* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Severe Diarrhea and Irritable Bowel Syndrome
Survey
Document related concepts
Transcript
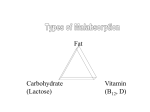
Nutrition and Disorders of the Lower GI Tract 報告者:臺北醫學大學•市立萬芳醫院 報告日期:民國 88 年 12 月 9 日 葉文慧 營養師 This chapter describes disorders of the lower GI tract that either influence nutrition status or are affected by diet. Severe Diarrhea and Irritable Bowel Syndrome Two common disorders of the GI tract are diarrhea and irritable bowel syndrome. Diarrhea Diarrhea is not a disease but a symptom of many medical conditions and treatments. Acute--lasting less than 2 weeks Chronic--lasting longer Mild diarrhea that remits in 24 to 48 hours is seldom a cause for concern unless the person is already dehydrated A person with severe, persistent diarrhea may rapidly become dehydrated, lose weight, and develop multiple nutrient deficiencies. A child or infant can lose proportionately more fluid and weight and can develop dehydration and malnutrition in a short time. Causes of Diarrhea Acute diarrhea 1.It occurs abruptly in a healthy person frequently results from viral, bacterial, or protozoal infections or as a side effect of medications. 2.It can also occur in the person who begins to eat foods or begins a tube feeding after a period of fasting or starvation. 3.Infants often develop diarrhea when given formulas their immature GI tracts cannot handle or when they are ill. 4.When used in large quantities, food ingredients such as sorbitol and olestra may cause diarrhea in some people. Chronic diarrhea 1.It can occur as a result of disorders that alter GI tract motility, such as the irritable bowel syndrome. 2.From any disorder that causes malabsorption. 3.From food intolerance (for example: lactose intolerance) 4.From some infections, including some parasitic infections and human immunodeficiency virus (HIV). 5.Associated with the dumping syndrome. Treatment of Diarrhea Food--If a food is responsible for diarrhea, then that food must be omitted from the diet. Drug--If a drug is responsible, a different drug, when possible, or different drug form (for example: injectable versus oral) may alleviate the problem. Oral Diets Often people with diarrhea can tolerate regular diets. Avoid highly seasoned foods, fatty foods, gas-forming foods (Table 22-1), lactose-containing foods, caffeinated beverages, and any food that aggravates the diarrhea. In other cases, clients may be advised to drink only clear liquids (Table 22-2) to avoid irritating the GI tract while replacing fluids and electrolytes. Homemade or commercial oral rehydration formulas--simple solutions of water, salts, and sugar--provide needed fluids and electrolytes. For mild cases of diarrhea, fluids and electrolytes can be replaced using fruit juices, sport drinks, caffeine-free carbonated beverages, tea, and broth with crackers. A regular diet by adding moderately seasoned, low-fiber, low-fat foods as tolerated. Frequent small meals are easiest to tolerate at first. Excludes lactose and any foods believed to have irritated the GI tract. Bowel Rest In severe cases of diarrhea, stop placing demands on the GI tract by withholding all foods and beverages until the diarrhea remits, usually in about 24 to 48 hours. Alternative Feedings Nutritionally complete, lactose-free liquid formulas People with severe diarrhea who are unable to tolerate any type of oral or tube feeding, intravenous nutrition is indicated, and nothing is given by mouth (NPO). Irritable Bowel Syndrome Syndrome indigestion, nausea, abdominal pain, bloating, flatulence, diarrhea, constipation, or alternating diarrhea and constipation. Emotional stress may worsen the symptoms, which frequently occur shortly after a person eats and often resolve temporarily following a bowel movement. Treatment Mild diarrhea may remit without treatment Severe diarrhea can lead to dehydration, electrolyte imbalances, and malnutrition. During treatment, diet therapy may range from complete bowel rest to individualized regular diets. A low-fat diet provided in small meals, with a gradual increase in fiber, is helpful. How to lessen the symptoms of Irritable Bowel Syndrome Recommend Identify individual food intolerances by keeping a food record that includes symptoms and the time they occur in relation to meals Avoid offending foods or substances Common