* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Bacillus anthracis
Germ theory of disease wikipedia , lookup
Triclocarban wikipedia , lookup
Globalization and disease wikipedia , lookup
Gastroenteritis wikipedia , lookup
Marine microorganism wikipedia , lookup
Urinary tract infection wikipedia , lookup
Human microbiota wikipedia , lookup
Hepatitis B wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Schistosomiasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Neonatal infection wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Infection control wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
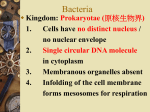
Aerobic and anaerobic sporeforming Gram-positive rods: Bacillus and Clostridium genus Obligate anaerobic bacteria Katalin Kristóf MD. Gram-positive, Aerobic or Facultative Endospore-forming Bacteria (formerly, "The Genus Bacillus") Todar's Online Textbook of Bacteriology In 1872, Ferdinand Cohn, a contemporary of Robert Koch, recognized and named the bacterium Bacillus subtilis. The organism is Gram-positive, capable of growth in the presence of oxygen, and forms a unique type of resting cell called an endospore. Endospores The formation of endospores is a complex and highly-regulated form, the process of spore formation can be divided into seven defined stages (0-VI). The vegetative cell begins spore development when the DNA coils along the central axis of the cell as an "axial filament„, b) The DNA then separates and one chromosome becomes enclosed in plasma membrane to form a protoplast, c) The protoplast is then engulfed by the mother cell membrane to form a intermediate structure called a forespore, d) Between the two membranes, The core (cell) wall, cortex and spore coats are synthesized, e) As water is removed from the spore and as it matures, it becomes increasingly heat resistant and more refractile, f) The mature spore is eventually liberated by lysis of the mother cell. The entire process takes place over a period of 6-7 hours and requires the temporal regulation of more than 50 unique genes (Pasteur Institute). a) In cross section, Bacillus spores show a more complex ultrastructure (by Viake Haas, University of Wisconsin) The spore protoplast (core; calciumdipicolate) is surrounded by: The core wall is composed of the same type of peptidoglycan as the vegetative cell wall; The cortex is composed of a unique peptidoglycan; The outer spore coat represents 30-60 percent of the dry weight of the spore. The spore coat proteins have an unusually high content of cysteine and of hydrophobic amino acids, and are highly resistant to treatments that solubilize most proteins. Depending on the species, an exosporium may be present Endospore – cryptobiotic state They are highly resistant to environmental stresses - high temperature (some endospores can be boiled for several hours and retain their viability), - irradiation, - strong acids, - disinfectants, etc. Their differentiation begins when a population of vegetative cells passes out of the exponential phase of growth, usually as a result of nutrient depletion. They germinate and become vegetative cells when the environmental stress is relieved. Endospore-formation is a mechanism of survival (millions of years) rather than a mechanism of reproduction. Classification and Phylogeny Their taxonomic hierarchy (Bergey's 2004) /largely by analysis of 16S rRNA molecules by oligonucleotide sequencing / Kingdom: Bacteria; Phylum: Firmicutes; Class: Bacilli; Order: Bacillales; - Family: Acyclobacillaceae (genus: Acyclobacillus); - Family: Bacillaceae (genus: Bacillus, Geobacillus); - Family: Paenibacillaceae (genus: Paenibacillus, Brevibacillus); - Family: Planococcaceae (genus: Sporosarcina). Robert Koch's original photomicrographs of Bacillus anthracis, the agent of anthrax (1877) The anthrax bacillus, Bacillus anthracis, was the first bacterium shown to be the cause of a disease. In 1877, Robert Koch grew the organism in pure culture, demonstrated its ability to form endospores, and produced experimental anthrax by injecting it into animals. Bacillus anthracis Morphology: - large (3-8um) Grampositive rods with