodular melanoma, the appearance of a new lump
anywhere on the skin (such lesions should be referred without delay to a
dermatologist). At later stages, the mole may itch, ulcerate or bleed. Early
signs of melanoma are summarized by the mnemonic "ABCDE":
Asymmetry
Borders (irregular)
Color (variegated)
136
Diameter (greater than 6 mm (0.24 in), about the size of a pencil eraser)
Evolving over time
These classifications do not, however, apply to the most dangerous form of
melanoma, nodular melanoma, which has its own classifications:
Elevated above the skin surface
Firm to the touch
Growing
Metastatic melanoma may cause nonspecific paraneoplastic symptoms,
including loss of appetite, nausea, vomiting and fatigue. Metastasis of early
melanoma is possible, but relatively rare: less than a fifth of melanomas
diagnosed early become metastatic. Brain metastases are particularly
common in patients with metastatic melanoma. It can also spread to the
liver, bones, abdomen or distant lymph nodes.
In general, cancers are caused by damage to DNA. Melanomas are usually
caused by DNA damage resulting from exposure to ultraviolet (UV) light
from the sun. Ultraviolet UVB light (wavelengths between 315 – 280 nm)
from the sun is absorbed by skin cell DNA and results in a type of direct
DNA damage called cyclobutane pyrimidine dimers (CPDs), i.e. thyminethymine, cytosine-cytosine or cytosine-thymine dimers that are formed by
the joining of two adjacent pyrimidine bases within a strand of DNA.
Somewhat similarly to UVB, UVA light (longer wavelengths between 400 –
315 nm) from the sun or from tanning beds can also be directly absorbed
by skin DNA (at about 100 to 1000 fold lower efficiency than UVB is
absorbed). UVA light mainly causes thymine-thymine dimers. UVA also
produces reactive oxygen species and these generate other DNA
damages, primarily single strand breaks, oxidized pyrimidines and the
oxidized purine 8-oxoguanine (a mutagenic DNA damage) at 1/10th, 1/10th
and 1/3rd the frequencies of UVA-induced thymine-thymine dimers,
respectively.
If unrepaired, CPD photoproducts can lead to mutations by inaccurate
translesion synthesis during DNA replication or repair. The most frequent
mutations due to inaccurate synthesis past CPDs are cytosine to thymine
(C>T) or CC>TT transition mutations. These are commonly referred to as
UV fingerprint mutations, as they are the most specific mutation caused by
UV, being frequently found in sun-exposed skin but rarely found in internal
organs. Errors in DNA repair of UV photoproducts, or inaccurate synthesis
137
past these photoproducts, can also lead to deletions, insertions and
chromosomal translocations.
The entire genomes of 25 melanomas were sequenced (not only the
protein-coding regions of the genome which are just 1% of the genome).
On average, there were about 80,000 mutated bases (mostly C>T
transitions) and about 100 structural rearragements per melanoma
genome. This is a very high frequency, compared to the low mutation
frequency of about 70 new mutations in the entire genome between
generations (parent to child) in humans. Among the 25 melanomas, about
6,000 protein-coding genes had missense, nonsense or splice site
mutations.
Should a malignant melanoma be present you should consider it a local
contraindication.
Melkersson–Rosenthal syndrome
Melkersson–Rosenthal syndrome, is a rare neurological disorder
characterized by recurring facial paralysis, swelling of the face and lips
(usually the upper lip), and the development of folds and furrows in the
tongue. Onset is in childhood or early adolescence. After recurrent attacks
(ranging from days to years in between), swelling may persist and increase,
eventually becoming permanent. The lip may become hard, cracked, and
fissured with a reddish-brown discoloration. The cause of Melkersson–
Rosenthal syndrome is unknown, but there may be a genetic
predisposition.
Treatment is symptomatic and may include nonsteroidal anti-inflammatory
drugs (NSAIDs) and corticosteroids to reduce swelling, antibiotics and
immunosuppressants. Surgery may be indicated to relieve pressure on the
facial nerves and reduce swelling, but its efficacy is uncertain. Massage
and electrical stimulation may also be prescribed.
Melkersson–Rosenthal syndrome may recur intermittently after its first
appearance. It can become a chronic disorder.
Massage is indicated for Melkersson–Rosenthal syndrome.
138
Microsporum audounii
Microsporum audouinii is an anthropophilic fungus in the genus
Microsporum. It is a type of dermatophyte that colonizes keratinized tissues
(primarily hair) causing infection. The fungus is characterized by its spindle
shaped macroconidia (7-30 × 35-160 µm), clavate microconidia (2.5-3.5 ×
4-7 µm) as well as its pitted or spiny external walls.
This fungus is often found in soil that is rich in keratinous material.
However, there are other factors that can influence its growth, such as pH,
relative humidity, organic carbon, nitrogen and temperature. Microsporum
audouinii appears to prefer a neutral pH in the range of 6.8-7.0 and room
temperature for growth. Drastic increases or decreases in temperature can
inhibit its growth. Microsporum audouinii is effective in utilizing its carbon
sources, but growth is strongest in the hexoses (glucose, mannose and
fructose) and weakest in maltose, sucrose, lactose and galactose. It is
unable to synthesize the vitamins thiamine, niacin and riboflavin and
requires an exogenous supply of these materials to support its growth. The
fungus is only able to utilize organic nitrogen sources, particularly nitrogen
from arginine and urea.
Microsporum audouinii causes the infections Tinea capitis (scalp ringworm)
and Tinea corporis. These superficial dermal diseases are generally found
in prepubescent children (starting at 6 months) and rarely affect adults.
There are a few reasons why children are more susceptible to M. audouinii.