intolerances include milk and milk products (lactose), fatty foods, gas-forming foods and beverages (Table 22-1), caffeine, alcohol, and foods containing large amounts of fructose or sorbitol Eat frequent small meals at a relaxed pace and at regular times Gradually add dietary fiber to the diet by including more who1e-grain breads and cereals, fruits and vegetables, dried beans and peas, and nuts. Because high-flier foods are often gas producing, add fiber gradually to allow the CI tract time to adapt Drink plenty of fluids. Fiber attracts water as it moves through the GI tract, so more water is needed. Get regular physical activity to reduce stress. ※Physicians may also recommend bran or hydrophilic colloids to help relieve constipation. Bran is likely to produce gas, so hydrophilic colloids may be a better choice for some people. Nutrition Consequences of Malabsorption Many disorders cad to malabsorption, and any nutrient can lie involved. The lower GI disorders that affect nutrition most profoundly are those that cause fat malabsorption, which consequently affects the absorption and metabolism of many other nutrients. Unabsorhed fat--steatorrhea Protein malabsorption--malnutrition Fat Malabsorption Fat absorbing depends on lipase from the pancreas and bile from the liver and is more complex than the process for absorbing protein and carbohydrate. The loss of fat in the stools means that valuable food energy, fat-soluble vitamins, and some minerals are lost as well (Figure 22-2) The loss of food energy affects protein metabolism as well. Vitamin and Mineral Malabsorption Fat-soluble vitamins lost when far is excreted in steatorrhea. Minerals normally are absorbed in the colon, but when fat malabsorprion occurs, unabsorbed fatty acids form soaps with calcium and magnesium and carry these minerals out of the body Vitamin D losses further aggravate calcium malabsorption. Oxalate Stones Hyperoxaluria--Oxalate normally binds with some of the calcium in the gut and is excreted with it. But when fatty acids bind the calcium, the oxalate remains unbound, The intestine absorbs the unbound oxalate, but the body cannot metabolize it and so excretes it in the urine, High urinary oxalate favors the formation of kidney stones. Treatments for Fat Malabsorption Drug therapy Surgery Dietary fat is often restricted Enzyme replacements Fat-Restricted Diets Usually it ranges from 20 to 40 percent of total energy Person with malabsorption begins with a diet containing 35 to 45 grams of fat. The person may gradually increase fat intake to provide additional energy as needed. Table 22-3 Medium-Chain Triglycerides Diet is not severely restricted in fat for any longer than is necessary; the person needs food energy. Instead, the diet may provide some fat from medium-chain triglycerides (MCT) rather than long-chain triglycerides (LCT). MCT oil does not contain essential fatty acids, so the diet must include some LCT. Water-Miscible Fat-Soluble Vitamins Person with malabsorption absorbs enough fat-soluble vitamins so that a standard supplement can be given. Oxalate-Restricted Diets To reduce the risk of oxatate stones--limit foods high in oxalate. High oxalate contents include spinach, rhubarb, beets, nuts, chocolate, tea, wheat bran, and strawberries. Enzyme Replacement Therapy Enzyme replacements:Extracts of pork or beef pancreatic enzymes that taken as supplements to help with digestion Enzyme replacements are used when the person suffers malabsorption related to chronic and severe damage to the pancreas or whenever steatorrhea is severe Lessen the malalbsorption of protein and fat, but may not fully correct it. Fat undergoes the most complex process of digestion and absorption and, therefore, is the most likely to be affected by disorders that cause malabsorption. The loss of fat in the stools leads 1.loss of food energy 2.The malabsorption of fat-soluble vitimins, calcium, and magnesium 3.The increased absorption of oxatate Dietary therapy for fat malahsorption include 1.Fat- and oxalate-restricted diets 2.Use or MCT, water-miscible fat-soluble vitamins 3.Use enzyme replacements How to improve acceptance Fat restricted diets Malabsorption Syndromes Malabsorption can occur when the flow of enzymes from the pancreas or bile from the liver is disrupted Pancreatitis Pancreatic secretions digestion of protein, fat, and carbohydrate, together