characteristic squared ends - ovale spore in the center - spores do not deform the shape of the bacteria www.textbookofbacteriology.net Bacillus anthracis Morphology: - capsule from D- glutamic acid - no motile Left:India ink capsule outline 1000X. www.textbookofbacteriology.net Right a fluorescent-labeled antibody is reacted specifically with the capsular material which renders the capsule fluorescent 1000X. Bacillus anthracis Cultivation: ⇒„simpleagar”: dry, groundglass appearance ⇒ Blood agar: no haemolysis Virulence factors (encoded by plasmids) pX02 ⇒ Poly-D-glutamyl capsule protect the organism against complement and the bactericidal components of serum and phagocytes, and against phagocyte engulfment and destruction. plays most important role during the establishment of the infection, and a less significant role in the terminal phases of the disease. Mucoid colonies of Bacillus anthracis. This culture was probably incubated at an increased CO2 tension (5% CO2) which greatly enhances production of the poly-D-glutamyl capsule and accounts for the mucoid colony type. pX01 ⇒ Factor I =Edema factor (EF) : calmodulindependent adenylate cyclase Factor II =Protective antigen (PA), binds to specific receptors on the host cell surface – as the B „binding” moiety) Factor III = Lethal factor (LF) : Znmetalloprotease, leading to cell death PA binds to receptors on host cell surfaces: Brain, heart, intestine, lung, skeletal muscle, pancreas, macrophages Virulent anthrax bacilli multiply at the site of the lesion - capsule! A short range effect of the toxin is its further impairment of phagocytic activity and its lethal effect on leukocytes, including phagocytes, at the site. After the organisms and their toxin enter the circulation, the systemic pathology, which may be lethal, will result Combinations of two or three of the toxin components yield the following results PA+LF combine to produce lethal activity EF+PA produce edema PA+LF+EF produces edema and necrosis and is lethal Epidemiology: Anthrax is primarily a disease of domesticated and wild animals, particularly herbivorous animals – „black-bone” (cattle, sheep, horses, mules and goats) Humans become infected incidentally when brought into contact with diseased animals, which includes their flesh, bones, hides, hair and excrement. Even in endemic areas, anthrax occurs irregularly, often with many years between occurrences. In the United States: 1-2 cases of cutaneous disease per year 2001: 22 cases of anthrax (11 inhalation, 11 cutaneous) were identified in the USA following intentional contamination of the mail (5 death). Bioterrorism! Anthrax cases - natural 1. 2. 1. Epidemy (animals) 2. Local infection (animals) Forrás: anthrax BBC tények Human Diseases 1. Cutaneous anthrax : malignant pustule (95%) → spores from the soil or a contaminated animal through injured skin → the spores germinate → vegetative cells multiply → characteristic edema and → painless papule at the site of inoculation → progressing to an ulcer surrounded by vesicles → necrosis Day 6 Malignant pustule Day 10 Day 15 Local laesion + oedema Source: CDC Anthrax Images Pustula maligna + oedema Pustula maligna and oedema 2. Pulmonary anthrax („wool sorters’ disease”): Inhalation → hemorrhagic pneumonia, mediastinitis → respiratory failure The disease begins abruptly with high fever and chest pain. It progresses rapidly to a systemic hemorrhagic pathology and is often fatal if treatment cannot stop the invasive aspect of the infection. Biological weapon ! Inhalation/Lung anthrax (X-ray) Mediastinal widening Source: CDC Anthrax Images … and pleural effusion 3. Gastrointestinal anthrax - Bloody diarrhoea: Ingestion of spores (very rare in humans!) Ulcers form at site of invasion (mouth, oesophagus, intestine) → mesenteric lymphadenopathy → abdominal pain, vomiting → oedema, sepsis (100% mortality) Bacillus anthracis - Biological Warfare Anthrax spores may survive in the soil, water and/or surfaces for many years a cloud of anthrax spores would be released at a strategic location to be inhaled by the individuals under attack hemorrhagic pneumonia an infection of local animal populations (sheep, cattle) could follow a biological attack with spores infected animals could then transmit the disease to humans Diagnosis: 1. 