* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Efficacy of Lidocaine Iontophoresis Using Either Alternating or Direct
Pharmaceutical industry wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacognosy wikipedia , lookup
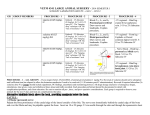
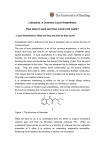
J Med Dent Sci 2013; 60: 63-71 Original Article Efficacy of Lidocaine Iontophoresis Using Either Alternating or Direct Current in Hairless Rats Atsushi Nakajima, Ryo Wakita, Haruka Haida and Haruhisa Fukayama Section of Anesthesiology and Clinical Physiology, Department of Oral Restitution, Division of Oral Health Sciences, Graduate School, Tokyo Medical and Dental University The aim of this study was to determine transport of lidocaine ions through a hairless rat skin in vivo and to compare the efficacy of alternating current (AC) with that of direct current (DC) iontophoresis (IOP). We measured the concentration of lidocaine transported through a cellophane membrane or a hairless rat dorsal skin applying either AC-IOP or DC-IOP. The results revealed that lidocaine concentration increased in a time-dependent manner in vitro in both DC-IOP and AC-IOP. However, the in vivo study showed different tendencies in lidocaine concentration. In the DCIOP group, lidocaine concentration reached its maximum 20 min after current application and then decreased rapidly; the AC-IOP group showed an increase in lidocaine concentration in a timedependent manner. There were no side effects such as electrical burns in the rats. In conclusion, AC can be applied for long periods and DC for short periods, or their application time can be appropriately scheduled. Our study also suggests the mechanism by which voltage waveforms affect the skin when applied by IOP. In the future, these findings will be a solid foundation for developing various kinds of medical equipment such as scheduled drug delivery system that can easily deliver various types of drug. Corresponding Author: Atsushi Nakajima Section of Anesthesiology and Clinical Physiology, Department of Oral Restitution, Division of Oral Health Sciences, Graduate School, Tokyo Medical and Dental University 1-5-45 Yushima Bunkyo-ku, Tokyo 113-8549, Japan Tel: +81-3-5803-5549 Fax: +81-3-5803-0206 E-mail: [email protected] Received February 19;Accepted June 14, 2013 Key words: Iontophoresis, Alternating current, Lidocaine, Hairless rat, Microdialysis 1. Introduction Iontophoresis (IOP) is one of the transdermal drug delivery methods that utilize current to enhance the movement of an ionic or a noncharged drug and facilitate the penetration of the drug across the skin via three principal mechanisms: electrorepulsion, electroosmosis, 1, 2 and electroporation . Local anesthetics, opioids, steroids, nonsteroidal anti-inflammatory drugs (NSAIDS), and antiviral agents among others have been used in transdermal drug delivery studies 3, 4. Generally, direct current (DC) IOP has often been selected because of its higher transport efficiency. The IOP of anesthetics such as lidocaine is used in clinical settings 5-9. However, DC-IOP could cause some side effects such as electrical burns, chemical burns, and erythema due to electrolysis and attenuates the transport effect owing to electrode polarization10, 11. This side effects limit the DC iontophoresis duration to less than 15 min at current density as low as 1 mA/cm2 12. Many studies report and suggest current density of experimental p r o t o c o l w a s a p p l i e d u p t o 0 . 5 m A / c m2 f o r D C iontophoresis 3, 13. Recent study shows electrochemical burns and skin irritation were avoided by alternating current iontophoresis (AC-IOP)11, 14 . The periodic polarity changes of AC-IOP can neutralize pH changes. Our study group has examined the efficiency of AC-IOP in transporting lidocaine into the skin effectively. We demonstrated, using by in vitro studies, that lidocaine ions can be successfully transported through a cellophane membrane by applying AC and that the efficacy of lidocaine iontophoresis using a bipolar square wave depends on the duty cycle and correlates 64 A. Nakajima et al. J Med Dent Sci with average voltage10, 15-21. The average voltage U ave can be expressed as U ave = 1 T T ʃ U (t )dt (1) 0 where t is the time, U(t) is the voltage between the electrodes at t, and T is the period of the square wave. However, there have been fewer studies in which the efficacy of AC-IOP