with bicarbonate-rich juices that provide the optimal pH necessary to activate these enzymes. Acute Pancreatitis Typical symptoms: severe abdominal pain, nausea, and vomiting. Complications: reduced blood volume, acute renal failure, respiratory failure, pancreatic hemorrhages, fistulas, and abscesses. Gallstones or alcoholism(the reasons are unclear) Treatment of Pancreatitis Initial therapy in all cases aims to suppress pancreatic secretions. Nasogastric tube Intravenous fluids necessary. Mild-to-Moderate Pancreatitis A clear-liquid diet a low-fat diet a regular diet as tolerated If intake fails more than a weektube feeding(to the jejunum to stimulate pancreatic secretions) use easy-to absorb formulas Intravenous feedings(if enteral feedings worsen abdominal pain, edema, or drainage from fistulas, or if vomiting is a problem) Chronic Pancreatitis 1.The pancreatic cells permanently destroyed 2.Chronic alcohol abuse With extensive degeneration of the pancreas and chronic pancreatitis, however, digestion, especially of fat, becomes permanently impaired. Abdominal pain, frequently vomiting, and severe weight loss. Nutrition Support The goal of diet therapy 1.To maintain optimal nutrition status 2.Reduce steatorrhea 3.Minimize pain 4.Avoid subsequent attacks of active pancreatitis Health care professionals recommend 1.Moderate fat-restricted diet 2.Small meals 3.No alcohol 4.Enzyme replacements Complicating Conditions Pancreatitis damages the cells that produce the hormones insulin and glucagon 1.glucose intolerant, as in diabetes 2.Glucagon deficiency hypoglycemia the task of regulating blood glucose Cystic Fibrosis A hereditary disorder characterized by the production of thick mucus that affects many organs, including the lungs, pancreas, liver, heart, gallbladder, and small intestine. Three major consequences 1.Chronic lung disease 2.Pancreatic insufficiency 3.Abnormally high electrolyte concentrations in the sweat Treatment of Cystic Fibrosis 1.To promote appropriate growth development 2.Prevent respiratory failure and complications. 3.Treatment includes respiratory, diet, and drug therapy. Energy and Nutrient Needs Nutrient losses through 1. Malabsorption 2. Frequent infections 3. Rapid turnover of protein and essential fatty acids 4. High protein catabolism 5. High basal energy expenditures raise People with cystic fibrosis to between 120 and 150 percent of the RDA for sex and age. Extra energy is needed simply to breathe. Dietitians estimate individual energy requirements based on basal metabolic rate, activity level, pulmonary function, and degree of malabsorption. Loss of appetite 1.Repeated infections 2.Emotional stress 3.Drug therapy 4.Coughing Diet and Enzyme Replacement Therapy High energy needs, fat restrictions are inappropriate Pancreatic enzyme replacements are used to control steatorrhea, relieve abdominal pain, and reduce the mass and frequency of stools passed Feeding Infants Infants with cystic fibrosis, breastfeeding can sustain normal growth, if enzyme replacements are given. Needs about 1/8 to 1/4 teaspoon of table salt daily, given with water to replace sweat-induced electrolyte losses Infants who are not breastfed can usually tolerate regular infant formulas. Special formulas Feeding Children and Adults A high-kcalorie, nutritionally balanced diet carefully tailored to the child's tolerances Indirect calorimetry may provide a more accurate assessment of energy needs than formula estimates, especially in preadolescent children Nutrient Supplementation Carbohydrate supplements, MCT oil and protein powders can be added to foods to boost energy and protein intakes Multivitamin supplements fat-soluble vitamins water-miscible vitamin(severe steatorrhea) Minerals Abnormally high concentrations of electrolytes (sodium and chloride) in sweat Table salt and fluids is encouraged. Alternate Feedings Need regular nutrition assessments(Height and weight measurements) For adults, the goal is to maintain a healthy weight for height. For children, to maintain weight at greater than 90 percent of that appropriate for height, gender, and age. 1.If weight below 85 percent of standard weight, feeding by tube 2.If weight below 75 percent malnutrition feeding by tube or by vein Home nutrition programs that include oral diets during waking hours and tube feedings or intravenous nutrition during sleep Emotional Support