2. Smear: fluid from local lesion Cultivation 1. 2. 3. Non-hemolytic, adherent colonies McFadyean's reaction showing short chains Morphology Bacillus anthracis cells lying among Confirmed by demonstrating of amorphous, disintegrated capsular material. capsule (india-ink, DFA) or White blood cells can also be seen by lysis with gamma phage 3. PCR (pX01, pX02) 4. LF protein detection 5. Anti-PA IgG ELISA Therapy: Quinolones (penicillin, tetracyclin) administered before the onset of lymphatic spread! Anthrax immune globulin Prevention: Possible vaccination for „risk” groups protective antigen recovered from the culture filtrate of an avirulent, nonencapsulated strain of Bacillus anthracis that produces PA during active growth (6 subcutaneous injections, annual booster injections) Vaccination of animals (Pasteur 1881) Burning of burial of animals that died of anthrax Bacillus cereus Morphology: Gram-positive, spore-forming rod www.textbookofbacteriology.net Bacillus cereus Cultivation : „simple” agar: „cut-glass” appearence Blood agar: β - hemolysis Egg-yolk agar: lecitinase reaction Clinical findings 1. Food poisoning - food-borne illnesses A) Emetic form („short incubation”, like S.aureus~) from contaminated rice dishes that have been cooked and then held at warm temperatures for several hours; Mexican and Chinese restaurants 1-6 hrs incubation period nausea, vomiting, abdominal cramps Heat-stable enterotoxin: emetic toxin (?) B) Diarrheal form („long incubation form”, like C.perfringens~) From contaminated meat, vegetables, sauces 8-16 hrs incubation period abdominal cramps, watery diarrhoeae Heat-labile enterotoxin:acts by activation of adenylate cyclase enzymes. Diagnosis - - The emetic form of the disease is diagnosed by the isolation of B. cereus from the incriminated food (greater than or equal to 105 B. cereus organisms per gram) The long-incubation form is diagnosed by isolation of the organism from stool and food. Treatment - Because B. cereus gastroenteritis is generally a benign, self-limited illness, antimicrobial agents are of no value in management. Prevention - Since the bacteria grow best at temperatures ranging from 4 to 60 °C, infection may be prevented if cold food is refrigerated and if hot food is held at greater than 60°C before serving. 2. Ocular infection After traumatic, penetrating injuries IV. drug users – systemic diseaes Virulence factors: Necrotic toxin, cereolysin (hemolysin), phospholipase C (lecithinase) Treatment: vancomycin, clindamycin, fluoroquinolones 3. Intravascular catheter-associated infection, sepsis 4. Fatal pneumonia? Other aerobic sporeformers Antibiotic Producers: antibiotics produced by the are often, but not always, polypeptides. Brevibacillus brevis (e.g. gramicidin, tyrothricin), Bacillus cereus (e.g. cerexin, zwittermicin), Bacillus circulans (e.g. circulin), Brevibacillus laterosporus (e.g. laterosporin), Bacillus licheniformis (e.g. bacitracin), Paenibacillus polymyxa (e.g. polymyxin, colistin), Bacillus pumilus (e.g. pumulin) Bacillus subtilis (e.g. polymyxin, difficidin, subtilin, mycobacillin). Paenibacillus alvei, B. megaterium, B. coagulans, Brevibacillus laterosporus, B. subtilis, B. sphaericus, B. circulans, Brevibacillus brevis, B. licheniformis, P. macerans, B. pumilus and B. thuringiensis have been occasionally isolated from human infections. Gastroenteritis, opportunistic infection Geobacillus stearothermophilus are used to test heat sterilization procedures THE CONTROL OF THE AUTOCLAVE’S NORMAL FUNCTION -NORMAL FUNCTION- the spores consume, the color is yellow -NOT NORMAL FUNCTION - the spores survive, and start to germinate, multiply, the color will be change from purple to yellow Anaerobes: general characteristics 1. For growing: → low oxido-reduction potencial Don’t able to grow on the rigid cultivation surface, if >10% CO2; >18% O2 (def. by Finegold) 2. Anaerobic bacteria do not have Cytochrome system for oxygen metabolism Superoxide-dismutase 2O2 + 2H+→O2 + H2 O2 Catalase (partly) H2O2 + H2O2 → 2H2O + O2 Peroxidase (partly) H2O2 + H2R → 2H2O + R Effects of oxygen on aerobic, anaerobic, and facultative anaerobic bacteria 3. Anaerobes are part of the normal flora Mouth CFU/ml 109/ml aerob/anaerob 1/30 Colon 1011/ml 1/1000 (100-400 different anaerobic species) Vagina 107/ml skin ? ? 