is compared with that of DCIOP, which is widely used. Yan et al. reported the good correlations between phenylalanine and mannitol transport across human epidermal membrane during DC and AC-plus-DC iontophoresis 22. Li et al. showed skin resistance can be maintained at a constant level during AC iontophoresis 23. Some studies showed that the concentrations of drugs transported from the skin to the target can be measured using a microdialysis system. The use of microdialysis system that directly measures tissue drug concentration is more appropriate for local anesthetic studies than indirect estimations of tissue drug concentrations from plasma drug concentrations. The system is promising and less invasive for assessing cutaneous drug delivery. Other studies showed the increased percutaneous absorption of lidocaine and prilocaine in pigs and also the percutaneous penetration of flurbiprofen into the rat skin by DC-IOP 24, 25. The aim of this study was to compare the efficacy of waveforms that were set at the same average voltage in vitro and determine the concentration of lidocaine ions transported through a hairless rat skin in vivo applying AC-IOP and DC-IOP. 2. Materials and methods 2.1 In vitro protocol 2.1.1 Materials Lidocaine hydrochloride (C14H22N2O·HCl; FW 270.8; H2O content 1 mol/mol) was purchased from SigmaAldrich Co. Ltd. (St. Louis, MO, USA). One percent lidocaine hydrochloride was prepared using distilled and deionized water (resistivity > 18 MΩ). The pH of 1 % lidocaine was 4.6. The cellophane membrane (Futamura Chemical Co. Ltd., Nagoya, Japan) used was about 36 μm thick with a pore size range of 2 - 3 nm. This pore size range is about twice larger than the lidocaine molecule. 2.1.2 Procedure of in vitro experiments (Fig.1, Fig.2) To evaluate the transport of lidocaine ions through Fig. 1 The setup of in vitro experimental system. Fig. 2 Experimantal protocol. the cellophane membrane, a cylindrical acryl drug delivery cell consisting of two chambers was originally constructed. An experimental system and methods, prepared as previously described, were basically used in all the in vitro experiments19. Platinum plate electrodes with a diameter of 20 mm and a thickness of 0.2 mm were installed at the opposite ends of two components of the cell. The length of each component was 10 mm. The cellophane membrane was placed between the two components. The available diffusion area was about 3.1 cm2. The donor and receptor chambers were filled with 1 % lidocaine hydrochloride solution (3.0 ml, pH 4.6) and distilled water (3.0 ml), respectively. Acryl cells were set in a water bath (36.0 ℃). A thermocouple microprobe (BAT, Physitemp, NJ, USA) was inserted at the center of the donor chamber to monitor the temperature of the solution in Efficacy of Lidocaine IOP in Hairless Rats Fig. 3 Experimental Waveforms. (a) Square wave with 70 % duty cycle at 1 kHz (b) Direct current The duty cycle is the ratio of the positive cycle to the full cycle. EAC and EDC represent applied voltage. In vitro experiment, EAC was 7.5 V and EDC was 3 V. In vivo experiment, EAC was 10 V and EDC was 4 V. Both (a) and (b) were set at the same average voltage. the chamber. The solution in the two cell chambers was not stirred because the bulk flow caused by stirring and the rotator-induced magnetic field could affect lidocaine transport. The tube was inserted into the receptor chamber and connected to a peristaltic pump (ALITEA XV, Sweden). Samples were extracted from the receptor chamber every 30 min. After collecting the first sample, voltage was applied as described below. A square wave (duty cycle 70 %; 7.5 V; 1kHz) and DC (3 V) which were set at the same average voltage (Fig. 3), were continuously applied between the parallel platinum electrodes for 270 min using a function/ arbitrary waveform generator (Agilent Technologies, Colorado, USA) and a high-speed power amplifier (4025, NF Electric Instruments, Kanagawa, Japan), while the waveform and voltage were monitored using a digitizing oscilloscope (HP54503A, Hewlett Packard, Tokyo, Japan) throughout the experiment. 2.1.3 Measurement system 19 Measurement system referred to Hayashiʼs protocol . The concentration of lidocaine in the receptor chamber was measured using a spectrophotometer (U-3310; absorbance range, -2 - 4 Abs; precision, 0.002 Abs; HITACHI, Tokyo, Japan) at room temperature. The samples were diluted 25 times with distilled and deionized water. The absorbance of the samples was measured at a wavelength of 262 nm and an optical path of 10 mm. Lidocaine concentration was determined using a calibration curve 16. 