Differences in the chemical composition and quantity of the triglycerides in
hair sebum secreted are the primary reasons. In instances whereby the
triglyceride content in the sebum decreases so does the susceptibility of a
person to the fungus. Cases like those are seen in postmenopausal women
of whom suffer hormonal changes which can contribute to triglyceride
reduction. In addition, increased sweat production as well as the presence
of Pityrosporum ovale decreases the ability for M. audouinii to thrive.
Pityrosporum ovale is an opportunistic lipophilic yeast that is a part of the
human cutaneous flora in adults. In most cases of adult onset Tinea capitis
due to M. audouinii, there is at least one predisposing factor such as
immunocompromise (e.g., diabetes mellitus, systemic lupus, organ
transplant and HIV), a local animal reservoir (e.g., infected pet or farm
animal) and hormonal changes in postmenopausal women.
Generally, Tinea capitis is primarily seen in areas where there is high
immigration. Especially in tropical, rural and suburban regions. In the 19th
139
and early 20th centuries, M. audouinii was the primary fungus responsible
for Tinea capitis throughout the US and Western Europe. With the advent
of antimycotic agents, its prevalence has decreased. But in the poorer parts
of Africa, especially Central and West Africa, M. audouinii remains the
primary dermatophyte responsible for this disease. A recent increase in the
M. audouinii-related Tinea capitis in Europe is thought to be related to
migration of infected individuals from Africa.
Tinea capitis develops when an inoculum from another individual or animal
comes into a 'compromised scalp.' A compromised scalp can occurs when
the stratum corneum of the scalp is exposed. This can be due to trauma of
the scalp, tight hair braiding or hair styling with infected tools. In general,
fungal spread is facilitated by poverty, poor hygiene and overcrowding.
Once the fungus has entered the stratum corneum is continues to invade
the epidermis, it then enters a hair follicle, penetrates the hair shaft and
grows down the length of the hair. The hyphae grow distally until they reach
the upper limits of the zone of keratinization where the nucleated hair shaft
cornifies completely and is converted into hard, anucleated keratin. The
terminal end of the growing hyphae forms a ring (Adamson's Fringe). As
the hair continues to grow outwards, hyphae are brought to the surface
(scalp) and arthroconidia are produced. Eventually due to mechanical
forces (the movement of the fungi) and keratinase (a chymotrypsin-like
enzyme with optimal activity at an acidic pH), all but 1–2 mm of the
diseased hair follicle weakens and falls off. The remaining hair has a
characteristic dark grey appearance due to the Adamson's Fringe.
There is an array of different tests to differentiate between fungi. Direct
microscopy with 10% KOH would show small to medium conidia with
ectothrix hair invasion. Performing a wet mount would show 'racquet
shaped hyphae' with few macro and microconidia. Histological examination
of a diseased hair shows clefts that between the inner root sheath and hair.
Microsporum audouinii fluoresces when examined in ultraviolet light
(Wood's lamp). The two main growth media employed to test for M.
audouinii are Sabouraud's Dextrose agar and potato dextrose agar. On the
former, growth is slow with and poor sporulation with most strains
producing a few abortive macroconidia and sparse microconidia. The
colonies are flat, dense and cottony in texture with a greyish-white to
140
reddish brown hue. On Potato Dextrose agar, colonies are white with a
silky texture and a peach-coloured underside.
Microsporum audouinii can be differentiated from non-sporulating strains of
the similar M. canis by culture on autoclaved rice. Under these conditions,
M. canis typically yields abundant growth and little to no pigmentation
whereas M. audouinii produces no visible growth and abundant brown
pigment on the rice grains. PCR fingerprinting is a fairly new diagnostic tool
for the rapid identification of these fungi.
A symptomatic patient will present an unusual amount of itching and
alopecia. Primary treatment involves griseofulvin, an antimycotic agent. For
patients who don't respond to Griseofulvin, other drugs, Itraconazole,
fluconazole, and terbinafine can be used as a replacement to or in
conjunction with griseofulvin. These drugs are preferred over griseofulvin
as they have a shorter duration for treatment. However, these agents have
drug-drug interactions and over a prolonged period of time can cause liver
damage. Currently, squalamine, an aminosterol with fungicidal properties is
being researched as its mechanism of action is different from that of the
aforementioned medicines, making it a good drug for those who don't
respond well to Itraconazole, fluconazole or terbinafine. Systemic treatment
with oral medication and anti-fungal shampoos has also been effective.
Antifungal shampoos (Ketoconazole 2% shampoo or selenium sulfide 2.5%
) are effective as they reduce the transmission of the diseased hair by
preventing its shedding. Other treatments include, epilation of the infected
follicles, topical ointments and steroidal treatments. Topical ointments
immobilize the fungus and reduce shedding but they do not penetrate the
hair follicle and hence must be used in conjunction with other treatment
methods. Steroidal treatments aid in inflammation and pain reduction.
Griseofulvin inhibits fungal cell mitosis via disruption of the mitotic spindle
structure and preventing cell division at the metaphase stage. In addition, it
inhibits nucleic acid synthesis. Both Itraconazole and Fluconazole inhibits
the synthesis of ergosterol which is an important component of fungal cell
membranes. Consequently, Fluconazole use leads to changes in the
permeability and function of the cell membrane. Squalene epoxidase
contributes to the formation of ergosterol Terbinafine, inhibits squalene
epoxidase thereby preventing cell membrane formation.
141
The presence of Microsporum audouinii, as well as the resulting Tinea
capitis and Tinea corporis contraindicate massage therapy.
Molluscum contagiosum
Molluscum contagiosum is caused by a virus and usually causes a mild
skin disease. The virus affects only the outer (epithelial) layer of skin and
does not circulate throughout the body in healthy people.
The virus causes small white, pink, or flesh-colored raised bumps or
growths with a dimple or pit in the center. The bumps are usually smooth
and firm. In most people, the growths range from about the size of a
pinhead to as large as a pencil eraser (2 to 5 millimeters in diameter).