Face repeated hospitalizations and often an early death Nutrition is only one They must manage daily respiratory therapy treatments, enzyme replacements1 and, often, antibiotics Crohn's Disease Inflammation and ulceration along the length of the GI tract, often with granulomas; also called regional ileitis. The two most prevalent disorders that inflame the bowel are Crohn's disease and ulcerative colitis. Inflammatory bowel diseases (IBD) share some clinical features but are distinct conditions. Their causes remain unknown, although heredity environment, and immune functions are thought to be contributing factors. In Crohn's disease, cracklike ulcers and many granulomas accompany inflammation of the bowel. Crohn's disease most often affects the ileum and colon, but can affect the entire Gl tract and even the liver, kidneys, joints, eyes, and skin. The incidence: 1.20-40 years of age 2.Jews There is no medical cure for Crohn's disease, and even after acute symptoms resolve, recurrences are likely Complications As the disease progresses, fibrous tissue forms in the intestine, reducing its absorptive ability, narrowing the intestinal lumen, and sometimes causing an obstruction. The intestine may also rupture and cause a severe, and sometimes fatal, infection (peritonitis) Fistulas may develop if an inflamed loop of intestine sticks to another loop of intestine, to another organ, or to the skin and gradually erodes 1.If a fistula forms between the stomach or the upper portion of the small intestine and the colon, ingested food is shunted directly into the colon, and further malabsorption results, Bacteria from the colon can then invade the stomach or upper small intestine, contributing to further malabsorption, increasing the risk of serious infections, and causing severe inflammation, nausea, and vomiting. 2.If a fistula forms between the small intestine and the skin, significant malabsorption can occur if large volumes of fluid are lost. Surgery to remove a diseased or obstructed portion of the intestine or to repair a fistula further taxes nutrition status. Nutrition Status The person with Crohn's disease often experiences emotional stress, anorexia, weight loss, fever, diarrhea, malabsorption, and cramping abdominal painall can lead to nutrient deficiency. 1.Oral intake may be withheld so that the bowel can rest 2.Drug therapy can further impair nutrition status. 3.If the person requires surgery or develops an infection, nutrient needs become even greaten (Short-Bowel Syndrome). 4.Children with Crohn's disease need additional nutrients to support growth and maturation Protein-energy malnutrition (PEM) and deficiencies of calcium, magnesium, zinc, iron, vitamin B12, folate, vitamin C, and fat-soluble vitamins are commonly reported. Low serum albumin and multiple nutrient deficiencies threaten immune function and may reduce the effectiveness of drug therapy, Nutrition Support Formulas provided by mouth or by tube or total nutrition by vein 1.Oral 2.Enteral nutrition (hydrolyzed) 3.Feedings by vein (1) when oral or tube feedings significantly aggravate pain and diarrhea (2) when the bowel is obstructed or the client is at risk for obstruction (3) when complete bowel rest might help a fistula to close (4) when oral or tube feedings cannot meet nutrient requirements. Oral Diets A high-kcalorie, high-protein diet. A fat-restricted diet (fat malabsorption) Low-fiber diets(partial obstructions of the intestine) Intolerant to certain foods or food components(lactose) Supplemental vitamin-mineral Encourage clients a nutrient-rich, well-balanced diet Malabsorption Caused by Bacterial Overgrowth Colon normally houses a bacterial population, the small intestine is protected from bacteria overgrowth by gastric acid, which kills bacteria, and peristalsis, which flushes microorganisms through the small intestine before they can flourish Figure 22-3 Consequences of Bacterial Overgrowth Bacteria in the small intestine partly dismantle the bile saltsaffect fat digestion and absorption Fat malabsorption Figure 22-4 The bacteria also compete with the body for vitamin B12 and folate Treatment of Bacterial Overgrowth Antibiotics.