2.2 In vivo protocol 2.2.1 Materials Two percent lidocaine hydrochloride was purchased from AstraZeneca (Osaka, Japan). Three percent 65 mepivacaine hydrochloride (C15H22N2O·HCl; FW 282.8) was purchased from Nippon Shika Yakuhin Co. Ltd. (Shimonoseki, Japan). An iontophoretic patch originally developed by TTI ellebeau Ltd, (Tokyo, Japan) was used in this study. The patch was composed of a silver/silver chloride electrode, a circular anode, and a circular cathode with a nonwoven fabric reservoir (diameter, 1.7 cm) with a capacity of 0.4 mL of a drug solution. 2.2.2 Microdialysis system A linear microdialysis probe (MDP) with a cellulose membrane length of 10 mm (o.d. 0.22 mm; i.d. 0.105 mm) and a molecular weight cutoff of 50 kDa (Eicom OP-100-10, Kyoto, Japan) was prepared. The inlet tube of the probe was connected to a gas-tight syringe (1 ml) on a microinjection pump (CMA/100). The outlet tube of the probe was connected to a microfraction collector (CMA/140) with a Teflon tube. 2.2.3 Experimental procedure in vivo (Fig. 2, Fig. 4) Hairless rats (8-week-old males, 250-300 g) were housed in an air-conditioned room and used for this study. The institutional Review Board of Tokyo Medical and Dental University approved the animal experimental protocol. The experiment was conducted in accordance with the guidelines of this review board. The rats were anesthetized by the intraperitoneal injection of sodium pentobarbital (40 mg/kg). The surface of the dorsal skin was swabbed with alcohol and dried before surgery. A linear microdialysis probe was inserted into the subcutaneous tissue, unilateral to the skin at the dorsum using a guide needle. The guide needle was withdrawn leaving the probe. Acetate Ringer solution was perfused at a flow rate of 2 μl / min with 0.0015 % mepivacaine added as a recovery calibrator (internal standard). There was an equilibration period of 60 min to relieve minor trauma caused by the probe insertion. Seven samples were collected from the subcutaneous tissue every 20 min. After collecting the first sample, the iontophoretic device having two electrodes containing 2 % lidocaine solution (0.4 ml) and saline (0.4 ml) was applied to the dorsal region. A square wave (duty cycle 70 %; 10 V; 1 kHz) and DC (4 V), which were set at the same average voltage (Fig. 3), were produced by a function generator. Either the square wave (AC-IOP group) or DC (DC-IOP group) was applied to the rats for 120 min. The device without IOP was applied to the rats as the passive absorption group (passive group) for 120 min. The concentration of lidocaine was determined 66 A. Nakajima et al. J Med Dent Sci Fig. 4 The setup of the experimental system. by a high performance liquid chromatography (HPLC) and compared among the three groups. After this experiment, the dorsal skin was excised to measure probe depth and examine skin damage. Probe depth was assessed by H-E staining. Mathy et al. showed the way in detail 25. 2.2.4 In vitro recovery In vitro recovery was determined to ensure that the probe would provide reproducible and efficient sampling of lidocaine. The probe was placed in a 1-L beaker that contained saline and connected to the microdialysis system. The perfusate was 0.01 % lidocaine or 0.003 % mepivacaine. Six samples were collected every 20 min after the start of perfusion. Eight microdialysis probes that were used in this study were examined whether these membranes were intact. Lidocaine and mepivacaine concentration were determined by HPLC. 2.2.5 HPLC of in vivo and in vitro samples The HPLC system used in this study was composed of a UV-VIS detector (SPD-10A), a column oven (CTO10A), a system controller (SCL-10A), an auto injector (SIL-10AD), a liquid chromatograph (LC-10AD), a degasser (DGU-14A), and a column. The mobile phase consisted of 100 mM phosphate buffer (pH 6.9) and acetonitrile at a volume ratio of 45/55. The flow rate was 0.8 ml/min. Twenty-microliter samples were automatically injected into the HPLC system for analysis. The column oven was maintained at 40 ℃. Lidocaine was detected at 220 nm by UV detection. Standard lidocaine solutions of 0.00002 % - 0.001 % diluted with pure water were used to obtain standard curves, which were linear in this range (r 2 = 0.986). Values obtained from HPLC analysis applied to standard curve and lidocaine concentration were calculated. Using the recovery rate of lidocaine, lidocaine concentration of the subcutaneous tissue was identified. Mepivacaine was used to confirm stable recovery. 