* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download File - Ilford VTS The Home for Trainee GPs in Ilford
Survey
Document related concepts
Transcript
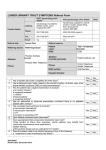
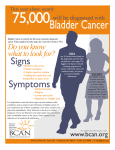
Multiple Sclerosis By Dr A Francis GPST3 Most common cause of neurological disability in young adults after trauma Approximately 14 people are newly diagnosed with MS in the UK each day 100,000 people in the UK have MS In a GP surgery of approx. ……… ………. may have MS. • Multiple Symptoms • Varying Severity • How can we lend our Support • It is a chronic condition that affects the central nervous system. Thought to be due to an autoimmune issue where the myelin, coating around the nerves, becomes damaged. • The exact cause is unknown. Thought to involve multiple genes and various environmental factors that trigger an over active immune response. • Less common in hot tropical regions near the equator but increased incidence in countries like UK regardless of ethnic origin. • Viruses/ bacteria such as EBV thought to be a possible trigger. • Low vitamin D. • 3X more common in women • Presents often in 20s and 30s, but can be younger or later. Multiple Symptoms • People with MS can experience different symptoms • The symptoms patients experience depends on which nerves are affected / location of damage in the CNS • Symptoms can be brief or long lasting • Gps need to think of the possible diagnosis and refer to Neurologist for tests and treatment Case Study: Mrs C • Clinical Presentation: Case History # 1 • Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to fall. Her visual acuity also seemed to change periodically during several years. Two months ago the patient was working very hard and was under a lot of stress. She got sick with a flu and her neurologic condition worsened. At that time, she could not hold objects in her hands, had significant tremors and severe exhaustion. She also had several bad falls. Since that time she had noticed arthralgia on the right and subsequently on the left side of her body. Then, the patient abruptly developed a right hemisensory deficit after several days of work. The MRI scan was performed at that time and revealed a multifocal white matter disease areas of increased T2 signal in both cerebral hemispheres. Spinal tap was also done which revealed the presence of oligoclonal bands in CSF. Visual evoked response testing was abnormal with slowed conduction in optic nerves. (Q.1) (Q. 2) (Q.3) • Today, the patient has multiple problems related to her disease: she remains weak and numb on the right side; she has impaired urinary bladder function which requires multiple voids in the mornings, and nocturia times 3. She became incontinent and now has to wear a pad during the day. (Q.4) She also has persistent balance problems with some sensation of spinning, and she is extremely fatigued. • REVIEW OF SYSTEMS is also significant for a number of problems related to her suspected MS. The patient has a tendency to aspirate liquids and also solids. (Q.5) (Q.6) She complains of tinnitus which is continuous and associated with hearing loss, more prominent on the left. She has decreased finger dexterity and weakness of the hands bilaterally. She also complains of impaired short-term memory and irritability. • FAMILY HISTORY is significant for high blood pressure, cancer and heart disease in the immediate family. • PERSONAL HISTORY is significant for mumps and chicken pox as a child, and anemia and allergies with hives later in life. She also had a tubal ligation. NEUROLOGIC EXAMINATION: • Cranial Nerve II - disks are sharp and of normal colour. • Funduscopic examination is normal. Cranial Nerves III, IV, VI - no extraocular motor palsy or difficulties with smooth pursuit or saccades are seen. Remainder of the cranial nerve exam is normal except for decreased hearing on the left, and numbness in the right face, which extends down into the entire right side. The Weber test reveals greater conductance to the right. Rinne's test reveals air greater than bone bilaterally. (Q.7) The palate elevates well. Swallow appears to be intact. Tongue movements are slowed, but tongue power appears to be intact. • Motor examination reveals relatively normal strength in the upper extremities throughout. However, rapid alternating movements are decreased in both upper extremities and the patient has dysdiadochokinesia in the left hand. (Q.8) Mild paraparesis is noted in both legs without severe spasticity. • Deep tendon reflexes are +2 and symmetrical in the arms, +3 at the ankles and at the knees. Bilateral extensor toe sign are present. • Sensory exam reveals paresthesia on the right to touch and decreased pin sensation on the right diffusely. The patient has mild vibratory sense loss in the distal lower extremities. • Romberg's is negative. (Q.9) Tandem gait is mildly unstable. • Presenting / Early Symptoms of MS A) B) C) D) E) F) Vison Problems: Optic Neuritis, Diplopia, Nystagmus Balance disturbance / Dizziness Loss of sensation in different areas of the body (Numbness) Weakness in one or more limbs ( eg. Legs giving way) Stiffness / slow movements / Spasms Tremors Varying Severity • Each person’s experience of MS is unique • The disease progresses differently for different people • In general the progression of the disease: A) 85% : Relapsing and Remitting B) Secondary Progressive C) 10-15%: Primary Progressive Refer to Neurology for Tests • McDonalds criteria for diagnosis • MRI Scanning • Evoked Potentials • Lumbar Puncture Various Possible Complications & Implications • Complications from the disease itself and from medications • Affect multiply systems, if severe can be life threatening a) Bladder - recurrent UTIs, urge incontinence, incomplete emptying b) Bowel – constipation, incontinence c) Reduced mobility – pressure sores, cellulitis, DVT, risk of amputations d) Pain / Fatigue e) Speech & Swallowing f) Memory & Thinking • The implications for daily life a) Physical – eg, use of wheelchair, driving, poor sleep b) Work life – studies, employment c) Social / Family life – home, relationships, children d) Emotional – fear of the unpredictable, dependence, social isolation, reduced self esteem So how can we Support those living with MS • Medical Care - Prompt diagnosis and medical intervention: MDT approach - Preventing & Managing complications - Improving access to health services for those with disabilities • Social care • Emotional support - compassionate care that encourages hope Drugs to treat relapses in MS • High dose steroids for acute relapses • Aim of DMT (Disease Modifying Therapies) is to reduce the number and severity of relapses • To slow down progression of disease • Drugs work by dampening the immune system and reducing inflammation • As a GP consider possible complications / side effects eg risk of infections, thyroid disorder, blood disorder Treating Symptoms Main Symptom Solutions Impaired vision : Optic Neuritis Diplopia Nystagmus Steroid, avoid trigger eg heat Eye patch, glasses Gabapentin Constipation Fluid intake, balanced diet, exercise/activity Laxatives, suppository/enema Bladder urgency and incontinence Exclude UTI ? retaining – residual >100mls intermittent self catheterisation Oxybutynin, Solifenacin, Botox to bladder wall Suprapubic catheter Surgery Incomplete Bladder emptying Stiffness & Spasms Physio + OT Baclofen, Gabapentin, diazepam Pain Gabapentin, pregablin Depression Psychological therapies, Amitriptyline, fluoxetine, citalopram Adapting & Inspiring https://www.youtube.com/watch?v=C5-31p3-lzA