10/1 genus Peptococcus,Peptostreptococcus, Lactobacillus, Bifidobacterium, Actinomyces, Bacteroides, Porphyromonas, Fusobacterium, Treponema, … Peptococcus,Peptostreptococcus, Lactobacillus, Bifidobacterium, Eubacterium, Clostridium, Bacteroides, Porphyromonas, Fusobacterium Lactobacillus, Bifidobacterium, Peptostreptococcus, Eubacterium, Bacteroides, Prevotella, … P.acnes, other Propionibacterium 4. Anaerobes are potentially pathogenic when displaced from normal environments and implanted in dead or dying tissue - predisposing factors! medmicro Types of infection commonly produced by anaerobic bacteria disease bacteriemia Brain abscesses subdurale empyema chronic otitis media After aspirations → pneumonia Lung abscessus Intra-abdominal infections Liver abscessus appendicitis, peritonitis Vulvovaginale abscessus Pelvic inflammation endometritis Bacterial vaginosis 5. Often cause polymicrobial infection frequency 5-20 % 89% 10% 52% 93% 95% 93% 50-100% 96% 74% 92% 73% 100% Disease caused by anaerobic bacteria Exogen infection Spore-forming clostridia Monobacterial Toxin-mediated Endogen infection Non spore-forming bacteria Polymicrobial infection Complex pathogenesis Predisposing factors: O2 ↓: shock, angiopathia, d.m., „cut the barrier”: aspiartion, operation, trauma, Clostridia-general characteristics Clostridia are strictly anaerobic to aerotolerant sporeforming bacilli Found in soil as well as in normal intestinal flora of man and animals Large, Gram-positive rods Form characteristic spores, the position of which is useful in species identification Wide variety of extracellular enzymes (biodegradation & invasive infection) Exotoxin production Classification and Phylogeny Their taxonomic hierarchy (Bergey's 2004) /largely by analysis of 16S rRNA molecules by oligonucleotide sequencing / Kingdom: Bacteria; Phylum: Firmicutes; Class: Clostridia; Order: Clostridiales; - Family: Clostridiaceae 11 genera, including Clostridium genus Clostridium perfringens Large, (1-2 um * 7-8 um), ovale-spores are central Non-motile, has capsule oregonstate.edu/research/Images/SarkerSlide.jpg www.textbookofbacteriology.net Clostridium perfringens Blood agar plate: double β, α-hemolysis Metabolically active → gas production (CO2, H2S,CH4) Clostridium perfringens Type : A, B, C, D, and E Toxins: α-toxin = lecithinase, phospholipase C Damage to cell membrane Lysis of RBC, WBC, PLT, endothelial cells Increased vascular permeability with massive haemolysis & bleeding, tissue destruction Hepatic toxicity + myocardial dysfunction β-toxin → necrotizing activity ε-toxin → increases vascular permeability of the GI wall Iota-toxin → the same + necrotic activity Enterotoxin (superantigen) Enzymes: Collagenases, hyaluronidases, DN-ase, lipases, proteases 1. Gas gangrene: - Exogenic infection -penetrating wound, contaminated with spores - Endogenic infection: after gut ruptura, appendicitis perforata (rare), after amputation - Septic abortus Gas gangrene is the most deadly type of gangrenous infection because it spreads so rapidly and does the most damage. Incubation period:1-3days → Pain, edema around the infected wound → Severe systemic, toxic symptoms, high fever → Brownish, or bloody serous exudate with the discoloration of the surrounding skin → foul or sweet smell → Gas is detected among tissues (blood vessel compression - ischemia) Diagnosis Clinical specimen: pus, necrotic tissue, blood Direct smear, cultivation Spores and WBC-s are not seen in smears from clinical samples Phase-contrast M Nagler plate lecithinase activity - when a culture is grown on a medium rich in phospholipids such as egg yolk agar, lecithinase activity is detected as a opalescence which develops around the colonies as the phospholipids are split into insoluble diglycerides. Nagler-reaction positive - neutralisation of lecithinase C by a specific antitoxin Treatment It can be fatal if not treated immediately Surgical debridements (amputation) Very high dose penicillin therapy The role of hyperbaric oxygen remains controversial Supportive therapy G-CSF Prevention State of art surgical management of wound in regard preventing from anaerobic conditions is essential. Gas gangrene - other clostridia C. septicum 20 % motile, peritrich flagellae α-toxin => necrotic, haemolytic activity /From blood culture – underlying intestinal malignancy!