The bumps may appear anywhere on the body, alone or in groups. They
are usually painless, although they may be itchy, red, swollen and/or sore.
Molluscum usually disappears within 6 to 12 months without treatment and
without leaving scars. Some growths may remain for up to 4 years.
Molluscum infections occur worldwide but are more common in warm,
humid climates and where living conditions are crowded. There is evidence
that molluscum infections have been on the rise in the United States since
1966, but these infections are not routinely monitored because they are
seldom serious and routinely disappear without treatment.
Molluscum is common enough that you should not be surprised if you see
someone with it or if someone in your family becomes infected. Although
not limited to children, it is most common in children 1 to 10 years of age.
People with weakened immune systems (i.e., HIV-infected persons or
persons being treated for cancer) are at higher risk for getting molluscum,
and their growths may look different, be larger, and be more difficult to
treat.
The virus that causes molluscum is spread from person to person by
touching the affected skin. The virus may also be spread by touching a
surface with the virus on it, such as a towel, clothing, or toys. Once
someone has the virus, the bumps can spread to other parts of their body
by touching or scratching a bump and then touching another part of the
body. Molluscum can be spread from one person to another by sexual
contact.
142
Although the virus might be spread by sharing swimming pools, baths,
saunas, or other wet and warm environments, this has not been proven.
Researchers who have investigated this idea think it is more likely the virus
is spread by sharing towels and other items around a pool or sauna than
through water.
Molluscum looks like small white, pink, or flesh-colored raised bumps or
growths with a pit or dimple in the center. The bumps are usually smooth
and firm. They can be as small as the head of a pin and as large as a
pencil eraser (2 to 5 millimeters in diameter). The growths are usually
painless but may become itchy, sore and red and/or swollen. They may
occur anywhere on the body including the face, neck, arms, legs,
abdomen, and genital area, alone or in groups. The bumps are rarely found
on the palms of the hands or the soles of the feet.
Do not touch, pick, or scratch any skin with bumps or blisters.
The virus lives only in the skin and once the growths are gone, the virus is
gone and you cannot spread the virus to others.
Molluscum contagiosum is not like herpes viruses, which can remain
dormant (“sleeping”) in the body for long periods and then reappear. So,
assuming your client does not come in contact with another infected
person, once all the molluscum contagiosum bumps go away, they will not
develop any new bumps.
To prevent the spread of molluscum to other areas of the body or to other
people, it is important to keep every blister or bump covered either with
clothing or with a watertight bandage. However, to promote healthy skin,
they should remove the bandage at night and when there is no risk of
others coming into contact with their skin.
Cryotherapy (freezing the molluscum growth) is one treatment option. This
is the same way that warts are removed from the skin. Another option is to
remove the fluid inside the bumps (termed curettage). Lasers also can
remove molluscum bumps.
All three options may be a little painful and should only be done by a health
care professional. Both curettage and cryotherapy methods may leave
143
scars. In a small percentage of cases, natural healing of molluscum
contagiosum bumps lead to scars regardless of type of therapy.
Molluscum contagiosum is (as the name implies) highly contagious and
obviously contraindicates massage therapy.
Mycetoma
Mycetoma is a local, chronic, slowly progressive infection of skin,
subcutaneous tissues, fascia, bone, and muscle, most commonly of the
foot or hand, characterized by swelling or tumorfaction draining sinuses,
and granules; the exudate contains grains that may be yellow, white, red,
brown, or black depending on the causative microorganisms.
The first medical reports were from doctors in Madura, India--an alternate
name for the disease is Madura foot. The infection is characterized by an
abnormal tissue mass beneath the skin, formation of cavities within the
mass, and a fluid discharge.
Pathogens live in soil and enter through minor traumatic breaks in the skin.
Infection begins in skin and subcutaneous tissues, extending into fascial
planes, destroying contiguous tissues.
Mycetoma is more common in men than women, particularly those aged 20
to 50. It generally presents as a single lesion on an exposed site and may
persist for years. Two thirds arise on the foot. It starts as a small hard
painless lump under the skin, then grows slowly until the surface skin is
scarred and pale. Left unchecked it can result in considerable deformity
and often makes it difficult to walk.
Massage is contraindicated due to the infectious nature of the disease.
144
Mycetoma
Necrobiosis lipoidica
Necrobiosis lipoidica is a necrotising skin condition that usually occurs in
patients with diabetes but can also be associated with Rheumatoid Arthritis.
In the former case it may be called necrobiosis lipoidica diabeticorum
(NLD). NLD occurs in approximately 0.3% of the diabetic population, with
the majority of sufferers being women (approximately 3:1 females to males
affected).
The severity or control of diabetes in an individual does not affect who will
or will not get NLD. Better maintenance of diabetes after being diagnosed
with NLD will not change how quickly the NLD will resolve.
NL/NLD most frequently appears on the patient's shins, often on both legs,
although it may also occur on forearms, hands, trunk, and, rarely, nipple,
penis, and surgical sites. The lesions are often asymptomatic but may
become tender and ulcerate when injured. The first symptom of NL is often
a "bruised" appearance (erythema) that is not necessarily associated with a
known injury. The extent to which NL is inherited is unknown.
NLD appears as a hardened, raised area of the skin. The center of the
affected area usually has a yellowish tint while the area surrounding it is a
dark pink. It is possible for the affected area to spread or turn into an open
sore. When this happens the patient is at greater risk of developing ulcers.
145
If an injury to the skin occurs on the affected area, it may not heal properly
or it will leave a dark scar.
Although the exact cause of this condition is not known, it is an
inflammatory disorder characterised by collagen degeneration, combined
with a granulomatous response. It always involves the dermis diffusely, and
sometimes also involves the deeper fat layer. Commonly, dermal blood
vessels are thickened (microangiopathy).
It can be precipitated by local trauma, though it often occurs without any
injury.