2.3 Statistical analyses All values are presented as the mean ± S.D. Twoway ANOVA was carried out to determine the time and waveform dependences of the transport efficiency of lidocaine. One-way ANOVA was used to analyze the time dependence of the recovery rate of microdialysis probes. In addition, for comparison of lidocaine concentration and cell temperature, the Dunnet test was carried out for intragroup comparisons and the Tukey test for intergroup comparisons. Differences were considered significant at p < 0.05. All statistical analyses were performed using Kyplot 5.0 (KyensLab Inc., Tokyo, Japan). Efficacy of Lidocaine IOP in Hairless Rats 3. Results 3.1 Probe depth and skin damage Table 1 shows the probe depth in each group. The mean probe depth was 1.67 ± 0.31 mm (± S.D., n = 15). No significant differences in probe depth were found among the three groups and there were no side effects such as an erythema or electrical burns in the three groups. Table 1 Probe depth in in vivo experiment. No significant differences in probe depth were found among the three groups. 67 where Cperfusate is the drug concentration in the perfusate and Cdialysate is the drug concentration in the dialysate. The samples collected from this experiment showed that the recovery rate in vitro was 24.12 ± 4.08 % for lidocaine and 24.28 ± 3.14 % for mepivacaine. A little variation of recovery rate was observed among the probes. However, no significant differences in recovery rate were found in each probe. Fig. 5 shows recovery rate of lidocaine maintained almost constant level throughout the experiment. Recovery rates of lidocaine and mepivacaine were almost the same value. (2) 3.3 In vitro experiment Figure 6 shows the changes in lidocaine concentration in the receptor chamber to which the square wave, DC, and passive diffusion were applied. The lidocaine concentration in the receptor chamber increased in a time-dependent manner in all the three groups. The lidocaine concentrations in the current applied groups (both AC-IOP and DC-IOP) were significantly elevated after 30 min compared with that in the passive group (p < 0.05). There were no significant differences between the AC-IOP group and the DC-IOP group at both time points. The temperature of the donor chamber increased in both the AC-IOP and DC-IOP groups (Fig. 7). It became constant after 120 min (AC-IOP group, 37.3 ℃; DC-IOP group, 36.0 ℃). The difference in temperature between the two groups was statistically significant after 30 min (p < 0.05). The DC-IOP group showed a significantly higher temperature than the passive group (p < 0.05). Fig. 5 Recovery rate of lidocaine determined by retrodialysis for subcutaneous probe. Values are means ± S.D. (n = 8). Recovery rates of lidocaine were almost the same value and maintained almost constant level throughout the experiment. Fig. 6 Changes in lidocaine concentration in vitro . (○) AC-IOP group (n = 5), (△) DC-IOP group (n = 5), (□) passive group (n = 5). The values are plotted in the middle of each sampling time. The error bars represent the standard deviation of the mean. *p < 0.05 vs passive group. Experimental number AC-IOP group DC-IOP group Passive group 1 1.75 mm 2.14 mm 1.92 mm 2 1.50 mm 1.07 mm 1.73 mm 3 2.25 mm 1.42 mm 1.54 mm 4 1.76 mm 1.60 mm 1.35 mm 5 1.47 mm 1.61 mm 1.35 mm 1.74 ± 0.31 mm 1.57 ± 0.38 mm 1.69 ± 0.25 mm Mean ± SD total 1.67 ± 0.31 mm (n = 15) 3.2 Recovery rate in vitro determined by retrodialysis Disappearance rate was calculated using Eq. (2) and taken as the recovery rate in vitro . Recovery rate = 100 (Cperfusate ‒ Cdialysate) / Cperfusate 68 A. Nakajima et al. J Med Dent Sci between the AC-IOP group and the other two groups after 60 min and thereafter (p < 0.05). At 120 min, the lidocaine concentration in the AC-IOP group increased through intradermal absorption, which was approximately 6.5 times and 13 times those of the DCIOP and passive groups, respectively. 