/ C. novyi A 40% Motile, peritrich flagellae Toxaemia α, β, δ, ε toxin => haemolytic, necrotic activity phospholipases, lipases C. histolyticum 10-20% C. sordelii Clostridium septicum Necrotizing fasciitis Background: colon tumor Hello My name is C. perfringens. I'm a Gram Positive rod and anaerobic. I live in soil and can make spores to survive to for a long time. I can cause myonecrosis, or "gas gangrene". I get into your muscles in wounds and make toxins. As I eat away at your muscles, I let off gases that build up between them. When I am "type A", I can cause food poisoning. I live in undercooked meat and make spores in your gut. I make an enterotoxin that gives you cramping and diarrhoea. My "type C" form causes "necrotising enteritis". You have to eat undercooked pork with me in it. You also have to eat a lot of foods like sweet potatoes, which have a chemical called trypsin inhibitor in them. When they are together, I can make my β-toxin and eat away at your bowels. Clostridium perfringens–2. Food poisoning Clostridium perfringens „A” produces an enterotoxin and is an important cause of food poisoning C. perfringens is a ubiquitous, and a frequent contaminant of meat and poultry. By sporulating, this organism can survive high temperatures during initial cooking; the spores germinate during cooling of the food, and vegetative forms of the organism multiply if the food is subsequently held at temperatures of 16-52oC. If served without adequate reheating, live vegetative forms of C. perfringens may be ingested. The bacteria then elaborate the enterotoxin 8-24 hours incubation period Watery diarrhea, abdominal cramping, vomiting, fever Self-limited (24-48 hours) Clostridium perfringens–2. Food poisoning Diagnosis: Enterotoxin detection – from fecal sample Cultivation: greater than or equal to 105 organisms per gram of epidemiologically implicated food. An alternate criterion is that cultures of stool samples from persons affected yield greater than or equal to 106 colonies per gram C. perfringens–3.enteritis necrotisans β-toxin producing „C” type Incubation period:8-12 h (pork meat) Necrotic lesions in jejunum, Bloody diarrhea, peritonitis, shock High mortality Diagnosis: Enterotoxin detection – from fecal sample www.3tres3.com Clostridium tetani Morphology: ⇒ Gram-positive rods, spores are terminal (cells look like drumsticks) WWW.textbookofbacteriology.net Clostridium tetani Cultivation: more sensitive to oxygen Broth culture:no evidence of gas production Dextrose-blood agar: greyish colonies, no hemolysis Clostridium tetani Found in soil & colonizes the GI tract of many animals & humans (0-25%) small puncture wounds or lacerations which become contaminated with C. tetani spores that germinate and produce toxin Incubation period varies 45 days to weeks tetanus is a highly fatal disease of humans mortality rates reported vary from 40% to 78% Clostridium tetani Tetanospazmin (subunit A and B) Heat-labile, plasmid encoded Produced during stationary phase of growth Released when the cell is lysed Being internalized & moves from the peripheral nerve terminals to the central nervous system by retrograde axonal transport Being released from the postsynaptic dendrites Localized within vesicles in the presynaptic nerve terminals Acts by blocking the release of inhibitory neurotransmitters (GABA) Causing exitatory synaptic activity to be unregulated Tetanus Generalized: the most frequent type Trismus /lockjaw:spasms of the masseter muscles Sardonic smile/risus sardonicus:facial muscles Opisthotonus :persistent back spasms irritability Involvement of the autonomic nervous system (cardiac arrhytmias,... Neonatal The site of primary infection is the umbilical stump Progresses to