(drug therapy) Fat-restricted diets Administered vitamin B12 and oral folate supplements Surgery (If medical treatment failssurgery to remove the blind loop). Short-Bowel Syndrome Syndrome diarrhea, weight loss, muscle wasting, bone disease, protein and fat malabsorption, hypocalcemia, hypomagnesemia, and anemia Short-towel syndrome frequently results from surgery to remove a significant portion of the small intestine, which may be necessary for people with 1.inflammatory bowel diseases 2.cancer of the intestine 3.obstructions 4.fistulas 5.diverticulitis 6.impaired blood supply to the intestine The length, location, and health of the remaining intestine determine the degree to which nutrient absorption is affected Figure 22-5 Extent and Location of the Resection resection(if the terminal ileum, the ileocecal valve, and the colon remain intact) (1) up to 50 percent of the intestine without serious nutrition consequences (2) up to 80 percent may be well tolerated, When the ileum has been resected, however, the absorption of fat, protein, carbohydrate, fat-soluble vitamins, vitamin B12, calcium, and magnesium can be impaired The Ileocecal Valve Without the valve, transit time through the small intestine is rapid, and the time available for nutrient absorption is limited The Colon Bacteria in the colon salvage energy from some of the unabsorbed carbohydrate by metabolizing it to short-chain fatty acids Adaptation Maximum bowel adaptation may take as long as one to two years following a resection. Begin enteral nutrition as early as possible With an extensive bowel resection, however even adaptation will fail to compensate for the reduced surface area Nutrition Support following Small Bowel Resections After surgery, the primary nutrition concern is to maintain fluid and electrolyte balance. 1.For resections of less than 50 percent of the intestine, oral nutrition begins a few days after surgery. A moderate fat-restricted diet with supplemental vitamin B12 is recommended. 2.For more extensive resections, parenteral nutrition is often provided initially to ensure that nutrient needs Enteral nutrition (usually by tube feeding) is initiated as early as possible to stimulate adaptation. Oral intake begins high in complex carbohydrates (60 percent of kcalories) restricted in fat (20 percent of kcalories) low in oxalate If additional energy is needed and if the fat does not precipitate steatorrhea or diarrheafat intake can be liberalized Celiac Disease Celiac disease is a hereditary disorder with an incidence of about 1 in every 2000 to 3000 births. It alters the intestinal mucosal cells, so that they become sensitive to gliadin Gliadin is a fraction of the protein gluten, which is found in wheat, oats, rye, and barley. Gliadin acts as a toxic substance, causing the intestinal villi to atrophy and seriously reducing the absorptive surface of the intestinal tract. Malabsorprion result Deficiency of fat, protein, carbohydrate, fat-soluble vitamins, iron, calcium, magnesium, zinc, and some water-soluble vitamins Nutrition Status Symptoms steatorrhea diarrhea weight loss malnutrition. (1)Anemiairon, folate, or vitamin B12 deficiency (2)Edemaprotein malabsorption(serum protein levels fall dramatically) (3)Precipitate clotting abnormalities and bleed easilyvitamin K deficiency may (4)Tetany and bone paincalcium deficiency Treatment of Celiac Disease Gluten -restricted diets Lactase deficiency and lactose intolerance may be restricted If the person fails to follow the gluten-restricted diet, the symptoms will return, Gluten-Restricted Diets Eliminate gluten wheat, oats, rye, and barley Be careful:ice cream, salad dressings, and canned foods often use wheat flour as an extender Table 22-5 Suggestions Use corn, potato, rice, and soybean flours as substitutes for wheat flour in recipes. A low-gluten wheat starch flour Lactose intolerant will also need to exclude milk and milk products Disorders of the Large Intestine Diverticular disease, ulcerative colitis, and resections of the large intestine Diverticular Disease of the Colon Diverticula bulge out through the muscles surrounding the large intestine, often at points where blood vessels enter the muscles Evidence suggests that the pouches result from high pressure in the intestinal lumen combined with weakness of the supporting muscles in the intestinal wall. Strong intestinal contractions pinch off segments of the Intestine; pressure then builds in these segments arid forces parts of the intestinal membrane to balloon outward through the muscle layer. Aging and low-fiber diets may increase