4. Discussion Fig. 7 Temperature of donor chamber. (○) AC-IOP group (n = 5), (△) DC-IOP group (n = 5), (□) passive group (n = 5). The error bars represent the standard deviation of the mean. *p < 0.05 vs DC-IOP group. †p< 0.05 vs passive group 3.4 In vivo experiments (Fig. 8) In the AC-IOP group, lidocaine concentration significantly increased time-dependently. In contrast, the DC-IOP group showed unique characteristics and the highest lidocaine concentration was detected at 20 min. The lidocaine concentration in the DC-IOP group was about 30 times and 168 times those in the AC-IOP and passive groups, respectively. After 40 min, both the DC-IOP and passive groups showed low lidocaine concentrations. There were significant differences Fig. 8 Changes in lidocaine concentration in vivo . (○) AC-IOP group (n = 5), (△) DC-IOP group (n = 5), (□) passive group (n = 5). The error bars represent the standard deviation of the mean. *p < 0.05 vs the passive group. †p< 0.05 vs the AC-IOP group. 4.1 Skin damage after iontophoresis application In this study, there were no signs of skin damage such as erythema or burns in the AC-IOP or DC-IOP group, to which electrical current was applied. Generally, DCIOP has side effects described above because of the hydrogen and hydroxide ions generated by DC. However, low current density less than 0.5mA/cm2 does not cause these side effects13. This study did not measure the current flow of the skin and the current density at direct 4 V might not reach the concerned level. Moreover, pH changes did not occur in vivo study possibly because the silver/silver chloride electrodes prevented pH variation. Owing to the polarization of the skin or electrodes surface and formation of insoluble silver chloride, the effective current flow was limited. Additionally, the skin was observed 120 min after applying the DC, which was much later than 20 min. Thus, no side effects could be observed in the skin. Although AC-IOP also generates insoluble product, the periodic polarity alternation neutralizes it. This fact was capable of long-term current application. This finding indicates that AC-IOP is useful for clinical application as well as DC-IOP. In the in vitro experiments, the temperature of the donor cell increased in the AC-IOP group. The increase of the vibration energy of the ion given by alternating electric potential applied between electrodes causes the decrease of effective Stokes radius of the ion and plays a decisive role in the ion transport 15. However, this vibration energy leads to increasing kinetic energy and resulting in temperature increase of donor chamber. In our in vivo study, we didnʼt measure temperature of the system. The vibration energy may cause kinetic energy of ionized subcutaneous molecules in a timedependent manner, resulting in elevation of skin temperature. There is a possibility that this increase causes the skin burns. Therefore, it is necessary to determine the optimal voltage that does not cause human skin burns. Efficacy of Lidocaine IOP in Hairless Rats 4.2 Recovery rate determined by retrodialysis and compensation In this study, the recovery rate of lidocaine was measured by retrodialysis. It is assumed that the rate of disappearance of compounds from the probe through the semipermeable membrane is equal to the rate of recovery from the extracellular medium; this assumption was successfully employed in many studies 26. However, the in vitro and in vivo recovery rates of compounds usually differ. Generally, the recovery rate in vivo is often lower than that in vitro because the diffusion in the tissue is hardly detected compared with that in a simple solution 27. Thus, in vitro recovery rate cannot be used for in vivo calculations owing to differences in transport characteristics between tissues and solutions. To estimate lidocaine concentration, mepivacaine was added to the perfusion as an internal standard, because the molecular weight of mepivacaine is almost the same as that of lidocaine. By measuring the concentration of mepivacaine in the samples collected in in vivo experiments, we were able to estimate the concentration of lidocaine in the subcutaneous tissue. Small variations in the concentration of mepivacaine in each sample indicated that the microdialysis probe could recover the lidocaine nearly constantly and membranes of probes were in good condition. Consequently, this analytical procedure enables the precise estimation of the concentration of lidocaine at an area applied with current. 