generalized – 90% mortality rate Localized Cephalic Clostridium tetani Sir Charles Bell’s portrait of a soldier dying of tetanus www.textbookofbakteriology.net Laboratory diagnosis: Clinical symptoms (anamnesis, immunization history) Culture from wounds are not useful… Samples for antitoxin level (DD:strychnine poisoning) Treatment: passive immunisation with antitoxin (Human Tetanus Immunoglobulin) Surgical management Tetanus toxoid – active immunisation Metronidazol Critical care unit Prevention: /even a lethal dose of tetanospasmin is insufficient to provoke an immune response/ Prophylactic immunization is accomplished with tetanus toxoid, as part of the DPT (DTaP) vaccine or the DT (TD) vaccine.. Clostridium botulinum Morphology: Gram positive rods, subterminal spore www.textbookofbacteriology.net Clostridium botulinum Botulinum toxin: Group I: A, B, F Group II: B, E, F Group III: C, D, Group IV: G „B” : protects the toxic subunit from being inactivated by gastric acids A : Specific for cholinerg nerves (neurotoxin) Blocks the release of acetylcholine at peripheral cholinerg synapses Flaccid paralysis • Single strain almost always produces only one toxin type • 1 mg 30M LD50 mouse D • Spores are found throughout the world in soil samples and marine sediments • These spores are able to tolerate 100°C for hours Clostridium botulinum Clinical syndromes 1. Foodborne botulism – Intoxication Fish fillets Canned salmon Corned beef Pasta products Canned vegetables toxin production outside the body After 1-2 days of consuming the contaminated food Blurred vision, fixed dilated pupils Dry mouth, constipation, abdominal pain Bilateral descending weakness of the peripheral muscles flaccid paralysis (symmetrical) Death – due to respiratory paralysis Clear sensorium through out the disease, no fever Blurred vision, fixed dilated pupils dry, furrowed tongue 2. Infant botulism – infection caused by toxin producing in vivo Bacteria can colonise the GI tract of infants younger than 6 months – the absence of competitive bowel microbes Source of infection : honey constipation, weak sucking ability and generalized weakness Possible cause of sudden infant death 3. Wound botulism Symptoms are similar to those of foodborne infection Incubation period is longer Clostridium botulinum Diagnosis: Isolation of microorganism – faeces, food Toxin activity – serum, faeces, food ELISA Animal inoculation (mouse bioassay) Treatment: Passive immunisation as soon as possible with trivalent (A,B,E) antitoxic serum (equine) Supportive therapy Prevention: Proper food handling and preparation Clostridium difficile Part of the normal GI flora in a small number Pathogenesis: Endogenous source disease: Broad spectrum antibiotics alters the normal enteric flora Permitting the overgrowth of C.difficile antibiotic associated diarrhea pseudomembranous colitis Clostridium difficile Exogenous source: The hospitalized patient more susceptible to the exogenous aquisition of C.difficile – nosocomial infection Proliferation in the colon A toxin : mainly enterotoxin B toxin : cytotoxin toxin production hemorrhagic necrosis Treatment: atb EX, + metronidazole or vancomycin administered orally Fecal transplantation Clostridium difficile CDAD: an emerging public health crisis Hypervirulent toxin-producing strains – O27/NAP1 Many severe cases + binary toxin (ADP ribosylating toxin) Clostridium difficile Diagnosis: Rapid test: toxin detection Immunochromatogen PCR ELISA, EIA Cultivation CCFA (the colonies are generally flat, gray in colour, with irregular margin and ground-glass appearence; Distinctive „barnyard” odour Antibiotic-associated colitis. Assay of C. difficile toxin showing normal babyhamster kidney cells (left) and cells after exposure to toxin (right). Note rounding up of cells folowing exposure to toxin. Gram negative anaerobic bacteria Bacteroides fragilis Prevotella spp. P.bivia, P.disiens Porphyromonas spp. F. nucleatum, - GI - intraabdominal infection - mouth - periodontitis, orofacial abscess - vagina - pelvic abscessus - mouth - periodontitis, orofacial abscess - mouth, colon, vagina - mixed pyogenic infection F.perodonticum „ - lower respiratory tract