NL is diagnosed by a skin biopsy, demonstrating superficial and deep
perivascular and interstitial mixed inflammatory cell infiltrate (including
lymphocytes, plasma cells, mononucleated and multinucleated histiocytes,
and eosinophils) in the dermis and subcutis, as well as necrotising
vasculitis with adjacent necrobiosis and necrosis of adnexal structures.
Areas of necrobiosis are often more extensive and less well defined than in
granuloma annulare. Presence of lipid in necrobiotic areas may be
demonstrated by Sudan stains. Cholesterol clefts, fibrin, and mucin may
also be present in areas of necrobiosis. Depending on the severity of the
necrobiosis, certain cell types may be more predominant. When a lesion is
in its early stages, neutrophils may be present, whereas in later stages of
development lymphocytes and histiocytes may be more predominant.
There is no clearly defined cure for necrobiosis. Although there are some
techniques that can be used to diminish the signs of necrobiosis such as a
steroid cream or injection into the affected area, this process may be
effective for only a small amount of those treated.
Necrobiosis lipoidica contraindicates massage therapy due to the presence
of open lesions in the skin.
Necrotizing fasciitis
Necrotizing fasciitis is a rare infection of the deeper layers of skin and
subcutaneous tissues, easily spreading across the fascial plane within the
subcutaneous tissue.
146
Necrotizing fasciitis is a fast moving and dangerous disease with a rapid
onset and is usually treated immediately with high doses of intravenous
antibiotics.
Type I describes a polymicrobial infection, whereas Type II describes a
monomicrobial infection. Many types of bacteria can cause necrotizing
fasciitis (e.g., Group A streptococcus (Streptococcus pyogenes),
Staphylococcus aureus, Vibrio vulnificus, Clostridium perfringens,
Bacteroides fragilis). Such infections are more likely to occur in people with
compromised immune systems, over 70% have at least one of the following
clinical situations: immunosuppression, diabetes, alcoholism/drug abuse,
malignancies, and chronic systemic diseases. It does occasionally occur in
people with an apparently normal general condition and really, really bad
luck.
The infection begins locally at a site of the injury (where the skin is
compromised). The severity of the injury itself is not a factor, it can happen
with a condition as minor as a non-venomous spider bite. In the early
stages, signs of inflammation may not be apparent if the bacteria are deep
within the tissue. If they are not deep, signs of inflammation, such as
redness and swollen or hot skin, develop very quickly. Skin color may
progress to violet, and blisters may form, with subsequent necrosis (death)
of the subcutaneous tissues.
Clients with this condition usually complain of intense pain that may seem
out of step with the minor appearance of the injury. With progression of the
disease, often within hours, tissue becomes swollen. Diarrhea and vomiting
are also common symptoms.
Clients with necrotizing fasciitis typically have a fever and appear very ill.
Mortality rates have been noted as high as 73 percent if left untreated.
Without surgery and medical assistance, such as antibiotics, the infection
will rapidly progress and will eventually lead to death.
It should be noted that the expression "Flesh-eating bacteria" is a
misnomer, as the bacteria do not actually "eat" the tissue. They do cause
destruction of skin and muscle by releasing toxins (virulence factors), which
include streptococcal pyogenic exotoxins. S. pyogenes produces an
exotoxin known as a superantigen. This toxin is capable of activating Tcells non-specifically, which causes the overproduction of cytokines and
147
severe systemic illness (Toxic shock syndrome). So really, it is just a matter
of semantics.
It should go without saying that this condition is contraindicated for
massage.
Netherton’s syndrome
Netherton syndrome is a severe, autosomal recessive form of ichthyosis
associated with mutations in the SPINK5 gene. It is named after Earl W.
Netherton (1910–1985), an American Dermatologist who discovered it in
1958.
Netherton syndrome is characterized by chronic skin inflammation,
universal pruritus (itch), severe dehydration, and stunted growth. Patients
with this disorder tend to have a hair shaft defect (trichorrhexis invaginata),
also known as "bamboo hair".
The disrupted skin barrier function in affected individuals also presents a
high susceptibility to infection and allergy, leading to the development of
scaly, reddish skin similar to atopic dermatitis. In severe cases, these
atopic manifestations persist throughout the individual's life, and
consequently post-natal mortality rates are high. In less severe cases, this
develops into the milder ichthyosis linearis circumflexa.
Allergies to nuts and fish are also common, although not universal,
amongst affected people.
Netherton's syndrome has recently been characterised as a primary
immunodeficiency, which straddles the innate and acquired immune
system, much as does Wiskott-Aldrich syndrome. A group of Nethertons'
patients have been demonstrated to have altered immunoglobulin levels
(typically high IgE and low to normal IgG) and immature natural killer cells.
These Natural Killer cells have a reduced lytic function; which can be
improved with regular infusions of immunoglobulin; although the
mechanism for this is not clear.
Patients are more prone than healthy people to infections of all types,
especially recurrent skin infections with staphylococcus. They may have
more severe infections; but are not as vulnerable to opportunistic
pathogens as patients with true Natural Killer cell deficiency-type SCID.
148
There is no known cure at the moment but there are several things that can
be done to relieve the symptoms. Moisturising products are very helpful to
minimize the scaling/cracking, and anti-infective treatments are useful
when appropriate because the skin is very susceptible to infection. Extra
protein in the diet during childhood is also beneficial, to replace that which
is lost through the previously mentioned "leaky" skin.
Steroid and retinoid products have been proven ineffective against
Netherton syndrome, and may in fact make things worse for the affected
individual.
Massage therapy is medically contraindicated for Netherton's syndrome,
meaning it should not be given unless the client’s treating physician has
approved it.