the risk of diverticular disease. Diverticulosis and Diverticulitis Diverticulosisfrequently symptom-free and unaware of the disorder. Diverticulitisfecal material and bacteria get trapped in the diverticula, result inflammation and infection develops Diverticulitis Symptoms abdominal pain alternating periods of diarrhea and constipation dyspepsia flatus abdominal distention fever ※peritonitis(diverticulum ruptures infection) ※If the diverticula become inflamed repeatedly, the intestinal wall can thicken (fibrosis), narrowing the intestinal lumen and creating an obstruction. An inflamed bowel segment can also stick to other pelvic organs, forming a fistula. Nutrition Support Both drugs and diet For many years:Low-fiber diet Now: (a) High-fiber diet(generous servings of plant foods: grains, fruits, and vegetables, especially legumes) (b)But avoid foods with seeds such as okra and strawberries Diverticular diseases do not affect the intestine’s absorptive functions, ulcerative colitis and intestinal resections can have a serious impact on these functions. Ulcerative Colitis An inflammatory bowel disease that develops in the large intestine Symptoms severe diarrhea(malabsorption and major losses of fluids and electrolytes) rectal bleeding cramping abdominal pain anorexia weight loss Anemia(bleeding and nutrient losses). Medical therapy surgery to remove the colon and rectum Nutrition Support Diet No dietary interventions seem to lessen disease activity. People with severe abdominal pain and diarrhea need complete bowel rest with no enteral stimulation. Parenteral nutrition To help maintain nutrition status, espetially when surgery is anticipated. Medications can help to control disease symptoms. Oral Diets Ensure adequate intakes of fluids and electrolytes High-kcalorie, high-protein foods Restricts fat if the client has symptoms of fat malabsorption Individual tolerances determine if other foods should be restricted(lactose intolerance) Supplemental vitamins and minerals may be necessary. Resections of the Large Intestine People with ulcerative colitis or cancer of the colon sometimes need surgery to remove the affected portion of the colon Fluids and electrolytes can be a problem. 1.Colostomy:a segment of the colon, rectum, or both is removed The remaining portion is then brought out through the abdominal wall via a stoma to allow for defecation 2.Ileostomy:both the entire colon and the rectum are removed, and the ileum becomes the terminal GI segment. ※In an alternative to an ileostomy, called the ileal pouch/anal anastomosis, is made at the time of surgery to give the intestine time to heal. After about two to three months, the ileostomy is closed, Figure 22-4 The consistency of the stools depending on both the length and the portion of the resected bowel, In general, ileostomies result in watery stools and colostomies in more formed stools, Nutrition Support following Ostomies Oral intake is permitted following surgery colostomies or ileostomies often receive low-fiber, bland diets (1) to prevent obstructions (2) help promote healing of the stoma (3) prevent GI upsets Try other foods as soon as possible one at a time in small amounts Preventing Obstructions Some foods are more likely than others to be incompletely digested and cause obstructions for ostomates. (1) Stringy foods:celery, spinach, and bean sprouts (2) Foods with tough skins:dried fruits, raw apples, and corn, foods with seeds, mushrooms and nuts. ※Cuts the food into small pieces and chews them thoroughly Encouraging Fluids Drinking fluids helps prevent constipation and dehydration Controlling Diarrhea (1) Foods that thicken the stool and help control diarrhea:applesauce, bananas, cheese, creamy peanut butter, and starchy foods such as breads, rice, and potatoes. (2) Foods that may aggravate diarrhea:apple, grape, and prune juices; highly seasoned foods; and caffeine ※The foods mentioned here are suggestions only; what works for the individual is determined by trial and error Reducing Gas and Odors Gas-forming foods:asparagus, beans, beer, broccoli, brussels sprouts, cabbage, carbonated beverages, cauliflower, eggs, fish, garlic, and onions. Reduce odors foods:buttermilk, cranberry juice, parsley and yogurt. Providing Emotional Support Ostomates will have many adjustments to make after surgery, so emotional support is best begun before surgery occurs