4.3 In vitro lidocaine transport efficiency Hayashi et al. suggested that lidocaine transport was enhanced in a voltage- and duty-cycle-dependent manners and was related to average voltage19. AC or DC with the same average voltage was used in this in vitro study. Figure 6 shows that the transport of lidocaine ions using both waveforms showed similar tendencies and was more efficient than the transport by passive absorption. Therefore, this result suggests that voltage application adds energy to lidocaine ions and increases transport efficiency, suggesting that average voltage is related to lidocaine transport efficiency. In vitro experiment, pH may change using platinum electrodes. The pH of the solution in the donor chamber tended to decrease after applying the currency19 . The pH of 1 % lidocaine hydrochloride solution is 4.6 and pKa of lidocaine is 7.86. Therefore, the lidocaine molecules were almost completely dissociated and ionized throughout experiments in the donor chamber and pH changes in vitro study were thought to be less influence on the result. AC-IOP does not facilitate pH 69 changes due to alternating polarities. However, the increase in temperature in the donor chamber could also add energy for the transport of lidocaine ions across the cellophane membrane. A higher temperature may enhance lidocaine transport in the AC-IOP group compared with the DC-IOP group. 4.4 In vivo lidocaine transport efficiency Results of in vitro experiments showed the relevance of average voltage to transport efficiency. Therefore, in vivo experiments were performed using waveforms that were at the same average voltage in DC and AC settings to determine whether both waveforms have the same lidocaine transport efficiency. As shown in the results, lidocaine was successfully transported through the dorsal skin of a living hairless rat receiving both AC and DC-IOP. In the DC-IOP group, the lidocaine concentration reached its maximum 20 min after the application of current and decreased rapidly thereafter. Large variability of the lidocaine concentration was also shown at this point. This indicated that the maximum concentration in the tissue could be detected between 0 and 40 min and there were differences in the amount of transporting agent at each experiment. Some studies showed that DC-IOP caused undesirable effects on the skin and was considered to enhance irritations or subcutaneous vasodilatation due to current flow 28-30. An increased vascular blood flow c aus e d b y v a s o dila t a t ion pr om o t e s ele c t r ol y t e accumulation in the intracellular space, which leads to the decrease in electrical resistance, resulting in a greater flow of electrical current. After this phenomenon, electropolarization, which is a disadvantage of DC IOP, reduces current flow and increases blood flow owing to vasodilatation. Finally, lidocaine ions flow out of the area of application. Since Wakita et al. reported that the application of lidocaine with epinephrine as a vasoconstrictor has a greater anesthetic effect than that of lidocaine only when applying DC iontophoresis, vasodilatation has been considered one of the factors that decrease anesthetic efficiency 20. On the other hand, it was observed that the AC-IOP group showed an increase in lidocaine concentration in a time-dependent manner. The mechanism underlying this increase is considered to be that AC changes the polarity of electrodes periodically without generating electropolarization and that the anesthetic could pass through the rat skin. Comparing DC-IOP, AC-IOP could have constant transport efficiency because of low variability. Li et al. also reported constant skin 70 A. Nakajima et al. resistance AC iontophoresis generally provide less inter- and intra-subject variability than conventional constant current DC 23 . This feature could make it possible to infiltrate any agent into the skin at targeted concentration. However, the lidocaine concentration in the AC-IOP group increased to a lesser extent than that in the DC-IOP group. It cannot be denied that lidocaine ions were possibly drawn “back and forth” to the electrode because of the periodic negative phase of AC. Usually, the skin is negatively charged, which enables the transport of positive ions efficiently. However, when negative voltage is applied, this may promote the extraction of positive ions that penetrated into the subcutaneous tissue. Some studies showed that pulsed DC without negative components could yield a low resistance, enhance drug delivery, and reduce the risk of burns 31, 32. More studies are