Ochronosis
Ochronosis is the syndrome caused by the accumulation of homogentisic
acid in connective tissues. The phenomenon was first described by Rudolf
Virchow in 1865. The condition was named after the yellowish (ocher-like)
discoloration of the tissue seen on microscopic examination. However,
macroscopically the affected tissues appear bluish grey because of a light
scattering phenomenon known as the Tyndall effect.
The condition is most often associated with alkaptonuria but can occur from
exogenous administration of phenol complexes like hydroquinone.
The endogenous variety is an autosomal recessive disease, that is caused
by a lack of homogentisic oxidase enyme. Exogenous ochronosis is an
avoidable dermatitis that can be caused by the topical application of
compounds such as hydroquinone or phenols. It was first seen in 1912,
when a patient who used phenol on a leg ulcer was found to have this
condition by Beddard and Plumtre.
Hydroquinone induced exogenous ochronosis was found by Findlay in
1975, who observed the condition in patients who used skin lightening
creams containing the compound.
There are three clinical stages of exogenous ochronosis:
Erythema and mild hyperpigmentation
Hypergimentation and ‘’caviar-like’’ lesions
149
Papulo-nodular lesions
Exogenous ochronosis can be caused from long term usage of certain “skin
lightening products’’, even if the hydroquinone is in amounts as small as
2%. Skin lightening products are still prevalent in many parts of the world.
Reasons for this may be due to aesthetic or social standing reasons, in
areas where a lighter skin tone is considered to be a sign of wealth or
beauty. As well, skin-lightening creams containing compounds such as
hydroquinone are commonly used to help with hyperpigmentation disorders
such as melasma.
Hydroquinone is the compound most frequently used in skin whitening
products. Due to concerns about its side effects, it was almost banned by
the FDA in 2006, as there were medical issues of carcinogenicity and
reports of disfiguring ochronosis. In the European Union Hydroquinone has
been banned in cosmetic creams since 2000.
Long term use of creams containing this compound may lead to exogenous
ochronotic lesions. The duration of the use is directly proportional to the
risk of developing the condition with most cases being after years of use.
Around 10-15 million skin lightening products are sold annually, with Japan
being the major buyer.
Symptoms of Exogenous Ochronosis
Yellow-brown, banana-shaped fibers
Caviar-like papules
Brown-grey or blue-black hyperpigmentation
The majority of the lesions will be seen on areas of the body that get the
most sun.
Hydroquinone-induced exogenous ochronosis is an avoidable dermatosis
that is exceedingly difficult to treat. However, some studies show that
treatment may be possible with a Q-switched alexandrite (755 nm) laser.
It is recommended that individuals with this disorder stop using
hydroquinone containing compounds. It is important to be aware of this as
dermatologists may think the symptoms a patient is exhibiting are a
melasma, and prescribe a hydroquinone containing cream.
150
Ochronosis occurs because of deposition of phenols (such as homogentisic
acid and hydroquinone) as plaques in the matrix of cartilage. The pigments
can also be incorporated into collagen and elastin fibers. In the skin, the
pigment alters the structure of the fibers causing enlargement and curling.
They come to closely resemble fibers seen in biopsies of solar elastosis.
The embedded pigments also form cross-linkages with pigment depositions
in adjacent fibers, stabilizing and reducing the elastic recoil of the fibers.
This results in hardening of elastic structures increasing their rigidity and
brittleness.
Once ruptured, the exposed pigments cause a foreign body reaction and
inflammation. This pigment deposition also invokes deposition of
hydroxyapatite, the mineral responsible for bone calcification, further
hardening the connective tissue. The pigment can also be excreted by
glandular cells in apocrine and ceruminous sweat glands as well as breast
and prostate tissue. This results in darkly pigmented sweat and breast milk.
Excretion of the pigment is only found in endogenous ochronosis and
should not occur from topical phenols.
Skin: The pigment is deposited throughout the skin but only becomes
apparent in certain locations where the concentration is great enough to be
seen clinically. This usually occurs in areas where connective tissue is thick
(joints, tympanic membrane) or close to the surface of the skin (thenar and
hypothenar eminences and the sides of the fingers). In exogenous
ochronosis, the hyperpigmentation is localized to the area where the
inciting agent is applied. Intradermal nevi can appear like blue nevi.
Eye: The most obvious change is darkening around the palpebral fissure.
The cornea can become hyperpigmented if exposed to phenol vapors.
Cartilage: Darkening and hardening of ear cartilage is a prominent feature
of ochronosis. Nasal cartilage is also frequently involved. The voice can be
affected by hardening of the laryngeal cartilage. Stiffening of the ribs with
decreased lung function has also been reported. The intravertebral
cartilage is also more prone to herniation.
Connective tissue: Hardening of tendons and ligaments can predispose
them to rupture. Color changes in the joints can be observed clinically.
Arthropathy is common due to chronic inflammation and microruptures.
151
Heart valves: Stenosis can results from the increased rigidity of the
connective tissue as well as chronic inflammation.
Ochronosis contraindicates massage locally on the skin where there is
bluish tint or hardening and may contraindicate it completely if the tissue of
the heart valves is compromised.
Panniculitis
Panniculitis refers to a group of conditions that involve inflammation of the
fat under the skin. Despite having very diverse causes, most forms of
panniculitis have the same clinical appearance. The diagnosis is
established by a skin biopsy as there are characteristic microscopic
features depending on the cause.
The classification of panniculitis is complicated but, in general, different
types can be divided into mostly septal or mostly lobular panniculitis
depending on where the microscopic inflammation is most concentrated. In
reality, most types of panniculitis have both lobular and septal
inflammation. Further classification is based on whether or not there is
inflammation involving the blood vessels of the fat, i.e. vasculitis.
Panniculitis can also be classified based on the presence or absence of
systemic symptoms. Panniculitis without systemic disease can be a result
of trauma or cold; Panniculitis with systemic disease can be caused:
By connective tissue disorders such as lupus erythematosus or
scleroderma;
By lymphoproliferative disease such as lymphoma or histiocytosis;
By pancreatitis or pancreatic cancer;
By sarcoidosis with cutaneous involvement (seen in up to 20 percent)
and by many other causes.