infection F. mortiferum „ - intraabdominal infection F. necrophorum „ - pelvic abscessus Leptotrichia buccalis - mouth - ulcerative gingivo-stomatitis Gram negative anaerobic bacteria Bacteroides (B.fragilis, B.distanosis,…) capsular polysaccharide superoxid dismutase hyaluronidase, fibrinolysin, DN-ase, heparinase Prevotella (P. melaninogenica, P. bivia…) IgA protease collagenase, fibrinolysin Porphyromonas (P.asaccharolytica, P.gingivalis) has trypsin-like activity collagenase Fusobacterium (F. nucleatum, F. varium) Gram negative anaerobic bacteria medmicro Vincent’s angina Ulcerative tonsillitis causing tissue necrosis often due to extension of acute ulcerative gingivitis Fusobacterium nucleatum in combination with oral spirochates (Treponema vincentii and others) causes the fusospirochaetal infections www.lg1.ch Giemsa stained smear - Angina Plaut-Vincent Acute necrotizing ulcerative gingivitis (Vincent’s infection. Ulceration of the gingival margin spreading into the gums. NOMA Bacterial necrosis that develops in the mouth and ravages the faces of its victims. It destroys both the soft and bone tissues of the face and mostly affects young children between the ages of two and six. As the disease progresses, the jaws become locked. Victims slowly lose the use of their mouths. The infection gradually attacks the nose and sometimes the eyes, making it difficult to eat, breathe or see. 80 percent death rate peritonitis Lung abscess Most (>90%) cases of lung abscess reflect the aspiration of anaerobic bacteria from the oropharynx. The infections are typically polymicrobial, with fusiform bacteria and Bacteroides species often isolated. Other organisms encountered in lung abscesses caused by aspiration include S. aureus, K. pneumoniae, S. pneumoniae, and Nocardia. Bacterial vaginosis. The clue-cell – a vaginal epithelial cell with attached microorganism. The attached bacteria give the clue cell a stippled appearance. periodontitis Gram negative anaerobic bacteria Fusobacterium nucleatum (Vincent’disease) Fusobacterium sp. Fusobacterium spp. pharmacie.univ-lille2.fr Bacteroides fragilis capsular polysaccharide superoxid dismutase hyaluronidase, fibrinolysin, DN-ase, heparinase Bacteroides Bile Esculin Agar (BBE) Colonies of Bacteroides fragilis growing on an agar surface www.bdj.co.jp web.bio.ed.ac.uk Eosin/Carbol fuchsin capsule smear of population of B. fragilis grown in defined medium broth showing phase variation; note non-capsulate bacteria and those with small and large capsules (viewed with x100 objective). www.sanger.ac.uk Prevotella melaninogenica Prevotella (P.melaninogenica, P. bivia…) - IgA protease - collagenase, - fibrinolysin Prevotella intermedia Porphyromonas spp. Anaerobic cocci Changing of the nomenclature Changing of the clinical relevance Diagnostic problems Anaerobic cocci Gram-negative : Veilonella spp., Acidaminococcus fermentans, Megasphera elsdenii normal flora: mouth, skin, intestinal tract, genitourinary tract infection is usually results from invasion of damaged tissue by normal microbial flora Gram-positive Peptostreptococcus anaerobius, Peptococcus niger, Finegoldia magna, Anaerococcus spp., Gallicola sp, Micromonas sp., Peptoniphilus spp., Atopobium parvulum normal flora: mouth, skin, intestinal tract, genitourinary tract clinical manifestation: a great variety of infections : abscesses, gangrene, cellulitis, bacteraemia, pneumonia, peritonitis, bite wounds, pelvic inflammatory disease Mixed infection Fig. 2.92 Lung abscess. Gram stain of pus showing Gram-positive cocci and varoius Gram negative and Gram positive rods. By courtesy of J.R. Cantey Isolation and identification of anaerobes MIC PCR General laboratory diagnosis Anaerobic conditions are required for sample collection, culturing and identification Antibiotics : after MIC determination metronidazol clindamycin imipenem penicillin Chloramphenicol resistance intrinsic/natural : aminoglycosides! Extrinsic/acquired: beta-lactamase; B.fragilis penicillin R PBP changing; cefoxitin R bacteroides OMP permeabilitate changing; pl.cefoxitin R bacteroides tetracyclin R metronidazol R chloramphenicol R Thank you for your attention!