required to determine other waveforms that may be effective. T h e in vivo stu d y sh o we d th a t th e tra ns por t efficiencies were significantly different between the AC-IOP group and the DC-IOP group even when using the same average voltage. Hayashi et al. suggested transport efficiency is dependent on the average voltage19. On the other hand, our experimental model showed different tendency of transport. This discrepancy can be derived from these settings; in vitro or in vivo . Although transported lidocaine ions accumulated in the receptor cell owing to the closed system in the in vitro study, the lidocaine ions in the in vivo study accumulated to a lesser extent owing to the open system used in this study. This discrepancy suggests that transport efficiency could depend on the way current flow is applied and further study will be needed to identify whether the average voltage relates to transport efficiency. Yan et al. reported that the frequency of AC is related to the control of drug permeation, and Xu et al. showed that a frequency lower than 1 kHz is more effective14, 33. More studies are needed to determine the optimal frequency of AC. DC-IOP has higher transport efficiency than ACIOP but it is unsuitable for long-term application. In contrast, AC-IOP is inferior to DC in terms of rapid drug permeation, but it is suitable for long-term application. These findings indicate the possible clinical primary and secondary applications of DC and AC respectively, that is, DC is applied to rapidly increase lidocaine concentration, followed by AC to maintain the concentration. If the application time relates the dose of transdermal absorption and long-term AC-IOP maintains J Med Dent Sci the local concentration of the target area, it will enable each patient to administer appropriate drug dose and prevent them from overdosing. For example, this could be very useful device especially for elderly persons who might have hepatic or renal dysfunction. Further studies are also required for the applications of both DC-IOP and AC-IOP. 5. Conclusions Our experimental system was successfully applied to the evaluation of the effects of both AC-IOP and DC-IOP on lidocaine transport across a living hairless rat skin. Following the application of DC-IOP, the concentration of lidocaine in the subcutaneous tissue immediately increased and then decreased rapidly. On the other hand, AC-IOP gradually increased the concentration in a time-dependent manner. The results of our study indicated that AC-IOP and DC-IOP have different effect on transporting lidocaine ions in vivo . Consequently, this study suggests that both AC and DC-IOP protocol should be adjusted to increase and maintain the drug concentration at target tissue according to clinical situations. 1. 2. 3. 4. 5. 6. 7. 8. References Guy RH, Kalia YN, Delgado-Charro MB, Merino V, López A, Marro D. Iontophoresis: electrorepulsion and electroosmosis. J Control Release. 2000; 64(1-3): 129-32. Singh P, Maibach HI. Iontophoresis in drug delivery: basic principles and applications. Crit Rev Ther Drug Carrier Syst. 1994; 11(2-3): 161-213. Kalia YN, Naik A, Garrison J, Guy RH. Iontophoretic drug delivery. Adv Drug Deliv Rev. 2004; 56(5): 619-58. Chien YW, Siddiqui O, Sun Y, Shi WM, Liu JC. Transdermal iontophoretic delivery of therapeutic peptides/proteins. I: Insulin. Ann N Y Acad Sci. 1987; 507: 32-51. Zeltzer L, Regalado M, Nichter LS, Barton D, Jennings S, Pitt L. Iontophoresis versus subcutaneous injection: a comparison of two methods of local anesthesia delivery in children. Pain. 1991; 44(1): 73-8. Galinkin JL, Rose JB, Harris K, Watcha MF. Lidocaine iontophoresis versus eutectic mixture of local anesthetics (EMLA) for IV placement in children. Anesth Analg. 2002; 94(6): 1484-8, table of contents. Greenbaum SS, Bernstein EF. Comparison of iontophoresis of lidocaine with a eutectic mixture of lidocaine and prilocaine (EMLA) for topically administered local anesthesia. J Dermatol Surg Oncol. 1994; 20(9): 579-83. Maloney JM, Bezzant JL, Stephen RL, Petelenz TJ. Iontophoretic administration of lidocaine anesthesia in office practice. An appraisal. J Dermatol Surg Oncol. 1992; 18(11): 937-40. Efficacy of Lidocaine IOP in Hairless Rats 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. Irsfeld S, Klement W, Lipfert P. Dermal anaesthesia: comparison of EMLA cream with iontophoretic local anaesthesia. Br J Anaesth. 