Alpha 1-antitrypsin deficiency, also, is a major cause of Panniculitis.
An area of skin involved with panniculitis feels thickened and woody to
touch. It may or may not demonstrate discolouration of the overlying skin,
either reddening or darker, brownish pigmentation. The area is often
tender. Most often, the affected areas appear as raised nodules or lumps
under the skin, but may be a plaque or large flat area of thickened skin.
When the inflammation has settled, a depression in the skin may be left
behind temporarily or permanently (localised lipodystrophy).
152
Massage therapy is contraindicated during periods of inflammation.
Psoriasis
Psoriasis is a skin condition than could occur in both men and women of
any age. It usually first appears as thick, silver or red flaky skin patches on
the elbows, knees, or other parts of the body.
The flaking of skin that we see with psoriasis is commonly called “scaling”.
In the beginning only a few small flaky patches might appear. These are
known as “plaques” and they will increase in size and number. In some rare
instances the psoriasis may erupt suddenly all over the client.
Psoriasis is a persistent condition and can come and go many times in a
persons life. It is generally found in people between the years of 20-40 and
is very rare in people under the age of 5. The majority of people that exhibit
symptoms of psoriasis are under the age of 30. In the United States
psoriasis can be found in about two or three out of every hundred people.
Psoriasis most often is found on areas that are under stress, like the
elbows, knees and knuckles. It can also be found on the scalp, torso arms
and legs. In some instances it can be found on external sex organs,
fingernails and toenails.
Psoriatic arthritis is diagnosed based on a physician examination, the
patients medical history, and any relevant family history. Occasionally
lab tests and X-rays are required to determine the severity of the condition
and rule out other diagnosis.
Due to the fact that it affects 1-3% of the population psoriasis is considered
to be a fairly common skin condition. The number of people affected is
approximately 7.5 to 8.5 million people in the United States alone, with
about 125 million people being affected world wide. African Americans are
less likely to be affected, having reported approximately half the cases of
Caucasians.
Your client that is diagnosed with psoriasis has many treatment choices
available to him or her. Their doctor will determine which treatment method
is best for them based on their unique symptoms and presentation of the
153
disease, which means the severity of the flaking and how much of the body
is affected.
For a mild case where less than 10% of the total body skin surface is
effected the doctor would most likely prescribe a topical cream or lotion. A
small injection of steroids may be directly applied to areas that are
particularly tough and scaly.
A moderate to severe case of psoriasis is one that affects 20% or more of
the total skin surface of the body. In these cases topical medications may
not be effective or even practical. If this is the case a systemic “total body
approach” may be applied with pills and/or injections.
For psoriatic arthritis, systemic medications that can stop the progression of
the disease may be required. Topical therapies are not effective.
As with any condition, one must weigh the possible side effects of any
medication or treatment against the actual symptoms themselves to decide
if the treatment is appropriate. Some patients do not feel that the possible
risks of side effects are warranted for a condition that is largely cosmetic,
not painful and not life threatening. In many cases the decision on whether
or not to seek medical condition is decided not so much by the severity of
the condition, but by the location of the condition. People that suffer from
scaling in highly visible places are more likely to seek out medical care than
those who have scaly patches in areas that are easily concealed.
At the present time there is no cure for psoriasis. The disease can go into
remission and show no symptoms for long periods of time, and in some
cases the person may go the rest of their life without seeing a patch of
scaling. Scientists are still conducting research and are making progress in
treatments.
Research studies have not shown it to be contagious from person to
person. You cannot catch it from anyone, and you cannot pass it to anyone
else by skin-to-skin contact. You can directly touch someone with psoriasis
every day and never catch the skin condition.
Massage is medically contraindicated for Psoriasis. If they are receiving
medical treatment and are under the care of a physician massage can be
154
fine for someone with Psoriasis as long as the skin is intact. If the skin is
broken or blistered, or it is in the acute stage, massage should be avoided.
155
A back with Psoriasis
156
Rosacea
Rosacea is a condition/disorder of skin, commonly causing inflammations
and redness, to facial skin. Rosacea has also been called acne rosacea or
adult rosacea. Over 45,000 million people are affected worldwide
especially, white skinned Northwestern Europeans. In United States about
14 million people have rosacea including women and adults between thirty
to sixty age group especially, individuals with blonde hair, lighter skin and
blue eyes. Rosacea is a chronic disease that is often misunderstood for
sunburn and acne. Rosacea is often hereditary and usually women are
afflicted more than men. It is often cyclic, flaring up for weeks/months.
The exact cause of rosacea has not been identified. The reason is believed
to be swelling of blood vessels, environmental factors and hereditary.
Another belief is that it is caused by a mite of name Demodex folliculorum,
living in the hair follicles. The mites cause inflammation by clogging the oil
glands. Fungus and malfunction of some connective tissue found under the
skin are also cited as reasons of rosacea.
Redness appears on forehead, nose, cheeks, chin and sometimes, on
neck, ears, scalp and the chest. Sometimes redness increases to cause a
ruddy appearance or the blood vessels appear visible.
Rosacea is not contra-indicated for massage therapy, however certain
lubricants can irritate the skin of clients with Rosacea and the increase in
blood flow and skin temperature could exacerbate the condition in some
people.
Document any product sensitivity or post-massage acne breakouts for the
future massages.
157
Rosacea in the face.
158
Warts(common)
Warts are small harmless tumors of the skin caused by a virus called the
human papillomavirus. There are at least 63 genetically different types of
HPVs. The virus enters the skin after direct contact with recently shed
viruses kept alive in warm, moist environments such as a locker room, or
by direct contact with an infected person. The entry site is often an area of
recent injury. The incubation time-from when the virus is contracted until a
wart appears-can be 1-8 months. Contrary to popular belief, touching a frog
will not give you warts. Warts are common in children. Most cases occur
between ages 12-16 years. Up to 30% of warts disappear by themselves
within 6 months. Most will disappear without any treatment within 3 years.
The appearance of warts can differ based on the type of wart and where it
is located on the body. Most warts are well defined bumps, with skin
thickening.
The 3 most common types of nongenital (not appearing on the genitals)
warts are these:
•Common warts (verrucae vulgaris): These common warts typically develop
on the hand, especially around the nail. Common warts are gray to flesh
colored, raised from the skin surface, and covered with rough, hornlike
projections.
•Plantar warts (verrucae plantaris): Plantar warts, by definition, occur on
the plantar surface, or bottom, of the foot. They usually occur in highpressure areas such as the heel and the metatarsal heads (just behind the
toes).Plantar wartsusually grow into the skin, not outward like common
warts. This growing into the skin makesplantar wartsmore difficult to treat.
•Flat warts (verrucae plana): Flat warts are most commonly seen on the
face and the back of the hands. They usually appear as small individual
bumps about 1/4 inch across. Flat warts may spread rapidly on the face
from the activities involved in shaving.
159
A common Wart.
Shingles
Shingles (herpes zoster) is a painful, blistering skin rash. It is caused by the
varicella-zoster virus. This is the virus that also causes chickenpox, and as
you know, that virus is very contagious.
Almost 1 out of every 3 people in the United States will develop shingles.
There are an estimated 1 million cases each year in this country. Anyone
who has ever had chickenpox may develop shingles; including young
children. After a person recovers from chickenpox, the virus stays in the
body in a dormant (inactive) state. For reasons that are not fully known, the
virus can reactivate years later, causing shingles. Herpes zoster is not
caused by the same virus that causes genital herpes, a sexually
transmitted disease.
The risk of getting shingles increases with age, about half of all cases occur
among men and women 60 years old or older.
People who have medical conditions that keep their immune systems from
working properly, such as certain cancers, including leukemia and
160
lymphoma, and human immunodeficiency virus (HIV), and people who
receive immunosuppressive drugs, such as steroids and drugs given after
organ transplantation are also at greater risk of getting shingles.
People who develop shingles typically have only one episode in their
lifetime. In rare cases, however, a person can have a second or even a
third episode.
Signs & Symptoms
Rash on back of the body. Shingles usually starts as a painful rash on one
side of the face or body. The rash forms blisters that typically scab over in
7–10 days and clears up within 2–4 weeks.
Before the rash develops, there is often pain, itching, or tingling in the area
where the rash will develop. This may happen anywhere from 1 to 5 days
before the rash appears on the body.
Most commonly, the rash occurs in a single stripe around either the left or
the right side of the body. In other cases, the rash occurs on one side of the
face. In rare cases (usually among people with weakened immune
systems), the rash may be more widespread and look similar to a
chickenpox rash. Shingles can affect the eye and cause loss of vision.
Transmission
Shingles cannot be passed from one person to another. However, the virus
that causes shingles, the varicella zoster virus, can be spread from a
person with active shingles to a person who has never had chickenpox.
In these cases, the person exposed to the virus might develop chickenpox,
but they would not develop shingles. The virus is spread through direct
contact with fluid from the rash blisters, not through sneezing, coughing or
casual contact.
A person with shingles can spread the virus when the rash is in the blisterphase. A person is not infectious before blisters appear. Once the rash has
developed crusts, the person is no longer contagious.
Shingles is less contagious than chickenpox and the risk of a person with
shingles spreading the virus is low if the rash is covered.
161
For Massage Therapists
The rashes of shingles are painful, so it is very unlikely that someone with
an active outbreak would come in for a massage. However if they did, there
is a chance a massage therapist could contract the varicella-zoster virus if
they come into direct contact with the virus.
If you do accidentally come into contact with an infected area you should
immediately wash your hands in accordance with the standards published
by the Center for Disease Control.
A person that has had Shingles in the past but has recovered is perfectly
safe for massage therapy. The only time massage therapy is
contraindicated for this condition is when the rash is active.
Summary of Pathology of the Integumentary System
Massage therapists are in a unique position to spot potentially dangerous
skin conditions on our clients in areas they might not be able to see, like
the top of the scalp, between the toes, or on the back.
It is not our job to diagnose our clients or to frighten them when we notice
skin abnormalities. We do have an ethical responsibility to give good advice
to our clients about consulting a dermatologist when they have suspicious
or undiagnosed changes in the skin.
162
Certificate of Completion and Transcript
In order to receive your certificate of completion and an updated transcript
for this course you must complete and pass the quiz.
Once we have received your quiz we will generate your certificate and
transcript and both will be emailed to you. If you completed the last quiz
during our business hours (Monday-Friday 8:00 am-5:00 pm Pacific
Standard Time) it should be emailed to you within a few minutes.
If you complete the last quiz after business hours, or on a weekened it will
still be emailed to you as quickly as possible. We check the system every
hour until midnight most days so it should go out within an hour of you
taking it.
If you take the last quiz after midnight you will probably have to wait until
the next morning, we do sleep.
Please give us a full 24 hours before you call us if you have not received
your certificate and transcript. We pride ourselves on being very fast, but if
there is a condition beyond our control (the Internet Service Provider is
down, etc) it may take us longer than usual.
Also please be aware that many people wait until the last minute to do their
courses. For this reason, the last few days of the month (28th, 29th, 30th,
etc) are usually very, very busy times for us so our turn around time may be
a little slower-but it should still be within 24 hours.
If it has been more than 24 hours and you still have not received your
emailed certificate, by all means call us! The number is (209) 777-6305.