1993; 71(3): 375-8. Umino M, Oda N, Yasuhara Y. Experimental and theoretical studies of the effect of electrode polarisation on capacitances of blood and potassium chloride solution. Med Biol Eng Comput. 2002; 40(5): 533-41. Howard JP, Drake TR, Kellogg DL. Effects of alternating current iontophoresis on drug delivery. Arch Phys Med Rehabil. 1995; 76(5): 463-6. Yan G, Li SK, Peck KD, Zhu H, Higuchi WI. Quantitative study of electrophoretic and electroosmotic enhancement during alternating current iontophoresis across synthetic membranes. J Pharm Sci. 2004; 93(12): 2895-908. Wang Y, Thakur R, Fan Q, Michniak B. Transdermal iontophoresis: combination strategies to improve transdermal iontophoretic drug delivery. Eur J Pharm Biopharm. 2005; 60(2): 179-91. Yan G, Li SK, Higuchi WI. Evaluation of constant current alternating current iontophoresis for transdermal drug delivery. J Control Release. 2005; 110(1): 141-50. Shibaji T, Yasuhara Y, Oda N, Umino M. A mechanism of the high frequency AC iontophoresis. J Control Release. 2001; 73(1): 37-47. Kinoshita T, Shibaji T, Umino M. Transdermal delivery of lidocaine in vitro by alternating current. J Med Dent Sci. 2003; 50(1): 71-7. Haga H, Shibaji T, Umino M. Lidocaine transport through living rat skin using alternating current. Med Biol Eng Comput. 2005; 43(5): 622-9. Ogami S, Hayashi S, Shibaji T, Umino M. Pentazocine transport by square-wave AC iontophoresis with an adjusted duty cycle. J Med Dent Sci. 2008; 55(1): 15-27. Hayashi S, Ogami S, Shibaji T, Umino M. Lidocaine transport through a cellophane membrane by alternating current iontophoresis with a duty cycle. Bioelectrochemistry. 2009; 74(2): 315-22. Wakita R, Oono Y, Oogami S, Hayashi S, Umino M. The relation between epinephrine concentration and the anesthetic effect of lidocaine iontophoresis. Pain Pract. 2009; 9(2): 115-21. Wakita R, Nakajima A, Haida Y, Umino M, Fukayama H. The relation between the duty cycle and anesthetic effect in lidocaine iontophoresis using alternating current. Pain Pract. 2011; 11(3): 261-6. Yan G, Higuchi WI, Szabo A, Li SK. Correlation of 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 71 transdermal iontophoretic phenylalanine and mannitol transport: test of the internal standard concept under DC iontophoresis and constant resistance AC iontophoresis conditions. J Control Release. 2004; 98(1): 127-38. Li SK, Higuchi WI, Zhu H, Kern SE, Miller DJ, Hastings MS. In vitro and in vivo comparisons of constant resistance AC iontophoresis and DC iontophoresis. J Control Release. 2003; 91(3): 327-43. Wei H, Chen Y, Xu L, Zheng J. Percutaneous penetration kinetics of lidocaine and prilocaine in two local anesthetic formulations assessed by in vivo microdialysis in pigs. Biol Pharm Bull. 2007; 30(4): 830-4. Mathy FX, Lombry C, Verbeeck RK, Préat V. Study of the percutaneous penetration of flurbiprofen by cutaneous and subcutaneous microdialysis after iontophoretic delivery in rat. J Pharm Sci. 2005; 94(1): 144-52. Kreilgaard M. Assessment of cutaneous drug delivery using microdialysis. Adv Drug Deliv Rev. 2002; 54 Suppl 1: S99-121. Simonsen L, Jørgensen A, Benfeldt E, Groth L. Differentiated in vivo skin penetration of salicylic compounds in hairless rats measured by cutaneous microdialysis. Eur J Pharm Sci. 2004; 21(2-3): 379-88. Durand S, Fromy B, Bouyé P, Saumet JL, Abraham P. Vasodilatation in response to repeated anodal current application in the human skin relies on aspirin-sensitive mechanisms. J Physiol. 2002; 540(Pt 1): 261-9. Horiuchi Y, Droog EJ, Henricson J, Wikström T, Lennquist S, Sjöberg F. Role of histamine release in nonspecific vasodilatation during anodal and cathodal iontophoresis. Microvasc Res. 2004; 67(2): 192-6. Tartas M, Bouyé P, Koïtka A, Jaquinandi V, Tan L, Saumet JL, et al. Cathodal current-induced vasodilation to single application and the amplified response to repeated application in humans rely on aspirin-sensitive mechanisms. J Appl Physiol. 2005; 99(4): 1538-44. Pikal MJ, Shah S. Study of the mechanisms of flux enhancement through hairless mouse skin by pulsed DC iontophoresis. Pharm Res. 1991; 8(3): 365-9. Meyer PF, Oddsson LI. Alternating-pulse iontophoresis for targeted cutaneous anesthesia. J Neurosci Methods. 2003; 125(1-2): 209-14. Xu Q, Kochambilli RP, Song Y, Hao J, Higuchi WI, Li SK. Effects of alternating current frequency and permeation enhancers upon human epidermal membrane. Int J Pharm. 2009; 372(1-2): 24-32.