Lost Certificates and Transcripts
If you need another copy of your documents emailed to you we will gladly
do that for free at any time, just go to the contact page on our website and
ask for it.
163
Course Evaluation
We would like to hear some feedback form you. You can complete the
evaluation online by clicking this link:
http://www.sasionline.com/courseevaluation.html
If you are using the “embedded” version of this course you will not be able
to click the link above but there should be one you can access on the
webpage itself.
Thanks for taking our course; we really appreciate your business and we
hope you come back to us next time you need continuing education hours.
We would also love it if you would “Like us” on facebook, you can find us at
www.facebook.com/beyondmassageschool.
Errata
If you found a typo PLEASE LET US KNOW what page it is on and the
paragraph and we will fix it ASAP. This book has 50,000 words in the
course content alone. Some of those are going to be misspelled. We’re not
perfect, but we strive to be- so help us out.
Help and Technical Support
We have worked hard to make this course as easy to use as possible, but it
does rely on technology and sometimes there are factors that are out of our
control (like your local internet provider, your computer, your browser
version, the device you are using etc).
If for some reason you are not able to access the quiz you can call us and
let us know, and we will problem solve it for you. We have office hours,
Monday-Friday 8:00 am-5:00 pm PST but you can call or email for help at
any time after hours, I monitor the system every hour until I go to sleep, so
call if you need to and I will do my best to help you. The number is (209)
777-6305.
164
Bibliography
Beck, Mark F Theory and Practice of Therapeutic Massage.
Milady 4 edition (2007)
Werner, Ruth A Massage Therapist's Guide to Pathology
Lippincott Williams & Wilkins; 4 edition (2008)
Virendra N Govind Srivastava M.D. Sehgal Diagnosis and Treatment of
Common Skin Diseases Anshan Pub; 2 edition June 30, 2005
de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H (Jun
2004). "Classification of papillomaviruses". Virology 324
Brownell I, Pomeranz M, Ma L (2005). "Eumycetoma"
Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine.
(6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
Habif, Thomas P. (2009). Clinical dermatology (5th ed. ed.). Edinburgh:
Mosby. ISBN 978-0-7234-3541-9.
Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine.
(6th ed.). Page 685. McGraw-Hill. ISBN 0-07-138076-0.
Acne
Conglobata
overview
http://emedicine.medscape.com/article/1072716-
Acne
Conglobata
Treatment
&
http://emedicine.medscape.com/article/1072716-treatment
Management
Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007).
Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
Testosterone and anabolic steroids and acne fulminans. Arch Dermatol.
1989; 125(4):571-2 (ISSN: 0003-987X)
Case reports: acne fulminans in Marfan syndrome. J Drugs Dermatol.
2005; 4(4):501-5 (ISSN: 1545-9616)
165
Acne conglobata and arthritis. Arthritis Rheum.
0004-3591)
1961; 4:632-5 (ISSN:
Acne fulminans with synovitis-acne-pustulosis-hyperostosis-osteitis
(SAPHO) syndrome treated with infliximab. J Am Acad Dermatol. 2005;
52(5 Suppl 1):S118-20 (ISSN: 1097-6787)
Khumalo NP, Jessop S, Gumedze F, Ehrlich R. Hairdressing and the
prevalence of scalp disease in African adults. Br J Dermatol. Nov
2007;157(5):981-8.
Grunwald MH, Ben-Dor D, Livni E, Halevy S. Acne keloidalis-like lesions on
the scalp associated with antiepileptic drugs. Int J Dermatol. Oct
1990;29(8):559-61
Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine.
(6th ed.). Page 685. McGraw-Hill. ISBN 0-07-138076-0.
Wolff, Klaus Dieter; et al. (2008). Fitzpatrick's Dermatology in General
Medicine. McGraw-Hill Medical. ISBN 0-07-146690-8.
James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of
the Skin: Clinical Dermatology. (10th ed.). Saunders. Page 245. ISBN 07216-2921-0.
Alikhan, Ali; Lynch, Eisen (2009). "Hidradenitis suppurativa:
comprehensive review". J Am Acad Derm 60 (4): 539–561.
a
Kumar, Vinay; Fausto, Nelso; Abbas, Abul (2004) Robbins & Cotran
Pathologic Basis of Disease (7th ed.). Saunders. Page 1230. ISBN 0-72160187-1.
Michalczyk, A; Varigos, G; Catto-Smith, A; Blomeley, Rc; Ackland, Ml
(August 2003). "Analysis of zinc transporter, hZnT4 ( Slc30A4), gene
expression in a mammary gland disorder leading to reduced zinc secretion
into milk". Human Genetics 113 (3): 202–10. doi:10.1007/s00439-0030952-2. PMID 12743795.
James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of
the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
166
Andrews' Diseases of the Skin: Clinical Dermatology - Expert Consult Online and Print, 11e (James, Andrew's Disease of the Skin) William D.
James MD (Author), Timothy Berger MD (Author), Dirk Elston MD (Author)
Oculocutaneous albinism. Okulicz JF1, Shah RS, Schwartz RA, Janniger
CK.J Eur Acad Dermatol Venereol. 2003 May;17(3):251-6.
Phornphutkul C, Introne WJ, Perry MB, et al. (2002). "Natural history of
alkaptonuria". New England Journal Medicine 347 (26): 2111–21.
doi:10.1056/NEJMoa021736. PMID 12501223.
Doctoroff A, Oberlender AS, Purcell SM. Full face carbon dioxide
resurfacing in the management of a patient with the nevoid basal cell
carcinoma syndrome. Dermatol Surg, 2003;29(12):1236-1240
Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial
pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 141, 142, 163, 689,
713. ISBN 0721690033.
Saulsbury FT (2001). "Henoch-Schönlein purpura". Current Opinion in
Rheumatology 13 (1): 35–40. doi:10.1097/00002281-200101000-00006.
PMID 11148713.
167